Hussien Mohammed Jumaah
CABMLecturer in internal medicine
Mosul College of Medicine
2016
learning-topics
Palliative care and painPRINCIPLES OF PALLIATIVE CARE
Palliative care is the active total care of patients withfar advanced, rapidly progressive and ultimately fatal
disease. Its focus is quality of life rather than cure, and
it encompasses a distinct body of knowledge and skills
that all good physicians must possess to allow them to
care effectively for patients at the end of life. In palliative
care, there is a fundamental change of emphasis in
decision-making away from a focus on prolonging life
towards decisions that balance comfort and the individual’s
wishes with treatments that might prolong life.
There is a growing recognition that the principles of, and
some specific interventions developed in the palliative
care of patients with cancer are equally applicable to
other conditions. The principles of palliative care may
therefore be applied not only to cancer but also to any
chronic disease state.
Palliative care is often seen as a means of managing
distress and symptoms in patients with cancer, where
metastatic disease has been diagnosed and death is seen
as inevitable. In other illnesses, the challenge is recognising
when patients have entered this phase of their illness, as there are fewer clear markers and the course of the illness is much more variable.
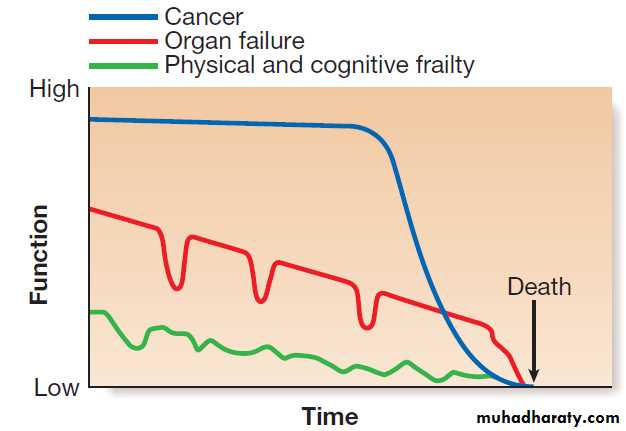
Traditionally, palliative care has been associated with
cancer because the latter is typified by a progressivedecline in function which was more predictable than
in many other diseases. This ‘rapid decline’ trajectory
is the best-recognised pattern need for palliative care and many traditional hospice services are designed to meet the needs of people on this trajectory: for example, motor neuron disease, or AIDS where ART is not available. Many chronic diseases, such as advanced COPD and intractable congestive heart failure, carry as high a burden of symptoms as cancer, as well as psychological and family distress. The ‘palliative phase’ of these illnesses may be more difficult to identify because of periods of relative stability interspersed with acute episodes of severe illness.
The challenge is that symptom management needs to be delivered at the same time as treatment for acute exacerbations. This leads to difficult decisions as to the balance between symptom relief and aggressive
management of the disease. The starting point of need for care is the point at which consideration of comfort and individual values becomes important in decision-making, often alongside management of the underlying disease. The main challenge lies in providing nursing care and ensuring that plans are agreed for the time when medical intervention is no longer beneficial. In a situation where death is inevitable and foreseeable, palliative care balances the ‘standard textbook’ approach with the wishes and values of the patient and a realistic assessment of the benefits of medical interventions.
This often results in a greater focus on comfort, symptom control and support for patient and family, and may enable withdrawal of interventions that are ineffective or burdensome.
Commonly, the outcome is less certain. In many cases, there is a substantial risk that the patient will die but there may be a small chance of improvement with further treatment. In these circumstances, it is often (but not always) correct and helpful to share this information with the patient so that better decisions can be made about further care.
The principles of palliative care are being used
increasingly in many different diseases so that death can
be managed effectively and compassionately.
Archetypal trajectories of dying.
PRESENTING PROBLEMS IN PALLIATIVE CAREPain
The International Association for the Study of Pain
(IASP) has defined pain as ‘an unpleasant sensory and
emotional experience associated with actual or potential
tissue damage or described in terms of such damage’. It
follows that each patient’s experience and expression of
pain are different, and that severity of pain does not
correlate with the degree of tissue damage. Effective
pain treatment facilitates recovery from injury or surgery, aids rapid recovery of function, and may minimize chronic pain and disability. Unfortunately, the delivery of effective pain relief is often impeded by factors such as poor assessment and concerns about the use of opioid analgesia.
Pain classification and mechanisms
Pain can be classified into two types:
• Nociceptive: due to direct stimulation of peripheral
nerve endings by a noxious stimulus such as
trauma, burns or ischaemia.
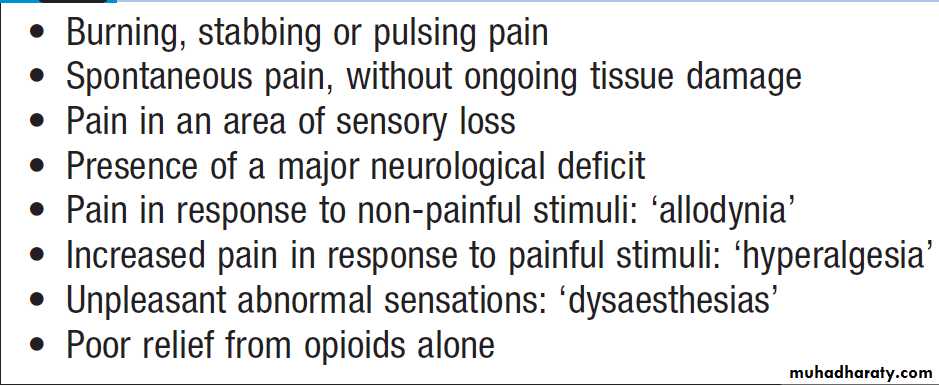
• Neuropathic: due to dysfunction of the pain
perception system within the peripheral or central
nervous system as a result of injury, disease or
surgical damage, such as continuing pain
experienced from a limb which has been amputated
(phantom limb pain). This should be identified early because it is more difficult to treat once established.
The pain perception system is not a simple hard-wired circuit of nerves connecting tissue pain receptors to the brain, but a dynamic system in which a continuing pain stimulus can cause central changes that lead to an increase in pain perception.
This plasticity (changeability) applies to all the peripheral and central components of the pain pathway.
Early and appropriate treatment of pain reduces the potential for chronic undesirable changes to develop.
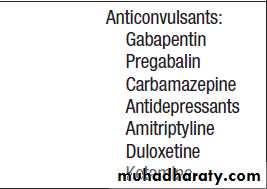
Features of neuropathic pain
Assessment and measurement of pain
Accurate assessment of the patient is the first step in
providing good analgesia.
History and measurement of pain
A full pain history should be taken, to establish its
causes and the underlying diagnoses. Patients may have
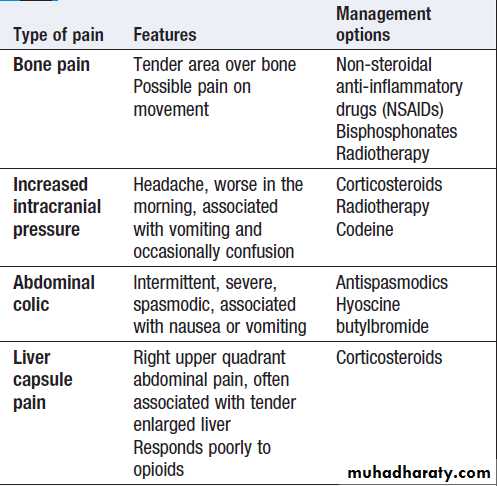
more than one pain; for example, bone and neuropathic
pain may both arise from skeletal metastases .
A diagram of the body on which the patient can mark
the pain site can be helpful.
When asked to score pain, patients consistently rate it higher than health professionals and should, if able, always be asked to rate pain themselves.
Methods include:
• Verbal rating scale. Different verbal descriptions are
used to rate pain – ’no pain’, ‘mild pain’, ‘moderate
pain’ and ‘severe pain’.
• Visual analogue scale. A question is used, such as
‘Over the past 24 hours, how would you rate your
pain, if 0 is no pain and 10 is the worst pain you
could imagine?’
• Behavioural rating scale. It can be particularly difficult
to decide whether a patient with cognitive
impairment is suffering pain.
A variety of measures are available which use observed behaviours, such as agitation and withdrawn posture, to assess levels of pain. Commonly used scales include Abbey and Dolorplus. Changes in behavioural rating pain
scores can indicate whether drug measures have
been successful.
Regular recording of formal pain assessment and
patient-rated pain scores improves pain management
and reduces the time taken to achieve pain control.
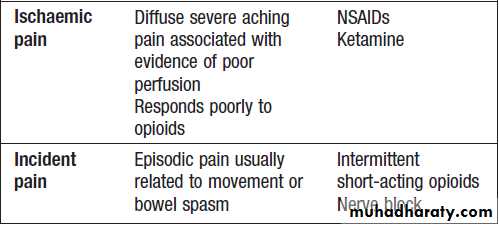
Types of pain
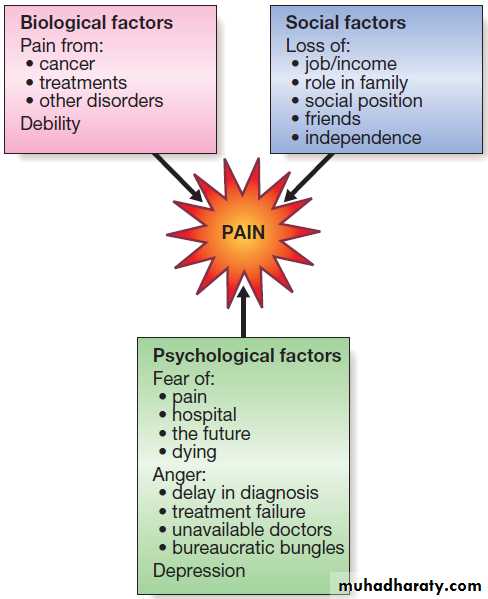
Psychological aspects of chronic painPerception of pain is influenced by many factors other
than the painful stimulus, and pain cannot therefore be
easily classified as wholly physical or psychogenic in
any individual . Patients who suffer chronic pain will be affected emotionally and, conversely, emotional distress can exacerbate physical pain .
Full assessment for symptoms of anxiety and depression is
essential to effective pain management.
Examination
This should include careful assessment of the painful
area, looking for signs of neuropathic pain or bony tenderness suggestive of bone metastases. In patients with cancer, it should not be assumed that all pains are due to the cancer or its metastases.
Components of pain.
Appropriate investigationsInvestigations should be directed towards diagnosis of
an underlying cause, remembering that treatable conditions
are possible even in patients with advanced
disease. Imaging may be indicated, such as plain X-ray
for fracture or magnetic resonance imaging (MRI) for
spinal cord compression.
Management of pain
Many of the principles of pain management apply to anypainful condition. There are, however, distinct differences
between management of acute, chronic and palliative
pain. Acute pain post-surgery or following trauma should be controlled with medication without causing unnecessary side-effects or risk to the patient. Chronic, non-malignant pain is more difficult and it may be impossible to relieve completely. In the management of chronic pain there is a greater emphasis on non-pharmacological treatments and on enabling the patient to live with pain. Strong opioids may help chronic pain but need to be used with caution after full assessment. They are used more readily in patients with a poorer prognosis.
Two-thirds of patients with cancer experience moderate
or severe pain, and a quarter will have three or moredifferent pains. Many of these are of mixed aetiology
and 50% of pain from cancer has a neuropathic element.
Careful evaluation to identify the likely pain mechanism
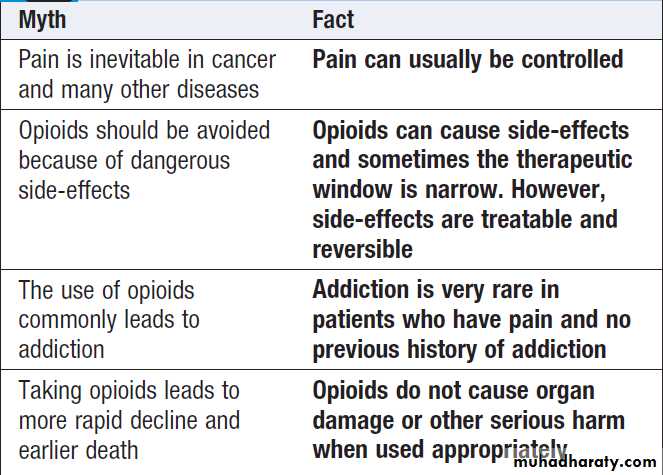
facilitates appropriate treatment . It is vital that the patient’s concerns about opioids are explored.
Patients should be reassured that, when they are used
for pain, psychological dependence and tolerance are
extremely rare.
Nearly all types of pain respond to morphine to
some degree. Some are completely opioid-responsive
but others, such as neuropathic and ischaemic pain, are
relatively unresponsive. Opioid-unresponsive or poorly
responsive pain will only be relieved by opioids at a
dose which causes significant side-effects. In these situations, effective pain relief may only be achieved with the use of adjuvant analgesics (see below).
Opioid myths
Pharmacological treatmentsNon-opioids
• Paracetamol. This is often effective for mild to
moderate pain. For severe pain, it is inadequate
alone, but is a useful and well-tolerated adjunct.
• NSAIDs. These are effective in the treatment of mild
to moderate pain, and are also useful adjuncts in
the treatment of severe pain. Adverse effects may
be serious, especially in the elderly .
Weak opioids
Codeine and dihydrocodeine are weak opioids. They
have lower analgesic efficacy than strong opioids and a ceiling dose. They are effective for mild to moderate pain.
Strong opioids
Immediate-release (IR) oral morphine takes about
20 minutes to have an effect and usually provides pain
relief for 4 hours. Most patients with continuous pain
should be prescribed IR oral morphine every 4 hours
initially, as this will provide continuous pain relief over
the whole 24-hour period.
Controlled-release (CR) morphine lasts for 12 or 24 hours but takes longer to provide analgesia.
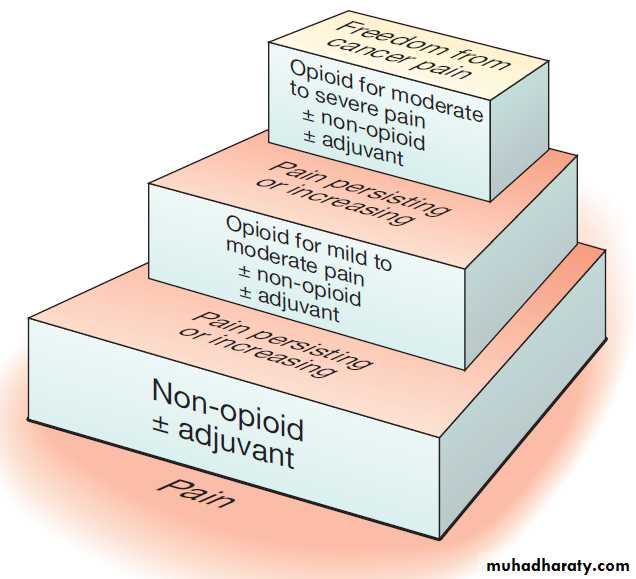
The WHO analgesic ladder
The basic principle of the WHO ladder is that analgesia which is appropriate for the degree of pain should be prescribed. If pain is severe or remains poorlycontrolled, strong opioids should be prescribed and
increased as indicated by the patient’s need for additional
analgesia (opioid titration).
A patient with mild pain is started on a non-opioid
analgesic drug, such as paracetamol 1 g 4 times daily
(step 1).
If the maximum recommended dose is not sufficient or the patient has moderate pain, a weak opioid, such as codeine 60 mg 4 times daily, should be added (step 2).
If adequate pain relief is still not achieved with the maximum recommended dosages or if the patient has severe pain, a strong opioid is substituted for the weak opioid (step 3). It is important not to move ‘sideways’ (change from one drug to another of equal potency) on a particular step of the ladder.
All patients with severe pain should receive a full trial of
strong opioids with appropriate adjuvant analgesia, as
described below.
In addition to the regular dose, an extra dose of IR
morphine should be prescribed ‘as required’ for when
the patient has pain that is not controlled by the regular
prescription (breakthrough pain).
This should be one-sixth of the total 24-hour dose of opiate. The frequency of breakthrough doses should be dictated by their efficacy and any side-effects, rather than by a fixed time interval. A patient may require breakthrough analgesia as frequently as hourly if pain is severe, but this should lead to early review of the regular prescription. The patient and/or carer should note the timing of any breakthrough doses and the reason for them. These should be reviewed daily and the regular 4-hourly dose increased for the next 24 hours on the basis of:
• frequency of and reasons for breakthrough
analgesia
• degree and acceptability of side-effects.
The regular dose should be increased by adding the
total of the breakthrough doses over the previous24 hours, unless there are significant problems with
unacceptable side-effects. When the correct dose has
been established, a CR preparation can be prescribed,
usually twice daily.
Worldwide, the most effective and appropriate route
of administration is oral, though transdermal preparations
of strong opioids (usually fentanyl) are useful in
certain situations, such as in patients with dysphagia or
those who are reluctant to take tablets on a regular basis.
Diamorphine is a highly soluble strong opioid used for
subcutaneous infusions, particularly in the last few days
of life, but is only available in certain countries.
The WHO analgesic ladder.
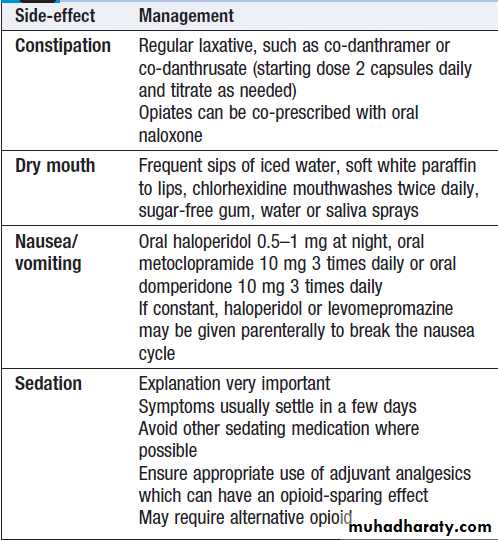
Common side-effects of opioids are shown in Box .Nausea and vomiting occur initially but usually settle after a few days. Confusion and drowsiness are dose-related and reversible. In acute dosing, respiratory depression can occur but this is rare in those on regular opioids.
Opioid toxicity
All patients will develop dose-related side-effects, such
as nausea, drowsiness, confusion or myoclonus; this is
termed opiate toxicity. The dose at which this occurs
varies from 10 to 5000 mg of morphine, depending on
the patient and the type of pain. When opiates are being
titrated, side-effects should be assessed regularly. The
earliest side-effects are often visual hallucinations (often
a sense of movement at the periphery of vision) and a
distinct myoclonic movement.
Pain should be re-assessed to ensure that appropriate adjuvants are being used.
Parenteral rehydration is often helpful to speed upexcretion of active metabolites of morphine. The dose of
opioid may need to be reduced or changed to an alternative strong opiate.
Different opioids have different side-effect profiles
in different people. If a patient develops side-effects,
switching to an alternative strong opioid may be helpful.
Options include oxycodone, transdermal fentanyl,
alfentanil, hydromorphone and occasionally methadone,
any of which may produce a better balance of
benefit against side-effects.
Fentanyl and alfentanil have no renally excreted active metabolites and may be particularly useful in patients with renal failure.
Pethidine is used in acute pain management but not
for chronic or cancer pain because of its short half-life
and ceiling dose.
It is important to be very careful when switching
opiates, as it is easy to make calculation mistakes and
prescribe too much or too little.
Opioid side-effects
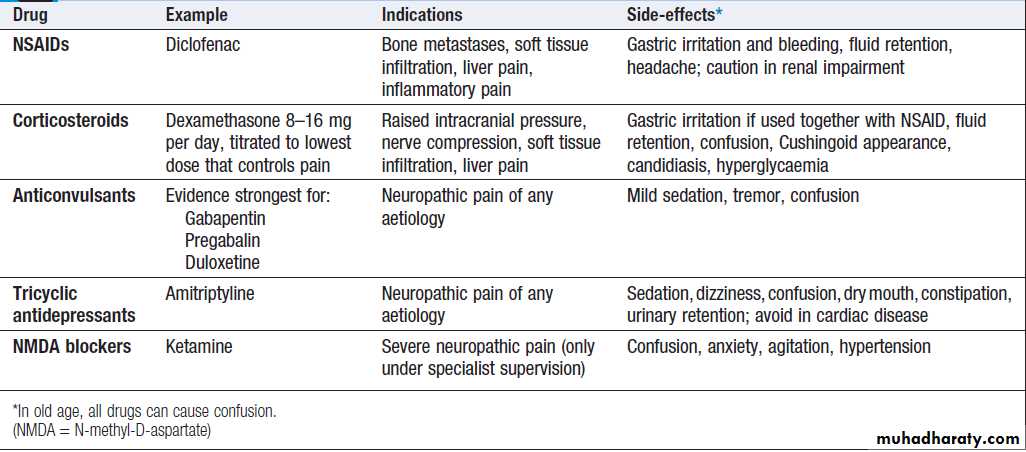
Adjuvant analgesicsAn adjuvant analgesic is a drug with a primary indication
other than pain but which provides analgesia in
some painful conditions and may enhance the effect of
the primary analgesic. At each step of the WHO analgesic
ladder, an adjuvant analgesic should be considered,
the choice depending on the type of pain
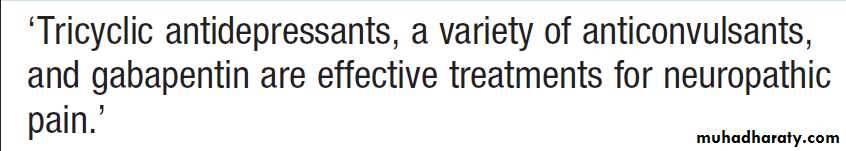
Treatment of neuropathic pain
Adjuvant analgesics
Non-pharmacological and complementary treatmentsRadiotherapy
Radiotherapy can improve pain from bone metastases
and may be considered for cancer in other sites .
Physiotherapy
This helps to alleviate pain and restore function, through
active mobilisation and specific physiotherapy techniques, such as spinal manipulation, massage, application of heat or cold, and exercise. Immediate application of cold with ice packs can reduce subsequent swelling and inflammation after a direct injury.
Psychological techniques
These include simple relaxation, hypnosis, cognitivebehavioural therapies and biofeedback ,
which train the patient to use coping strategies and
behavioural techniques. This is often more relevant in
chronic non-malignant pain than in cancer pain.
Stimulation therapies
Acupuncture has been used successfully in Eastern medicine for centuries. It causes release of endogenous analgesics (endorphins) within the spinal cord. It can be particularly effective in pain related to muscle spasm. Transcutaneous electrical nerve stimulation (TENS) may have a similar mechanism of action to acupuncture and can be used in both acute and chronic pain.
Acupuncture.
Herbal medicine and homeopathyThese are widely used for pain, but often with little
evidence for efficacy . Safety regulations for these
treatments are limited, compared with conventional
drugs, and the doctor should be wary of unrecognised
side-effects which may result.
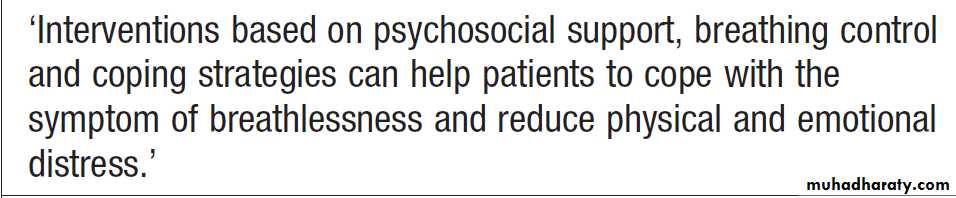
Breathlessness
The sensation of breathlessness is the result of a complex interaction between different factors at the levels of production (the pathophysiological cause), perception(the severity of breathlessness perceived by the patient)
and expression (the symptoms expressed by an individual
patient). A patient’s perception and expression of
breathlessness can be significantly improved, even if
there is no reversible ‘cause’ . Assessment and treatment should therefore be targeted at modifying these factors, particularly when there is no reversible pathophysiology.
Clearly reversible causes of breathlessness should be identified and managed, but investigation and
treatment should be appropriate to the prognosis and
stage of disease. A therapeutic trial of corticosteroids
(dexamethasone 8 mg for 5 days) and/or nebulised salbutamol may be helpful.
Breathlessness may be worsened by specific anxieties
and beliefs; these should be explored. Many people with
heart failure are concerned that exertional breathlessness
will lead to worsening of their heart condition. Patients with advanced disease have specific panic– breathlessness cycles in which breathlessness leads to panic, which leads to worsening breathlessness and worsening panic.
These should be identified and explained to the patient. Many fear that they will die during one of these episodes, and explanation of the panic cycle can be very reassuring. Another frequently expressed fear is that breathlessness will continue to worsen until it is continuous and unbearable, leading to a distressing and undignified death. Reassurance should again be given that this is uncommon and can be effectively managed with opioids and benzodiazepines.
A rapidly acting benzodiazepine, such as sublingual
lorazepam, or non-drug measures, such as relaxation
techniques, may help panic–breathlessness cycles.
Attention to energy conservation (thinking clearly about
using limited energy reserves sensibly) and pacing ofactivity is also extremely helpful. Physiotherapists are
good at this and should be involved in developing an
individual plan for each patient.
Perception of breathlessness may also be improved
by night-time or regular morphine, or by regular
benzodiazepines.
Oxygen does not help breathlessness unless the patient is hypoxic. An electric fan, piped air or an open window can be as effective as oxygen in patients who are breathless but not hypoxic. The patient’s, family’s or even professional beliefs about the benefits and need for oxygen may be the main reason for its apparent efficacy in non-hypoxic patients who feel less breathless when using oxygen.
Palliative treatment of breathlessness
CoughCough can be a troubling symptom in cancer and other
illnesses such as motor neuron disease, cardiac failure
and COPD. There are many possible causes .
Management should focus on treating the underlying
condition if possible. If this fails to bring about the
desired response, antitussives, such as codeine linctus,
are sometimes effective, particularly for cough at night.
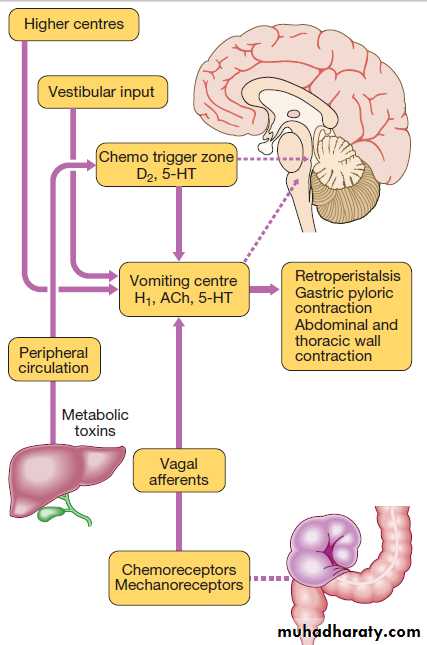
Nausea and vomiting
The presentation of nausea and vomiting differs,
depending on the underlying cause, of which there are
many .Large-volume vomiting with little nausea
is common in intestinal obstruction, whereas constant
nausea with little or no vomiting is often due to metabolic
abnormalities or drugs. Vomiting related to raised
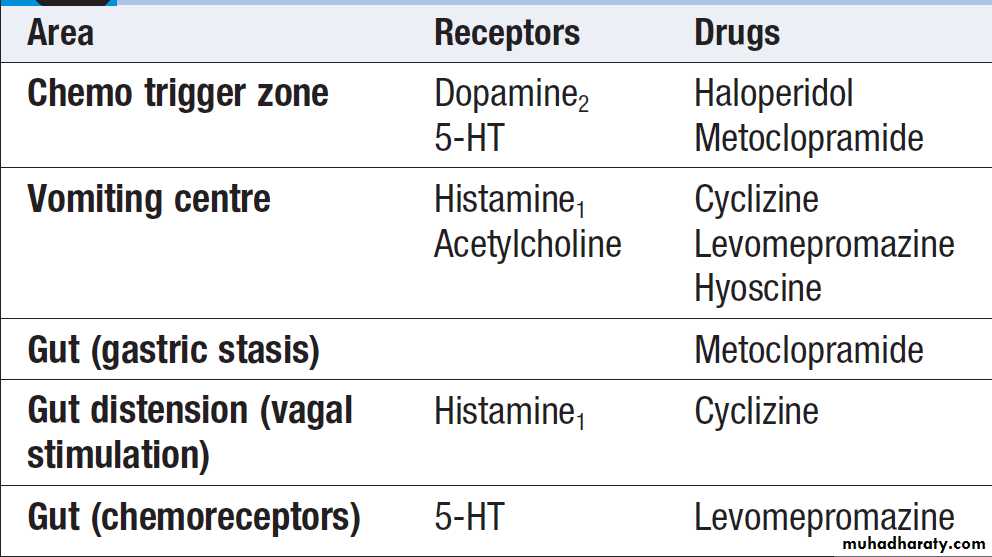
intracranial pressure is worse in the morning. Different receptors are activated, depending on the cause or causes of the nausea . For example, dopamine receptors in the chemotactic trigger zone in the fourth ventricle are stimulated by metabolic and drug causes of nausea, whereas gastric irritation stimulates histamine receptors in the vomiting centre via the vagus nerve.
Reversible causes, such as hypercalcaemia and constipation, should be treated appropriately.
Drug-induced causes should be considered and the offending drugs stopped if possible.
As different classes of antiemetic drug act at different receptors, antiemetic therapy should be based on a careful assessment of the probable causes and a rational decision to use a particular class of drug. The subcutaneous route is often required initially to overcome gastric stasis and poor absorption of oral medicines.
Mechanisms of nausea.
(ACh = acetylcholine; D2 = dopamine;5-HT = 5-hydroxytryptamine, serotonin;
H1 = histamine)
Receptor site activity of antiemetic drugs
Gastrointestinal obstructionGastrointestinal obstruction is a frequent complication
of intra-abdominal cancer. Patients may have multiple
levels of obstruction and symptoms may vary greatly in
nature and severity. Surgical mortality is high in patients
with advanced disease and obstruction should normally
be managed without surgery.
The key to effective management is to address the
presenting symptoms – colic, abdominal pain, nausea,
vomiting, intestinal secretions – individually or in combination, using drugs which do not cause or worsen
other symptoms. This can be problematic when a specific
treatment worsens another symptom.
Cyclizine improves nausea and colic responds well to anticholinergic agents, such as hyoscine butylbromide, but both slow gut motility. Nausea will improve with metoclopramide, although this is contraindicated in the presence of colic because of its prokinetic effect. There is
some evidence that corticosteroids (dexamethasone
8 mg) can shorten the length of obstructive episodes.
Somatostatin analogues, such as octreotide, will reduce
intestinal secretions and therefore large-volume vomits.
Occasionally, a nasogastric tube is required to reduce
gaseous or fluid distension.
Weight loss and general weakness
Patients with cancer lose weight due to an alteration of
metabolism by the tumour known as the cancer cachexia
syndrome. NSAIDs and megestrol may be helpful in
early-stage disease but are unlikely to be effective in
advanced cancer. Corticosteroids can temporarily boost
appetite and general well-being, but may cause false
weight gain by promoting fluid retention. Their benefits
need to be weighed against the risk of side-effects.
Anxiety and depression
Depression is common in palliative care but diagnosis ismore difficult, as the physical symptoms of depression
are similar to those of advanced disease. Anxiety and
depression may still respond to treatment with a combination of drugs and psychotherapeutic approaches.
Citalopram and mirtazapine are better tolerated
in patients with advanced disease. It should not be
assumed that depression is an ‘understandable’ consequence of the patient’s situation.
Delirium and terminal agitation
Many patients become confused or agitated in the lastdays of life. It is important to identify and treat potentially
reversible causes , unless the patient is too close to death for this to be feasible. Early diagnosis and effective management of delirium are extremely important. As in other palliative situations, it may not be possible to identify and treat the underlying cause, and the focus of management may be to ensure comfort. It is important to distinguish between behavioural change due to pain and that due to delirium, as opioids will improve one and worsen the other. It is important, even in palliative care to treat delirium with antipsychotic medicines such as haloperidol rather than regard it as distress or anxiety and use benzodiazepines only.
DEATH AND DYING
Talking about and planning towards dying
There have been dramatic improvements in medical
treatment and care of patients with cancer and other
illnesses over recent years, but the inescapable fact
remains that everyone will die at some time. Planning
for death is not required for people who die suddenly
but should be actively considered in patients with
chronic diseases when the death is considered to be foreseeable or inevitable. Doctors rarely know exactly when a patient will die but we are often aware that the risk of dying is increasing and that medical interventions are unlikely to prolong life or improve function.
Many people wish their doctors to be honest about this situation to allow them time to think ahead, make plans and
address practical issues. A smaller number do not wish
to discuss future deterioration or death; this avoidance
of discussion should be respected. For doctors, it is helpful to understand an individual’s wishes and values about medical interventions at this time, as this can help guide decisions about ceilings of intervention. Some interventions will not work in patients with far advanced disease. It is useful to distinguish between those that will not work (a medical decision) and those that do not confer sufficient benefit to be worthwhile (a decision that can only be reached with a patient’s involvement and consent).
A common example of this would be decisions about not attempting cardiopulmonary resuscitation.
In general, people wish for a dignified and peaceful
death and most prefer to die at home. Families also are
grateful for the chance to prepare themselves for the
death of a relative, by timely and gentle discussion
with their doctor or other health professionals. Early
discussion and effective planning improve the chances
that an individual’s wishes will be achieved.
Diagnosing dying
When patients with cancer become bed-bound, semicomatose, unable to take tablets and only able to take
sips of water, with no reversible cause, they are likely to
be dying and many will have died within 2 days. Patients
with other conditions also reach a stage where death is
predictable and imminent.
Doctors are sometimes poor at recognising this, and should be alert to the views of other members of the multidisciplinary team. A clear decision that the patient is dying should be agreed and recorded.
Management
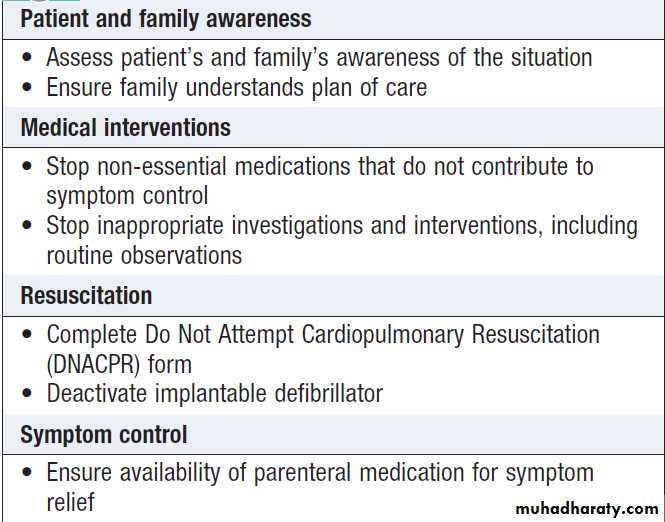
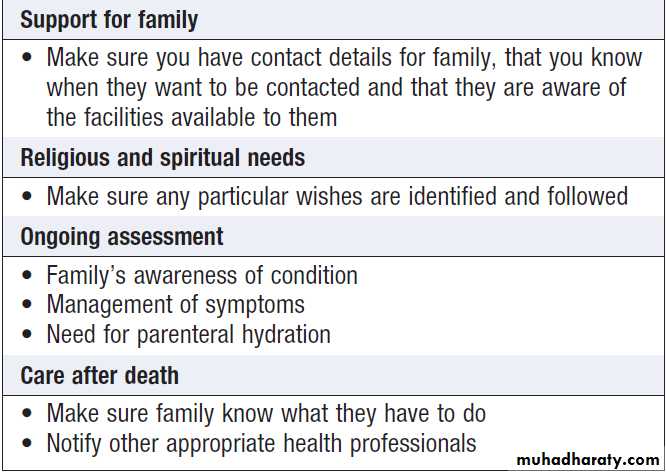
Once the conclusion has been reached that a patient isgoing to die in the next few days, there is a significant shift in management . Symptom control, relief of distress and care for the family become the most important elements of care. Medication and investigation are only justifiable if they contribute to these ends.
When patients can no longer drink because they are
dying, intravenous fluids are usually not necessary and
may cause worsening of bronchial secretions. Medicines
should always be prescribed for the relief of symptoms.
For example, morphine or diamorphine may be used
to control pain, levomepromazine to control nausea,haloperidol to treat confusion, diazepam or midazolam
to treat distress, and hyoscine hydrobromide to reduce
respiratory secretions. Side-effects, such as drowsiness,
may be acceptable if the principal aim of relieving distress
is achieved. It is important to discuss and agree the
aims of care with the patient’s family.
How to manage a patient who is dying
How to manage a patient who is dying – cont’d
Ethical issues at the end of lifeIn Europe, between 25 and 50% of all deaths are associated with some form of decision which may affect the
length of a patient’s life. The most common form of decision
involves withdrawing or withholding further treatment:
for example, not treating a chest infection in a patient who is clearly dying from advanced cancer. It is important to have a framework for considering such decisions (such as the four ethical principles: autonomy, beneficence, non-maleficence and justice), which balances degrees of importance when there is conflict:
for example, when a patient wishes to receive treatment
which a doctor believes will be ineffective or which may
cause harm.
A decision has to be taken as to which principle is most important: whether it is better to respect a patient’s wishes, even if it causes harm, or to reduce the risk of harm but not accede to those wishes.
A futile treatment is one which has no chance of
achieving worthwhile benefit: that is, the treatment
cannot achieve a result that the patient would consider,
now or in the future, to be worthwhile.
Doctors are not required to institute futile treatments, such as resuscitation, in the event of cardiac arrest in a patient with terminal cancer.
Incapacity and advance directives
Patients’ wishes are very important in Western medical
ethics, although other cultures emphasise the views of
the family. If a patient is unable to express his or her
view because of communication or cognitive impairment,
that person lacks ‘capacity’. In order to decide
what the patient would have wished, as much information
as possible should be gained about any previously
expressed wishes, along with the views of relatives and
other health professionals.
An advance directive is a previously recorded, written document of a patient’s wishes.
It should carry the same weight in decision-making as a patient’s contemporaneously expressed wishes, but may not be sufficiently specific to be used in a particular clinicalsituation. The legal framework for decision-making
varies in different countries.
Hydration
Deciding whether to give intravenous fluids can be difficult when a patient is very unwell and the prognosis is uncertain.If a patient is clearly dying and has a prognosis
of a few days, rehydration may cause harm by
increasing bronchial secretions, and will not benefit
the patient by prolonging life.
A patient with a major stroke, who is unable to swallow but expected to survive the event, will develop renal impairment and thirst if not given fluids and should be hydrated. Each decision should be individual and discussed with the patient’s family.
Euthanasia
In the UK and Europe, between 3 and 6% of dying
patients ask a doctor to end their life. Many of these
requests are transient; some are associated with poor
control of physical symptoms or a depressive illness. All
expressions of a wish to die are an opportunity to help
the patient discuss and address unresolved issues and
problems.
Reversible causes, such as pain or depression, should
be treated. Sometimes, patients may choose to discontinue
life-prolonging treatments, such as diuretics or
anticoagulation, following discussion and the provision
of adequate alternative symptom control.