Hussien Mohammed Jumaah
CABMLecturer in internal medicine
Mosul College of Medicine
2016
learning-topics
Medical psychiatryPsychiatric disorders have traditionally been considered
as ‘mental’ rather than as ‘physical’ illnesses. This isbecause they manifest with disordered functioning in
the areas of emotion, perception, thinking and memory,
and/or have had no clearly established biological basis.
However, as research identifies abnormalities of the
brain in an increasing number of psychiatric disorders
and an important role for psychological and behavioural
factors in many medical illnesses, a clear distinction
between mental and physical illness has become increasingly questionable. We therefore refer to psychiatric disorders simply to mean those conditions traditionally regarded as the province of psychiatry.
CLASSIFICATION OF PSYCHIATRIC DISORDERS
There are two main classifications of psychiatric disorders in current use:
• the American Psychiatric Association’s Diagnostic
and Statistical Manual (4th edition), or DSM-IV
• the World Health Organization’s International
Classification of Disease (10th edition), known as
ICD-10.
The two systems are similar; here we use the ICD-10
classification .
Classification of psychiatric disorders
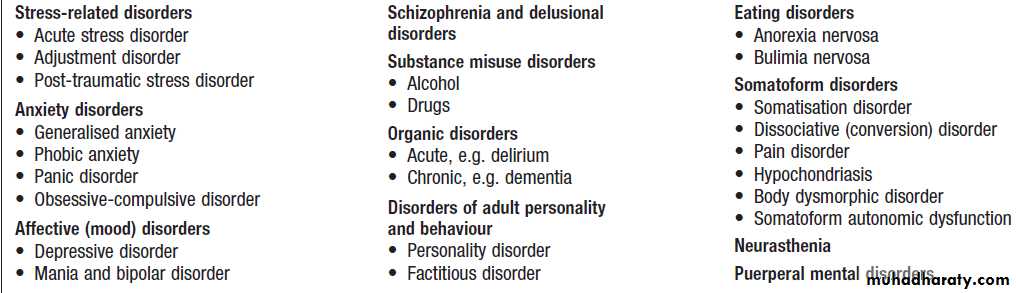
EPIDEMIOLOGY OF PSYCHIATRIC DISORDERSPsychiatric disorders are amongst the most common of
all human illnesses. The relative frequency of each varies
with the setting (Box).
In the general population,
depression, anxiety disorders and adjustment disorders
are most common (10%) and psychosis is rare (1–2%);
In acute medical wards of general hospitals, organic disorders such as delirium (20–30%) are prevalent;
in specialist general psychiatric services, psychoses are the most common disorders.
Prevalence of psychiatric disorders by medical setting
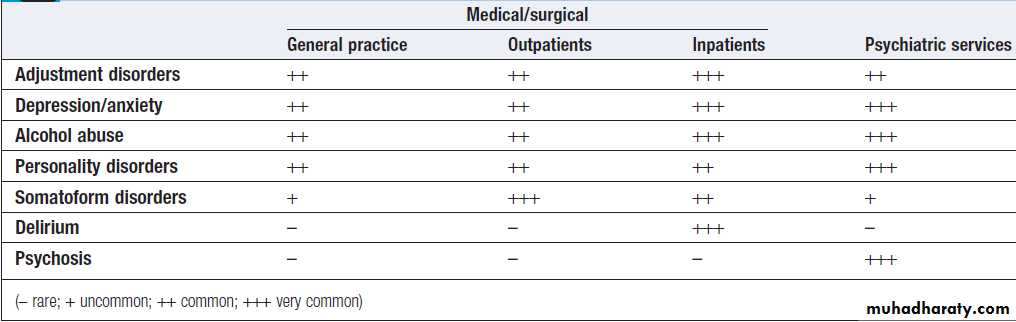
Classification of aetiological factors in
psychiatric disordersAETIOLOGY OF PSYCHIATRIC DISORDERS
The aetiology is multifactorial, with a combination of biological, psychological and social causes.Biological factors
Genetic
Genetic factors play a predisposing role in many psychiatric disorders, including schizophrenia and bipolar affective disorder. However, whilst some disorders such as Huntington’s disease are due to mutations in a single gene, the genetic contribution to most psychiatric disorders is polygenic in nature and mediated by the combined effects of several genetic variants, each with modest effects and modulated by environmental factors.
Brain structure and function
Brain structure is grossly normal in most psychiatricdisorders, although abnormalities may be observed
in some conditions, such as generalised atrophy in
Alzheimer’s disease and enlarged ventricles with a
slight decrease in brain size in schizophrenia. The
functioning of the brain, however, is commonly altered
with, for example, changes in neurotransmitters such
as dopamine, noradrenaline (norepinephrine) and
5-hydroxytryptamine (5-HT, serotonin), and differences
in activity of specific areas of the brain, as seen on functional brain scans.
Psychological and behavioural factors
Early environment
Childhood emotional deprivation or abuse, predisposes to psychiatric disorders such as depression and eating disorders.
Personality
The relationship can be difficult to assess because the development of psychiatric disorder can change a patient’s personality. However, some personality types predispose
to psychiatric disorder; for example, a depressive personality increases the risk of depression. A disordered personality may also perpetuate a psychiatric disorder. Behaviour
Predispose to the development of a disorder (e.g. excess alcohol intake leading to dependence, and dieting to anorexia) or perpetuate it.
Social and environmental factors
Social isolationThe lack of a close, confiding relationship predisposes
to some psychiatric disorders such as depression. The
reduced social support resulting from having a psychiatric
disorder may also act to perpetuate it.
Stressors
Social and environmental stressors often play an important role in precipitating psychiatric disorder in those
who are predisposed. For example, trauma in posttraumatic stress disorder, losses (such as bereavement)
in depression, and events perceived as threatening (such
as potential loss of employment) in anxiety.
DIAGNOSING PSYCHIATRIC DISORDERS
Differs from a standard medical assessment :• There is greater emphasis on the history.
• It includes a systematic examination of the patient’s
thinking, emotion and behaviour (mental state).
• It commonly includes the routine interviewing of an
informant (usually a relative or friend who knows
the patient), especially when the illness affects the
patient’s ability to give an accurate history.
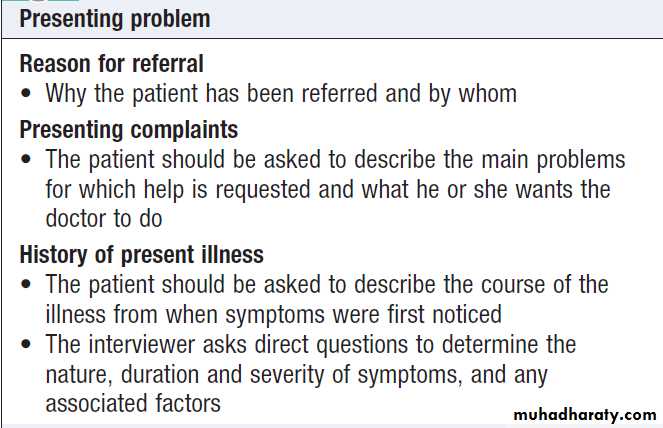
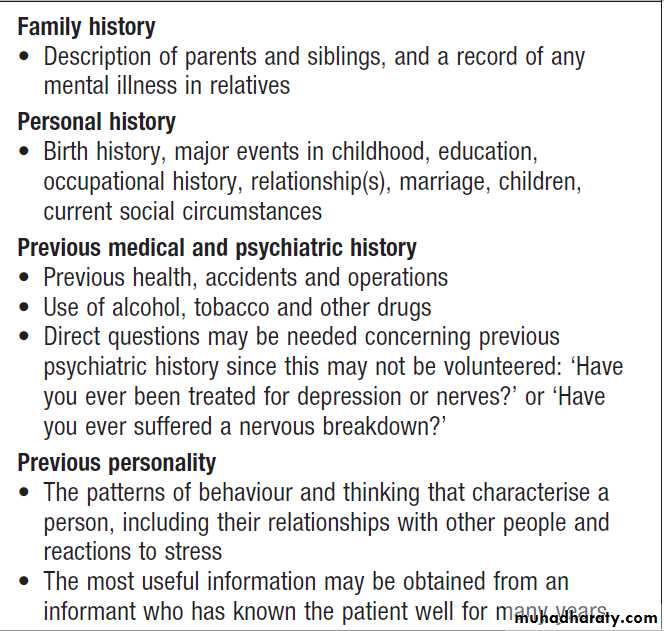
Because of its greater complexity, a full psychiatric history (Box) and detailed mental state examination (MSE) may take an hour or more. However, a brief mental state examination, usually taking no more than a few minutes (see below), should be part of the assessment of all patients, not merely those deemed to be ‘psychiatric’.
How to structure a psychiatric interview
How to structure a psychiatric interview
– cont’dPsychiatric interview
The aims of the interview are to:• establish a therapeutic relationship with the patient
• elicit the symptoms, history and background information
• examine the mental state
• provide information, reassurance and advice.
Whilst some aspects of the patient’s mental state
may be observed whilst the history is being taken, specific enquiries for important features should always be made.
Mental state examination
General appearance and behaviour
Any abnormalities of alertness or behaviour, such
as restlessness or retardation, are noted. The level of
consciousness, especially in the assessment of delirium.
Speech
Speed and fluency should be observed, including slow
(retarded) speech and word-finding difficulty.
‘Pressure of speech’ describes rapid speech that is difficult to interrupt.
Mood
Judged by facial expression, posture and movements. Patients should also be asked if they feel sad or depressed and if they lack ability to experience pleasure (anhedonia).
Are they anxious, worried or tense? Is mood elevated with excess energy and a reduced need for sleep, as in mania?
Thoughts
The content of thought can be elicited by asking ‘What
are your main concerns?’ Is thinking negative, guilty or
hopeless, suggesting depression?
Are there thoughts of self-harm?
If so, enquiry should be made about plans. Is he or she excessively worried about many things, suggesting anxiety? Does the patient think that he or she is especially powerful, important or gifted (grandiose thoughts), suggesting mania? The form of thinking may also be abnormal.
In schizophrenia, patients may display loosened associations between ideas, making it difficult to follow their train of thought. There may also be abnormalities of thought possession, when patients experience the intrusion of alien thoughts into their mind or the broadcasting of their own thoughts to other people.
Abnormal beliefs
A delusion is a false belief, out of keeping with a patient’s
cultural background, which is held with conviction
despite evidence to the contrary .
Abnormal perceptions
Illusions are abnormal perceptions of real stimuli. Hallucinations are sensory perceptions which occur in the
absence of external stimuli: for example, hearing voices when no one is present.
Cognitive function
The Mini-Mental State Examination (MMSE) is a useful
screening questionnaire to detect cognitive impairment.
A score of less than 24 out of 30 typically suggests cognitive impairment. A brief assessment is as follows:
• Memory. Registration of memories is tested by asking
the patient to repeat simple new information, such as a name and address, immediately after hearing it.
Short-term memory is assessed by asking him or her to repeat it after an interval of 1–2 minutes, during which time the patient’s attention should be diverted elsewhere. Long-term memory is assessed by gauging the recall of previous events.
• Concentration. Serial 7s is a test in which the patient
is asked to subtract 7 from 100 and then 7 from theanswer, and so on.
• Orientation. This is assessed by asking the patient
about place – his or her exact location; time – what
day, date, month and year it is now; and person
– details of personal identity, such as name, date of
birth, marital status and address.
• Intellectual ability. This can be gauged from the
history of the patient’s educational background and
attainments but can also be assessed during the
interview from the patient’s speech, vocabulary and
grasp of the interviewer’s questions.
Note that the degree of cognitive impairment in delirium
typically fluctuates over time, and consequently may be missed by a single assessment.
Patients’ own understanding of their symptoms (‘insight’)
Patients should be asked what they think their symptoms
are due to, and whether they warrant treatment.
Lack of insight refers to a failure to accept that one is ill
and/or in need of treatment,
and is characteristic of acute psychosis.
PRESENTING PROBLEMS IN PSYCHIATRIC ILLNESS
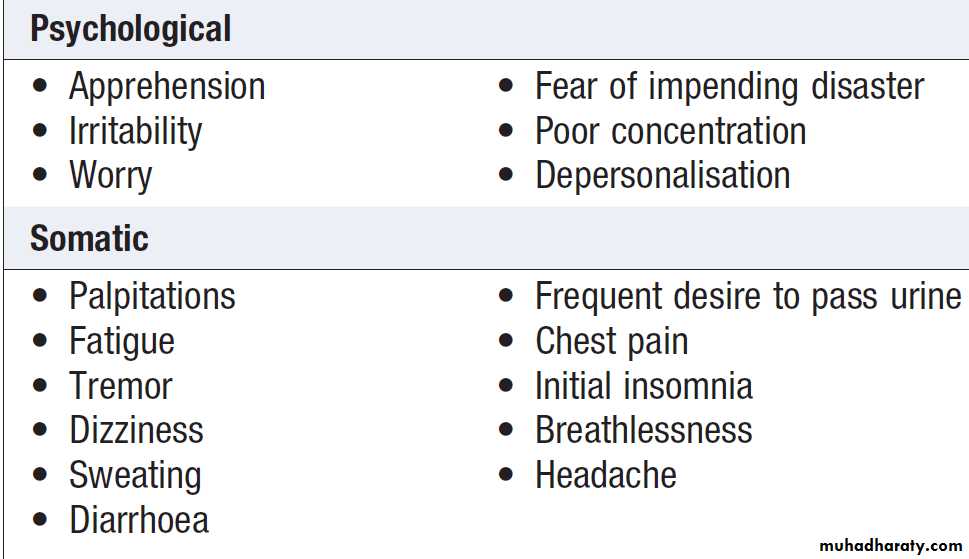
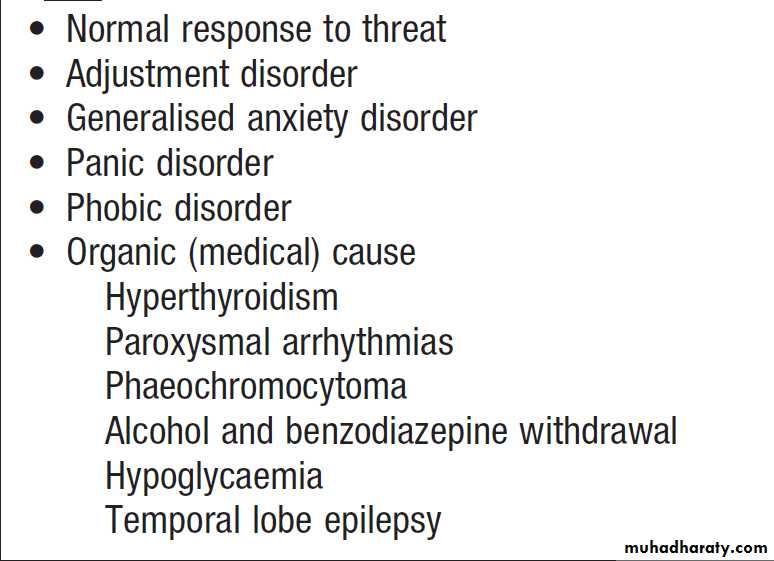
Anxiety symptomsAnxiety may be transient, persistent, episodic or limited
to specific situations. The symptoms of anxiety are both
psychological and somatic (Box). The differential
diagnosis of anxiety is shown in Box. Most anxiety
is part of a transient adjustment to stressful events:
adjustment disorders . Anxiety may occasionally be a manifestation of a medical condition such as thyrotoxicosis.
Symptoms of anxiety disorder
Differential diagnosis of anxiety
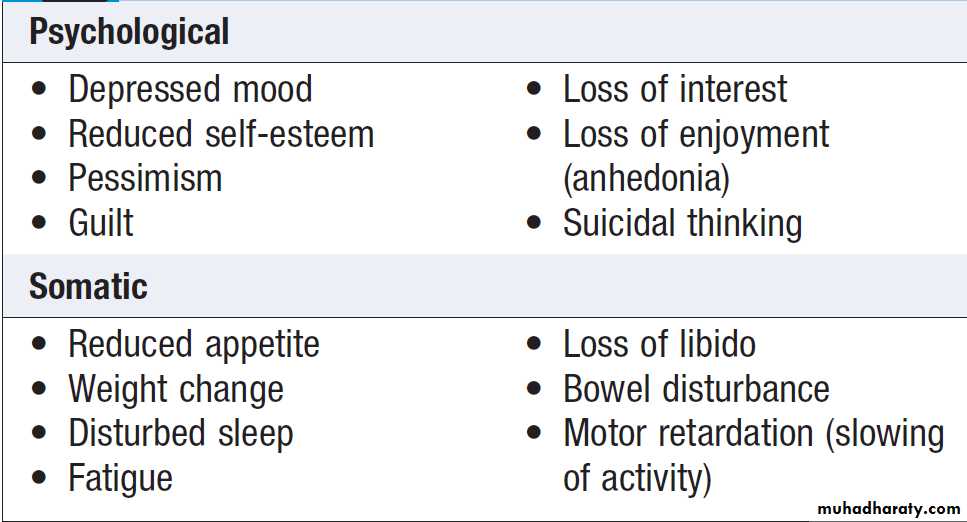
Depressed moodDepressive disorder is common, with a prevalence of
approximately 5% in the general population. Depression
is at least twice as common in the medically ill. It
is important to note that depression has physical as
well as mental symptoms (Box). The diagnosis of
depression in the medically ill, who may have physical
symptoms of disease, relies on detection of the core
psychological symptoms of low mood and anhedonia.
Symptoms of depressive disorders
Differential diagnosis
Depressive disorder must be differentiated from an
adjustment disorder with depressed mood.
Adjustment disorders are common, self-limiting reactions
to adversity, including physical illness, which are
transient and require only general support.
Depressive disorders are characterised by a more severe and persistent disturbance of mood and require specific
treatment.
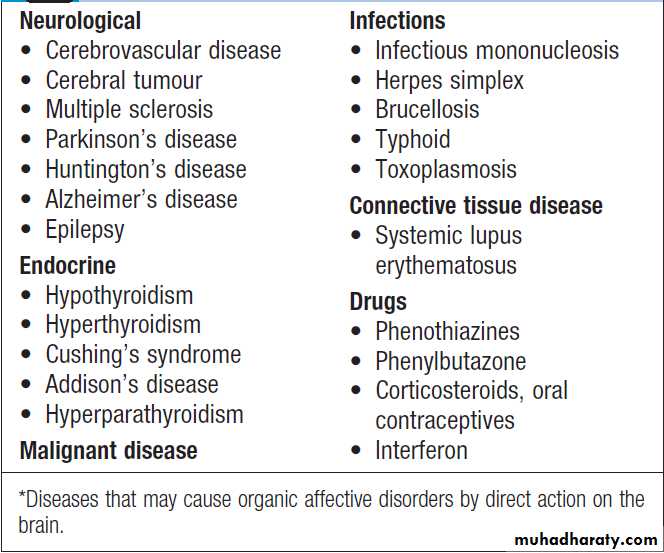
In some cases, depression may occur as a result of a direct effect of a medical condition or its treatment on the brain, when it is referred to as an ‘organic mood disorder’.
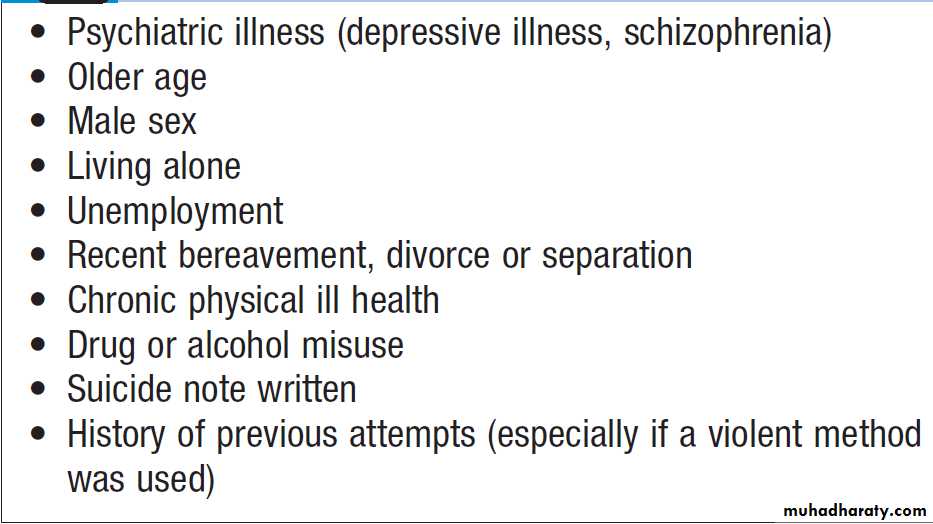
Suicide
Depression is the major risk factor for suicide. Other riskfactors are shown in Box. When depression is suspected,
tactful enquiry should always be made into suicidal
thoughts and plans.
Asking about suicide does not increase the risk of it occurring, whereas failure to enquire denies the opportunity to prevent it.
Organic mood disorders*
Risk factors for suicide
Elated moodElation, or euphoria, is the converse of depression and
is characteristic of mania. It may manifest as infectious
joviality, over-activity, lack of sleep and appetite, undue
optimism, over-talkativeness, irritability, and recklessness
in spending and sexual behaviour. When elated
mood is severe, psychotic symptoms are often evident,
such as delusions of grandeur (e.g. believing erroneously
that one is royalty). Elevated mood is much less common than depressed mood, and in medical settings
is often secondary to drug or alcohol misuse, an organic
disorder or medical treatment. Where none of these
applies, the patient may have a bipolar disorder.
Medically unexplained somatic symptoms
Patients commonly present to doctors with physicalsymptoms. Whilst these symptoms may be an expression
of a medical condition, they often are not. They
may then be referred to as ‘medically unexplained
symptoms’ (MUS). MUS are very common in patients
attending general medical outpatient clinics. Almost any
symptom can be medically unexplained, e.g.:
• pain (including back, chest, abdominal and headache)
• fatigue
• dizziness
• fits, ‘funny turns’ and feelings of weakness.
Patients with MUS may receive a medical diagnosis
of a so-called functional somatic syndrome, such as irritable
bowel syndrome (Box), and may also merit a
psychiatric diagnosis on the basis of the same symptoms.
The most frequent psychiatric diagnoses associated
with MUS are anxiety or depressive disorders.
When these are absent, a diagnosis of somatoform disorder may be appropriate.
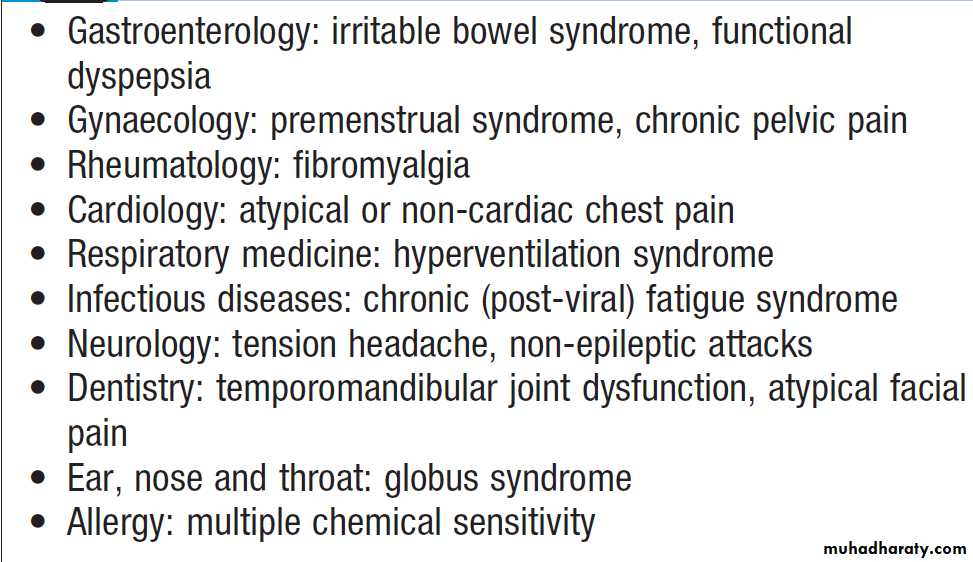
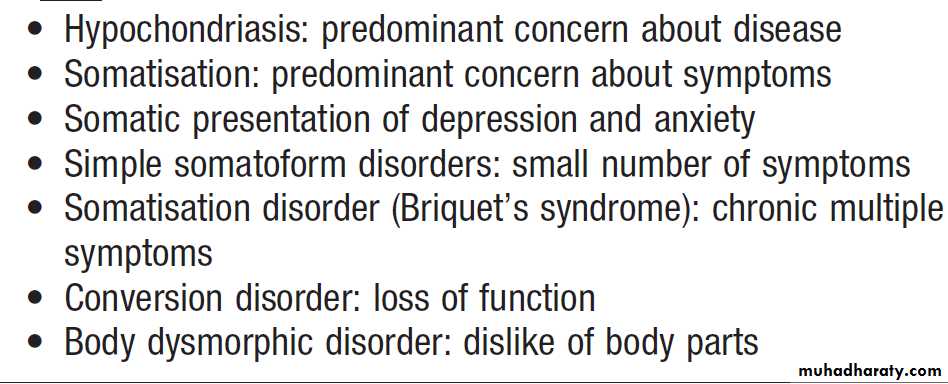
Functional somatic syndromes
Psychiatric diagnoses for medically unexplained somatic symptoms
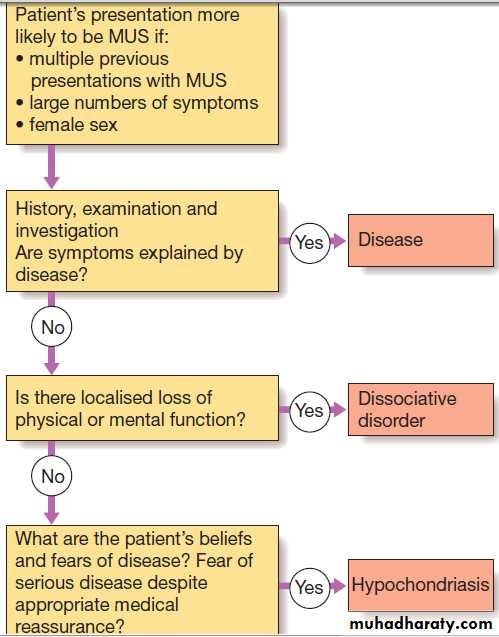
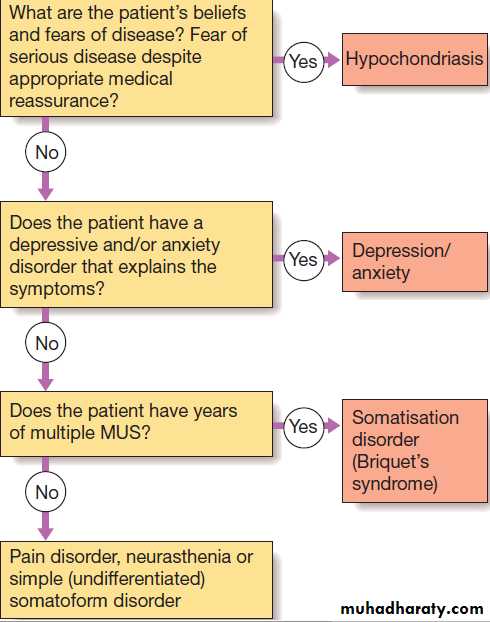
Differential diagnosisThe main medical differential diagnosis for MUS is from
symptoms of a medical disease. Diagnostic difficulties
are most likely with unusual presentations of common
diseases and with rare diseases. MUS are commonly an expression of depression and anxiety. A medical and
psychiatric assessment should be completed in all cases .
Diagnosis of medically unexplained symptoms (MUS).
Delusions and hallucinationsDelusions
Various types of delusion are identified on the basis of
their content. They may be:
• persecutory, such as a conviction that others are out
to get me
• hypochondriacal, such as an unfounded conviction
that one has cancer
• grandiose, such as a belief that one has special
powers or status
• nihilistic, e.g. ‘My head is missing’, ‘I have no
body’, ‘I am dead’.
Delusions should be differentiated from over-valued
ideas, which are strongly held but not fixed.
Hallucinations
These are perceptions without external stimuli. They
can occur in any sensory modality, most commonly
visual or auditory. Typical examples are hearing voices
when no one else is present, or seeing ‘visions’. Hallucinations have the quality of ordinary perceptions and
are perceived as originating in the external world, not
in the patient’s own mind (when they are termed
pseudo-hallucinations). Those occurring when falling
asleep (‘hypnagogic’) and on waking (‘hypnopompic’)
are not pathological. Hallucinations should be distinguished
from illusions, which are misperceptions of real external stimuli (such as mistaking a shrub for a person in poor light).
Differential diagnosis
Agitation, terror or the fear of being thought ‘mad’may make patients unable or unwilling to volunteer or
describe their abnormal beliefs or experiences. Careful
and tactful enquiry is therefore required. The nature
of hallucinations can be important diagnostically; for
example, ‘running commentary’ voices that discuss the
patient are strongly associated with schizophrenia. In
general, auditory hallucinations suggest schizophrenia,
while hallucinations in other sensory modalities, especially
vision but also taste and smell, suggest an ‘organic
psychosis’ such as delirium or temporal lobe epilepsy. Hallucinations and delusions often co-occur; if their
content is consistent with coexisting emotional symptoms,
they are described as ‘mood-congruent’.
Thus, patients with severely depressed mood may believe
themselves responsible for all the evils in the world, and
hear voices saying ‘You’re worthless. Go and kill yourself.’In this case, the diagnosis of depressive psychosis
is made on the basis of the congruence of different
phenomena (mood, delusion and hallucination). Incongruence between hallucinations, delusions and mood
suggests schizophrenia. Where hallucinations and delusions arise within disturbed consciousness and impaired cognition, the diagnosis is usually an organic disorder, most commonly delirium and/or dementia .This differential
diagnosis is made by assessing the nature, extent and
time course of any cognitive disturbances, and by investigating for underlying causes.
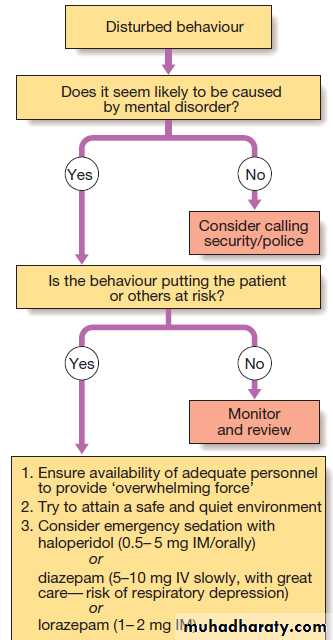
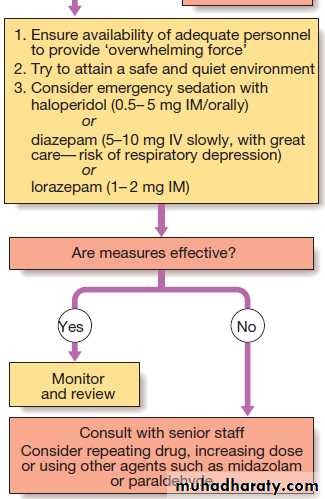
Disturbed and aggressive behaviour
Is common in general hospitals, especially in emergency departments. Most behavioural disturbance arises not from medical or psychiatric illness, but from alcohol intoxication, reaction to the situation and personality characteristics. Thekey principles of management are, first, to establish
control of the situation rapidly and thereby ensure the safety of the patient and others, and, second, to assess
the cause of the disturbance in order to remedy it. Hospital security staff and sometimes the assistance of the police may be required. In all cases, the staff approach is
important; a calm, non-threatening manner expressing
understanding of the patient’s concerns is often all that
is required to defuse potential aggression (Box).
If sedating drugs are required, antipsychotic drugs,
such as haloperidol, and benzodiazepines, such asdiazepam, are commonly used. The choice of drug, dose,
route and rate of administration will depend on the patient’s age, sex and physical health, as well as the
likely cause of the disturbed behaviour. Haloperidol can cause acute dystonias, including oculogyric crises, the benzodiazepines can precipitate respiratory depression in patients with lung disease, and encephalopathy in those with liver disease.Thus, for a frail with emphysema and delirium, sedation may be achieved with a low dose (0.5 mg) of oral haloperidol, while for a strong young man with an acute psychotic episode, at least 10 mg of IVdiazepam and a similar dose of haloperidol may be needed.
A parenterally administered anticholinergic agent, such as procyclidine, should be available to treat extrapyramidal effects arising from haloperidol, and flumazenil to reverse respiratory depression if large doses of benzodiazepines are used.
Differential diagnosis
Many factors may contribute to disturbed behaviour.
When the patient is cooperative, these are best determined at interview. Other sources of information about the patient include medical and psychiatric records, and discussion with nursing staff, family members and other
informants, including the patient’s general practitioner.
The following information should be sought:
• psychiatric, medical (neurological) andcriminal history• current psychiatric and medical treatment
• alcohol and drug misuse
• recent stressors
• the time course and accompaniments of the current
episode in terms of mood, belief and behaviour. Observation of the patient’s behaviour may also yield
useful clues.
Do they appear to be responding to hallucinations?
Are they alert or variably drowsy and confused?
Are there physical features suggestive of drug or
alcohol misuse or withdrawal?
Are there new injuries or old scars, especially on the head? Do they smell of alcohol or solvents?
Do they bear the marks of drug injection?
Are they unwashed and unkempt, suggesting a gradual development of their condition?
If the person has an acute psychiatric disorder, then
admission to a psychiatric facility may be indicated. If a
medical cause is likely, psychiatric transfer is usually
inappropriate and the patient should be managed in a
medical setting, with whatever nursing and security
support is required.
Where it is clear that there is no medical or psychiatric illness, the person should be removed from the hospital, to police custody if necessary.
Measures such as restraint, sedation, the investigation
and treatment of medical problems, and psychiatric transfer all raise legal as well as medical issues .
In most countries, including the UK, common law
confers upon doctors the right, and indeed the duty, to
intervene against a patient’s wishes in cases of acute
behavioural disturbance, if this is necessary to protect
the patient or other people. Many countries, such as the
UK, also have specific mental health legislation that may
be used to detain patients.
Acute management of disturbed behaviour.
Psychiatric emergencies
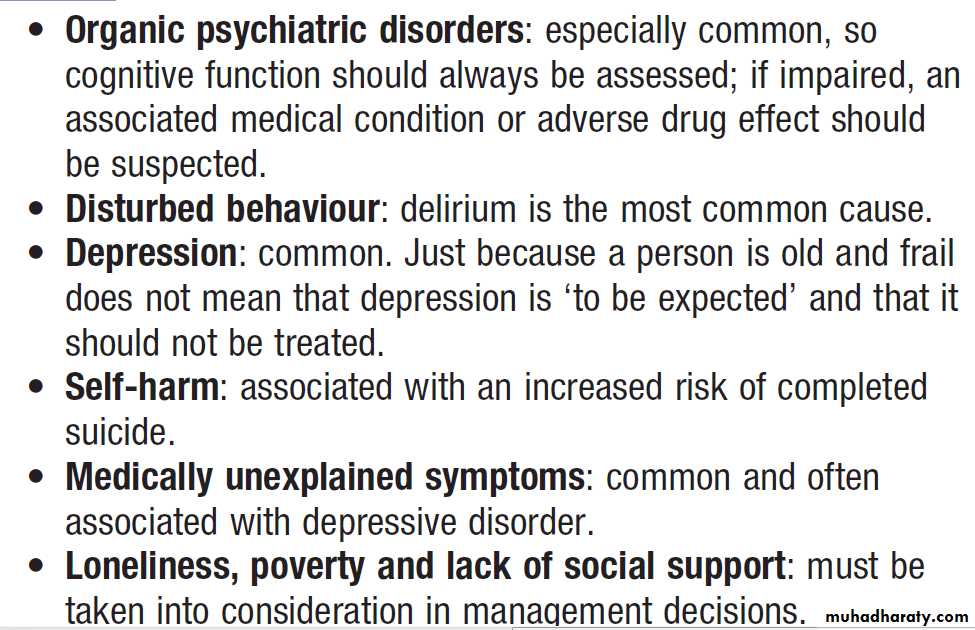
Medical psychiatry in old age
ConfusionThis is a vague term used to describe a range of primarily
cognitive problems, including disturbances in
perception, belief and behaviour. ‘Confusion’ usually
presents as a problem when it becomes clear that the
patient cannot comply with medical care; they may
repeatedly wander off the ward, pull out essential cannulae and catheters, and hit nurses. The methods of
assessment of cognitive function range from simple
screening questions to detailed psychometric testing. All
doctors should be able to undertake a brief cognitive
assessment, as outlined above.
Differential diagnosis
A history from the patient and informants is essentialto establish the time course, variability and functional
consequences of any cognitive deficit. Mental state
examination is necessary to seek evidence of associated
mood disorder, hallucinations, delusions or behavioural
abnormalities, and physical examination to identify any
relevant medical conditions.
The assessment should seek to distinguish between:
• organic disorders such as delirium, dementia, and
focal deficits secondary to brain lesions
• psychiatric disorders such as depressive pseudodementia
and dissociative disorder
• malingering
Self-harm
Self-harm (SH) is a common reason for presentation
to medical services. The term ‘attempted suicide’ is potentially misleading, as most such patients are not
unequivocally trying to kill themselves. Most cases of
SH involve overdose, of either prescribed or nonprescribed
drugs . Less common methods include
asphyxiation, drowning, hanging, jumping from a
height or in front of a moving vehicle, and the use of
firearms. Methods that carry a high chance of being fatal
are more likely to be associated with serious psychiatric
disorder. Self-cutting is common and often repetitive,
but rarely leads to contact with medical services.
The incidence of SH varies over time and between
countries. In the UK, the lifetime prevalence of suicidalideation is 15% and that of acts of SH is 4%. SH is more
common in women than men, and in young adults than
the elderly. (In contrast, completed suicide is more
common in men and the elderly (see Box).) There is
a higher incidence of self-harm among lower socioeconomic groups, particularly those living in crowded,
socially deprived urban areas. There is also an association
with alcohol misuse, child abuse, unemployment
and recently broken relationships.
Differential diagnosis
The main differential diagnosis is from accidental poisoning
and so-called ‘recreational’ overdose in drug
users. It must be remembered that SH is not a diagnosis
but a presentation, and may be associated with any psychiatric diagnosis, the most common being adjustment
disorder, substance and alcohol misuse, depressive disorder and personality disorder. In many cases, however,
no psychiatric diagnosis can be made.
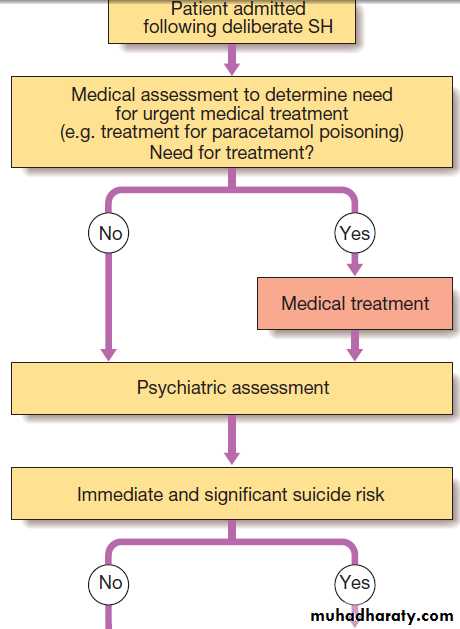
Initial management
A thorough psychiatric and social assessment shouldbe attempted in all cases (Fig.), although some
patients will discharge themselves before this can take
place. The need for psychiatric assessment should not,
however, delay urgent medical or surgical treatment,
and may need to be deferred until the patient is well
enough for interview.
The purpose of the psychiatric assessment is to:
• establish the short-term risk of suicide
• identify potentially treatable problems, whether
medical, psychiatric or social.
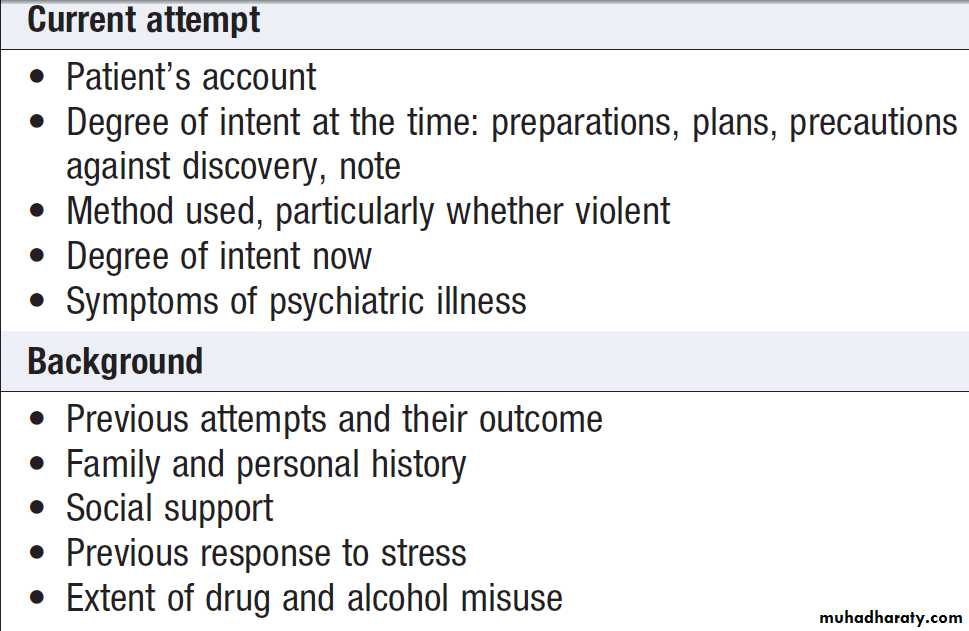
Topics to be covered when assessing a patient are
listed in Box.
Assessment of patients after self-harm
Assessment of patients admitted following self-harm (SH).
The history should include events occurring immediately before and after the act, and especially any evidence of planning. The nature and severity of any current psychiatric symptoms must be assessed, along with the personal and social supports available to the patient outside hospital.Most SH patients have depressive and anxiety symptoms
on a background of chronic social and personal difficulties and alcohol misuse but no psychiatric disorder.
They do not usually require psychotropic medication or specialised psychiatric treatment but may benefit from personal support and practical advice from a GP, social worker or community psychiatric nurse.
Admission to a psychiatric ward is necessary only for
persons who:• have an acute psychiatric disorder
• are at high risk of suicide
• need temporary respite from intolerable circumstances
• require further assessment of their mental state.
Approximately 20% of SH patients make a repeat
attempt during the following year and 1–2% kill themselves.
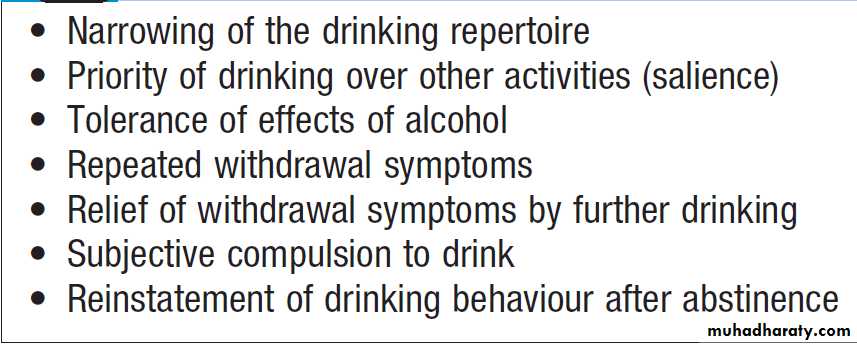
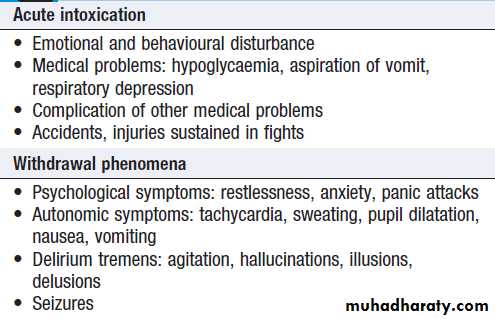
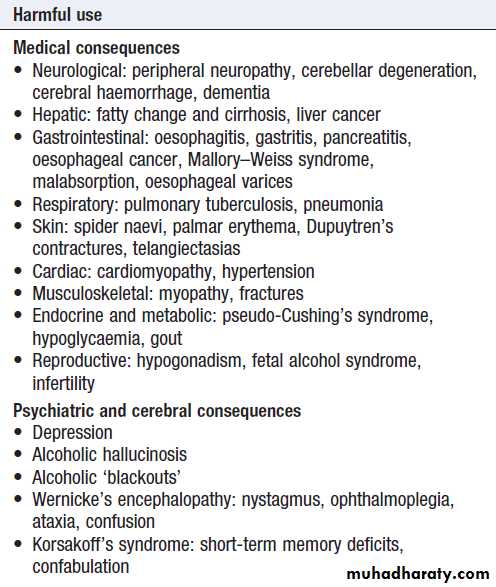
Alcohol misuse
Misuse of alcohol is a major problem worldwide. It
presents in a multitude of ways . In many cases, the link to alcohol will be all too obvious; in others, it may not be. Denial and concealment of alcohol intake are common.
In the assessment of alcohol intake, the patient should be asked to describe a typical week’s drinking, quantified in terms of units of alcohol (1 unit contains approximately 8 g alcohol and is the equivalent of half a pint of beer, a single measure of spirits or a small glass of wine). Drinking becomes hazardous at levels above 21 units weekly for men and 14 units weekly for women.
The history from the patient may need corroboration by the GP, earlier medical records and family members. The mean cell volume (MCV) and γ-glutamyl transferase (GGT) may be raised, but are abnormal in only half of problem drinkers; consequently, normal results on these tests do not exclude an alcohol problem.
When abnormal, these measures may be helpful in challenging denial and monitoring treatment response.
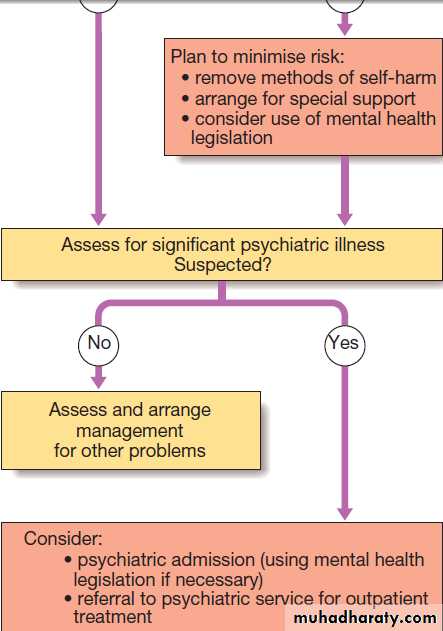
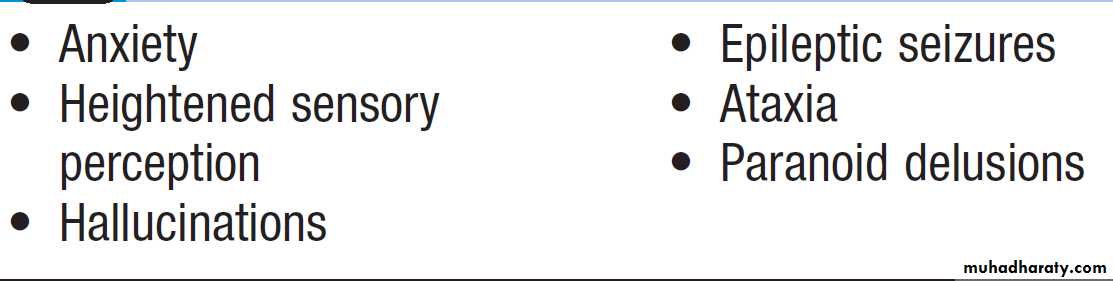
Substance misuse
The misuse of drugs of all kinds is also widespread.There are two additional sets of problems associated with drug misuse:
• problems linked with the route of administration,
such as intravenous injection
• problems arising from pressure applied to doctors
to prescribe the misused substances.
Substance misuse: additional presenting problems
Psychological factors affecting medical conditions
Psychological factors may influence the presentation,
management and outcome of medical conditions. Specific
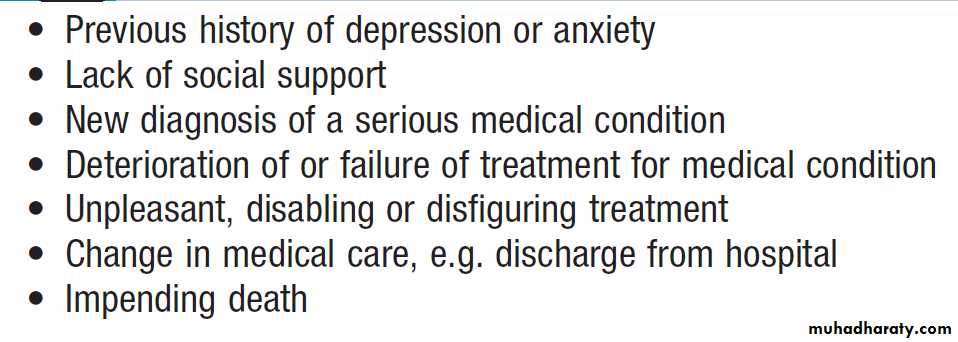
factors are shown in Box. The most common
psychiatric diagnoses in the medically ill are anxiety and depressive disorders. Often these appear understandable as adjustments to illness and its treatment; however, if the anxiety and depression are severe and persistent, they may complicate the management of the medical condition and active management is required. Anxiety may present as an increase in somatic symptoms such as breathlessness, tremor or palpitations, or as the avoidance of medical treatment.
It is most common in those facing difficult or painful treatments, deterioration of their illness or death. Depression may manifest as increased physical symptoms such as pain or fatigue and disability, as well as with depressed mood and loss of interest and pleasure. It is most common in patients who have suffered actual or anticipated losses, such as receiving a terminal diagnosis or undergoing disfiguring surgery.
Treatment is by psychological and/or pharmacological
therapies, as described below. Care is required when
prescribing psychotropic drugs to the medically ill in
order to avoid exacerbation of the medical condition and
harmful interactions with other prescribed drugs.
Risk factors for psychological problems associated with medical conditions
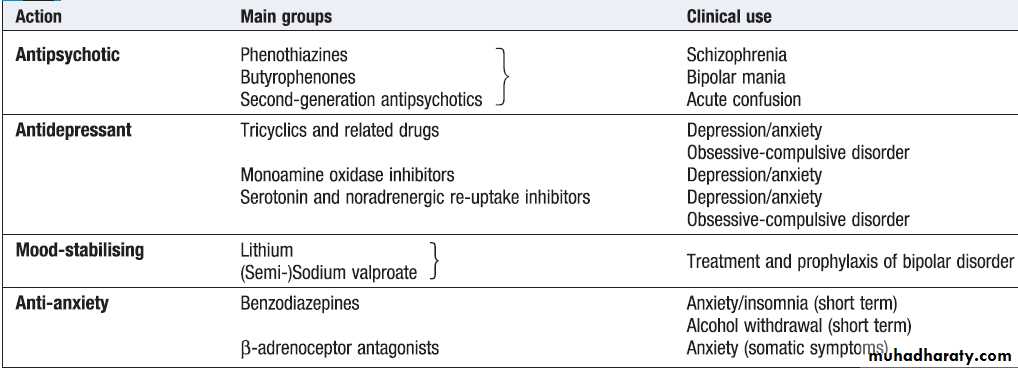
TREATING PSYCHIATRIC DISORDERSThe multifactorial origin of most psychiatric disorders
means that there are multiple potential targets for
treatment.
Biological treatments
These aim to relieve psychiatric disorder by modifying
brain function. The main biological treatments are
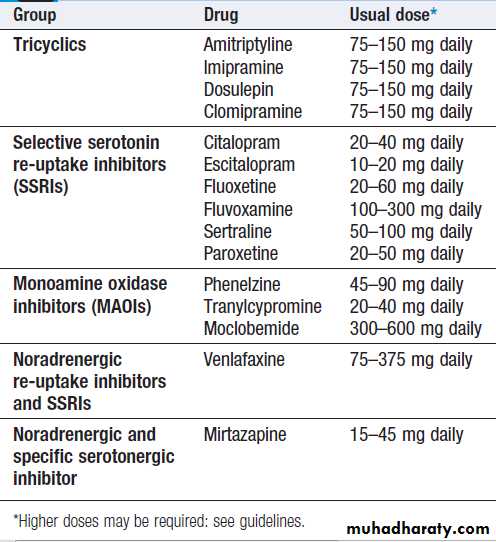
psychotropic drugs. These are widely used for various purposes; a pragmatic classification is set out in Box. It should be noted that some drugs have applications to more than one condition; for example, antidepressants are also widely used in the treatment of anxiety and chronic pain. The specific subgroups of psychotropic drugs are discussed in the sections on the appropriate disorders.
Electroconvulsive therapy (ECT) entails producing a
convulsion by the administration of high-voltage, brief,
direct-current impulses to the head while the patient
is anaesthetised and paralysed by muscle relaxant. If
properly administered, it is remarkably safe, has few
side-effects, and is of proven efficacy for severe depressive illness. There may be amnesia for events occurring a few hours before ECT (retrograde) and after it (anterograde).
Pronounced amnesia can occur but is infrequent and difficult to distinguish from the effects of severe depression. Surgery to the brain (psychosurgery) has a very limited place and then only in the treatment of severe chronic psychiatric illness resistant to other measures.
Classification of commonly used psychotropic drugs
Psychological treatmentsThese treatments are useful in many psychiatric disorders
and also in non-psychiatric conditions. They are based on talking with patients, either individually or in groups. Sometimes discussion is supplemented by ‘homework’ or tasks to complete between treatment sessions. Psychological treatments take a number of forms based on the duration and frequency of contact, the specific techniques applied and their underlying theory.
General or supportive psychotherapy
This should be part of all medical treatment.
It involves empathic listening to the patient’s account of their symptoms and associated fears and concerns, followed by the sympathetic provision of accurate information that addresses these.
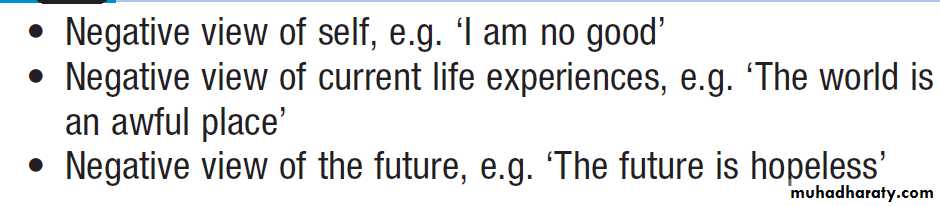
Cognitive therapy
This therapy is based on the observation that some psychiatric disorders are associated with systematic errors in the patient’s conscious thinking: for example, a tendencyto interpret events in a negative way or see them
as unduly threatening. A triad of ‘cognitive errors’ has
been described in depression (Box). Cognitive
therapy aims to help patients to identify such cognitive
errors and to learn how to challenge them. It is widely
used for depression, anxiety and eating and somatoform
disorders, and also increasingly in psychoses.
The negative cognitive triad associated with depression
Behaviour therapyThis is a practically orientated form of treatment, in
which patients are assisted in changing unhelpful
behaviour: for example, helping patients to implement
carefully graded exposure to the feared stimulus in
phobias.
Cognitive behaviour therapy (CBT)
CBT combines the methods of behaviour therapy and cognitive therapy.
It is the most widely available and extensively researched
psychological treatment.
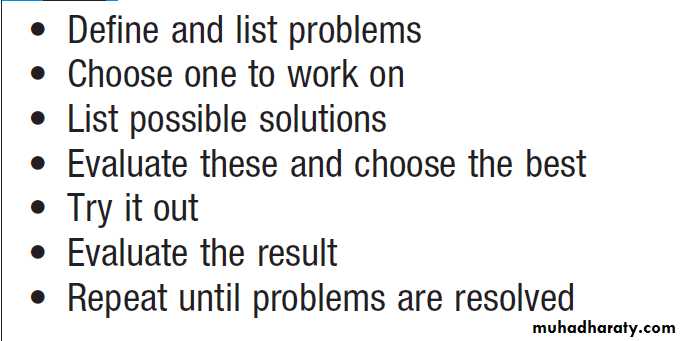
Problem-solving therapy
This is a simplified brief form of CBT, which helpspatients actively tackle problems in a structured way
(Box). It is of benefit in mild to moderate depression,
and can be delivered by non-psychiatric doctors
and nurses after appropriate training.
Psychodynamic psychotherapy
This treatment, also known as ‘interpretive psychotherapy’,
was pioneered by Freud, Jung and Klein,
amongst others. It is based upon the theory that early
life experience generates powerful but unconscious
motivations.
Psychotherapy aims to help the patient to become aware of these unconscious factors on the assumption that, once identified, their negative effects are reduced.
The relationship between therapist and patient is used as a therapeutic tool to identify issues in patients’ relationships with others, particularly parents, which may be replicated or transferred to their relationship with the therapist. Explicit discussion of this relationship (transference) is the basis for the treatment, which traditionally requires frequent sessions over a period of months or even years.
Stages of problem-solving therapy
Interpersonal psychotherapyInterpersonal psychotherapy (IPT) is a specific form of
brief psychotherapy that focuses on patients’ current
interpersonal relationships and is an effective treatment
for mild to moderate depression.
Social interventions
Some adverse social factors, such as unemployment,may not be readily amenable to intervention, but others,
such as access to benefits and poor housing, may be.
Patients can be helped to address these problems themselves by being taught problem-solving.
Befrienders and day centres can reduce social isolation, benefits advisers can ensure appropriate financial assistance, and medical recommendations can be made to local housing departments to help patients obtain more appropriate accommodation.
PSYCHIATRIC DISORDERS
Stress-related disordersAcute stress reaction
Following a stressful event such as a serious medical
diagnosis or a major accident, some people develop
a characteristic pattern of symptoms. These include
a sense of bewilderment, anxiety, anger, depression,
altered activity and withdrawal. The symptoms are transient and usually resolve completely within a few days.
Adjustment disorder
A more common psychological response to a major stressor is a less severe but more prolonged emotional reaction. The predominant symptom is usually depression and/or anxiety, which is insufficiently persistent or intense to merit a diagnosis of depressive or anxiety disorder.
There may also be anger, aggressive behavior and associated excessive alcohol use. Symptoms develop
within a month of the onset of the stress, and their duration and severity reflect the course of the underlying stressor.
Grief reactions following bereavement are a particular
type of adjustment disorder. They manifest as a brief
period of emotional numbing, followed by a period of
distress lasting several weeks, during which sorrow,
tearfulness, sleep disturbance, loss of interest and a
sense of futility are common. Perceptual distortions may
occur, including misinterpreting sounds as the dead person’s
voice. ‘Pathological grief’ describes a grief reaction
that is abnormally intense or persistent.
Management and prognosis
Ongoing contact with and support from a doctor orother who can listen, reassure, explain and advise are
often all that is needed. Most patients do not require
psychotropic medication, although benzodiazepines
reduce arousal in acute stress reactions and can aid
sleep in adjustment disorders.
Psychotherapy may be helpful for patients with abnormal grief reactions.
These conditions usually resolve with time but can develop into depressive or anxiety disorders and require treating as such.
Post-traumatic stress disorder (PTSD)
Is a protracted response to a stressful event of an exceptionally threatening or catastrophic nature. Examples of such events include natural disasters, terrorist activity, serious accidents and witnessing violent deaths.
PTSD may also sometimes occur after distressing medical treatments.
There is usually a delay ranging from a few days to
several months between the traumatic event and the
onset of symptoms.
Typical symptoms are recurrent intrusive memories (flashbacks) of the trauma, as well as sleep disturbance, especially nightmares (usually of the traumatic event) from which the patient awakes in a state of anxiety, symptoms of autonomic arousal, emotional blunting and avoidance of situations that evoke memories of the trauma. Anxiety and depression are often associated and excessive use of alcohol or drugs frequently complicates the clinical picture.
Management and prognosis
Immediate counselling for those who have survived amajor trauma is only likely to benefit those who request
it. The main aims are to provide support, direct advice
and the opportunity for emotional catharsis. In established
PTSD, structured psychological approaches
(CBT, eye movement desensitisation and reprocessing
(EMDR), and stress management) are effective. Antidepressant drugs are moderately effective. The condition runs a fluctuating course, with most patients
recovering within 2 years. In a small proportion, the
symptoms become chronic.
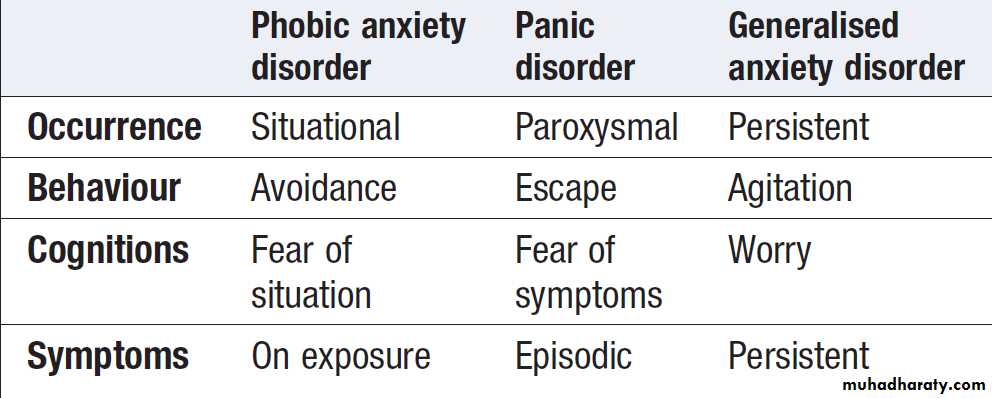
Anxiety disorders
These are characterised by the emotion of anxiety, worrisome thoughts, avoidance behaviour and the somaticsymptoms of autonomic arousal. Anxiety disorders are
divided into three main subtypes: phobic, paroxysmal
(panic) and generalised (Box).
The nature and prominence of the somatic symptoms often lead the patient to present initially to medical services. Anxiety may be stress-related and phobic anxiety may follow an unpleasant incident.
Patients with anxiety often also have depression.
Classification of anxiety disorders
Phobic anxiety disorderA phobia is an abnormal or excessive fear of an object
or situation, which leads to avoidance of it (such as
excessive fear of dying in an air crash leading to avoidance of flying).
A generalised phobia of going out alone or being in crowded places is called agoraphobia.
Phobic responses can develop to medical procedures such as venepuncture.
Panic disorder
Panic disorder describes repeated attacks of severeanxiety, which are not restricted to any particular situation
or circumstances. Somatic symptoms such as chest
pain, palpitations and paraesthesiae in lips and fingers
are common. The symptoms are in part due to involuntary
over-breathing (hyperventilation). Patients with
panic attacks often fear that they are suffering from a
serious illness such as a heart attack or stroke, and seek
emergency medical attention. Panic disorder is often
associated with agoraphobia.
Generalised anxiety disorder
This is a chronic anxiety state associated with uncontrollable worry. The associated somatic symptoms of muscle tension and bowel disturbance often lead to a medical presentation.
Management of anxiety disorders
Psychological treatment
Explanation and reassurance are essential, especially
when patients fear they have a serious medical condition.
Specific treatment may be needed. Treatments
include relaxation, graded exposure (desensitisation) to
feared situations for phobic disorders, and CBT.
Drug treatment
Antidepressants are the drugs of choice.
Benzodiazepines are useful in the short term but long-term use can lead to dependence. A β-blocker such as propranolol can help when somatic symptoms are prominent.
Obsessive-compulsive disorder (OCD)
Is characterised by obsessive thoughts, which are recurrent, unwanted and usually anxiety-provoking, but recognised as one’s own; and by compulsions, which are repeated acts performed to relieve the anxiety. An example is repeated hand-washing related to thoughts of contamination. The differential diagnosis is normal checking behavior and delusional beliefs about thought possession. Unlike other anxiety disorders, which are more common in
women, OCD is equally common in men and women.
Management and prognosis
OCD usually responds to some degree to antidepressantdrugs (SSRIs) and to CBT, which helps patients expose themselves to the feared thought or situation without performing the anxiety-relieving compulsions.
However, relapses are common and the condition often becomes chronic.
Mood disorders
Mood or affective disorders include:
• unipolar depression: one or more episodes of low
mood and associated symptoms
• bipolar disorder: episodes of elevated mood
interspersed with episodes of depression
• dysthymia: chronic low-grade depressed mood
without sufficient other symptoms to count as
‘clinically significant’ or ‘major’ depression.
Depression
Major depressive disorder has a prevalence of 5% in the
general population and approximately 10–20% in chronically ill medical outpatients. It is a major cause of disability and suicide.
If comorbid with a medical condition, depression magnifies disability, diminishes adherence to medical treatment and rehabilitation, and may even shorten life expectancy.
Aetiology
There is a genetic predisposition to depression, especially
when of early onset, number and identity of the genes are largely unknown but the serotonin transporter gene is a candidate. Emotional deprivation early in life also predispose to depression.Depressive episodes are often, but not always, triggered by stressful life events ,medical illnesses. Associated biologicalfactors include hypofunction of monoamine neurotransmitter systems (5-HT and noradrenaline )and abnormal hypothalamo-pituitary-adrenal axis (HPA) results in elevated cortisol levels that do not suppress with dexamethasone.
Diagnosis
Depression may be mild, moderate or severe. It may also be episodic, recurrent or chronic. It can be both a complication of a medical condition and a cause of MUS so physical examination is essential; an associated medical condition should always be considered.Management and prognosis
There is evidence that both drug and psychological
treatments work. Severe depression complicated by psychosis, dehydration or suicide risk may require ECT.
Drug treatment
Antidepressant drugs are effective in patients whose
depression is secondary to medical illness, as well as
those in whom it is the primary problem.
• Tricyclic antidepressants (TCAs). These agents inhibit the re-uptake of the amines noradrenaline and 5-HT at synaptic clefts. The therapeutic effect is noticeable within a week or two.
Side-effects, such as sedation, anticholinergic effects, postural hypotension, lowering of the seizure threshold and cardiotoxicity, can be troublesome during this period. TCAs may be dangerous in overdose and in people who have coexisting heart disease, glaucoma and prostatism.
• Selective serotonin re-uptake inhibitors (SSRIs). These
are less cardiotoxic and less sedative than TCAs,and have fewer anticholinergic effects. They are
safer in overdose, but can still cause headache,
nausea, anorexia and sexual dysfunction. They can
also interact with other drugs increasing serotonin
to produce ‘serotonin syndrome’. This is a rare
syndrome of neuromuscular hyperactivity, autonomic hyperactivity and agitation, and potentially seizures, hyperthermia, confusion and even death.
• Newer antidepressants. including venlafaxine, mirtazapine and duloxetine.They have slightly different modes of action and adverse effects but are generally no more effective than the agents listed above.
• Monoamine oxidase inhibitors (MAOIs). These drugs
increase the availability of neurotransmitters at
synaptic clefts by inhibiting metabolism of noradrenaline and 5-HT. They are now rarely prescribed in the UK, since they can cause potentially dangerous interactions with drugs such as amphetamines, and foods rich in tyramine
such as cheese and red wine. This is due to
accumulation of amines in the systemic circulation,
causing a potentially fatal hypertensive crisis.
These different classes of antidepressant have similar
efficacy and about three-quarters of patients respond totreatment. Successful treatment requires the patient to
take an appropriate dose of an effective drug for an
adequate period. For patients who do not respond, a
proportion will do so if changed to another antidepressant.
The patient’s progress must be monitored and,
after recovery, treatment should be continued for at least
6–12 months to reduce the high risk of relapse. The dose
should then be tapered off over several weeks to avoid
discontinuation symptoms.
Psychological treatments
Both CBT and interpersonal therapy are as effective as
antidepressants for mild to moderate depression. Antidepressant drugs are, however, preferred for severe
depression. Drug and psychological treatments can be
used in combination.
Over 50% of people who have had one depressive
episode and over 90% of people who have had three or
more episodes will have another. The risk of suicide in
an individual who has had a depressive disorder is ten
times greater than in the general population.
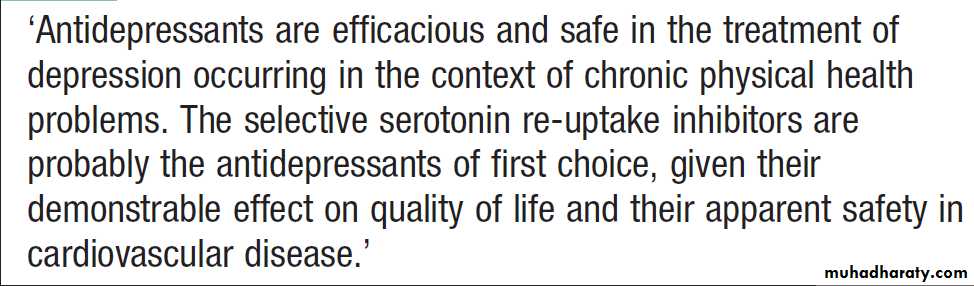
Antidepressants in the medically ill
Antidepressant drugs
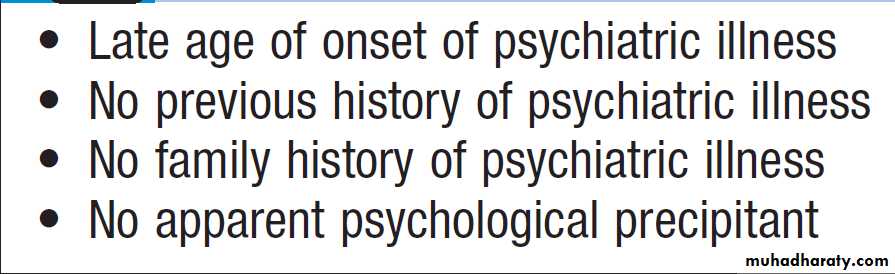
Pointers to an organic cause for psychiatric disorder
Bipolar disorderBipolar disorder is an episodic disturbance with interspersed periods of depressed and elevated mood; the latter is known as hypomania when mild or short-lived, or mania when severe or chronic.The lifetime risk of
developing bipolar disorder is approximately 1–2%.
Onset is usually in the twenties, and men and women are equally affected. In DSM-IV, bipolar disorder has
been divided into two types:
• Bipolar I disorder has a clinical course characterised
by one or more manic episodes or mixed episodes.
Often individuals have also had one or more major
depressive episodes.
• Bipolar II disorder features depressive episodes that
are more frequent and more intense than manicepisodes, but there is a history of at least one
hypomanic episode.
Aetiology
Bipolar disorder is strongly heritable (approximately
70%). Relatives of patients have an increased incidence
of both bipolar and unipolar affective disorder. Life
events, such as physical illness, sleep deprivation and
medication, may play a role in triggering episodes.
Diagnosis
The diagnosis is based on clear evidence of episodes of
depression and mania. Isolated episodes of hypomania
or mania do occur but they are usually preceded or followed by an episode of depression. Psychosis may occur in both the depressive and the manic phases, with delusions and hallucinations that are usually in keeping with
the mood disturbance. This is described as an affective
psychosis. Patients who present with symptoms of both
bipolar disorder and schizophrenia may be given a diagnosis of schizoaffective disorder. A clinical picture of
recurrent depression with one or more episodes of hypomania may be referred to as type 2 bipolar disorder.
Management and prognosis
Depression should be treated as described above.However, if antidepressants are prescribed, they should
be combined with a mood-stabilising drug (see below)
to avoid ‘switching’ the patients into (hypo)mania.
Manic episodes and psychotic symptoms usually
respond well to antipsychotic drugs .
Prophylaxis to prevent recurrent episodes of depression
and mania with mood-stabilising agents is important.
The main drugs used are lithium and sodium valproate. Olanzapine, quetiapine and risperidone are
increasingly used. Caution must be exercised when
stopping these drugs, as a relapse may follow.
• Lithium carbonate is the drug of choice. It is also used for acute mania, and in combination with a tricyclic as an adjuvant treatment for resistant depression. It has a narrow therapeutic range, so regular blood monitoring is required to maintain a serum level of 0.5–1.0 mmol/L. Toxic effects include nausea, vomiting, tremor and convulsions. With long-term treatment, weight gain, hypothyroidism, increased calcium and parathormone, nephrogenic diabetes insipidus and renal failure can occur. Thyroid and renal function should be checked before treatment is started and regularly thereafter. Lithium may be teratogenic, and should not be prescribed during the first trimester of pregnancy.
• Sodium valproate (an anticonvulsant) and olanzapine (an antipsychotic) are both used as prophylaxis in bipolar disorder, usually as a second-line alternative to lithium. Valproate conveys a high risk of birth defects and should also not be used in women of child-bearing age. Olanzapine can cause significant weight gain. (For a list of the adverse effects of antipsychotic drugs, see Box.) The relapse rate of bipolar disorder is high, although patients may be perfectly well between episodes. After one episode the annual average risk of relapse is about 10–15%, which doubles after more than three episodes. There is a substantially increased lifetime risk of suicide of 5–10%.
Somatoform disorders
The essential feature of these disorders is that thesomatic symptoms are not explained by a medical condition (medically unexplained symptoms), nor better diagnosed as part of a depressive or anxiety disorder.
Aetiology
The cause is incompletely understood but contributory factors include depression and anxiety, the erroneous interpretation of somatic symptoms as evidence of disease, excessive concern with physical illness and a tendency to seek medical care. A family history or previous history of a particular condition may have shaped the patient’s beliefs about illness. Doctors may exacerbate the problem, either by dismissing the complaints as non-existent or by overemphasizing the possibility of disease.
Somatisation disorder
Somatisation disorder (Briquet’s syndrome) is characterisedby the occurrence of chronic multiple somatic symptoms for which there is no physical cause. Symptoms
start in early adult life and may be referred to any
part of the body. The disorder is much more common in
women. Common complaints include pain, vomiting,
nausea, headache, dizziness, menstrual irregularities
and sexual dysfunction. Patients may undergo a multitude
of negative investigations and unhelpful operations,
particularly hysterectomy and cholecystectomy.
There is no proven treatment but minimisation of iatrogenic harm from multiple investigations and attempts at medical treatment is important.
Hypochondriacal disorder
Patients with this condition, also known as health
anxiety, have a strong fear or belief that they have a
serious, often fatal, disease and that fear persists despite
appropriate medical reassurance. They are typically
highly anxious and seek many medical opinions and
investigations in futile but repeated attempts to relieve
their fears. Treatment with CBT may be helpful. The
condition may become chronic.
In a small proportion of cases, the conviction that disease is present reaches delusional intensity. The bestknown example is that of parasitic infestation (‘delusional parasitosis’), which leads patients to consult dermatologists. Antipsychotic medication may be effective in such cases.
Body dysmorphic disorder
This describes a preoccupation with bodily shape orappearance, with the belief that one is disfigured in
some way (previously known as dysmorphophobia).
People with this condition may make inappropriate
requests for cosmetic surgery. CBT or antidepressants
may be helpful.
The belief in disfigurement may sometimes be delusional, in which case antipsychotic drugs may help.
Somatoform autonomic dysfunction
This describes somatic symptoms referable to bodilyorgans that are largely under the control of the autonomic
nervous system. The most common examples
involve the cardiovascular system (‘cardiac neurosis’),
respiratory system (psychogenic hyperventilation) and
gut (psychogenic vomiting and irritable bowel syndrome).
Antidepressant drugs and CBT may be helpful.
Somatoform pain disorder
This describes severe, persistent pain that cannot be
adequately explained by a medical condition. Antidepressant drugs (especially tricyclics and dual action
drugs such as duloxetine and mirtazapine) are helpful,
as are some of the anticonvulsant drugs, particularly
carbamazepine, gabapentin and pregabalin.
CBT and multidisciplinary pain management teams are also useful.
Chronic fatigue syndrome
Chronic fatigue syndrome (CFS) is also referred to asneurasthenia. It is characterised by excessive fatigue
after minimal physical or mental exertion, poor concentration, dizziness, muscular aches and sleep disturbance.
This pattern of symptoms may follow a viral infection
such as infectious mononucleosis, influenza or hepatitis.
Symptoms overlap with those of depression and anxiety.
There is good evidence that many patients improve with
carefully graded exercise and with CBT, as long as the
benefits of such treatment are carefully explained.
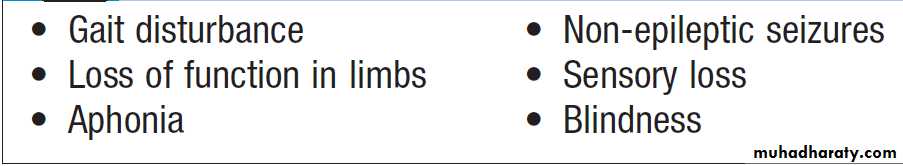
Dissociative (conversion) disorder
Dissociative disorder refers to a loss or distortion ofneurological functioning that is not fully explained by
organic disease. Psychological functions commonly
affected include conscious awareness and memory.
Physical functions affected (conversion) include changes
in sensory or motor function that may mimic lesions in
the motor or sensory nervous system (Box). The
aetiology of dissociation is unknown. There is an association
with adverse childhood experiences, including
physical and sexual abuse.
Organic disease may both facilitate dissociative mechanisms and provide a model for symptoms; thus, for example, non-epileptic seizures often occur in those with epilepsy. CBT may be of benefit.
Coexisting depression should be treated with CBT or antidepressant drugs.
Common presentations of dissociative
(conversion) disorderGeneral management for medically unexplained symptoms
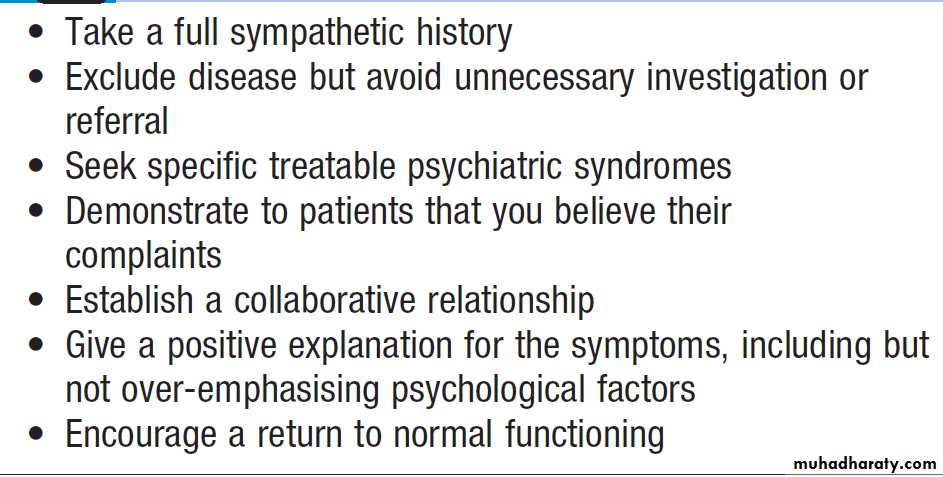
The management of the various syndromes of medicallyunexplained complaints described above is based on
general principles (Box).
Reassurance
Patients should be asked what they are most worried
about. Clearly, it may be unwise to state categorically
that the patient does not have any disease, as that is difficult to establish with certainty.
However, it can be emphasised that the probability of having a disease is low. If patients repeatedly ask for reassurance about the same health concern despite reassurance, they may have hypochondriasis.
General management principles for medically unexplained symptoms
Explanation
Patients need a positive explanation for their symptoms.It is unhelpful to say that symptoms are psychological
or ‘all in the mind’. Rather, a term such as ‘functional’
(meaning that the symptoms represent a reversible disturbance of bodily function) may be more acceptable.
When possible, it is useful to describe a plausible physiological mechanism that is linked to psychological
factors such as stress and implies that the symptoms are
reversible. For example, in irritable bowel syndrome,
psychological stress results in increased activation of the
autonomic nervous system, which leads to constriction
of smooth muscle in the gut wall, which in turn causes
pain and bowel disturbance.
Advice
This should focus on how to overcome factors perpetuatingthe symptoms: for example, by resolving stressful
social problems or by practising relaxation. The doctor
can offer to review progress, to prescribe (for example)
an antidepressant drug and, if appropriate, to refer for
physiotherapy or psychological treatments such as CBT.
The attitudes of relatives may need to be addressed if
they have adopted an over-protective role, unwittingly
reinforcing the patient’s disability.
Drug treatment
Antidepressant drugs are often helpful, even if the
patient is not depressed (Box).
Antidepressants for medically unexplained
somatic symptomsPsychological treatment
There is evidence for the effectiveness of CBT (Box ).Other psychological treatments such as IPT may
also have a role.
Rehabilitation
Where there is chronic disability, particularly in dissociative
(conversion) disorder, conventional physical
rehabilitation may be the best approach.
Shared care with the GP
Ongoing planned care is required for patients with
chronic intractable symptoms, especially those of somatization disorder.
Review by the same specialist, interspersed with visits to the same GP, is probably the best way to avoid unnecessary multiple re-referral for investigation, to ensure that treatable aspects of the patient’s problems, such as depression, are actively managed, and to prevent the GP from becoming demoralised.
CBT for medically unexplained somatic symptoms
Factitious disorder and malingeringIt is important to distinguish somatoform disorders
from factitious disorder and malingering.
Factitious disorder
This describes the repeated and deliberate production
of the signs or symptoms of disease to obtain medical
care. It is uncommon. An example is the dipping of
thermometers into hot drinks to fake a fever.
The disorder feigned is usually medical but can be a psychiatric illness, with false reports of hallucinations or symptoms of depression.
Münchausen’s syndrome
This refers to a severe chronic form of factitious disorder.Patients are usually older and male, with a solitary, peripatetic lifestyle in which they travel widely, sometimes visiting several hospitals in one day.
Although the condition is rare, such patients are memorable
because they present so dramatically. The history
can be convincing enough to persuade doctors to undertake investigations or initiate treatment, including
exploratory surgery. It may be possible to trace the patient’s history and show that he has presented similarly
elsewhere, often changing name several times.
Some emergency departments hold lists of such patients.
Management is by gentle but firm confrontation with
clear evidence of the fabrication of illness, together with
an offer of psychological support. Treatment is usually
declined but recognition of the condition may help to
avoid further iatrogenic harm.
Malingering
Malingering is a description of behaviour, not a psychiatric diagnosis.It refers to the deliberate and conscious
simulation of signs of disease and disability. Patients
have motives that are clear to them but which they
conceal from doctors. Examples include the avoidance
of burdensome responsibilities (such as work or court
appearances) or the pursuit of financial gain (fraudulent
claims for benefits or compensation). Malingering can be
hard to detect at clinical assessment, but is suggested by
evasion or inconsistency in the history.
Schizophrenia
Schizophrenia is a psychosis characterised by delusions,hallucinations and lack of insight. Acute schizophrenia
may present with disturbed behaviour, marked delusions,
hallucinations and disordered thinking, or with
insidious social withdrawal and other so-called negative
symptoms and less obvious delusions and hallucinations.
The prevalence is similar worldwide at about 1% and the disorder is more common in men. The children of one affected parent have approximately a 10% risk of developing the illness, but this rises to 50% if an identical twin is affected. The usual age of onset is the mid-twenties.
Aetiology
There is a strong genetic contribution, probably involving
many susceptibility genes, each of small effect. The
best candidates, such as disrupted in schizophrenia-1
(DISC1) and neuregulin-1 (NRG1), have supportive
linkage, association, animal model and basic neurobiological evidence. Environmental risk factors include obstetric complications and urban birth. Brain imaging techniques have identified subtle structural abnormalities, including an enlargement of the lateral ventricles and an overall decrease in brain size (by about 3% on average), with relatively greater reduction in temporal lobe volume (5–10%).
Episodes of acute schizophrenia may be precipitated by social stress and also by cannabis, which increase dopamine turnover and sensitivity.
Consequently, schizophrenia is now viewed as a neurodevelopmental disorder, caused by abnormalities of
brain development associated with genetic predisposition
and early environmental influences, but precipitated
by later triggers.
Diagnosis
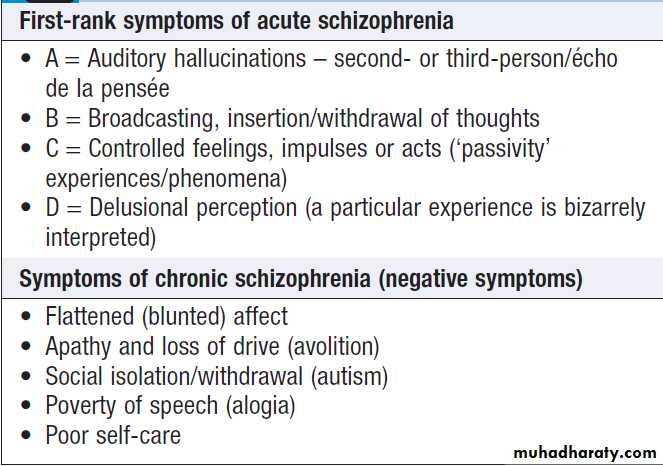
Schizophrenia usually presents with an acute episodeand progresses to a chronic state. Acute schizophrenia
should be suspected in any individual with bizarre
behaviour accompanied by delusions and hallucinations
that are not due to organic brain disease or substance
misuse. The diagnosis is made on clinical grounds, with investigations used principally to rule out organic brain
disease. The characteristic clinical features are listed
in Box. Hallucinations are typically auditory, although they can occur in any sensory modality. They commonly involve voices from outside the head that talk to or about the person.
Sometimes the voices repeat the person’s thoughts.
Patients may also describe ‘passivity of thought’, experienced as disturbances in the normal privacy of thinking – for example, the delusional belief that their thoughts are being ‘withdrawn’ from them, perhaps ‘broadcast’ to others, and/or alien thoughts being ‘inserted’ into their mind. Other characteristic symptoms are delusions of control: believing that one’s emotions, impulses or acts are controlled by others. Another phenomenon is delusional perception, a delusion that arises suddenly alongside a normal perception (e.g. ‘I saw the moon and I immediately knew he was evil’).
Many other, less specific symptoms may occur, including thought disorder, as manifest by incomprehensible speech and abnormalities of movement, such as those in which the patient can become immobile or adopt awkward postures for prolonged periods (catatonia).
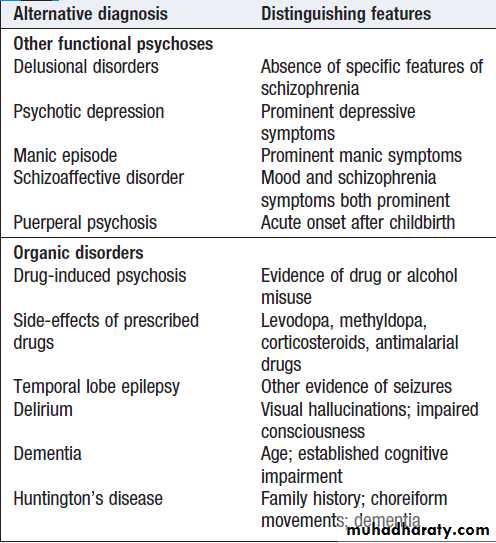
The main differential diagnosis of schizophrenia
(Box) is:
• Other functional psychoses, particularly psychotic depression and mania, in which delusions and hallucinations are congruent with a marked mood disturbance (negative in depression and grandiose in mania). If features of schizophrenia and affective disorder coexist in equal measure, a diagnosis of schizoaffective disorder is made .
Schizophrenia must also be differentiated from specific delusional disorders that are not associated with the other
typical features of schizophrenia.
• Organic psychoses, including delirium, in which
there is impairment of consciousness and loss of
orientation (not found in schizophrenia), typically
with visual hallucinations, and drug misuse, the
latter particularly in young people. Schizophrenia
must also be differentiated from other organic
psychoses such as temporal lobe epilepsy, in which
olfactory and gustatory hallucinations may occur.
Many of those who experience acute schizophrenia
go on to develop a chronic state in which the acute, so-called positive symptoms resolve, or at least donot dominate the clinical picture, leaving so-called
negative symptoms that include blunt affect, apathy,
social isolation, poverty of speech and poor self-care.
Patients with chronic schizophrenia may also manifest
positive symptoms, particularly when under stress, and
it can be difficult for those who do not know the patient
to judge whether or not these are signs of an acute relapse.
Symptoms of schizophrenia
Differential diagnosis of schizophrenia
ManagementFirst-episode schizophrenia usually requires admission
to hospital because patients lack the insight that they are
ill and are unwilling to accept treatment. In some cases,
they may be at risk of harming themselves or others.
Subsequent acute relapses and chronic schizophrenia
are now usually managed in the community.
Drug treatment
Antipsychotic agents are effective against the positive
symptoms of schizophrenia in the majority of cases.
They take 2–4 weeks to be maximally effective but have
some beneficial effects shortly after administration.
Treatment is then ideally continued to prevent relapse.
In a patient with a first episode of schizophrenia, this
will usually be for 1–2 years, but in patients with multiple
episodes, treatment may be required for many years.
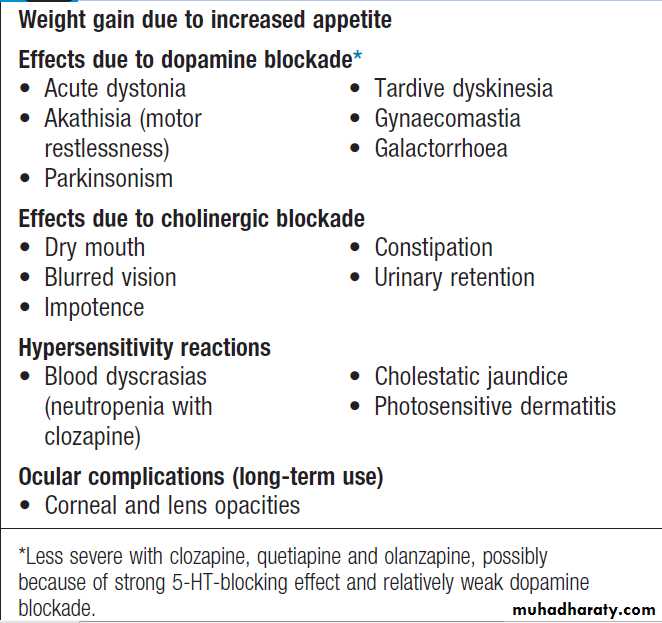
The benefits of prolonged treatment must be weighed
against the adverse effects, which include extrapyramidal
side-effects (EPSE) like acute dystonic reactions (which may require treatment with parenteral anticholinergics), akathisia, Parkinsonism and tardive dyskinesia (abnormal movements, commonly of the face, over which the patient has no voluntary control). For long-term use, antipsychotic agents are often given in slow-release (depot) injected form to improve patient adherence.
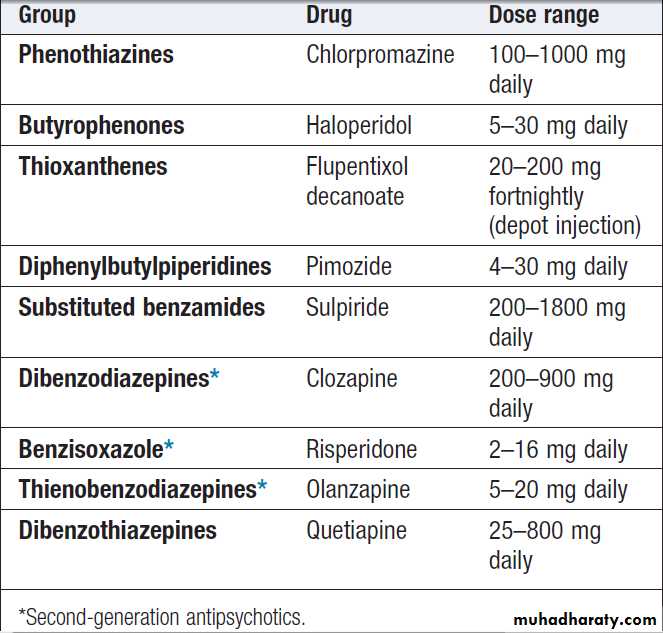
A number of antipsychotic agents are available (Box ).
These may be divided into conventional (typical,first-generation) drugs such as chlorpromazine and
haloperidol, and newer or atypical (also so-called novel
or second-generation) drugs such as clozapine. All are
believed to work by blocking D2 dopamine receptors in
the brain. Patients who have not responded to conventional
drugs may respond to newer agents, which are
also less likely to produce unwanted EPSE but do tend
to cause greater weight gain and metabolic disturbances
such as dyslipidaemia. Clozapine can also cause an
agranulocytosis and consequently requires regular monitoring of the white blood cell count, initially on a weekly basis. Details of the side-effects of antipsychotic drugs are listed in Box.
Serious adverse effects of antipsychotic drugs include:
• Neuroleptic malignant syndrome, which is a rare butserious condition. It is characterised by fever, tremor and rigidity, autonomic instability and confusion. Characteristic laboratory findings are an elevated creatinine phosphokinase and leucocytosis. Antipsychotic medication must be stopped immediately and supportive therapy provided, often in an intensive care unit. Treatment includes
ensuring hydration and reducing hyperthermia. Dantrolene sodium and bromocriptine may be helpful. Mortality is 20% untreated and 5% with treatment.
• Prolongation of the QTc interval, which may be
associated with VT, torsades de pointes and sudden death. Treatment is by stopping the drug, monitoring the ECG
and treating serious arrhythmias
Antipsychotic drugs
Side-effects of antipsychotic drugs
Psychological treatmentIncluding general support for the patient and his or her family, is now seen as an essential component of management. CBT may help patients to cope with symptoms. There is evidence that personal and/or family education, when given as part of an integrated treatment package, reduces the rate of relapse.
Social treatment
After an acute episode of schizophrenia has been controlled by drug therapy, social rehabilitation may be
required. Recurrent illness is likely to cause disruption
to patients’ relationships and their ability to manage
their accommodation and occupation; consequently,
they may need help to obtain housing and employment.
A graded return to employment and sometimes a period
of supported accommodation are required. Patients with chronic schizophrenia have particular difficulties and may need long-term, supervised accommodation.This now tends to be in sheltered or hostel accommodation in the community. Patients may also benefit from sheltered employment if they are unable to participate effectively in the labour market. Ongoing contact with a health worker allows monitoring for signs of relapse, sometimes as part of a multidisciplinary team working to agreed plans (the ‘care programme approach’). Partly because of a tendency to inactivity, smoking and a poor diet, patients with chronic schizophrenia are at increased risk of cardiovascular disease, diabetes and stroke, and require proactive medical as well as psychiatric care.
Prognosis
About one-quarter of those who develop an acute
Schizophrenic episode have a good outcome. One-third
develop chronic, incapacitating schizophrenia, and the
remainder largely recover after each episode but suffer
relapses. Most will not work or live independently. Prophylactic treatment with antipsychotic drugs reduces
the rate of relapse in the first 2 years after an episode of
schizophrenia from 50% to 10%.
Schizophrenia is associated with suicide, with up to 1 in 10 patients taking their own lives.
Delirium, dementia and other organic disorders
Delirium, dementia and other organic disorders couldbe considered to be medical conditions rather than psychiatric disorders, as they are a result of reduced brain
function; they are, however, included in psychiatric classifications and are sometimes misdiagnosed because
they often manifest with disturbed behaviour.
Delirium
Delirium is common in acute medical settings, especially
in the elderly and patients in high-dependency and
intensive care units.
Dementia
Dementia is a clinical syndrome characterised by a lossof previously acquired intellectual function in the
absence of impairment of arousal, and affects 5% of
those over 65 and 20% of those over 85. It is defined as
a global impairment of cognitive function, and is typically
progressive and non-reversible. Although memory
is most affected in the early stages, deficits in visuospatial
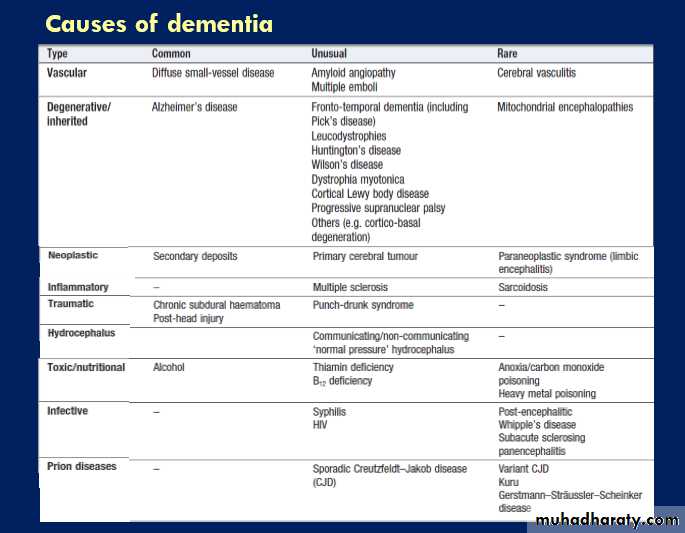
function, language ability, concentration and attention gradually become apparent. There are many causes (Box) but Alzheimer’s disease and diffuse vascular disease are the most common.
Rarer causes of dementia should be actively sought in younger patients and those with short histories.
Aetiology
Dementia may be divided into ‘cortical’ and ‘subcortical’types, depending on the clinical features. Many of the
primary degenerative diseases that cause dementia have
characteristic features that may allow a specific diagnosis
during life. Creutzfeldt–Jakob disease, for example,
is usually relatively rapidly progressive (over months),
is associated with myoclonus, and demonstrates characteristic abnormalities on EEG.
The more slowly progressive dementias are more difficult to distinguish during life, but fronto-temporal dementia typically presents with focal (temporal or frontal lobe) dysfunction, and Lewy body dementia may present with visual hallucinations. The course may also help to distinguish types of dementia, as it may be gradual (as in Alzheimer’s disease) or step-wise (as in vascular dementia).
Clinical features
The usual presentation is with a disturbance of personalityor memory dysfunction. A careful history is essential and it is important to interview both the patient and a close family member. Simple bedside tests such as the MMSE are useful in assessing the nature and severity of the cognitive deficit, although a more intensive neuropsychological assessment may sometimes be required, especially if there is diagnostic uncertainty.
It is important to exclude a focal brain lesion. This is done by determining that there is cognitive disturbance in more than one area. Mental state assessment is important to seek evidence of depression, which may coexist with or occasionally cause apparent cognitive impairment.
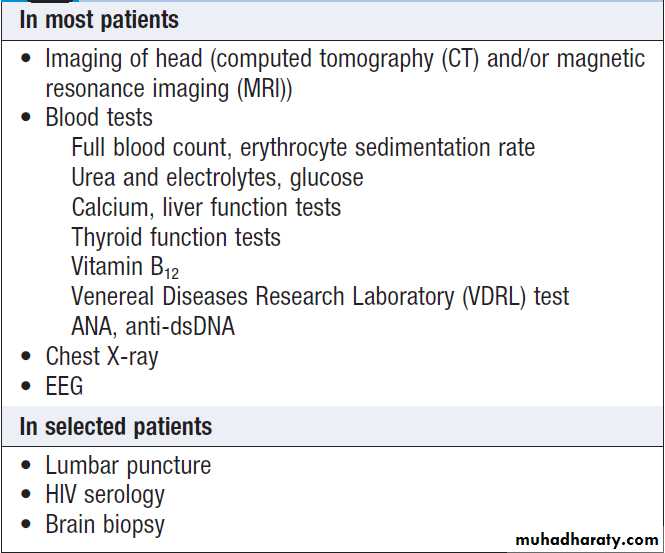
Investigations
The aim is to seek treatable causes and to estimate prognosis.This is done using a standard set of investigations.
Imaging of the brain can exclude potentially
treatable structural lesions, such as hydrocephalus, cerebral
tumour or chronic subdural haematoma, though
the only abnormality usually seen is that of generalised
atrophy. If the initial tests are negative, more invasive
investigations, such as lumbar puncture or, rarely, brain
biopsy, may be indicated.
Initial investigation of dementia
ManagementThis is directed at addressing treatable causes, and providing support for patient and carers if no specific
treatment exists. If the diagnosis is Alzheimer-type
dementia, anticholinesterase inhibitors and memantine
may arrest progression for a time. Treating vascular
risk factors may slow deterioration in vascular dementia.
Psychotropic drugs may help where there is associated
disturbance of sleep, perception or mood, but
should be used with care because of an increased mortality in patients who have been treated long-term with
these agents. Sedation is not a substitute for good care
for patients and carers or, in the later stages, attentive
residential nursing care.
In the UK, incapacity and mental health legislation may be required to manage patients’ financial and domestic affairs, as well as to determine their safe placement.
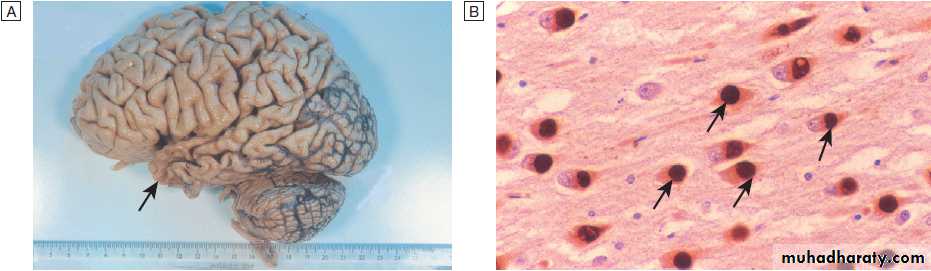
Alzheimer’s disease
Alzheimer’s disease is the most common cause of
dementia, but is rare under the age of 45 years.
Aetiology
Genetic factors play an important role and about 15% of
cases are familial. Familial cases fall into two main
groups: early-onset disease with autosomal dominant
inheritance and a later-onset group whose inheritance
is polygenic.
Mutations in several genes have been described.
The inheritance of one of the alleles of apolipoprotein
ε (apo ε4) is associated with an increased risk of developing the disease (2–4 times higher in heterozygotes and 6–8 times in homozygotes). Its presence is,
however, neither necessary nor sufficient for the development of the disease, so screening for its presence
is not clinically useful. The brain in Alzheimer’s disease
is macroscopically atrophic, particularly the cerebral
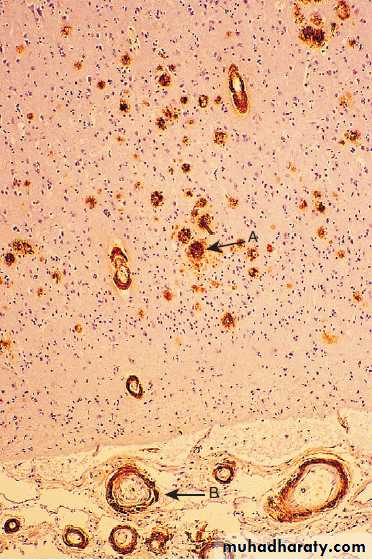
cortex and hippocampus. Histologically, the disease is
characterised by the presence of senile plaques and
neurofibrillary tangles in the cerebral cortex.
Histochemical staining demonstrates significant quantities of
amyloid in the plaques (Fig.), which typically stainpositive for the protein ubiquitin, involved in targeting
unwanted or damaged proteins for degradation. This
has led to the suggestion that the disease may be due
to defects in the ability of neuronal cells to degrade
unwanted proteins. Many different neurotransmitter
abnormalities have also been described. In particular,
there is impairment of cholinergic transmission, although abnormalities of noradrenaline, 5-HT, glutamate and
substance P have also been described.
Alzheimer’s disease. Section of neocortex stained with polyclonal antibody against βA4 peptide showing amyloid deposits in
plaques in brain substance (arrow A) and in blood vessel walls (arrow B).
Clinical features
The key clinical feature is impairment of the ability toremember new information. Hence, patients present
with gradual impairment of memory, usually in association with disorders of other cortical functions.
Short and long-term memory are both affected, but
defects in the former are usually more obvious. Later in
the course of the disease, typical features include apraxia,
visuo-spatial impairment and aphasia. In the early
stages of the disease, patients may notice these problems,
but as the disease progresses it is common for patients to deny that there is anything wrong (anosognosia).
In this situation, patients are often brought to
medical attention by their carers.
Depression is commonly present. Occasionally, patients become aggressive, and the clinical features can be made acutely worse by intercurrent physical disease. Investigations and management
Investigation is aimed at excluding treatable causes
of dementia (see Box), as histological confirmation
of the diagnosis usually occurs only after death. There
is no known treatment, though anticholinesterases such
as donepezil, rivastigmine and galantamine, and the
NMDA receptor antagonist, memantine, have been
shown to be of some benefit. Management consists
largely of providing a familiar environment for the
patient and support for the carers. Many patients
are depressed, and treatment with antidepressant
medication may be helpful.
Fronto-temporal dementia
This term encompasses a number of different syndromes,
including Pick’s diseases and primary progressive
aphasia. Patients may present with personality
change due to frontal lobe involvement or with language
disturbance due to temporal lobe involvement. These
diseases are much rarer than Alzheimer’s disease. Histological examination of the brain reveals argyrophilic
cytoplasmic inclusion bodies of tau (τ) protein rather
than the ubiquitin as in Alzheimer’s disease (Fig.).
Memory is relatively preserved in the early stages. There
is no specific treatment.
Fronto-temporal dementia.
A Lateral view of formalin-fixed brain from a patient who died of Pick’s disease, showing gyral atrophy of frontal and parietal lobes and a more severe degree of atrophy affecting the anterior half of the temporal lobe (arrow).B High power (× 200) of hippocampal pyramidal layer, prepared with monoclonal anti-tau antibody. Many neuronal cell bodies contain sharply circumscribed, spherical cytoplasmic inclusion bodies (Pick bodies).
Lewy body dementia
This is a neurodegenerative disorder clinically characterised by dementia and signs of Parkinson’s disease. The cognitive state often fluctuates and there is ahigh incidence of visual hallucinations. Affected individuals
are particularly sensitive to the side-effects of
anti-Parkinsonian medication and also to antipsychotic
drugs. The condition is associated with accumulation of
abnormal protein aggregates in neurons that contain the
protein α-synuclein in association with other proteins
including ubiquitin .The condition is often inherited and mutations in the α-synuclein and β-synuclein genes have been identified in affected patients. There is no specific treatment but anticholinesterase agents may well be helpful.
Alcohol misuse and dependence
Alcohol consumption associated with social, psychological
and physical problems constitutes misuse. The
criteria for alcohol dependence, a more restricted term,
are shown in Box . Approximately one-quarter of
male patients in general hospital medical wards in the
UK have a current or previous alcohol problem.
Aetiology
Availability of alcohol and social patterns of use appear
to be the most important factors. Genetic factors
predispose to dependence.
The majority of alcoholics do not have an associated psychiatric disorder, but a few drink heavily in an attempt to relieve anxiety or depression.
Criteria for alcohol dependence
DiagnosisAlcohol misuse may emerge during the patient’s history,
although patients may minimise their intake. It may also
present via its effects on one or more aspects of the
patient’s life, listed below. Alcohol dependence commonly
presents with withdrawal in those admitted to
hospital, as they can no longer maintain their high
alcohol intake in this setting.
Complications of chronic alcohol misuse
• Social problems include absenteeism from work,
unemployment, marital tensions, child abuse, financial difficulties and problems with the law, such as violence and traffic offences.
• Depression is common. Alcohol has a direct depressant effect and heavy drinking creates numerous social problems. Attempted and completed suicide are associated with alcohol misuse.
• Anxiety is relieved by alcohol in the short term.
People who are socially anxious may consequently use alcohol in this way and may develop dependence. Conversely, alcohol withdrawal increases anxiety.
• Alcoholic hallucinosis is a rare condition in which
alcoholic individuals experience auditory hallucination in clear consciousness.• Alcohol withdrawal is described in Box . Symptoms usually become maximal about 2–3 days after the last drink and can include seizures (‘rum fits’).
• Delirium tremens is a form of delirium associated
with severe alcohol withdrawal. It has a significant
mortality and morbidity (see Box).
Consequences of chronic alcohol misuse
Effects on the brain
The familiar features of drunkenness are ataxia, slurred
speech, emotional incontinence and aggression. Very
heavy drinkers may experience periods of amnesia for
events that occurred during bouts of intoxication, termed
‘alcoholic blackouts’. Established alcoholism may lead
to alcoholic dementia, a global cognitive impairment
resembling Alzheimer’s disease, but which does not
progress and may even improve if the patient becomes
abstinent. Indirect effects on behaviour can result
from head injury, hypoglycaemia and encephalopathy
A rare but important effect of chronic alcohol misuse
is the Wernicke–Korsakoff syndrome. This organic braindisorder results from damage to the mamillary bodies,
dorsomedial nuclei of the thalamus and adjacent areas
of periventricular grey matter caused by a deficiency of
thiamin (vitamin B1), which most commonly results from long-standing heavy drinking and an inadequate diet. It can also arise from malabsorption or even protracted vomiting. Without prompt treatment (see below), the acute presentation of Wernicke’s encephalopathy (nystagmus, ophthalmoplegia, ataxia and confusion) can progress to the irreversible deficits of Korsakoff’s syndrome (severe short-term memory deficits and confabulation, and also reduced red blood cell transketolase).
In those who die in the acute stage, microscopic
examination of the brain shows hyperaemia,petechial haemorrhages and astrocytic proliferation.
Effects on other organs
These are protean and virtually any organ can be
involved (see Box). These effects are discussed in
detail in the relevant chapters.
Management and prognosis
For the person misusing alcohol, provision of clear information from a doctor about the harmful effects of alcohol and the safe levels of consumption is often all that is needed. In more serious cases, patients may have to be
advised to alter leisure activities or change jobs to help
them to reduce their consumption. Psychological treatment
is used for patients who have recurrent relapses
and is usually available at specialised centres. Support
to stop drinking is also provided by voluntary organisations, such as Alcoholics Anonymous (AA) in the UK.
Alcohol withdrawal syndromes can be prevented,
or treated once established, with benzodiazepines.
Large doses may be required (e.g. diazepam 20 mg
4 times daily), tailed off over a period of 5–7 days as symptoms subside. Prevention of the Wernicke–Korsakoff syndrome requires the immediate use of high
doses of thiamine, which is initially given parenterally
in the form of Pabrinex (two vials 3 times daily for
48 hours) and then orally (100 mg 3 times daily). There
is no treatment for Korsakoff’s syndrome once it has
arisen.
The risk of side-effects, such as respiratory depression with benzodiazepines and anaphylaxis with Pabrinex, is small when weighed against the risks of no treatment. Acamprosate (666 mg 3 times daily) may help to
maintain abstinence by reducing the craving for alcohol.
Disulfiram (200–400 mg daily) can be given as a deterrent to patients who have difficulty resisting the impulse to drink after becoming abstinent. It blocks the metabolism of alcohol, causing acetaldehyde to accumulate. When alcohol is consumed, an unpleasant reaction follows, with headache, flushing and nausea. Disulfiram is always an adjunct to other treatments, especially supportive psychotherapy. Treatment with antidepressants may be required if depression is severe or does not resolve with abstinence. Antipsychotics (e.g. chlorpromazine 100 mg 3 times daily) are needed for alcoholic hallucinosis. Although such treatment may be successful, there is a high relapse rate.
Chronic alcohol misuse greatly increases the risk of
death from accidents, disease and suicide.
Substance misuse disorder
Dependence on and misuse of both illegal and prescribeddrugs is a major problem worldwide. They can be
grouped as follows.
Sedatives
These commonly give rise to physical dependence, the
manifestations of which are tolerance and a withdrawal
syndrome. Drugs include benzodiazepines, opiates (including morphine, heroin,methadone and dihydrocodeine) and barbiturates (now rarely prescribed). Overdosage with opiates and benzodiazepines can be fatal, primarily as a result of respiratory depression . Withdrawal from opiates is notoriously unpleasant, and withdrawal from benzodiazepines and barbiturates may cause seizures.
Intravenous opiate users are prone to bacterial infections,
hepatitis B , hepatitis C and HIV infection through needle contamination.Accidental overdose is common, mainly because of the
varied and uncertain potency of illicit supplies of the
drug. The withdrawal syndrome, which can start within
12 hours of last use, presents with intense craving,
rhinorrhoea, lacrimation, yawning, perspiration, shivering,
piloerection, vomiting, diarrhoea and abdominal cramps. Examination reveals tachycardia, hypertension,
mydriasis and facial flushing.
Benzodiazepine withdrawal symptoms
StimulantsStimulant drugs include amphetamines and cocaine.
They are less dangerous than the sedatives in overdose,
although they can cause cardiac and cerebrovascular
problems through their pressor effects. Physical dependence syndromes do not arise, but withdrawal causes a rebound lowering in mood and can give rise to an intense craving for further use, especially in any form of drug with a rapid onset and offset of effect, such as crack cocaine. Chronic ingestion can cause a paranoid psychosis similar to schizophrenia. A ‘toxic psychosis’ (delirium) can occur with high levels of consumption, and tactile hallucinations (formication) may be prominent.
Hallucinogens
The hallucinogens are a disparate group of drugs thatcause prominent sensory disturbances. They include
cannabis, ecstasy, lysergic acid diethylamide (LSD) and
Psilocybin (magic mushrooms). A toxic confusional state
can occur after heavy cannabis consumption. Acute psychotic episodes are well recognised, especially in those
with a family or personal history of psychosis, and there
is evidence that prolonged heavy use increases the risk
of developing schizophrenia. Paranoid psychoses have
been reported in association with ecstasy. A chronic psychosis has also been reported after regular LSD use.
Organic solvents
Solvent inhalation (glue sniffing) is popular in some
adolescent groups. Solvents produce acute intoxication
characterised by euphoria, excitement, dizziness and a
floating sensation. Further inhalation leads to loss of
consciousness; death can occur from the direct toxic
effect of the solvent, or from asphyxiation if the substance
is inhaled from a plastic bag.
Aetiology
Many of the aetiological factors for alcohol misusealso apply to drug dependence. The main factors are
cultural pressures, particularly within a peer group, and
availability of a drug. In the case of some drugs, medical
over-prescribing (for example, of synthetic opiates) has
increased their availability, but there has also been a
relative decline in the price of illegal drugs. Most drug
users take a range of drugs – so-called polydrug misuse.
Diagnosis
As with alcohol, the diagnosis either may be apparent
from the history, or may only be made once the patient
presents with a complication.
Drug screening of samples of urine or blood can be valuable in confirming the diagnosis, especially if the patient persists in denial.
Management and prognosis
The first step is to determine whether patients wish to
stop using the drug. If they do not, they can still benefit
from advice about how to minimise harm from their
habit: for example, how to obtain and use clean needles
for those who inject. For those who are physically
dependent on sedative drugs, substitute prescribing
(using methadone, for example, in opiate dependence)
may help stabilise their lives sufficiently to allow a gradual reduction in dosage until they reach abstinence.
Some specialist units offer inpatient detoxification. The drug lofexidine, a centrally acting α-agonist, can
be useful in treating the autonomic symptoms of opiate
withdrawal, as can clonidine, although this carries a risk
of hypotension and is best used by specialists. Longacting
opiate antagonists, such as naltrexone, may also
have a place, again in specialist hands, in blocking
the euphoriant effects of the opiate, thereby reducing
addiction.
In some cases, complete opiate withdrawal is not successful
and the patient functions better if maintained on
regular doses of oral methadone as an outpatient. This
decision to prescribe long-term methadone should only
be taken by a specialist, and carried out under long-term
supervision at a specialist drug treatment centre.
Substitute prescribing is neither necessary nor possible
for the hallucinogens and stimulants, but the principles
of management are the same as those that should
accompany prescribing for the sedatives. These include
identifying problems associated with the drug misuse
that may serve to maintain it, and intervening where
possible. Intervention may be directed at physical illness,
psychiatric comorbidity, social problems or family
disharmony.
Relapsing patients and those with complications
should be referred to specialist drug misuse services.
Support can also be provided by self-help groups and
voluntary bodies, such as Narcotics Anonymous in the UK.
Personality disorders (PD)
Personality refers to the set of characteristics and behavioural traits that best describes an individual’s patterns of interaction with the world. The intensity of particular traits varies from person to person, although many, such as shyness or irritability, are displayed to some degree by most people.A PD is diagnosed when an individual’s personality causes persistent and severe problems for the person or for others. For example, anxiety may be so pronounced that the individual rarely ventures into any situation where he or she fears scrutiny.
Antisocial traits, such as disregard for the well-being
of others and a lack of guilt concerning the adverseeffects of one’s actions on others, if pronounced, may
lead to damage to others and to criminal acts. PD is classified into several subtypes (such as emotionally
unstable, antisocial or schizotypal), depending on the particular behavioural traits in question. A patient
who meets diagnostic criteria for one subtype commonly
meets criteria for two or three others. As allocation
to one particular subtype gives little guidance to
management or prognosis, classification is of limited
value. PD commonly accompanies other psychiatric conditions, making treatment of the latter more difficult and
therefore affecting their prognosis.
Aetiology
Some personality disorders appear to have an inherited
aspect (especially paranoid and schizotypal types) but
most are more clearly related to an unsatisfactory
upbringing and adverse childhood experiences.
Management and prognosis
Personality disorders usually persist throughout life and
are not readily treated. However, they often become less
extreme with age. Treatment options are limited but
there is some evidence that emotionally unstable PD
may also respond to dialectical behavioural therapy (an
intensive type of CBT). Anxious (avoidant) and obsessional
(anankastic) PD may benefit from prescription of
anxiolytic, while paranoid/schizotypal PD may benefit from treatment with low doses of antipsychotic agents.
Eating disorders
There are two well-defined eating disorders, anorexianervosa (AN) and bulimia nervosa (BN); they share
some overlapping features. Ninety per cent of cases are
female. There is a much higher prevalence of abnormal
eating behaviour in the population that does not meet
diagnostic criteria for AN or BN.
In developed societies, obesity is arguably a much greater problem but is usually considered to be a disorder of lifestyle or physiology than a psychiatric disorder.
Anorexia nervosa
There is marked weight loss, arising from food avoidance,
often in combination with bingeing, purging,
excessive exercise, or the use of diuretics and laxatives.
Body image is profoundly disturbed so that, despite
emaciation, patients still feel overweight and are terrified of weight gain. These preoccupations are intense
and pervasive, and the false beliefs may be held with a
conviction approaching the delusional. Anxiety and
depressive symptoms are common accompaniments.
Downy hair (lanugo) may develop on the back, forearms
and cheeks. Extreme starvation is associated with a
wide range of physiological and pathological bodily
changes. All organ systems may be affected, although
the most serious problems are cardiac and skeletal.
Medical consequences of eating disorders
AetiologyThis is unknown but probably includes genetic and
environmental factors, including, in many societies, the
social pressure on women to be thin.
Diagnosis
The condition usually emerges in adolescence, with a
marked female preponderance. Diagnostic criteria are
shown in Box . Differential diagnosis is from other
causes of weight loss, including psychiatric disorders
such as depression, and medical conditions such as
inflammatory bowel disease, malabsorption, hypopituitarism and cancer. The diagnosis is based on a pronounced fear of fatness despite being thin, and on the
absence of alternative causes of weight loss.
Diagnostic criteria for eating disorders
Management and prognosisThe aims of management are to ensure patient’s physical
well-being, whilst helping them to gain weight by
addressing the beliefs and behaviours that maintain the low weight. Treatment is usually given on an outpatient
basis, inpatient treatment being indicated only if weight
loss is intractable and severe (for example, less than 65%
of normal), or if there is a risk of death from medical
complications or from suicide. There is a limited evidence
base for treatment, although CBT and family
therapy are commonly used. Psychotropic drugs are of
little benefit except in those with clear-cut comorbid
depressive disorder.
Weight gain is best achieved in a collaborative
fashion. Compulsory admission and refeeding (includingtube feeding) are very occasionally resorted to
when patients are at risk of death and other measures
have failed. Whilst this may produce a short-term
improvement in weight, it probably does not change
long-term prognosis. About 20% of patients with AN
have a good outcome, a further 20% develop a chronic
intractable disorder and the rest have an intermediate
outcome.
There is a long-term mortality rate of 10–20%, either due to the complications of starvation or from suicide.
Bulimia nervosa
In BN, patients are usually at or near normal weight
(unlike in AN), but display a morbid fear of fatness
associated with disordered eating behaviour. They
recurrently embark on eating binges, often followed by
corrective measures such as self-induced vomiting. The
prevalence is similar to or slightly greater than that of
AN, but only a small proportion of sufferers reach treatment services.
Diagnosis
BN usually begins later in adolescence than AN, and is
even more predominantly a female malady.
Diagnostic criteria are shown in Box.
Physical signs of repeated self-induced vomiting include pitted teeth (from gastric acid), calluses on knuckles (‘Russell’s sign’) and parotid gland enlargement. There are many associated physical complications, including the dental and oesophageal consequences of repeated vomiting, as well as electrolyte abnormalities, cardiac arrhythmias and renal problems .
Management and prognosis
CBT achieves both short-term and long-term improvements.Guided self-help and interpersonal psychotherapy
may also be of value. There is also evidence for
benefit from the SSRI, fluoxetine, although high doses
(60 mg daily) and long courses (1 year) may be required;
this appears to be independent of the antidepressant
effect.
Bulimia does not carry the mortality associated with
AN, and few sufferers develop anorexia.
At 10-year follow-up, approximately 10% are still unwell, 20% have a subclinical degree of BN, and the remainder have recovered.
Puerperal disorders
There are three common psychiatric disorders that occur
after childbirth. When managing these conditions, it is
important always to consider both the mother and the
baby, and their relationship (Box).
Post-partum blues
These are characterised by irritability, labile mood and
tearfulness. Most women are affected to some degree.
Symptoms begin soon after childbirth, peak on about the
fourth day and then resolve.
They may be related to hormonal or psychological changes associated with childbirth. No treatment is required, other than to reassure the mother.
Psychiatric illness and pregnancy
Post-partum depressionThis occurs in 10–15% of women and within a month of
delivery. Women with a previous history of depression
are at risk. Explanation and reassurance are important.
The usual psychological and drug treatments for depression
should be considered, as well as practical help with
childcare. If hospital admission is required, it should
ideally be to a mother and baby unit. Further episodes
of depression, both after childbirth and in response to
other stressors, are likely.
Puerperal psychosis
This has its onset in the first 2 weeks after childbirth.
It is a rare but serious complication affecting about 1 in
500 women and usually takes the form of a manic or
depressive psychosis. There is an association with a personal or familial history of bipolar disorder. Delirium is
rare with modern obstetric management but should still
be considered in the differential diagnosis. Admission to a psychiatric mother and baby unit may be required.
Management depends on the type of psychosis present. In addition, it is important to consider the welfare of the baby, especially if the mother has ideas of harming it. If so, the risk to the baby must be assessed and, if necessary, the baby temporarily removed. Most women recover but are at an increased (25%) risk of puerperal psychosis with the next pregnancy.
PSYCHIATRY AND THE LAW
Medicine takes place in a legal framework, made up oflegislation (statute law) drafted by parliament or other
governing bodies, and common law (case law) built up
from court judgements over time. Psychiatry is similar
to other branches of medicine in the applicability of
common law but differs in that patients with psychiatric
disorders can also be subject to legislative requirements
to remain in hospital or to undergo treatments they
refuse, such as the administration of antipsychotic drugs
to a patient with acute schizophrenia who lacks insight, and whose symptoms and/or behaviour pose a risk to
himself/herself or to others.
The UK has three different Mental Health Acts,
covering England and Wales, Scotland, and Northern
Ireland, and all of these have recently been revised.
Other countries may have very different provisions.
It is important for practitioners to be familiar with the
relevant provisions that apply in their jurisdictions
and are likely to arise in the clinical settings in which
they work.
All the countries that make up the UK have also introduced
Incapacity Acts in recent years, with detailed
provisions covering medical treatments for patients
incapable of consenting, whether this incapacity arises
from physical or mental illness.
In general, the guiding principle in British law is that people should be free to make their own decisions about medical treatment, except where their ability to decide is impaired by mental illness or physical incapacity, and where there
are clear risks to the health and safety of themselves or
others. Any restrictions or compulsions applied should
be the minimum necessary, and they should only be
applied for as long as is necessary; there should also be
provisions for appeals and oversight.