Hussien Mohammed Jumaah
CABMLecturer in internal medicine
Mosul College of Medicine
2016
learning-topics
Environmental and nutritionalfactors in disease
ENVIRONMENTAL FACTORS IN DISEASE
Environmental effects on healthHealth emerges from a highly complex interaction
between factors intrinsic to the patient and his or her
environment. Many factors within the environment
influence health, including aspects of the physical
environment, biological environment (bacteria, viruses),
built environment and social environment. Environmental changes affect many physiological systems and do not respect boundaries between medical specialties. The specialty of ‘public health’ is concerned with the investigation and management of health in communities and populations. Exposure to infectious agents is a major environmental determinant of health.
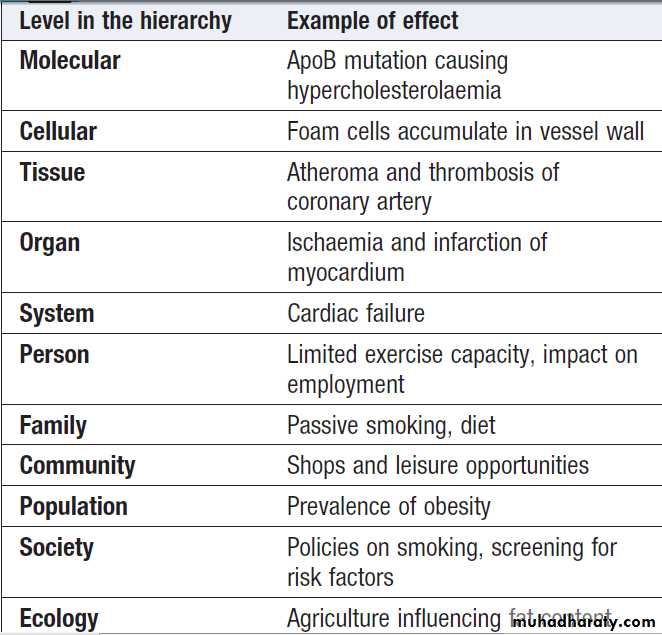
The hierarchy of systems – from molecules to ecologies
When assessing a patient, a clinician subconsciously
considers many levels at which problems may be occurring,
including molecular, cellular, tissue, organ and body systems. When the environment’s influence on health is being considered, this ‘hierarchy of systems’ extends beyond the individual to include the family, community, population and ecology.
Box shows an example of the utility of this concept in describing determinants of coronary heart disease operating at each level of a hierarchy.
‘Hierarchy of systems’ applied to ischaemic heart disease
Hierarchy of systems that influence population health.
Interactions between people and their environmentHealth is an emergent quality of a complex interaction between many determinants, including genetic inheritance, the physical circumstances in which people live (e.g. housing, air quality, working environment), the social environment (e.g. levels of friendship, support and trust), personal behaviour (smoking, diet, exercise), and access to money and the other resources that give people control over their lives.
Health care is not the only determinant and is usually not the major determinant – of health status in the population. These systems do not operate in isolation in separate
communities. When one group responds to ill health
by manipulating its environment, the consequences may be global.
For example, an Afghan farmer who starts growing opium for money in order to feed his children influences the environment of a teenager in Europe; in turn, drug misuse in Europe has fostered higher prevalence of blood-borne infectious diseases such as HIV/AIDS; in turn, these have spilled out into sexually transmitted disease.
Smoking, risky sexual activity and drug misuse.Influences on health can even operate before birth. Individuals with low birth weight have been shown to have a higher prevalence of conditions such as hypertension and type 2 diabetes as young adults and of cardiovascular disease in middle age. It has been suggested that under-nutrition during middle to late gestation permanently ‘programmes’ cardiovascular and metabolic responses.
Investigations in environmental health
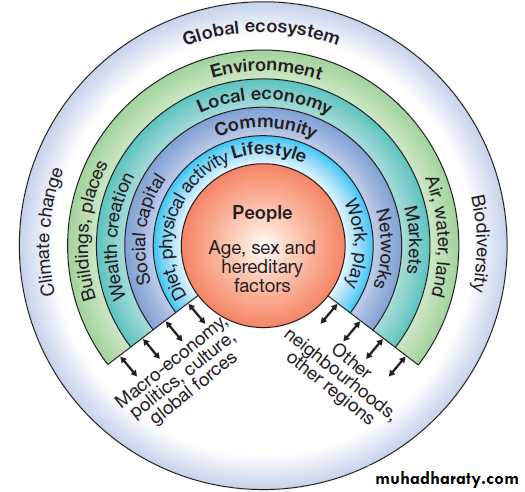
Incidence and prevalenceThe first task is to establish how common a problem is within the population.
This is expressed in two ways.
• If the problem is a continuing condition (e.g. enlarged spleen due to malaria), then prevalence is the appropriate measurement and is calculated by dividing the number of people with the condition at
a specified time by the number of people in the population at risk at that time. Prevalence tends to be higher if the problem is or if it is of longer duration.
• If the problem is an event that occurs at a clear point in time (e.g. fever due to malaria), then incidence is used. Incidence is a measure of the rate at which new cases occur (e.g. confirmed pyrexia with malaria parasites on a blood film) in the population at risk during a defined period of time.
Calculation of risk using descriptive epidemiology
Variability by time, person and placeThe next task is to establish how the problem varies in
terms of time, person and place. The incidence may fluctuate throughout the year; for example, malaria occurs
in the wet season but not the dry. Observation over
longer periods establishes whether a problem is becoming
more or less common: malaria may re-emerge due
to drug resistance. The next questions are,
who are the victims? Are males or females more commonly affected?
What is the age pattern? What are the occupations and
social positions of those affected?
In this example, symptomatic malaria is more common in poorer, ruraldwelling children.
Finally, there is the question of variability by place: the prevalence of malaria is dictated by the distribution of Anopheles mosquitoes.
Measuring risk
Epidemiology is also concerned with the numerical
estimation of risk. This is best illustrated by a simple
example. In a rural African town with a population of
5000, disease ‘d’ is under investigation. The majority of
the cases of disease ‘d’ (300 out of 360) occurred among
women and children who use the river. A formal experiment is established to measure risk. The 1000 women and children who use the river are followed up for 1 year and compared to a cohort with a similar age and sex distribution who use standpipes as their source of water. The incidence (new cases) of disease ‘d’ in the 1000
exposed to risk ‘r’ (river water) was 300.
The incidence (new cases) of disease ‘d’ in the 1000 not exposed to risk ‘r’ was 60.
The relative risk is the incidence in the exposed population (300 per 1000 per year) divided by the incidence in the non-exposed population (60 per 1000 per year); 300/60 = 5, meaning that those exposed to the river water are 5 times more likely to contract the disease – their relative risk is 5. The attributable risk of exposure ‘r’ for disease ‘d’ is the incidence in the exposed population (300) minus the incidence in the non-exposed population (60), which is 240 per 1000 per year. The fraction, or proportion, of the disease in the exposed population which can be attributed to risk (r) is called the attributable fraction, in this case (300−60)/300 = 0.8. This means that 80% of the disease can be attributed to exposure to river water.
Establishing cause and effect
Associations between a risk factor and a disease do notprove that the risk factor causes the disease. In the
northern hemisphere, both multiple sclerosis and blue
eyes are more common but it is implausible that having
blue eyes is the cause of multiple sclerosis.
Cause and effect can only be proven by more detailed investigation. In the above example, further investigation of the river water will be needed, using the criteria for causation defined in Koch’s postulates or the more generic Bradford Hill criteria.
Preventive medicine
There are many examples of epidemiological associationsdefining causative factors in disease, e.g. the association
between cigarette smoking and lung cancer.
However, as illustrated above, the complexity
of the interactions between physical, social and economic
determinants of health means that successful prevention
is often difficult. Moreover, the life course
perspective illustrates that it may be necessary to intervene
early in life or even before birth, to prevent important
disease in later life. Successful prevention is likely
to require many interventions across the life course and
at several levels in the hierarchy of systems.
ENVIRONMENTAL DISEASES
The term ‘homeostasis’ describes the capacity to maintain
the internal milieu by adapting to increases or
decreases in a given environmental factor. However,
there are limits to the coping abilities of any system, at
which ‘too much’ or ‘too little’ of a given environmental
factor will result in ill health. Too many calories lead to
obesity, while too few lead to malnutrition. Either involuntarily or deliberately, we expose ourselves to many
poisons and hazards. Examples discussed elsewhere
include industrial/occupational hazards, such as asbestos
and other carcinogens . ‘Social’ poisons, such as tobacco, alcohol and drugs of misuse, also need to be considered.
Alcohol
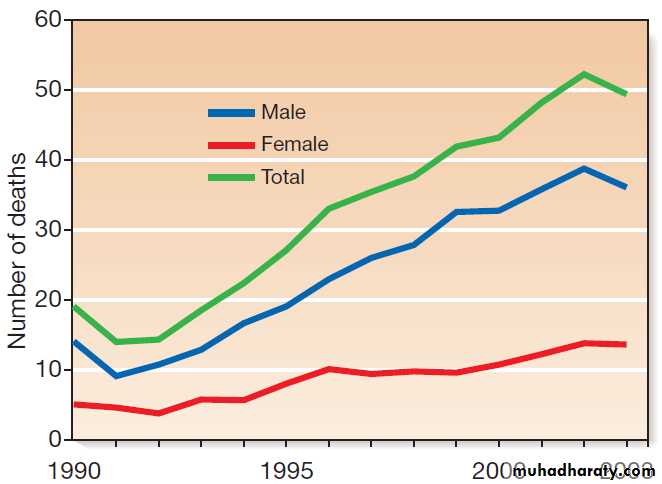
The WHO estimates that the harmful use of alcohol results in the death of 2.5 million people annually. Rates of alcohol-related harm vary by place and time but have risen dramatically in the UK, with Scotland showing the highest rates. (Fig. demonstrates the climbing rates during the 1990s, since when rates have stabilised at very high levels.) Why did Scotland experience this dramatic increase in alcohol deaths? The most likely explanation is that the environment changed.The price of alcohol fell in real terms and availability increased (more supermarkets sold alcohol and the opening times of public houses were extended).
Also, the culture changed in a way that fostered higher levels of consumption and more binge drinking. These changes have caused a trebling of male and a doubling of female deaths due to alcohol. Public, professional and governmental concern has now led to a minimum price being charged for a unit of alcohol, tightening of licensing regulations and curtailment of some promotional activity (e.g. two-for-one offers in bars). Many experts judge that even more aggressive public health measures will be needed to reverse the levels of harm in the community.
Alcohol-related deaths in Scotland by year and sex
(1990–2003). Principal (‘underlying’) and secondary (‘contributing’)
causes of death. (Source: General Register Office (Scotland))
Smoking
Smoking tobacco dramatically increases the risk ofdeveloping many diseases. It is responsible for a substantial majority of cases of lung cancer and chronic
obstructive pulmonary disease, and most smokers
die either from these respiratory diseases or from ischaemic heart disease. Smoking also causes cancers of the upper respiratory and gastrointestinal tracts, pancreas, bladder and kidney, and increases risks of peripheral vascular disease, stroke and peptic ulceration. Maternal smoking is an important cause of fetal growth retardation. Moreover, there is increasing evidence that passive (or ‘secondhand’) smoking has adverse effects on cardiovascular and respiratory health.
When the ill-health effects of smoking were first discovered, doctors imagined that warning people about
the dangers of smoking would result in them giving up.
However, it also took increased taxation of tobacco,
banning of advertising and support for smoking cessation
to maintain a decline in smoking rates. In several
European countries (including the UK), this has culminated
in a complete ban on smoking in all public places
– legislation that only became possible as the public
became convinced of the dangers of secondhand smoke.
However, smoking rates remain high in many poorer
areas and are increasing amongst young women.
In many developing countries, tobacco companies have
found new markets and rates are rising. Worldwide,
there are approximately 1 billion smokers, and it is estimated by WHO that 6 million die prematurely each year as a result of their habit.
In reality, there is a complex hierarchy of systems that
interact to cause smokers to initiate and maintain their
habit. At the molecular and cellular levels, nicotine acts
on the nervous system to create dependence, so that
smokers experience unpleasant effects when they
attempt to quit. So, even if they know it is harmful, the
role of addiction in maintaining the habit is important.
Even if a smoker decides to quit, there are a variety
of influences in the wider environment that reduce thechances of sustained success, including peer pressure,
cigarette advertising, and finding oneself in circumstances
where one previously smoked. The tobacco industry works very hard to maintain and expand the smoking habit, and its advertising budget is much greater than that available to health promoters.
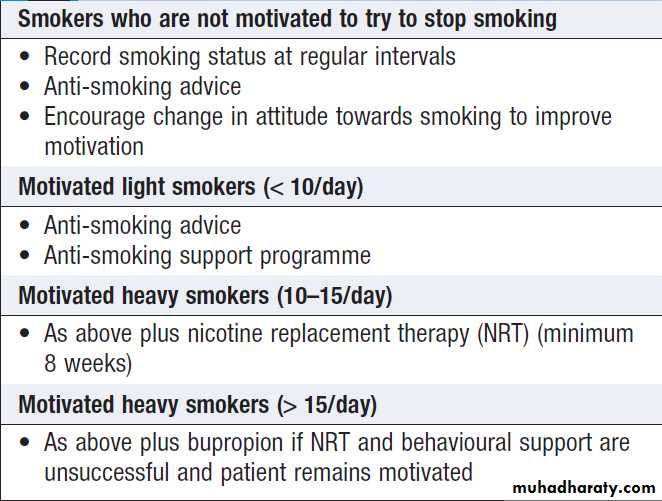
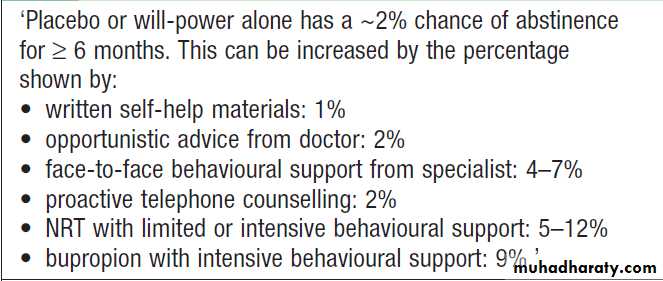
Strategies to help individuals quit smoking are outlined
in Boxes. Although the success rates are modest, these interventions are cost-effective and form an important part of the overall anti-tobacco strategy.
Methods for smoking cessation
Smoking cessation
ObesityObesity is a condition characterised by an excess of body
fat. In its simplest terms, obesity can be considered to
result from an imbalance between the amount of energy
consumed in the diet and the amount of energy expended
through exercise and bodily functions. In 2006, the number of obese and overweight people in the world overtook the numbers who are malnourished and underweight.
The best way, to understand current obesity epidemic is to consider humans as ‘obesogenic organisms’ who, for the first time in their history, find themselves in an obesogenic environment that is, one where people’s circumstances encourage them to eat more and exercise less.
This includes the availability of cheap and heavily marketed energy-rich foods, the increase in labour-saving devices (e.g. lifts and remote controls) and the increase in passive transport (cars as opposed to walking, cycling, or walking to public transport hubs). It is not surprising that we have problems coping with an environment that exerts constant pressure to increase energy intake and to decrease energy expenditure. The rise in obesity suggests that the effects of our obesogenic environment are overriding the biological regulatory mechanisms in more and more people. To combat the health impact of obesity, therefore, we need to help those who are already obese but also develop strategies that impact on the whole population and reverse the obesogenic environment.
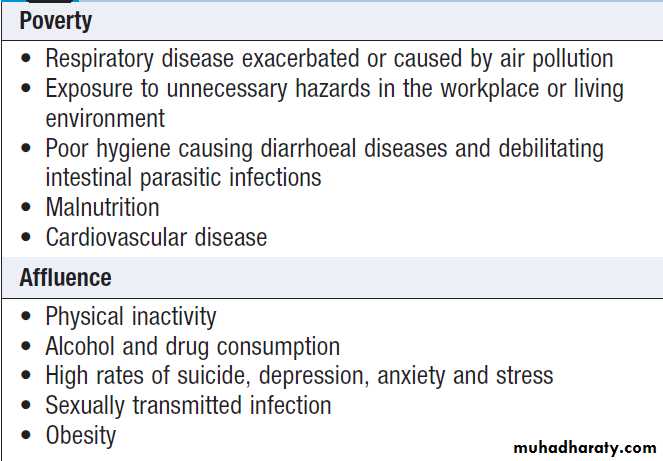
Poverty and affluence
The adverse and social consequences of povertyare :high birth rates, high death rates and short life expectancy. Typically, with industrialisation, the pattern changes: low birth rates, low death rates and longer life expectancy .Instead of infections, chronic conditions such as heart disease dominate in an older population.
Despite economic growth for the last 50 years, people in many industrialised countries are not growing any happier and socioeconomic problems – crime, congestion, inequality – persists. Living in societies that give pride of place to economic growth means that there is constant pressure to contribute by performing ever harder at work and by consuming as much as – or more than – we can afford.
As a result, people become stressed and may adopt unhealthy strategies to mitigate their discomfort; they overeat, overshop, or use sex or drugs (legal and illegal) as ‘pain-killers’. Many countries are now experiencing a ‘double burden’. They have large populations still living in
poverty who are suffering from problems such as diarrhea and malnutrition, alongside affluent populations
who suffer from chronic illness such as diabetes and heart disease. Recent research suggests that uneven distribution of wealth is a more important determinant of health than the absolute level of wealth; countries with a more even distribution of wealth enjoy longer life expectancies than countries with similar or higher gross domestic products (GDPs) but wider distributions of wealth.
Examples of effects of financial resources on health
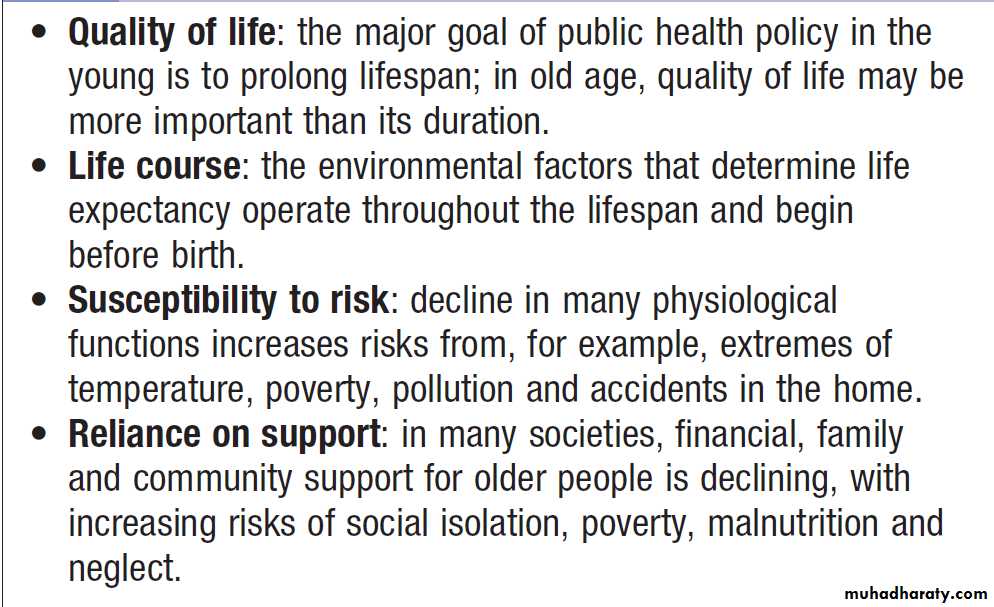
Environmental factors in disease in old age
Atmospheric pollutionEmissions from industry, power plants and motor vehicles
of sulphur oxides, nitrogen oxides, respirable particles
and metals are severely polluting cities and towns
in Asia, Africa, Latin America and Eastern Europe.
Increased death rates from respiratory and cardiovascular
disease occur in vulnerable adults, such as those with
established respiratory disease and the elderly, while
children experience an increase in bronchitic symptoms.
In nations like the UK that have reduced their primary
emissions, the new issue of greenhouse gases has
emerged. Developing countries also suffer high rates of
respiratory disease as a result of indoor pollution caused
mainly by heating and cooking combustion.
Carbon dioxide and global warming
Climate change is arguably the world’s most important
environmental health issue. A combination of increased
production of carbon dioxide and habitat destruction,
both caused primarily by human activity, seems to be
the main cause. The temperature of the globe is rising,
climate is being affected, and if the trend continues,
sea levels will rise and rainfall patterns will be altered
so that both droughts and floods will become more
common. These have already claimed millions of lives
during the past 20 years and have adversely affected the
lives of many more. The economic costs of property
damage and the impact on agriculture, food supplies
and prosperity have also been substantial.
The health impacts of global warming will also include changes in the geographical range of some vector-borne infectious diseases.
Currently, politicians cannot agree on an effective
framework of actions to tackle the problem. Meanwhile,
the industrialised world continues with lifestyles and
levels of waste that are beyond the planet’s ability to
sustain. Rapidly growing economies in the world’s two
most populous states, India and China, are going to be
a vital part of the unfolding problem or solution.
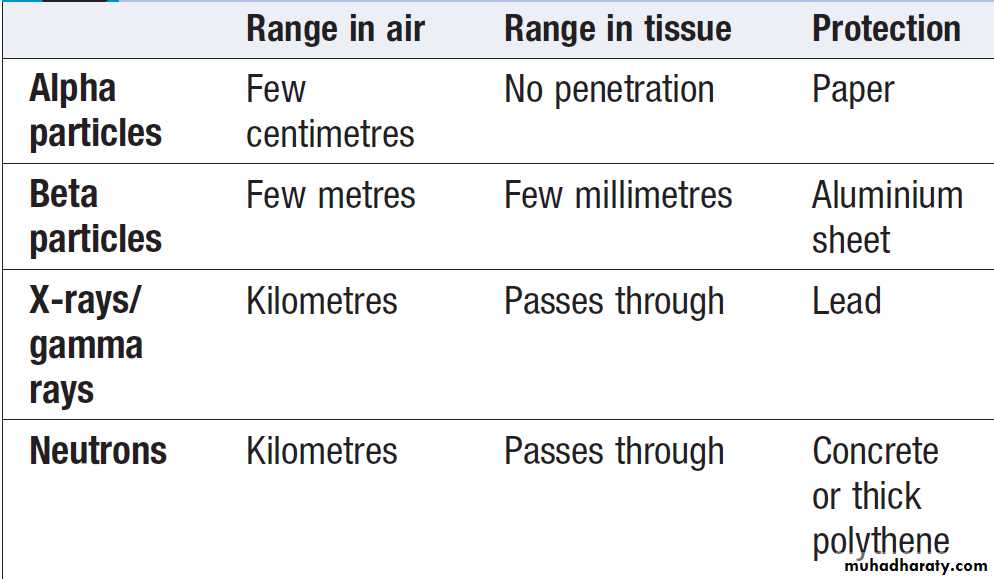
Radiation exposure
Radiation includes ionising (Box) and non-ionising
radiations (ultraviolet (UV), visible light, laser, infrared
and microwave). Whilst global industrialisation and the
generation of fluorocarbons have raised concerns about
loss of the ozone layer, leading to an increased exposure
to UV rays, and disasters such as the Chernobyl and
Fukushima nuclear power station explosions have demonstrated the harm of ionising radiation, it is important
to remember that it can be harnessed for medical benefit.
Ionising radiation is used in X-rays, computed tomography
(CT), radionucleotide scans and radiotherapy, and
non-ionising UV for therapy in skin diseases and laser
therapy for diabetic retinopathy.
Properties of ionising radiations
Types of ionising radiationThese include charged subatomic alpha and beta particles,
uncharged neutrons or high-energy electromagnetic radiations such as X-rays and gamma rays. When they
interact with atoms, energy is released and the resulting
ionisation can lead to molecular damage. The clinical
effects of different forms of radiation depend upon their range in air and tissue penetration.
Dosage and exposure
The dose of radiation is based upon the energy absorbed
by a unit mass of tissue and is measured in grays (Gy),
with 1 Gy representing 1 J/kg. To take account of different types of radiation and variations in the sensitivity
of various tissues, weighting factors are used to produce
a unit of effective dose, measured in sieverts (Sv).
This value reflects the absorbed dose weighted for the
damaging effects of a particular form of radiation and is
most valuable in evaluating the long-term effects of
exposure. ‘Background radiation’ refers to our exposure to naturally occurring radioactivity (e.g. radon gas and cosmic
radiation). This produces an average annual individual
dose of approximately 2.6 mSv per year, although this
varies according to local geology.
Effects of radiation exposure
Effects on the individual are classified as either deterministic or stochastic.Deterministic effects
Deterministic (threshold) effects occur with increasing
severity as the dose of radiation rises above a threshold
level. Tissues with actively dividing cells, such as bone
marrow and gastrointestinal mucosa, are particularly
sensitive to ionising radiation. Lymphocyte depletion is
the most sensitive marker of bone marrow injury, and
after exposure to a fatal dose, marrow aplasia is a
common cause of death. However, gastrointestinal
mucosal toxicity may cause earlier death due to profound
diarrhoea, vomiting, dehydration and sepsis.
The gonads are highly radiosensitive and radiation may
result in temporary or permanent sterility.
Eye exposure can lead to cataracts and the skin is susceptible to radiation burns. Irradiation of the lung and central nervous system may induce acute inflammatory reactions, pulmonary fibrosis and permanent neurological deficit respectively. Bone necrosis and lymphatic fibrosis are characteristic following regional irradiation, particularly for breast cancer. The thyroid gland is not inherently sensitive but its ability to concentrate iodine makes it susceptible to damage after exposure to relatively low doses of radioactive iodine isotopes, such as were released from Chernobyl.
Stochastic effects
Stochastic (chance) effects occur with increasing probabilityas the dose of radiation increases. Carcinogenesis
represents a stochastic effect. With acute exposures, leukaemias may arise after an interval of 2–5 years and solid tumours after an interval of about 10–20 years.
Thereafter the incidence rises with time. An individual’s
risk of developing cancer depends on the dose received,
the time to accumulate the total dose and the interval
following exposure.
Management of radiation exposure
The principal problems after large-dose exposures aremaintenance of adequate hydration, control of sepsis
and the management of marrow aplasia. Associated
injuries such as thermal burns need specialist management
within 48 hours of active resuscitation. Internal
exposure to radioisotopes should be treated with chelating agents (such as Prussian blue used to chelate
137-caesium after ingestion). White cell colony stimulation
and haematopoietic stem cell transplantation may
need to be considered for marrow aplasia.
Extremes of temperature
Thermoregulation
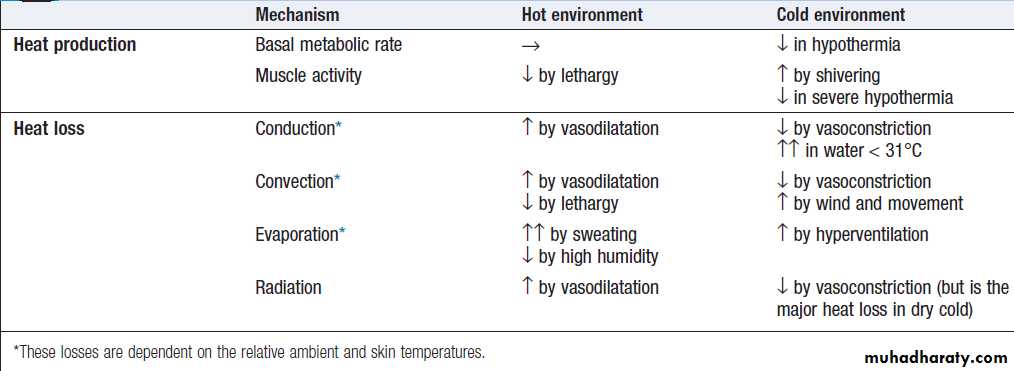
Body heat is generated by basal metabolic activity and
muscle movement, and lost by conduction (which is
more effective in water than in air), convection, evaporation and radiation (most important at lower temperatures when other mechanisms conserve heat) (Box).
Body temperature is controlled in the hypothalamus,
which is directly sensitive to changes in core temperature
and indirectly responds to temperature-sensitive
neurons in the skin. The normal ‘set-point’ of core temperature is tightly regulated within 37 ± 0.5°C, which
is necessary to preserve the normal function of many
enzymes and other metabolic processes.
The temperature set-point is increased in response to infection .
In a cold environment, protective mechanisms include cutaneous vasoconstriction and shivering; however, any muscle activity that involves movement may promote heat loss by increasing convective loss from the skin, and respiratory heat loss by stimulating ventilation. In a hot environment, sweating is the main mechanism for increasing heat loss. This usually occurs when the ambient temperature rises above 32.5°C or during exercise.Thermoregulation:
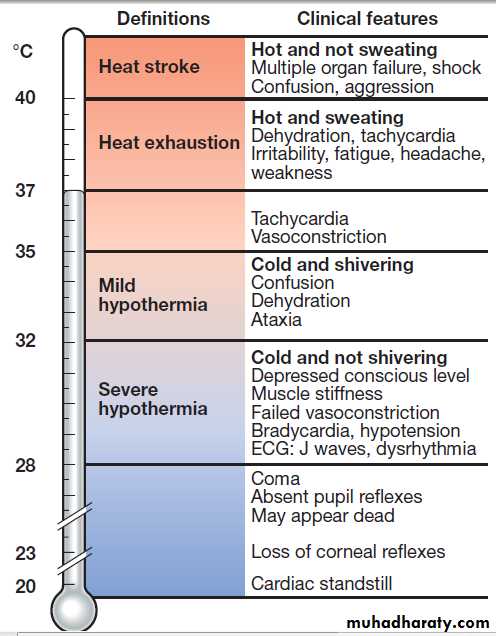
responses to hot and cold environmentsHypothermia
Hypothermia exists when the body’s normal thermal
regulatory mechanisms are unable to maintain heat
in a cold environment and core temperature falls below
35°C (Fig.). Whilst infants are susceptible to hypothermia because of their poor thermoregulation and high body surface area to weight ratio, it is the elderly who are at highest risk (Box). Hypothyroidism is often a contributory factor in old age, while alcohol and other drugs (e.g.
phenothiazines) commonly impede the thermoregulatory
response in younger people. More rarely, hypothermia
is secondary to glucocorticoid insufficiency, stroke,
hepatic failure or hypoglycaemia.
Hypothermia also occurs in healthy individuals whose thermoregulatory mechanisms are intact but insufficient to cope with the intensity of the thermal stress. Typical examples include immersion in cold water, when core temperature may fall rapidly (acute hypothermia), exposure to extreme climates such as during hill walking (subacute hypothermia), and slow-onset hypothermia, as develops in an immobilized older individual (subchronic hypothermia).
This classification is important, as it determines the method of rewarming.
Clinical features of abnormal core temperature.
The hypothalamus normally maintains core temperature at 37°C, but this set-point is altered – for example, in fever and may be lost in hypothalamic disease.In these circumstances, the clinical picture at a given core temperature may be different
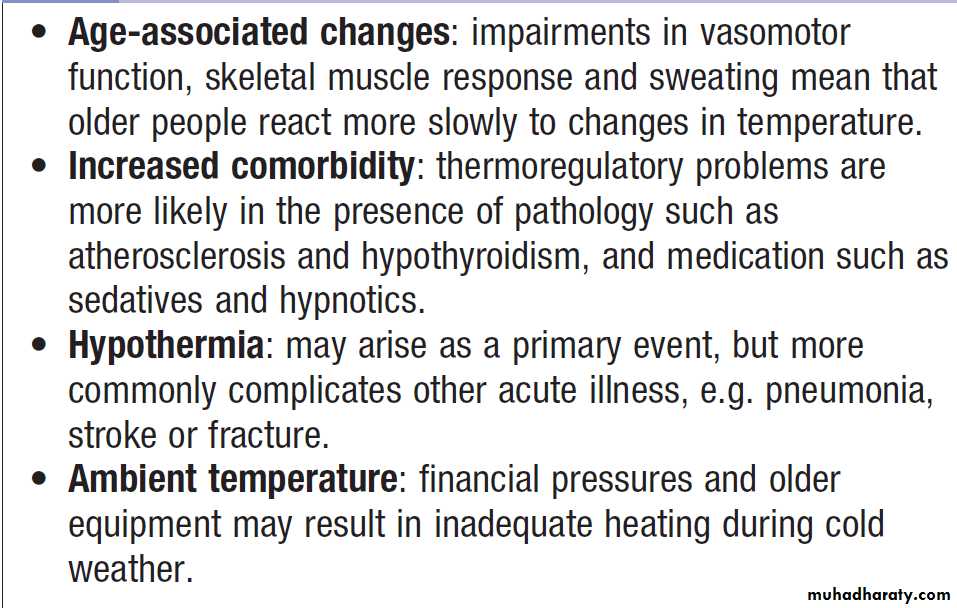
Thermoregulation in old age
Clinical featuresDiagnosis is dependent on recognition of the environmental circumstances and measurement of core (rectal) body temperature. Clinical features depend on the
degree of hypothermia (see Fig). In a cold patient, it is very difficult to diagnose death reliably by clinical means. It has been suggested that, in extreme environmental conditions, irreversible hypothermia is probably present if there is asystole (no carotid pulse for 1 minute), the chest and abdomen are rigid, the core temperature is below 13°C and serum potassium is > 12 mmol/L. However, in general, resuscitative measures should continue until the core temperature is normal and only then should a diagnosis of brain death be considered.
Investigations
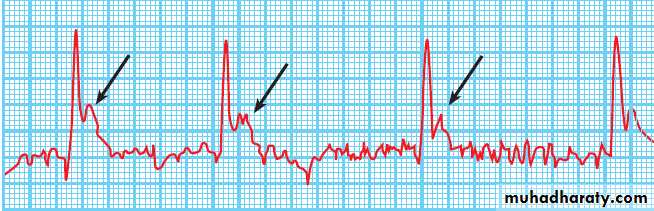
Blood gases, a full blood count, electrolytes, CX-ray .Haemoconcentration , metabolic acidosis are common, and the ECG may show characteristic J waves, which occur at the junction of the QRS complex and the ST segment . Cardiac dysrhythmias, including ventricular fibrillation, may occur, the arterial PO2 in the blood falls by 7%
for each 1°C fall in core temperature. Serum aspartate aminotransferase and creatine kinase may be elevated secondary to muscle damage and the serum amylase is often high due to subclinical pancreatitis. If the cause of hypothermia is not obvious, additional investigations for thyroid and pituitary dysfunction , hypoglycaemia and the possibility of drug intoxication should be performed.
Electrocardiogram showing J waves (arrows) in a hypothermic patient.
ManagementFollowing resuscitation, the objectives of management
are to rewarm the patient in a controlled manner while
treating associated hypoxia (by oxygenation and ventilation if necessary), fluid and electrolyte disturbance,
and cardiovascular abnormalities, particularly dysrhythmias.
Careful handling is essential to avoid precipitating
the latter. The method of rewarming is dependent not on the absolute core temperature, but on haemodynamic stability and the presence or absence of an effective cardiac output.
Mild hypothermia
Outdoors, continued heat loss is prevented by sheltering
the patient from the cold, replacing wet clothing, covering
the head and insulating him or her from the ground.
Once in hospital, even in the presence of profound hypothermia, if there is an effective cardiac output then
forced-air rewarming, heat packs placed in axilla, groin
and around the abdomen, inhaled warmed air and correction of fluid and electrolyte disturbances are usually
sufficient.
Rewarming rates of 1–2°C per hour are effective
in leading to a gradual and safe return to physiological
normality. Underlying conditions should be treated
promptly (e.g. hypothyroidism with triiodothyronine
10 μg IV 3 times daily.
Severe hypothermia
In the case of severe hypothermia with cardiopulmonaryarrest (non-perfusing rhythm), the aim is to restore
perfusion, and rapid rewarming at a rate greater than
2°C per hour is required. This is best achieved by
cardiopulmonary bypass or extracorporeal membrane
oxygenation. If these are unavailable, then veno–veno
haemofiltration, and pleural, peritoneal, thoracic or
bladder lavage with warmed fluids are alternatives.
Monitoring of cardiac rhythm and arterial blood gases,
including H+ (pH) is essential.
Significant acidosis may require correction.
Cold injury
Freezing cold injury (frostbite)
This represents the direct freezing of body tissues and
usually affects the extremities: in particular, the fingers,
toes, ears and face. Risk factors include smoking, peripheral vascular disease, dehydration and alcohol consumption. The tissues may become anaesthetised before freezing and, as a result, the injury often goes unrecognized at first. Frostbitten tissue is initially pale and doughy to the touch and insensitive to pain (Fig.). Once frozen, the tissue is hard. Rewarming should not occur until it can be achieved rapidly in a water bath. Give oxygen and aspirin 300 mg as soon as possible. Frostbitten extremities should be rewarmed in warm water at 37–39°C, with antiseptic added.
Adequate analgesia is necessary, as rewarming
is very painful. Vasodilators such as pentoxifylline (aphosphodiesterase inhibitor) have been shown to
improve tissue survival. Once it has thawed, the injured
part must not be re-exposed to the cold, and should be
dressed and rested.
Whilst wound débridement may be necessary, amputations should be delayed for 60–90 days, as good recovery may occur over an extended period.
Frostbite in a female Everest sherpa.
Non-freezing cold injury(trench or immersion foot)
This results from prolonged exposure to cold, damp conditions.
The limb (usually the foot) appears cold, ischaemic
and numb, but there is no freezing of the tissue. On
rewarming, the limb appears mottled and thereafter
becomes hyperaemic, swollen and painful. Recovery
may take many months, during which there may be
chronic pain and sensitivity to cold. The pathology
remains uncertain but probably involves endothelial
injury. Gradual rewarming is associated with less pain
than rapid rewarming.
The pain and associated paraesthesia
are difficult to control with conventional analgesia
and may require amitriptyline (50 mg nocte), best instituted
early. The patient is at risk of further damage on
subsequent exposure to the cold.
Chilblains
Chilblains are tender, red or purplish skin lesions that
occur in the cold and wet. They are often seen in horse
riders, cyclists and swimmers, and are more common in
women than men. They are short-lived, and although
painful, not usually serious.
Heat-related illness
When generation of heat exceeds the body’s capacityfor heat loss, core temperature rises. Non-exertional
heat illness (NEHI) occurs with high environmental temperature in those with attenuated thermoregulatory
control mechanisms: the elderly, the young, those with
comorbidity or those taking drugs that affect thermoregulation (particularly phenothiazines, diuretics and
alcohol). Exertional heat illness (EHI), on the other hand,
typically develops in athletes when heat production
exceeds the body’s ability to dissipate it.
Acclimatisation mechanisms to environmental heat
include stimulation of the sweat mechanism with
increased sweat volume, reduced sweat sodium content
and secondary hyperaldosteronism to maintain body
sodium balance. The risk of heat-related illness falls as
acclimatisation occurs. Heat illness can be prevented to
a large extent by adequate replacement of salt and water, although excessive water intake alone should be avoided because of the risk of dilutional hyponatraemia.
A spectrum of illnesses occurs in the heat (see Fig. ).
The cause is usually obvious but the differential diagnosis should be considered.
Differential diagnosis in patients with
elevated core body temperature• Heat illness (heat exhaustion, heat stroke)
• Sepsis, including meningitis
• Malaria
• Drug overdose
• Malignant hyperpyrexia
• Thyroid storm
Heat cramps
These painful muscle contractions occur following vigorous exercise and profuse sweating in hot weather.There is no elevation of core temperature. The mechanism
is considered to be extracellular sodium depletion
as a result of persistent sweating, exacerbated by replacement of water but not salt. Symptoms usually respond rapidly to rehydration with oral rehydration salts or intravenous saline.
Heat syncope
This is similar to a vasovagal faint and is related
to peripheral vasodilatation in hot weather.
Heat exhaustion
Heat exhaustion occurs with prolonged exertion in hot
and humid weather, profuse sweating and inadequate
salt and water replacement. There is an elevation in
core (rectal) temperature to between 37°C and 40°C,
leading to the clinical features shown in Figure.
Blood analyses may show evidence of dehydration
with mild elevation of the blood urea, sodium and
haematocrit. Treatment involves removal of the patient
from the heat, and active evaporative cooling using
tepid sprays and fanning (strip–spray–fan). Fluid losses
are replaced with either oral rehydration mixtures or
intravenous isotonic saline. Up to 5 L positive fluid
balance may be required in the first 24 hours. Untreated,
heat exhaustion may progress to heat stroke.
Heat stroke
Heat stroke occurs when the core body temperaturerises above 40°C and is a life-threatening condition. The
symptoms of heat exhaustion progress to include headache,
nausea and vomiting. Neurological manifestations
include a coarse muscle tremor and confusion, aggression
or loss of consciousness. The patient’s skin feels
very hot, and sweating is often absent due to failure of
thermoregulatory mechanisms. Complications include
hypovolaemic shock, lactic acidosis, disseminated intravascular coagulation, rhabdomyolysis, hepatic and renal failure, and pulmonary and cerebral oedema.
The patient should be resuscitated with rapid cooling
by spraying with water, fanning and ice packs in the
axillae and groins. Cold crystalloid intravenous fluids
are given but solutions containing potassium should be
avoided. Over-aggressive fluid replacement must be
avoided, as it may precipitate pulmonary oedema or
further metabolic disturbance.
Appropriate monitoring of fluid balance, including central venous pressure, is important.
Investigations for complications include routine haematology and biochemistry, coagulation screen, hepatic transaminases (aspartate aminotransferase and alanine aminotransferase), creatine kinase and chest X-ray.
Once emergency treatment is established, heat stroke patients are best managed in intensive care.
With appropriate treatment, recovery from heat
stroke can be rapid (within 1–2 hours) but patients who
have had core temperatures higher than 40°C should be
monitored carefully for later onset of rhabdomyolysis,
renal damage and other complications before discharge
from hospital. Clear advice to avoid heat and heavy
exercise during recovery is important.
High altitude
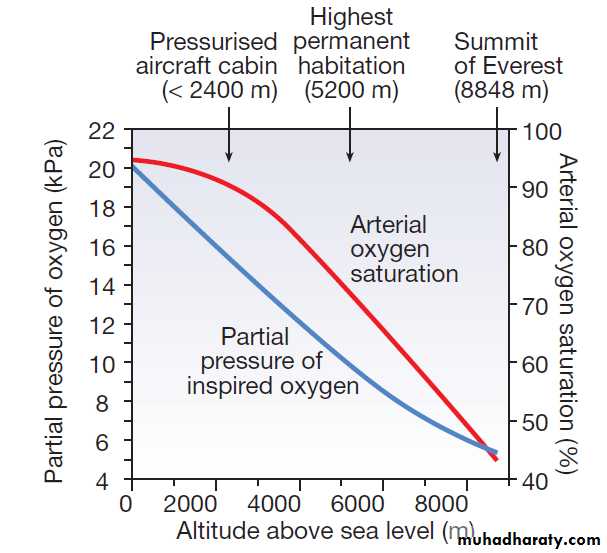
The physiological effects of high altitude are significant.On Everest, the barometric pressure of the atmosphere
falls from sea level by approximately 50% at base camp
(5400 m) and approximately 70% at the summit (8848 m).
The proportions of oxygen, nitrogen and carbon dioxide
in air do not change with the fall in pressure but their
partial pressure falls in proportion to barometric pressure
(Fig.). Oxygen tension within the pulmonary alveoli is further reduced at altitude because the partial
pressure of water vapour is related to body temperature
and not barometric pressure, and so is proportionately
greater at altitude, accounting for only 6% of barometric
pressure at sea level, but 19% at 8848 m.
Change in inspired oxygen tension and blood oxygen
saturation at altitude. The blue curve shows changes in oxygen availability at altitude and the red curve shows the typical resultant changes in arterial oxygen saturation in a healthy person. Oxygensaturation varies between individuals according to the shape of the oxygen–haemoglobin dissociation curve and the ventilatory response to hypoxaemia.
(To convert kPa to mmHg, multiply by 7.5.)
Physiological effects of high altitude
Reduction in oxygen tension results in a fall in arterialoxygen saturation (see Fig.). This varies widely
between individuals, depending on the shape of the
sigmoid oxygen–haemoglobin dissociation curve and the ventilatory response. Acclimatisation to hypoxaemia at high altitude involves a shift in this dissociation curve (dependent on 2,3- diphosphoglycerate (DPG)), erythropoiesis, haemoconcentration, and hyperventilation resulting from hypoxic drive (which is then sustained despite hypocapnia by restoration of cerebrospinal fluid pH to normal in prolonged hypoxia). This process takes several days, so travellers need to plan accordingly.
Illnesses at high altitude
Ascent to altitudes up to 2500 m or travel in a pressurisedaircraft cabin is harmless to healthy people. Above
2500 m high-altitude illnesses may occur in previously
healthy people, and above 3500 m these become common.
Sudden ascent to altitudes above 6000 m, as experienced
by aviators, balloonists and astronauts, may result in decompression illness with the same clinical features as seen in divers (see below), or even loss of consciousness. However, most altitude illness occurs in travellers and mountaineers.
Acute mountain sickness
Acute mountain sickness (AMS) is a syndrome comprised
principally of headache, together with fatigue,
anorexia, nausea and vomiting, difficulty sleeping or
dizziness. Ataxia and peripheral oedema may be present.
Its aetiology is not fully understood but it is thought
that hypoxaemia increases cerebral blood flow and
hence intracranial pressure. Symptoms occur within
6–12 hours of an ascent and vary in severity from trivial
to completely incapacitating.
The incidence in travelers to 3000 m may be 40–50%, depending on the rate of ascent.
Treatment of mild cases consists of rest and simple
analgesia; symptoms usually resolve after 1–3 days at astable altitude, but may recur with further ascent. Occasionally there is progression to cerebral oedema. Persistent symptoms indicate the need to descend but may
respond to acetazolamide, a carbonic anhydrase inhibitor
that induces a metabolic acidosis and stimulates ventilation;
acetazolamide may also be used as prophylaxis
if a rapid ascent is planned
High-altitude cerebral oedema
The cardinal symptoms of high-altitude cerebral oedema(HACE) are ataxia and altered consciousness. This is
rare, life-threatening and usually preceded by AMS. In
addition to features of AMS, the patient suffers confusion,
disorientation, visual disturbance, lethargy and
ultimately loss of consciousness. Papilloedema and
retinal haemorrhages are common and focal neurological
signs may be found.
Treatment is directed at improving oxygenation.
Descent is essential and dexamethasone (8 mg immediately
and 4 mg 4 times daily) should be given. If descent
is impossible, oxygen therapy in a portable pressurised
bag may be helpful.
High-altitude pulmonary oedema
High-altitude pulmonary oedema (HAPE) is a lifethreatening condition that usually occurs in the first 4
days after ascent above 2500 m. Unlike HACE, HAPE
may occur de novo without the preceding signs of AMS.
Presentation is with symptoms of dry cough, exertional
dyspnoea and extreme fatigue. Later, the cough becomes
wet and sputum may be blood-stained. Tachycardia and
tachypnoea occur at rest and crepitations may often be
heard in both lung fields.
There may be profound hypoxaemia,
pulmonary hypertension and radiological evidence
of diffuse alveolar oedema.
It is not known whether the alveolar oedema is a result of mechanical stress on the pulmonary capillaries associated with the high pulmonary arterial pressure, or an effect of hypoxia on capillary permeability. Reduced arterial oxygen saturation is not diagnostic but is a marker for disease progression.
Treatment is directed at reversal of hypoxia with
immediate descent and oxygen administration.
Nifedipine (20 mg 4 times daily) should be given to reduce
pulmonary arterial pressure, and oxygen therapy in a
portable pressurised bag should be used if descent is
delayed.
Chronic mountain sickness
(Monge’s disease)
This occurs on prolonged exposure to altitude and has
been reported in residents of Colorado, South America
and Tibet. Patients present with headache, poor concentration and other signs of polycythaemia. They are
cyanosed and often have finger clubbing.
High-altitude retinal haemorrhage
This occurs in over 30% of trekkers at 5000 m. The
haemorrhages are usually asymptomatic and resolve
spontaneously. Visual defects can occur with haemorrhage
involving the macula, but there is no specific treatment.
Venous thrombosis
This has been reported at altitudes over 6000 m. Riskfactors include dehydration, inactivity and the cold. The
use of the oral contraceptive pill at high altitude should
be considered carefully, as this is an additional risk
factor.
Refractory cough
A cough at high altitude is common and usually benign.
It may be due to breathing dry, cold air and increased
mouth breathing, with consequent dry oral mucosa. This
may be indistinguishable from the early signs of HAPE.
Air travel
Commercial aircraft usually cruise at 10 000–12 000 m, with the cabin pressurised to an equivalent of around 2400 m. At this altitude, the partial pressure of oxygen is 16 kPa (120 mmHg), leading to a PaO2 in healthy people of 7.0–8.5 kPa (53–64 mmHg). Oxygen saturation is also reduced, but to a lesser degree. Although well tolerated by healthy people, this degree of hypoxia may be dangerous in patients with respiratory disease.
Advice for patients with respiratory disease
The British Thoracic Society has published guidance onthe management of patients with respiratory disease
who want to fly. Specialist pre-flight assessment is
advised for all patients who have hypoxaemia (oxygen
saturation < 95%) at sea level, and includes spirometry
and a hypoxic challenge test with 15% oxygen (performed
in hospital). Air travel may have to be avoided
or undertaken only with inspired oxygen therapy during
the flight. Asthmatic patients should be advised to
carry their inhalers in their hand baggage. Following
pneumothorax, flying should be avoided while air
remains in the pleural cavity, but can be considered after
proven resolution or definitive (surgical) treatment.
Advice for other patients
Other circumstances in which patients are more susceptibleto hypoxia require individual assessment. These
include cardiac dysrhythmia, sickle-cell disease and
ischaemic heart disease. Most airlines decline to carry
pregnant women after the 36th week of gestation. In
complicated pregnancies it may be advisable to avoid air
travel at an earlier stage. Patients who have had recent
abdominal surgery, including laparoscopy, should
avoid flying until all intraperitoneal gas is reabsorbed.
Divers should not fly for 24 hours after a dive requiring
decompression stops.
Ear and sinus pain due to changes in gas volume
are common but usually mild, although patients with
chronic sinusitis and otitis media may need specialist
assessment. A healthy mobile tympanic membrane visualized during a Valsalva manoeuvre usually suggests a
patent Eustachian tube.
On long-haul flights, patients with diabetes mellitus
may need to adjust their insulin or oral hypoglycaemic
dosing according to the timing of in-flight and subsequent
meals . Advice is available from Diabetes
UK and other websites. Patients should be able to
provide documentary evidence of the need to carry
needles and insulin.
Deep venous thrombosis
Air travellers have an increased risk of venous thrombosisdue to a combination of factors, including loss of venous emptying because of prolonged immobilisation (lack of muscular activity) and reduced barometric pressure on the tissues, together with haemoconcentration as a result of oedema and perhaps a degree of hypoxia-induced diuresis. Venous thrombosis can probably be prevented by
avoiding dehydration and excess alcohol, and exercising
muscles during the flight.
Without a clear cost–benefit analysis, prophylaxis with aspirin or heparin cannot be recommended routinely, but may be considered in high-risk cases.
Under water
Drowning and near-drowningDrowning is defined as death due to asphyxiation following immersion in a fluid, whilst
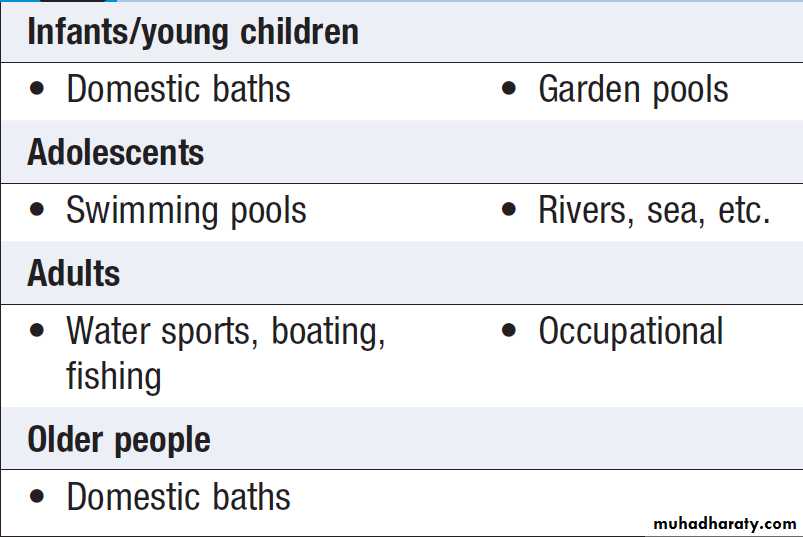
near-drowning is defined as survival for longer than 24 hours after suffocation by immersion. Drowning remains a common cause of accidental death throughout the world and is particularly common in young children (Box). In about 10% of cases, no water enters the lungs and death follows intense laryngospasm (‘dry’ drowning).
Prolonged immersion in cold water, with or without water
inhalation, results in a rapid fall in core body temperature
and hypothermia .
Following inhalation of water, there is a rapid onset
of ventilation–perfusion imbalance with hypoxaemia,
and the development of diffuse pulmonary oedema.
Fresh water is hypotonic and, although rapidly absorbed
across alveolar membranes, impairs surfactant function,
which leads to alveolar collapse and right-to-left shunting
of unoxygenated blood. Absorption of large amounts
of hypotonic fluid can result in haemolysis.
Salt water is hypertonic and inhalation provokes alveolar oedema, but the overall clinical effect is similar to that of fresh-water drowning.
Most common causes of drowning by age
Clinical featuresThose rescued alive (near-drowning) are often unconscious
and not breathing. Hypoxaemia and metabolic
acidosis are inevitable features. Acute lung injury
usually resolves rapidly over 48–72 hours, unless infection
occurs . Complications include dehydration,
hypotension, haemoptysis, rhabdomyolysis, renal
failure and cardiac dysrhythmias. A small number of
patients, mainly the more severely ill, progress to
develop the acute respiratory distress syndrome
(ARDS). Survival is possible after immersion for up to 30
minutes in very cold water, as the rapid development
of hypothermia after immersion may be protective,
particularly in children.
Long-term outcome depends on the severity of the cerebral hypoxic injury and is predicted by the duration of immersion, delay in resuscitation, intensity of acidosis and the presence of cardiac arrest.
Management
Initial management requires cardiopulmonary resuscitation
with administration of oxygen and maintenance
of the circulation .It is important to clear the airway of foreign bodies and protect the cervical spine.
Continuous positive airways pressure (CPAP) should be considered for spontaneously breathing patients with oxygen saturations below 94%. Observation is required for a minimum of 24 hours. Prophylactic antibiotics are only required if exposure was to obviously contaminated water.
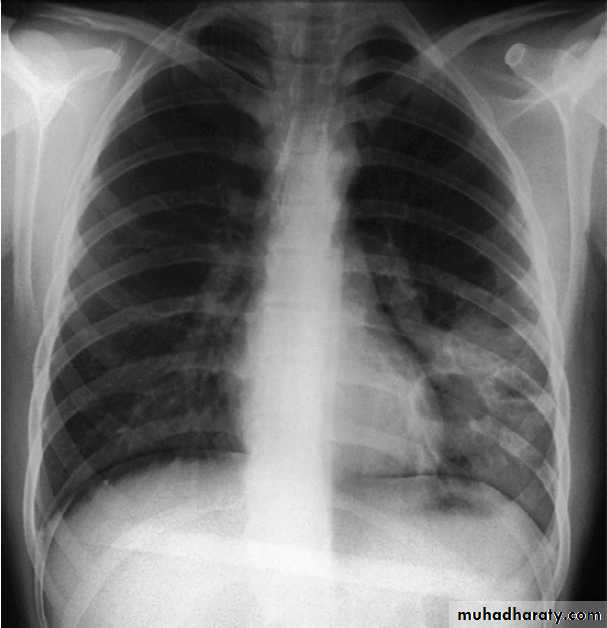
Near-drowning. Chest X-ray of a 39-year-old farmer, 2 weeks
after immersion in a polluted freshwater ditch for 5 minutes before rescue.Airspace consolidation and cavities in the left lower lobe reflect secondary
staphylococcal pneumonia and abscess formation.
Diving-related illness
The underwater environment is extremely hostile. Otherthan drowning, most diving illness is related to changes
in barometric pressure and its effect on gas behaviour.
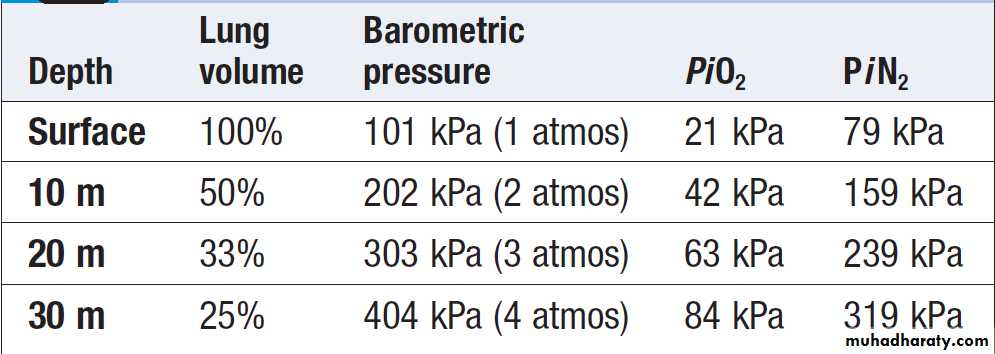
Ambient pressure under water increases by 101 kPa
(1 atmosphere) for every 10 metres of seawater (msw)
depth. As divers descend, the partial pressures of the
gases they are breathing increase and the blood and tissue concentrations of dissolved gases rise accordingly. Nitrogen is a weak anaesthetic agent, and if the inspiratory pressure of nitrogen is allowed to increase above −320 kPa (i.e. a depth of approximately 30 msw), it produces ‘narcosis’, resulting in impairment of cognitive function and manual dexterity, not unlike alcohol intoxication.
For this reason, compressed air can only be used for shallow diving. Oxygen is also toxic at inspired pressures above approximately 40 kPa (inducing apprehension, muscle twitching, euphoria, sweating, tinnitus, nausea and vertigo), so 100% oxygen cannot be used as an alternative. For dives deeper than approximately 30 msw, mixtures of oxygen with nitrogen and/or helium are used.
Whilst drowning remains the most common divingrelated
cause of death, another important group of disorders usually present once the diver returns to the
surface: decompression illness (DCI) and barotrauma.
Physics of breathing compressed air while
diving in sea waterClinical features
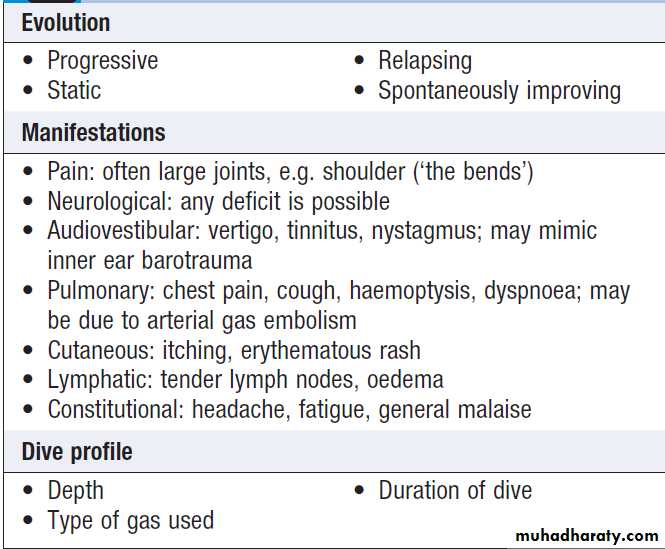
Decompression illnessThis includes decompression sickness (DCS) and arterial
gas embolism (AGE). Whilst the vast majority of symptoms
of decompression illness present within 6 hours of
a dive, they can also be provoked by flying and thus
patients may present to medical services at sites far
removed from the dive.
Exposure of individuals to increased partial pressures
of nitrogen results in additional nitrogen being
dissolved in body tissues; the amount dissolved depends
on the depth/pressure and on the duration of the dive.
On ascent, the tissues become supersaturated with nitrogen,
and this places the diver at risk of producing a critical quantity of gas (bubbles) in tissues if the ascent is too fast.
The gas so formed may cause symptoms locally, by bubbles passing through the pulmonary vascular bed (Box) or by embolisation elsewhere.
Arterial embolisation may occur if the gas load in the venous system exceeds the lungs’ abilities to excrete nitrogen, or when bubbles pass through a patent foramen ovale (present asymptomatically in 25–30% of adults).
Although DCS and AGE can be indistinguishable, their
early treatment is the same.
Assessment of a patient with decompression illness
BarotraumaDuring the ascent phase of a dive, the gas in the diver’s
lungs expands due to the decreasing pressure. The diver
must therefore ascend slowly and breathe regularly; if
ascent is rapid or the diver holds his/her breath, the
expanding gas may cause lung rupture (pulmonary
barotrauma). This can result in pneumomediastinum,
pneumothorax or AGE due to gas passing directly into
the pulmonary venous system.
Other air-filled body cavities may be subject to barotrauma, including the ear and sinuses.
Management
The patient is nursed horizontally, and airway, breathing
and circulation are assessed. Treatment includes the
following:
• High-flow oxygen is given by a tight-fitting mask
using a rebreathing bag. This assists in the washout
of excess inert gas (nitrogen) and may reduce the
extent of local tissue hypoxia resulting from focal
embolic injury.
• Fluid replacement (oral or intravenous) corrects the
intravascular fluid loss from endothelial bubble
injury and the dehydration associated with immersion. Maintenance of an adequate peripheral circulation is important for the excretion of excess dissolved gas.
Recompression is the definitive therapy. Transfer
to a recompression chamber facility may be bysurface or air, provided that the altitude remains
low (< 300 m) and the patient continues to breathe
100% oxygen. Recompression reduces the volume
of gas within tissues and puts nitrogen back into
solution.
The majority of patients make a complete recovery
with treatment, although a small but significant proportion
are left with neurological disability.
NUTRITIONAL FACTORS AND DISEASE
Obtaining adequate nutrition is a fundamental requirement
for survival of every individual and species. The
politics of food provision for humans are complex, and
constitute a prominent factor in wars, natural disasters
and the global economy. In recent decades, economic
success has been rewarded by plentiful nutrition
unknown to previous generations, which has led to a
pandemic of obesity and its serious consequences for
health. Yet, in many parts of the world, famine and
under-nutrition still represent a huge burden. Quality,
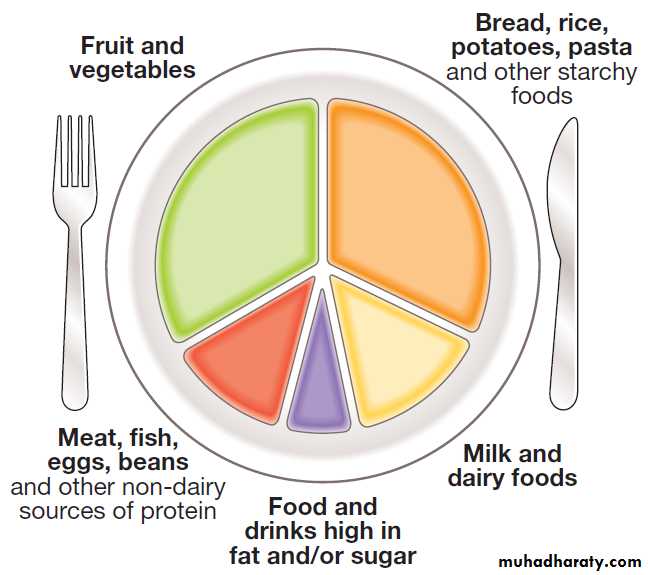
as well as quantity, of food influences health, with governmental advice on healthy diets maximising fruit and
vegetable intakes .
Inappropriate diets have been linked with diseases such as coronary heart disease and cancer.
Deficiencies of simple vitamins or minerals lead to avoidable conditions such as anaemia due to iron
deficiency or blindness due to severe vitamin A deficiency.
Proportion of key food groups recommended for a healthy, well-balanced diet.
Physiology of nutrition
Nutrients in the diet can be classified into ‘macronutrients’,which are eaten in relatively large amounts to provide fuel for energy, and ‘micronutrients’ (e.g. vitamins and minerals), which do not contribute to energy balance but are required in small amounts because they are not synthesised in the body.
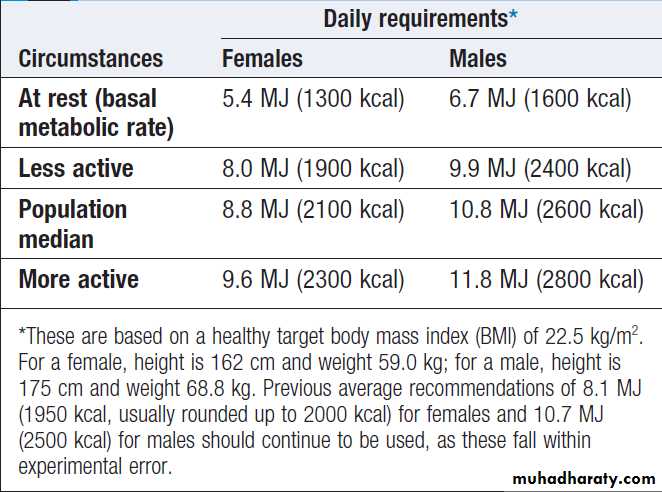
Energy balance
The laws of thermodynamics dictate that energy balanceis achieved when energy intake = energy expenditure.
Energy expenditure has several components. The
basal metabolic rate (BMR) describes the obligatory
energy expenditure required to maintain metabolic
functions in tissues and hence sustain life.
It is most closely predicted by fat-free mass (i.e. total body mass minus fat mass), which is lower in females and older
people . Extra metabolic energy is consumed during growth, pregnancy and lactation, and when febrile. Metabolic energy is also required for thermal
regulation, and expenditure is higher in cold or hot environments. The energy required for digestion of food
(diet-induced thermogenesis (DIT); Fig.) accounts
for approximately 10% of total energy expenditure, with
protein requiring more energy than other macronutrients.
Another component of energy expenditure is governed
by the level of muscular activity, which can vary
considerably with occupation and lifestyle . Physical activity levels are usually defined as multiples of BMR.
Energy intake is determined by the ‘macronutrient’
content of food. Carbohydrates, fat, protein and alcohol
provide fuel for oxidation in the mitochondria to generate
energy (as adenosine triphosphate (ATP). The
energy provided by each of these elements differs:
• carbohydrates (16 kJ/g)
• fat (37 kJ/g)
• protein (17 kJ/g)
• alcohol (29 kJ/g).
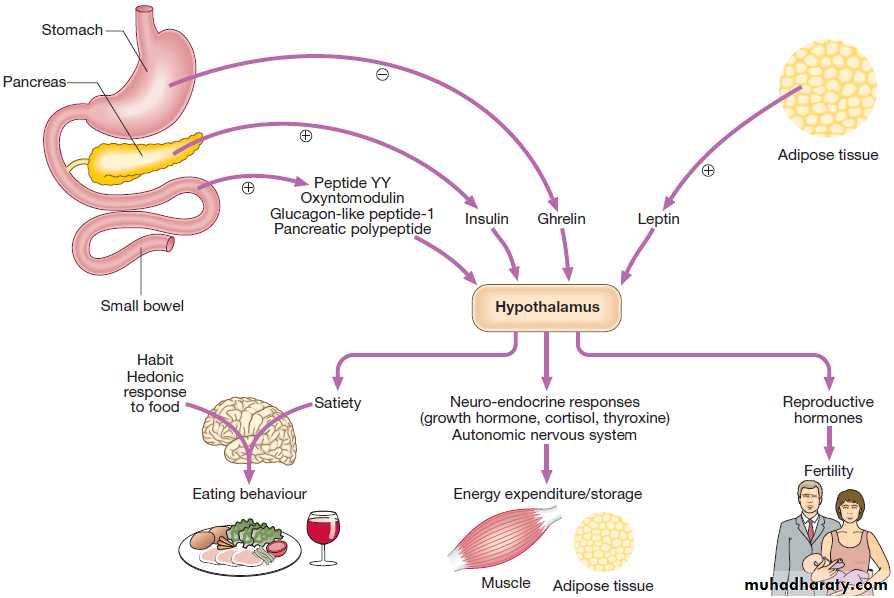
Regulation of energy balance is coordinated in the
hypothalamus, which receives afferent signals that indicate nutritional status in the short term (e.g. the stomach hormone ghrelin, which falls immediately after eating and rises gradually thereafter, to suppress satiety and signal that it is time for the next meal) and the long term (e.g. the adipose hormone leptin, which increases with growing fat mass and may also link fat mass to reproductive function). The hypothalamus responds withchanges in many local neurotransmitters that alter activity
in a number of pathways that influence energy balance including hormones acting on the pituitary gland and neural control circuits that connect with the cerebral cortex and autonomic nervous system.
Regulation of energy balance and its link with reproduction.
+ indicates factors that are stimulated by eating and induce satiety._ indicates factors that are suppressed by eating and inhibit satiety.
Responses to under-and over-nutrition
These complex regulatory pathways allow adaptation to
variations in nutrition. In response to starvation, reproductive function is suppressed, BMR is reduced, and
there are profound psychological effects, including
energy conservation through lethargy. These adjustments
can ‘defend’ body weight within certain limits. However, in the low-insulin state of starvation (see Fig. ), fuels are liberated from stores initially in glycogen (in liver and muscle), then in triglyceride (lipolysis in adipose tissue, with excess free fatty acid supply to the liver leading to ketosis) and finally in protein (proteolysis in muscle).
In response to over-nutrition, BMR is increased, and extra energy is consumed in the work of carrying increased fat stores, so that body weight is again ‘defended’ within certain limits. In the high-insulin state of over-nutrition, excess energy is invested in fatty acids and stored as triglycerides; these are deposited principally in adipose tissue but they may also accumulate in the liver and skeletal muscle. In the absence of hypothalamic function (e.g. in those with craniopharyngioma) or in rare patients with mutations in relevant genes (e.g. in leptin or melanocortin-4 receptors), loss of response to satiety signals, together with loss of adaptive changes in energy expenditure, result in relentless weight gain.
Macronutrients
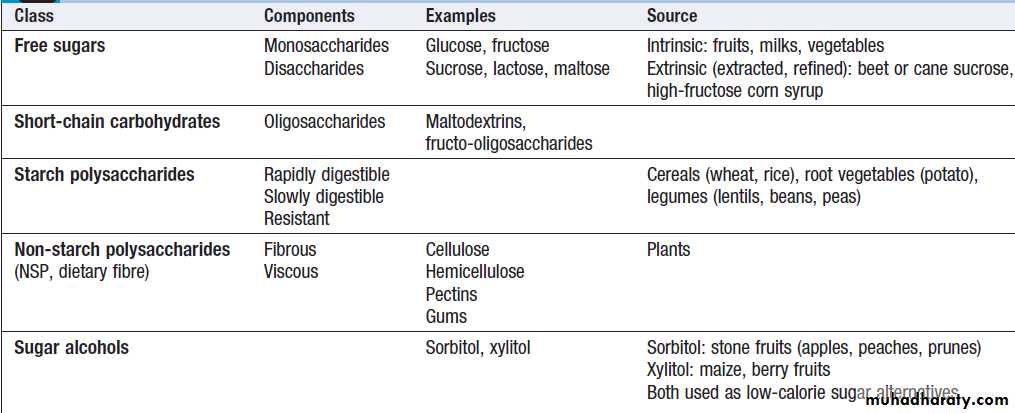
(energy-yielding nutrients)Carbohydrates
Types of carbohydrate and their dietary sources are
listed in Box. The ‘available’ carbohydrates (starches
and sugars) are broken down to monosaccharides before
absorption from the gut and supply over half the energy in a normal, well-balanced diet .
No individual carbohydrate is an essential nutrient, as carbohydrates can be synthesised de novo from glycerol or protein. However, if the carbohydrate intake is less than 100 g per day, increased lipolysis leads to ketosis
Dietary guidelines do not restrict the intake of intrinsic
sugars in fruit and vegetables or the sugars in milk.However, intake of non-milk extrinsic sugars (sucrose,
maltose, fructose), which increase the risk of dental
caries and diabetes mellitus, should be limited. Individuals
who do not produce lactase (‘lactose-intolerant’)
are advised to avoid or limit dairy products and foods
with added lactose. Starches in cereal foods, root foods
and legumes provide the largest proportion of energy
in most diets around the world. All starches are polymers
of glucose, linked by the same 1–4 glycosidic
linkages. However, some starches are digested promptly
by salivary and then pancreatic amylase, producing
rapid delivery of glucose to the blood.
Other starches are digested more slowly, either because they are protected in the structure of the food, because of their crystal structure, or because the molecule is unbranched (amylose).
These differences are the basis for the ‘glycaemic
index’ of foods. This is the area under the curve of
the rise in blood glucose concentration in the 2 hours
following ingestion of 50 g carbohydrate, expressed as a
percentage of the response to 50 g anhydrous glucose.
There is emerging evidence linking high glycaemic
index foods with obesity and type 2 diabetes . Sugar alcohols (e.g. sorbitol) that are used as replacement
sweeteners can cause diarrhoea if eaten in large amounts.
Dietary fibre
Dietary fibre is plant food that is not digested by humanenzymes in the gastrointestinal tract. Most dietary fibre
is known as the ‘non-starch polysaccharides’ (NSP). A small percentage of ‘resistant’ dietary starch may also pass unchanged into the large intestine. Dietary fibre can be broken down by the resident bacteria in the colon to produce short-chain fatty acids.
This is essential fuel for the enterocytes and contributes to bowel health.
The extent of flatus formed is dependent on the food source.
Some types of NSP, notably the hemicellulose of
wheat, increase the water-holding capacity of coloniccontents and the bulk of faeces. They relieve simple
constipation, appear to prevent diverticulosis and may
reduce the risk of cancer of the colon. Other viscous,
indigestible polysaccharides like pectin and guar gum
are important in the upper gastrointestinal tract, where
they slow gastric emptying, contribute to satiety, and
reduce bile salt absorption and hence plasma cholesterol
concentration.
Dietary carbohydrates
FatsFat has the highest energy density of the macronutrients
(37 kJ/g) and excessive consumption may be an insidious
cause of obesity . Free fatty acids are absorbed in chylomicrons, allowing access of complex molecules into the
circulation. The principal polyunsaturated fatty acid (PUFA) in plant seed oils is linoleic acid (18 : 2 ω6). This and alphalinolenic acid (18 : 3 ω3) are the ‘essential’ fatty acids, which humans cannot synthesise de novo. They undergo further desaturation and elongation, to produce, for example, γ-linolenic acid (18 : 3 ω6) and arachidonic acid (20 : 4 ω6). These are precursors of prostaglandins and eicosanoids, and form part of the structure of lipid
membranes in all cells.
Fish oils are rich in ω3 PUFA (e.g. eicosapentaenoic (20 : 5 ω3) and docosahexaenoic (22 : 6 ω3), which promote the anti-inflammatory cascade of prostaglandin production and occur in the lipids of the human brain and retina. They inhibit thrombosis by competitively antagonising thromboxane A2 formation. Substituting saturated fat (i.e. from animal sources:
butter, ghee or lard) with PUFA in the diet can lower the
concentration of circulating LDL cholesterol and may help prevent coronary heart disease.
High intakes of trans fatty acids (TFA) (isomers
of the natural cis fatty acids) reflect the use of oils that
have been partially hydrogenated in the food industry.
It is recommended that TFAs are limited to < 2% of the
dietary fat intake, as they are associated with cardiovascular disease.Changes in industrial practice in the UK and US have meant that TFA intake is now below 1%, with the residual amounts coming from milk as a result of ruminant digestion.
Cholesterol is also absorbed directly from food in
chylomicrons and is an important substrate for steroid
and sterol synthesis,
but not an important source of energy.
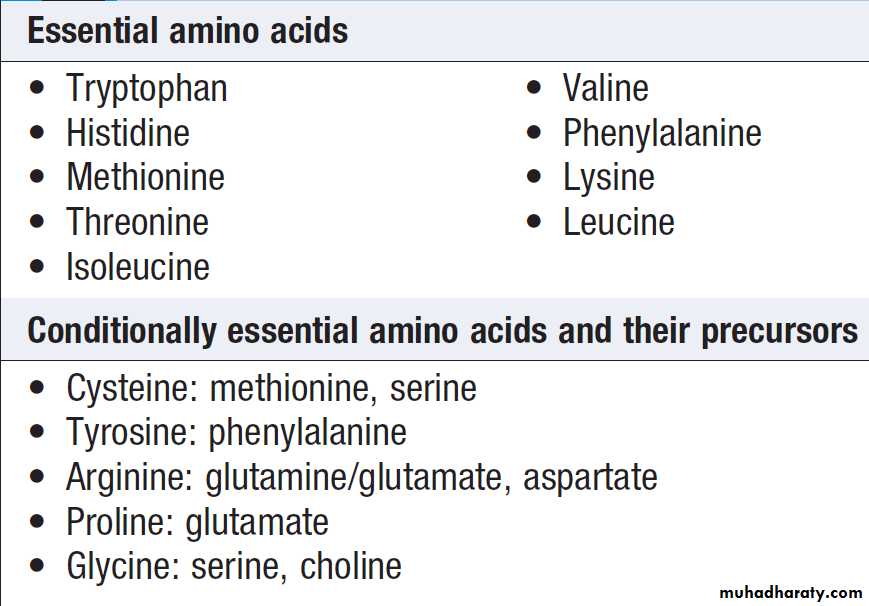
Proteins
Proteins are made up of some 20 different amino acids,
of which nine are ‘essential’ , i.e. they cannot
be synthesised in humans but are required for synthesis
of important proteins.
Another group of five amino acids are termed ‘conditionally essential’, meaning that they can be synthesised from other amino acids, provided there is an adequate dietary supply.
The remaining amino acids can be synthesised in the body by transamination, provided there is a sufficient supply of amino groups.
The nutritive or ‘biological’ value of different proteins
depends on the relative proportions of essentialamino acids they contain.
Proteins of animal origin, particularly from eggs, milk and meat, are generally of higher biological value than proteins of vegetable origin, which are low in one or more of the essential amino acids.
However, when two different vegetable proteins
are eaten together (e.g. a cereal and a legume), their
amino acid contents are complementary and produce an
adequate mix, an important principle in vegan diets.
Amino acids
Dietary recommendations for macronutrients
Recommendations for energy intake and proportions of macronutrients have been calculated to provide a balance of essential nutrients and minimise the risks of excessive refined sugar (dental caries, high glycaemic index/diabetes mellitus), saturated fat or trans fat (obesity, coronary heart disease).
Recommended dietary fibre intake is based on
avoiding risks of colonic disease.
The usual recommended protein intake for a healthy man doing light work is 65–100 g/day.
The minimum requirement is around 40 g of protein with a high proportion of essential amino acids.
Daily adult energy requirements in health
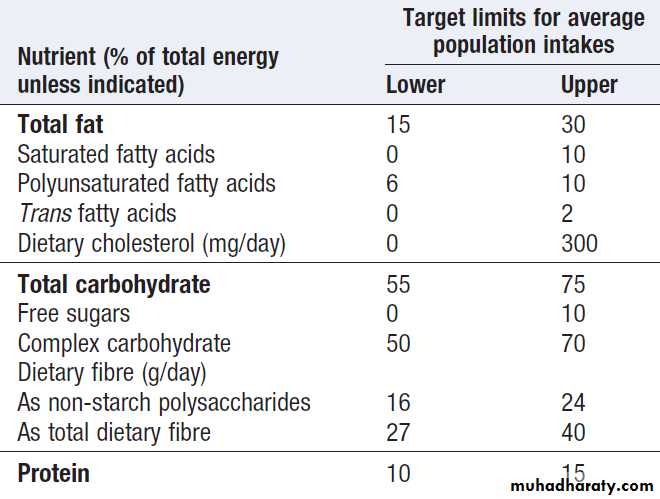
WHO recommended population macronutrient goals
Clinical assessment and investigation of nutritional statusThe diverse manifestations of inadequate nutrition dictate that its clinical assessment and investigation involve many systems. Energy balance is reflected in body composition, which is most readily assessed by clinical anthropometric measurements. It can also be tested non-invasively by the measurement of body fat by bio-impedance or dual energy X-ray absorptiometry (DEXA) scanning. Abnormal micronutrient status is commonly manifest in clinical signs in the skin and mucous membranes, or in other systems.
A dietary history provides useful information, especially
when obtained by a dietitian. A weighed food
diary is considered to be the gold standard dietary
assessment but is rarely conducted in clinical practice.
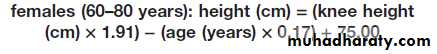
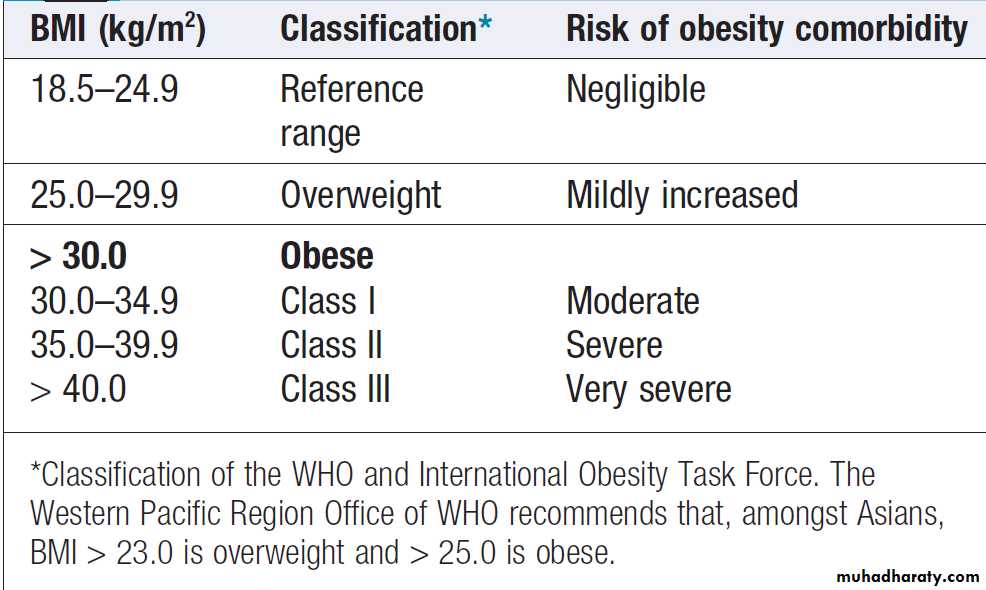
Anthropometric measurements
Body mass index (BMI) is useful for categorising underand
over-nutrition. It is the weight in kilograms divided
by the height in metres, squared. For example, an adult
weighing 70 kg with a height of 1.75 m has a BMI of
70/1.752 = 22.9 kg/m2. If height cannot be determined
(e.g. in older people with kyphosis or in those who
cannot stand), a surrogate measure is:
• the demispan: measured from the sternal notch to the
middle finger; height = 0.73 × (2 × demispan) + 0.43
• knee height:
BMI does not discriminate between fat mass and lean
body mass and can be increased by muscle mass (e.g. inathletes). Moreover, there are ethnic differences in body
fat content; at the same BMI, Asians have more body fat
than Europeans.
For optimal health, the BMI should be 18.5–24.9 kg/m2.
An indication of the degree of abdominal obesity
is the waist circumference, measured at the level of
the umbilicus. Hip circumference can be measured at
the level of the greater trochanters;
waist : hip ratios show whether the distribution of fat is android or gynoid (see below).
Skinfold measurements can be used to calculate body fat content, skinfold thickness over the triceps (using special callipers);
whereas relative loss of muscle and subcutaneous fat can be estimated by measuring mid-arm circumference (at the middle of the humerus) and
muscle mass is estimated by subtracting triceps skinfold thickness from mid-arm circumference.
DISORDERS OF ALTERED ENERGY BALANCE
ObesityObesity is widely regarded as a pandemic, with potentially disastrous consequences for human health.
Over one-quarter of adults in the UK were obese. Moreover, almost two-thirds are overweight (BMI ≥ 25 kg/m2). In developing countries, average national rates of obesity are low.
There is increasing public awareness of the health
implications of obesity. Many patients will seek medical
help for their obesity, others will present with one of the
complications of obesity, and increasing numbers are
being identified during health screening examinations.
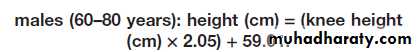
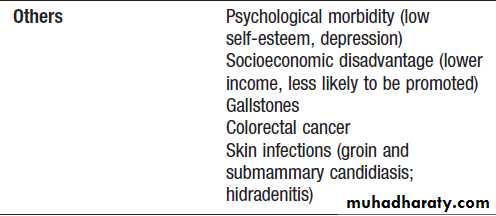
Complications of obesity
Obesity has adverse effects on both mortality and morbidity .Changes in mortality are difficult toanalyse due to the confounding effects of lower body
weight in cigarette smokers and those with other illnesses
(such as cancer). However, it is clear that the
lowest mortality rates are seen in Europeans in the BMI
range 18.5–24 kg/m2 (and at lower BMI in Asians). It is
suggested that obesity at age 40 years can reduce life
expectancy by up to 7 years for non-smokers and by
13 years for smokers. Coronary heart disease is the major cause of death but cancer rates are also increased in the overweight, especially colorectal cancer in males and cancer of the gallbladder, biliary tract, breast, endometrium and cervix in females.
Obesity has little effect on life expectancy above 70 years of age, but the obese do spend a greater proportion of their active life disabled. Epidemic obesity has been accompanied by an epidemic of type 2 diabetes and osteoarthritis, particularly of the knee. Although an increased body size results in greater bone density through
increased mechanical stress, it is not certain whether
this translates to a lower incidence of osteoporotic fractures.
Obesity may have profound psychological
consequences, compounded by stigmatisation of the
obese in many societies.
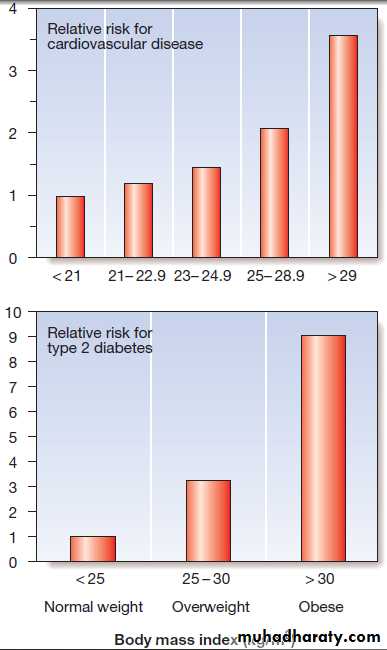
Complications of obesity
Risks of diabetes and cardiovascular disease in
overweight and obese women. Data are from the Nurses’ Health Studyin the USA, mostly of Caucasian women. In some ethnic groups (e.g. South
Asians, Native Americans) and in people with higher waist circumference,
the metabolic complications are even more severe at a given level of BMI.
Body fat distribution
For some complications of obesity, the distribution
rather than the absolute amount of excess adipose tissue
appears to be important. Increased intra-abdominal
fat causes ‘central’ (‘abdominal’, ‘visceral’, ‘android’
or ‘apple-shaped’) obesity, which contrasts with subcutaneous fat accumulation causing ‘generalised’ (‘gynoid’ or ‘pear-shaped’) obesity; the former is more common in men and is more closely associated with type 2
diabetes, the metabolic syndrome and cardiovascular
disease . The key difference between these
depots of fat may lie in their vascular anatomy, with
intra-abdominal fat draining into the portal vein and
thence directly to the liver.
Thus many factors that are released from adipose tissue (including free fatty acids; ‘adipokines’, such as tumour necrosis factor-α, adiponectin and resistin; and steroid hormones) may be at higher concentration in the liver and hence induce insulin resistance and promote type 2 diabetes .
Recent research has also highlighted the importance
of fat deposition within specific organs, especially the liver, as an important determinant of metabolic risk in the obese.
Aetiology
Accumulation of fat results from a discrepancy betweenenergy consumption and energy expenditure that is too
large to be defended by the hypothalamic regulation of
BMR. A continuous small daily positive energy balance
of only 0.2–0.8 MJ (50–200 kcal; < 10% of intake) would
lead to weight gain of 2–20 kg over a period of 4–10
years. Given the cumulative effects of subtle energy
excess, body fat content shows ‘tracking’ with age such
that obese children usually become obese adults.
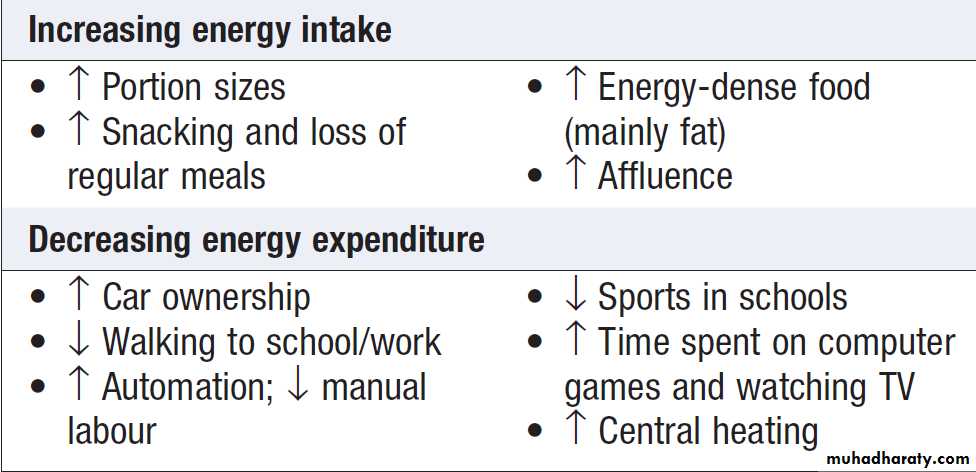
The pandemic of obesity reflects changes in both
energy intake and energy expenditure , although both are difficult to measure reliably.
In the US, the average daily energy intake of men reportedly rose from 10.2 MJ (2450 kcal) in 1971 to 11.0 MJ (2618 kcal) in 2000. Portion sizes, particularly of energy-dense foods such as drinks with highly refined sugar content and salty snacks, have increased.
Obesity is correlated positively with the number
of hours spent watching television, and inversely with
levels of physical activity (e.g. stair climbing). It is
suggested that minor activities such as fidgeting and
chewing gum may contribute to energy expenditure and
protect against obesity.
Susceptibility to obesity
It is not true that obese subjects have a ‘slow metabolism’, since their BMR is higher than that of lean subjects. Twin and adoption studies confirm a genetic influence on obesity. The pattern of inheritance suggests a polygenic disorder, with small contributions from a number of different genes, together accounting for 25–70% of variation in weight, some of which encode proteins known to be involved in the control of appetite or metabolism andsome of which have unknown function.
However, these genes account for less than 5% of the variation in body weight.
A few rare single-gene disorders have been identified that lead to severe childhood obesity. These include mutations of the melanocortin-4 receptor (MC4R), and mutations in the leptin gene . The latter can be treated by leptin injections. Additional genetic conditions in which obesity is a feature include the Prader– Willi and Lawrence–Moon–Biedl syndromes.
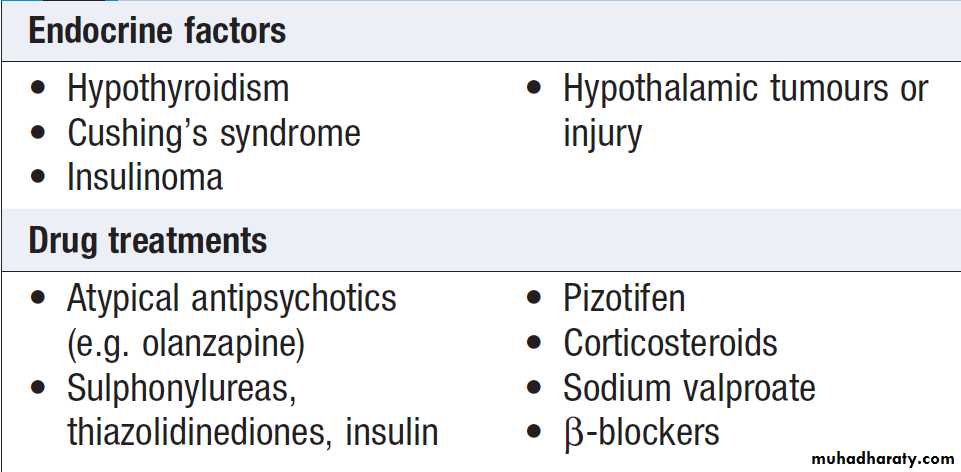
Reversible causes of obesity and weight gain
In a small minority of patients presenting with obesity,
specific causal factors can be identified and treated.
These patients are distinguished from those with idiopathic obesity by their short history, with a recent marked change in the trajectory of their adult weight gain.
Some reasons for the increasing prevalence of obesity – the ‘obesogenic’ environment
Clinical assessment and investigations
In assessing an individual presenting with obesity, theaims are to:
• quantify the problem
• exclude an underlying cause
• identify complications
• reach a management plan.
Severity of obesity can be quantified using the BMI.
A waist circumference of > 102 cm in men or > 88 cm in women indicates that the risk of metabolic and cardiovascular complications of obesity is high.
A dietary history may be helpful in guiding dietary
advice, but is notoriously susceptible to under-reporting
of food consumption.
It is important to consider ‘pathological’ eating behaviour (such as binge eating, nocturnal eating or bulimia), which may be the most important issue to address in some patients. Alcohol is an important source of energy intake and should be considered in detail.
A patient who has recently gained substantial weight or has gained weight at a faster rate than previously, and is not taking relevant drugs, is more likely to have an underlying disorder such as hypothyroidism or Cushing’s syndrome.
All obese patients should have thyroid function tests performed on one occasion, and an overnight
dexamethasone suppression test or 24-hour urine free
cortisol if Cushing’s syndrome is suspected.
The impact of obesity on the patient’s life and work is a major consideration.
Assessment of other cardiovascular risk factors is
important. Blood pressure should be measured with
a large cuff, if required . Associated type 2 diabetes and dyslipidaemia are detected by measuring blood glucose or HbA1c and a serum lipid profile, ideally in a fasting morning sample. Elevated serum transaminases occur in patients with non-alcoholic fatty liver disease.
Potentially reversible causes of weight gain
Quantifying obesity with body mass index
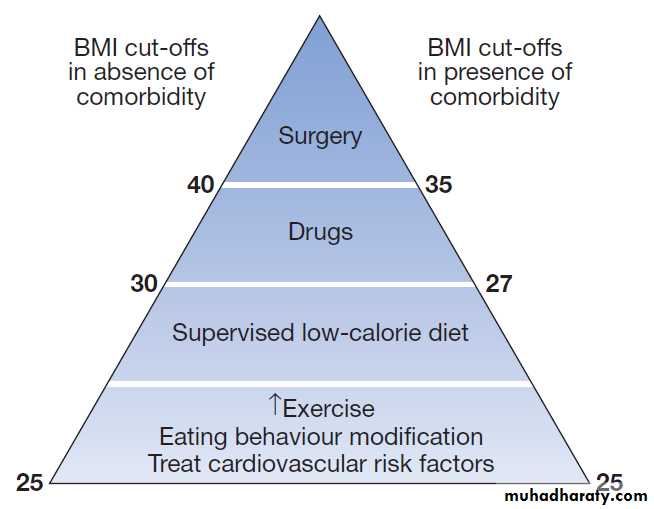
(weight/height2)Management
The health risks of obesity are largely reversible. Interventions proven to reduce weight in obese patients also ameliorate cardiovascular risk factors. Lifestyle advicethat lowers body weight and increases physical exercise
reduces the incidence of type 2 diabetes . Given the high prevalence of obesity and the large magnitude of its risks, population strategies to prevent and reverse obesity are high on the public health priority list for many countries. Unfortunately, ‘low-fat’ foods are often still energy-dense, and current lifestyles with labour saving devices, sedentary work and passive leisure activities have much lower energy requirements than the manual labour and household duties of previous generations.
Most patients seeking assistance with obesity are
motivated to lose weight but have attempted to do so
previously without long-term success. Often weight will
have oscillated between periods of successful weight
loss and then regain of weight (‘recidivism’).
A reasonable goal for most patients is to lose 5–10%
of body weight.
An empathetic explanation of energy balance, which
recognises that some individuals are more susceptible to
obesity than others and may find it more difficult to lose
and sustain body weight loss, is important.
Exclusion of underlying ‘hormone imbalance’ with simple tests is reassuring and shifts the focus on to consideration of energy balance.
The management plan will vary according to the
severity of the obesity and the associatedrisk factors and complications. It will also be influenced
by availability of resources; health-care providers and
regulators have generally been careful not to recommend
expensive interventions (especially long-term
drug therapy and surgery) for everyone who is overweight. Lifestyle advice
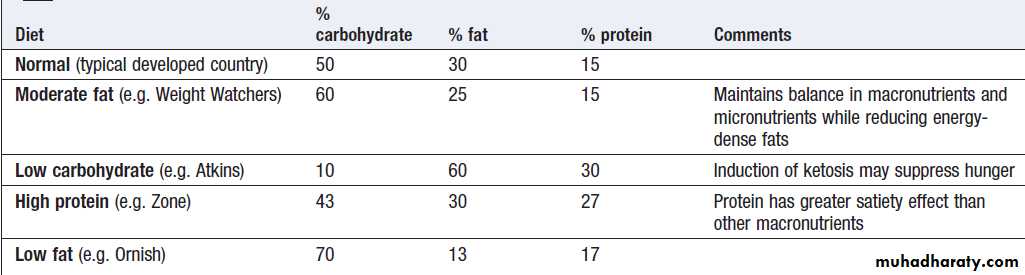
Behavioural modification to avoid some of the effects of
the ‘obesogenic’ environment is the cornerstone of long-term control of weight. Regular eating patterns and maximising physical activity are advised, with reference to the modest extra activity required to increase physical activity level (PAL) ratios .
Fig. Therapeutic options for obesity. Relevant comorbidities include type 2 diabetes, hypertension, cardiovascular disease, sleep apnoea, and waist circumference > 102 cm in men or 88 cm in women. This is an approximate consensus of the numerous national guidelines, which vary slightly in their recommendations and are revised every few years.
Where possible, this should be incorporated in the daily routine (e.g. walking rather than driving to work), since this is more likely to be sustained.
Alternative exercise (e.g. swimming) may be considered if musculoskeletal complications prevent walking. Changes in eating behaviour (including food selection, portion size control, avoidance of snacking,
regular meals to encourage satiety, and substitution of
sugar with artificial sweeteners) should be discussed.
Regular support from a dietitian or attendance at a
weight loss group may be helpful.
Weight loss diets
In overweight people, adherence to the lifestyle advicegiven above may gradually induce weight loss. Most involve recommending a reduction of daily total energy intake of −2.5 MJ (600 kcal) from the patient’s normal consumption.
Vitamin supplementation is wise in those diets in which macronutrient balance is markedly disturbed. In some patients, more rapid weight loss is required,
e.g. in preparation for surgery. There is no role for starvation diets, which risk profound loss of muscle mass and the development of arrhythmias (and even sudden death) secondary to elevated free fatty acids, ketosis and deranged electrolytes.
Very-low-calorie diets (VLCDs) are recommended for short-term rapid weight loss, producing losses of 1.5–2.5 kg/week, compared to 0.5 kg/week on conventional regimens, but require the supervision of an experienced physician and nutritionist.
The composition of the diet should ensure a minimum
of 50 g of protein each day for men and 40 g for women
to minimise muscle degradation. Energy content should be a minimum of 1.65 MJ (400 kcal) for women of height < 1.73 m, and 2.1 MJ (500 kcal) for all men and for women taller than 1.73 m. Side-effects are a problem in the early stages and include orthostatic hypotension, headache, diarrhoea and nausea.
Low-calorie diet therapy for obesity
DrugsA huge investment has been made by the pharmaceutical
industry in finding drugs for obesity. The side-effect
profile has limited the use of many agents, with notable
withdrawals from clinical use of sibutramine (increased
cardiovascular events) and rimonabant (psychiatric
side-effects) in recent years; only one drug, orlistat, is
currently licensed for long-term use. A number of other
agents are in development, so the situation could change
rapidly over the next few years.
There is no role for diuretics, or for thyroxine therapy without biochemical evidence of hypothyroidism.
Orlistat inhibits pancreatic and gastric lipases and
thereby decreases the hydrolysis of ingested triglycerides,reducing dietary fat absorption by approximately
30%. The drug is not absorbed and adverse side-effects
relate to the effect of the resultant fat malabsorption
on the gut: namely, loose stools, oily spotting, faecal urgency, flatus and the potential for malabsorption of
fat-soluble vitamins. Orlistat is taken with each of the
three main meals of the day and the dose can be adjusted
(60–120 mg) to minimise side-effects. Its efficacy is
shown in Figure; these effects may be explained because patients taking orlistat adhere better to low-fat diets in order to avoid unpleasant gastrointestinal side-effects.
Drug therapy is usually reserved for patients with
high risk of complications from obesity (see Fig.),
and its optimum timing and duration are controversial.
Although life-long therapy is advocated for many drugs
that reduce risk on the basis of relatively short-term
research trials (e.g. drugs for hypertension and osteoporosis), some patients who continue to take anti-obesity drugs tend to regain weight with time; this may partly reflect age-related weight gain, but significant weight gain should prompt reinforcement of lifestyle advice and, if this is unsuccessful, drug therapy should be discontinued.
Surgery
‘Bariatric’ surgery is by far the most effective long-termtreatment for obesity (see Fig. and Box) and is the only anti-obesity intervention that has been associated
with reduced mortality. Bariatric surgery should be
contemplated in motivated patients who have very high
risks of complications of obesity , in whom extensive dietary and drug therapy has been insufficiently
effective. It is usually reserved for those with severe obesity (BMI > 40 kg/m2), or those with a BMI > 35 kg/m2 and significant complications, such as type 2 diabetes or obstructive sleep apnoea. Only experienced
specialist surgeons should undertake these procedures,
in collaboration with a multidisciplinary team.
Several approaches are used and all can be performed laparoscopically. The mechanism of weight loss may not simply relate to limiting the stomach or absorptive capacity, but rather in disrupting the release of ghrelin
from the stomach or promoting the release of other peptides from the small bowel, thereby enhancing satiety
signalling in the hypothalamus.
Diabetes may improve rapidly after surgery, particularly after gastric bypass, and although this may be attributed to severe energy restriction in the perioperative period, it is possible that increased release of incretin hormones such as glucagon-like peptide (GLP)-1 may contribute to the improvement in glucose control.
Complications depend upon the approach. Mortality is low in experienced centres, but post-operative respiratory problems, wound infection and dehiscence, staple leaks, stomal stenosis, marginal ulcers and venous thrombosis may occur. Additional problems may arise at a later stage, such as pouch and distal oesophageal dilatation, persistent vomiting, ‘dumping’ and micronutrient deficiencies, particularly of folate, vitamin B12 and iron, which are of concern especially to women contemplating pregnancy.
Cosmetic surgical procedures may be considered in obese patients after successful weight loss.
Apronectomy is usually advocated to remove an overhang of abdominal skin, especially if infected or ulcerated. This
operation is of no value for long-term weight reduction
if food intake remains unrestricted.
Treatment of additional risk factors
Obesity must not be treated in isolation and other risk
factors must be addressed, including smoking, excess
alcohol consumption, diabetes mellitus, hyperlipidaemia,
hypertension and obstructive sleep apnoea.
Effects of orlistat and bariatric surgery on weight loss. Each obese subject undergoing surgery was matched with a control subject whose obesity was ‘treated’ by standard non-operative interventions. The maximum weight loss achieved with orlistat was approximately 11 %; surgery achieves much more substantial and prolonged weight loss.
Effectiveness and adverse effects of
laparoscopic bariatric surgical proceduresBariatric surgical procedures. A Laparoscopic banding, with the option of a reservoir band and subcutaneous access to restrict the
stomach further after compensatory expansion has occurred. B Sleeve gastrectomy. C Roux-en-Y gastric bypass. D Biliopancreatic diversion with duodenal switch.
Under-nutrition
Starvation and famineThere remain regions of the world, particularly rural
Africa, where under-nutrition due to famine is endemic,
the prevalence of BMI < 18.5 kg/m2 in adults is as high as 20%, and growth retardation due to undernutrition affects 50% of children. WHO reports that chronic under-nutrition is responsible for more than half of all childhood deaths worldwide. Starvation is manifest as marasmus (malnutrition
with marked muscle-wasting), or, when additional complicating mechanisms, such as oxidative stress, come
into play, malnourished children can develop kwashiorkor
(malnutrition with oedema).
Growth retardation is due to deficiency of key nutrients, e.g. protein, zinc, potassium, phosphorus and sulphur. Treatment of these childhood conditions is not discussed in this adult medicine textbook.
In adults, starvation is the result of chronic undernutrition,
i.e. sustained negative energy (calorie) balance.
Causes are shown in Box.
Classification of under-nutrition in adults by
body mass index (weight/height2)Causes of under-nutrition and weight loss in adults
Clinical assessmentIn starvation, the severity of malnutrition can be assessed
by anthropometric measurements, such as BMI . Demispan and mid-arm circumference measurements are most useful in monitoring progress during treatment.
The clinical features of severe undernutrition in adults include:
• weight loss
• thirst, craving for food, weakness and feeling cold
• nocturia, amenorrhoea or impotence
• lax, pale, dry skin with loss of turgor and,
occasionally, pigmented patches
• cold and cyanosed extremities, pressure sores
• hair thinning or loss (except in adolescents)
• muscle-wasting, best demonstrated by the loss of
the temporalis and periscapular muscles and
reduced mid-arm circumference
• loss of subcutaneous fat, reflected in reduced
skinfold thickness and mid-arm circumference
• hypothermia, bradycardia, hypotension and small heart
• oedema, which may be present without
hypoalbuminaemia (‘famine oedema’)
• distended abdomen with diarrhoea
• diminished tendon jerks
• apathy, loss of initiative, depression, introversion,
aggression if food is nearby
• susceptibility to infections
Under-nutrition often leads to vitamin deficiencies,
especially of thiamin, folate and vitamin C. Diarrhoea can lead to depletion of sodium, potassium and magnesium. The high mortality rate in famine situations is often due to outbreaks of infection, e.g. typhus or cholera, but the usual signs of infection may not be apparent. In advanced starvation, patients become completely inactive and may assume a flexed, fetal position.In the last stage of starvation, death comes quietly
and often quite suddenly. The very old are most vulnerable.
All organs are atrophied at necropsy, except the
brain, which tends to maintain its weight.
Infections associated with starvation
InvestigationsPlasma free fatty acids are increased and there is ketosis and a mild metabolic acidosis. Glucose is low but albumin concentration is often maintained because the liver still functions normally. Insulin secretion is diminished, glucagon and cortisol tend to increase, and reverse T3 replaces normal triiodothyronine .The resting metabolic rate falls, partly because of reduced lean body mass and partly because of hypothalamic compensation .The urine has a fixed specific gravity and creatinine excretion low. There may be mild anaemia, thrombocytopenia, leucopenia and ESR is normal. Tests of delayed skin hypersensitivity, e.g. to tuberculin, are falsely negative. The ECG shows sinus bradycardia and low voltage.
Management
Whether in a famine or in wasting secondary to disease,the severity of under-nutrition is graded according to
BMI . People with mild starvation are in no danger; those with moderate starvation need extra feeding; those who are severely underweight need hospital care. In severe starvation, there is atrophy of the intestinal epithelium and of the exocrine pancreas, and the bile is dilute. When food becomes available, it should be given by mouth in small, frequent amounts at first, using a suitable formula preparation . Individual energy requirements can vary by 30%. During rehabilitation, more concentrated formula can be given with additional food that is palatable and similar to the usual staple meal.
Salt should be restricted and micronutrient supplements may be essential (e.g. potassium, magnesium, zinc and multivitamins). Between 6.3 and 8.4 MJ/day (1500–2000 kcal/day) will arrest progressive under-nutrition, but additional energy may be required for regain of weight. During refeeding, a weight gain of 5% body weight per month indicates satisfactory progress. Other care is supportive, and includes attention to the skin, adequate hydration, treatment of infections, and careful monitoring of body temperature since thermoregulation may be impaired. Lastly, plans must be made for the
future for prevention and/or earlier intervention if
similar circumstances prevail.
WHO recommended diets for refeeding
Under-nutrition in hospital
Under-nutrition is a common problem in the hospitalsetting. The elderly are particularly at risk (Box).
Once in hospital, many patients lose weight due to
factors such as poor appetite, poor dental health, concurrent illness and even being kept ‘nil by mouth’ for
investigations. Under-nutrition is poorly recognised in
hospital and has serious consequences. Physical effects include impaired immunity and muscle weakness,
which in turn affect cardiac and respiratory function,
and delayed wound healing after surgery with increased
risks of post-operative infection.
The undernourished patient is often apathetic and withdrawn, which may be mistaken for a depressive illness and can affect cooperation with treatment and rehabilitation.
This can be averted with proper monitoring and
involvement of an appropriate multidisciplinary team.
As a minimum standard, all patients should be weighed
on admission to hospital and at least weekly until discharge.
A scoring system for identifying patients at nutritional risk is shown in Figure.
Nutritional support of the hospital patient
Normal dietAs a first step, patients should be encouraged to eat a
normal and adequate diet. In patients at risk of under-nutrition (see Fig.),quantities eaten should be recorded on a food chart.
Hospital staff must identify and overcome barriers to
adequate food intake, such as unpalatability of food,
cultural and religious factors influencing acceptability of
food, difficulty with hand dexterity (arthritis, stroke),
immobility in bed, or poor oral health
Dietary supplements
If sufficient nutritional intake cannot be achieved from normal diet alone, then dietary supplements should be used. These are drinks with high energy and protein content, and are available in cartons as manufactured, flavoured products or are made in the hospital kitchen from milk products and egg. They should be prescribed, and administered by nursing staff, to ensure that they are taken regularly. Dietary supplements do not significantly affect the patient’s consumption of normal food.
Enteral tube feeding
Patients who are unable to swallow may require artificialnutritional support: for example, after acute stroke
or throat surgery, or when there are long-term neurological
problems such as motor neuron disease and multiple
sclerosis. The enteral route should always be used
if possible, since feeding via the gastrointestinal tract
preserves the integrity of the mucosal barrier. This prevents bacteraemia and, in intensive care patients, reduces the risk of multi-organ failure .
If the need for artificial nutritional support is thought to be, short-term then feeding is instituted using a finebore nasogastric tube.
The position of the tube in the stomach must be confirmed before any fluid is administered, as severe respiratory complications can occur if fluid is inadvertently infused into a bronchus . Thereafter, specially prepared liquid feeds are administered either by continuous infusion or using a
bolus technique. If the patient fails to absorb the administered feed or vomits it, this may indicate gastric outlet obstruction or gastric stasis, which can be overcome by placing a nasojejunal tube.
If long-term artificial enteral feeding is needed, a percutaneous endoscopic gastrostomy (PEG) should be
sited (Fig.). A PEG tube is more comfortable for the
patient, since there is no irritation to the nasal mucosa.
The tube is less likely to become displaced or to be
pulled out, so the feed can be given more reliably.However, inserting a gastrostomy is an invasive procedure,
especially in frail patients with significant comorbidities.
It may be complicated by local infection (30%)
and inadvertent puncture of other intra-abdominal
organs, causing peritonitis and bleeding, so the indication
for placement must be carefully considered. It takes
approximately 10 days for a fibrous tract to form around
the PEG tube. If the PEG is displaced or removed during
that time, there is a high risk of peritonitis. If a problem
occurs with food absorption, a jejunal extension can be
placed through the PEG tube and liquid feed administered
directly into the small bowel.
Parenteral nutrition
IV feeding should only be used when enteral feeding is impossible. Parenteral feeding is expensive and carries higher risks of complications. There is little benefit if parenteral feeding is required for less than 1 week.
There are a number of possible routes for parenteral
nutrition:
• Peripheral venous cannula. This can only be used for
low-osmolality solutions due to the development of
thrombophlebitis, and is unsuitable for patients with high nutritional requirements.
• Peripherally inserted cannula (PIC). A 20 cm cannula is placed in a mid-arm vein. Once again, hyperosmolar solutions cannot be used.
• Peripherally inserted central catheter (PICC). A 60 cm
cannula is inserted into a vein in the antecubitalfossa. The distal end lies in a central vein, allowing
hyperosmolar solutions to be used.
• Central line. The subclavian route is preferred to the
internal jugular vein, due to lower infection rates.
Hyperosmolar solutions can be used without
difficulty. Lines need to be handled with strict
aseptic technique, and a single-lumen tube is
preferred, to prevent infection. If access has been gained to a central vein, nutritional support is usually given as an ‘all-in-one’ mixture. The main energy source is provided by carbohydrate, usually as glucose.
The solution also contains amino acids, lipid emulsion, electrolytes, trace elements and vitamins. These are mixed as a large bag in a sterile environment, with the constituents adjusted according to the results of regular blood monitoring.
Relevant tests include:
• daily: urea and electrolytes, glucose
• twice weekly: liver function tests, calcium,
phosphate, magnesium
• weekly: full blood count, zinc, triglycerides
• monthly: copper, selenium, manganese. If the patient develops fever or other features of septicaemia, it should be assumed to be due to a line infection .Blood cultures should be taken, the existing line removed, the tip sent for bacteriological analysis, and a new line inserted.
Refeeding syndrome
When nutritional support is given to an under-nourished
patient, there is a rapid conversion from a catabolic to
an anabolic state. Administration of carbohydrates
stimulates release of insulin, leading to cellular uptake
of phosphate, potassium and magnesium, which may
provoke significant falls in serum levels. The resulting
electrolyte imbalance can have serious consequences,
such as cardiac arrhythmias, so careful monitoring is
essential. In patients who are thiamin-deficient, Wernicke’s
encephalopathy can be precipitated by refeeding
with carbohydrates , this is prevented by administering thiamin before starting nutritional support.
Legal and ethical aspects of artificial nutritional support
The ability to intervene with artificial nutritional supportraises many legal and ethical dilemmas .
Starvation will inevitably lead to death, but inability to
eat may be part of the terminal stages of a disease
process. Difficult decisions are raised by situations such
as strokes, which affect swallowing. The instigation of
feeding may speed recovery and lead to better functional
outcome; on the other hand, feeding might prolong the process of dying in severe stroke. There will be different approaches to these decisions, depending on the local availability of resources as well as legal, cultural and religious influences. Some guidelines are given in Box.
Screening hospitalised patients for risk of malnutrition.
Acute illnesses include decompensated liver disease, cancer cachexia or being kept ‘nil by mouth’.Energy balance in old age
Fig. Percutaneous endoscopic gastrostomy (PEG) placement.
A Finger pressure on the anterior abdominal wall is noted by theendoscopist.
B Following insertion of a cannula through the anterior abdominal wall into the stomach, a guidewire is threaded through the cannula and grasped by the endoscopic forceps or snare.
C The endoscope is withdrawn with the guidewire. The gastrostomy tube is then attached to the guidewire.
D The guidewire and tube are pulled back through the mouth, oesophagus and stomach to exit on the anterior abdominal wall, and the endoscope is repassed to confirm the site of placement of the retention device. The latter closely abuts the gastric mucosa; its position is maintained by an external fixation device (see inset). It is also possible to place PEG tubes using fluoroscopic guidance in patients in whom endoscopy is difficult (radiologically inserted gastrostomy (RIG)).
Ethical and legal considerations in the
management of artificial nutritional support*Cachexia
Cachexia is the weight loss and muscle-wasting associated with chronic illness, which is characteristic ofchronic infections such as HIV-AIDS, end-stage organ failure and certain cancers (especially of the lung and
upper gastrointestinal tract). Although there is decreased
energy intake with loss of appetite, the main cause is
thought to be increased metabolic rate through the production of key cytokines and other proteolytic factors.
MICRONUTRIENTS, MINERALS AND THEIR DISEASES
VitaminsVitamins are organic substances with key roles in certain
metabolic pathways, and are categorised into those that
are fat-soluble (vitamins A, D, E and K) and those that
are water-soluble (vitamins of the B complex group and
vitamin C). Recommended daily intakes of micronutrients (Box ) vary between countries. Additional amounts of some micronutrients may be required in pregnancy and lactation.
Vitamin deficiency diseases are most prevalent
in developing countries but still occur in developed countries. Older people (and alcoholics) are at risk of
deficiencies in B vitamins and in vitamins D and C.
Summary of clinically important vitamins
Darker-skinned individuals living at higher latitude, and those who cover up or do not go outside are at increased risk of vitamin D deficiency due to inadequate sunlight exposure. Deficiencies of fat-soluble vitamins are seen in conditions of fat malabsorption .Some vitamins also have pharmacological actions when given at supraphysiological doses, e.g. the use of vitamin A for acne. Taking vitamin supplements is fashionable in many countries, although there is no evidence of benefit.Toxic effects are most serious with high dosages of vitamins A, B6 and D. Investigation of vitamin deficiency or excess may involve biochemical assessment of body stores . However, measurements in blood should be interpreted carefully in conjunction with the clinical presentation.
Nutrition in pregnancy and lactation
• Energy requirements: increased in mother and fetus.• Micronutrient requirements: adaptive mechanisms ensure increased uptake of minerals in pregnancy, but extra increments of some are required during lactation. Additional increments of some vitamins are recommended during pregnancy and lactation:
— Vitamin A: for growth and maintenance of the fetus, and toprovide some reserve (important in some countries to prevent blindness associated with vitamin A deficiency).Teratogenic in excessive amounts.
— Vitamin D: to ensure bone and dental development in the infant. Higher incidences of hypocalcaemia,
hypoparathyroidisim and defective dental enamel have been seen in infants of women not taking vitamin D
supplements at > 50° latitude.
— Folate: to avoid neural tube defects .
— Vitamin B12: in lactation only.— Thiamin: to meet increased fetal energy demands.
— Riboflavin: to meet extra demands.
— Niacin: in lactation only.
— Vitamin C: for the last trimester to maintain maternal
stores as fetal demands increase.
— Iodine: in countries with high consumption of staple foods (e.g. brassicas, maize, bamboo shoots) that contain
goitrogens (thiocyanates or perchlorates) that interfere with iodine uptake, supplements prevent infants being born with cretinism.
Periconceptual folate supplementation and neural tube defects
Biochemical assessment of vitamin status
Fat-soluble vitaminsVitamin A (retinol)
Pre-formed retinol is found only in foods of animal origin. Vitamin A can also be derived from carotenes, which are present in green and coloured vegetables and some fruits. Carotenes provide most of the total vitamin A in the UK, and constitute the only supply in vegans. Retinol is converted to several other important molecules:
• 11-cis retinaldehyde is part of the photoreceptor
complex in rods of the retina.
• Retinoic acid induces differentiation of epithelial cells by binding to specific nuclear receptors, which induce responsive genes. In vitamin A deficiency, mucus-secreting cells are replaced by keratinproducing cells.
• Retinoids are necessary for normal growth, fetal
development, fertility, haematopoiesis and immunefunction. Globally, the most important consequence of
vitamin A deficiency is irreversible blindness in young
children. Adults are not usually at risk because liver stores can supply vitamin A when foods containing vitamin A are unavailable. Early deficiency causes impaired adaptation to the dark (night blindness). Keratinisation of the cornea
(xerophthalmia) gives rise to characteristic Bitot’s spots,
and progresses to keratomalacia, with corneal ulceration,
scarring and irreversible blindness . In countries where vitamin A deficiency is endemic, pregnant women should be advised to eat dark-green, leafy vegetables and yellow fruits (to build up stores of retinol in the fetal liver), and infants should be fed the same.
WHO is according high priority to prevention in communities where xerophthalmia occurs, giving single prophylactic oral doses of 60 mg retinyl palmitate (providing 200 000 U retinol) to pre-school children. This also reduces mortality from gastroenteritis and respiratory infections.
Repeated moderate or high doses of retinol can cause
liver damage, hyperostosis and teratogenicity. Women
in countries where deficiency is not endemic are therefore advised not to take vitamin A supplements in pregnancy.Retinol intake may also be restricted in those at
risk of osteoporosis. Acute overdose leads to nausea and
headache, increased intracranial pressure and skin desquamation. Excessive intake of carotene can cause pigmentation of the skin (hypercarotenosis); this gradually
fades when intake is reduced.
Eye signs of vitamin A deficiency.
A Bitot’s spots in xerophthalmia, showing the white triangular plaques (arrows).B Keratomalacia in a 14-month-old child. There is liquefactive necrosis
affecting the greater part of the cornea, with typical sparing of the superior aspect.
Vitamin D
The natural form of vitamin D, cholecalciferol or vitaminD3, is formed in the skin by the action of UV light on
7-dehydrocholesterol, a metabolite of cholesterol. Few
foods contain vitamin D naturally and skin exposure to
sunlight is the main source. Moving away from the
equator, the intensity of UV light decreases, so that at
a latitude above 50° (including northern Europe), vitamin D is not synthesised in winter, and even above 30° there is seasonal variation. The body store accumulated during the summer is consumed during the winter. Vitamin D is converted in the liver to 25-hydroxy vitamin D (25(OH)D), which is further hydroxylated in the kidneys to 1,25-dihydroxy-vitamin D (1,25 (OH)2D), the active form .
1,25(OH)2D activates specific intracellular receptors which influence calcium metabolism, bone mineralization and tissue differentiation. The synthetic form, ergocalciferol, or vitamin D2, is considered to be less potent than the endogenous D3.
There is increasing evidence that vitamin D is important for immune and muscle function, and may reduce falls in the elderly. Margarines are fortified with vitamin D in the UK, and milk is fortified in some parts of Europe and in North America. An analogue of vitamin D (calcipotriol) is used for
treatment of skin conditions such as psoriasis. Excessive
doses of cholecalciferol, ergocalciferol or the hydroxylated
metabolites cause hypercalcaemia.
Vitamin E
There are eight related fat-soluble substances withvitamin E activity. The most important dietary form is α-tocopherol.
Vitamin E has many direct metabolic actions:
• It prevents oxidation of polyunsaturated fatty acids
in cell membranes by free radicals.
• It helps maintain cell membrane structure.
• It affects DNA synthesis and cell signalling.
• Involved in the anti-inflammatory and immune systems.
Human deficiency is rare and has only been described
in premature infants and in malabsorption. It cancause a mild haemolytic anaemia, ataxia and visual
scotomas. Vitamin E intakes are considered safe up to
3200 mg/day (1000-fold greater than recommended
intakes). Diets rich in vitamin E are consumed in countries with lower rates of coronary heart disease. However, randomised controlled trials have not demonstrated cardioprotective effects of vitamin E or other antioxidants.
Vitamin K
Vitamin K is supplied in the diet mainly as vitamin K1
(phylloquinone) in the UK, or as vitamin K2 (menaquinone)
from fermented products in parts of Asia. Vitamin
K2 is also synthesised by bacteria in the colon. Vitamin
K is a co-factor for carboxylation reactions: in particular,
the production of γ-carboxyglutamate (gla). Gla residues are found in four of the coagulation factor proteins (II, VII, IX and X), conferring their capacity to bind to phospholipid surfaces in the presence of calcium. Other important gla proteins are osteocalcin and matrix gla protein, which are important in bone mineralisation.
Vitamin K deficiency leads to delayed coagulation
and bleeding. In obstructive jaundice, dietary vitamin Kis not absorbed and it is essential to administer the
vitamin in parenteral form before surgery. Warfarin and
related anticoagulants act by antagonising
vitamin K. Vitamin K is given routinely to newborn
babies to prevent haemorrhagic disease. Symptoms of
excess have been reported only in infants, with synthetic
preparations linked to haemolysis and liver damage.
Water-soluble vitamins
Thiamin (vitamin B1 )Thiamin is widely distributed in foods of both vegetable
and animal origin. Thiamin pyrophosphate (TPP) is
a co-factor for enzyme reactions involved in the metabolism of macronutrients (carbohydrate, fat and
alcohol), including:
• decarboxylation of pyruvate to acetyl-co-enzyme A,
which bridges between glycolysis and the
tricarboxylic acid (Krebs) cycle
• transketolase activity in the hexose monophosphate
shunt pathway
• decarboxylation of α-ketoglutarate to succinate in
the Krebs cycle.
In thiamin deficiency, cells cannot metabolise glucose
aerobically to generate energy as ATP. Neuronal cells
are most vulnerable, since they depend almost exclusively
on glucose for energy requirements. Impaired
glucose oxidation also causes an accumulation of
pyruvic and lactic acids, which produce vasodilatation
and increased cardiac output.
Deficiency – beri-beri
In the developed world Thiamin deficiency is mainly encountered in chronic alcoholics. Poor diet, impaired absorption, storage in the liver, and the increased requirements for thiamin to metabolise ethanol all contribute. In the developing world, deficiency usually arises as a consequence of a diet based on polished rice. The body has very limited stores of thiamin, so deficiency is manifest after only 1 month on a thiamin-free diet.There are two forms of the disease in adults:
• Dry (or neurological) beri-beri manifests with chronic peripheral neuropathy and with wrist and/or foot drop, and may cause Korsakoff’s psychosis and Wernicke’s encephalopathy .
• Wet (or cardiac) beri-beri causes generalised oedema
due to biventricular heart failure with pulmonary congestion.
In dry beri-beri, response to thiamin administration
is not uniformly good. However, multivitamin therapyseems to produce some improvement, suggesting
that other vitamin deficiencies may be involved.
Wernicke’s encephalopathy and wet beri-beri should
be treated without delay with intravenous vitamin B
and C mixture (‘Pabrinex).
Korsakoff’s psychosis is irreversible and does not respond to thiamin treatment.
Riboflavin (vitamin B2 )
Riboflavin is required for the flavin co-factors involved
in oxidation–reduction reactions. It is widely distributed
in animal and vegetable foods. Levels are low in staple
cereals but germination increases its content. It is
destroyed under alkaline conditions by heat and by
exposure to sunlight.
Deficiency is rare in developed countries. It mainly
affects the tongue and lips and manifests as glossitis,
angular stomatitis and cheilosis. The genitals may be
affected, as well as the skin areas rich in sebaceous
glands, causing nasolabial or facial dyssebacea. Rapid
recovery usually follows administration of riboflavin
10 mg daily by mouth.
Niacin (vitamin B3 )
Niacin encompasses nicotinic acid and nicotinamide.Nicotinamide is an essential part of the two pyridine
nucleotides, nicotinamide adenine dinucleotide (NAD)
and nicotinamide adenine dinucleotide phosphate (NADP), which play a key role as hydrogen acceptors
and donors for many enzymes.
Niacin can be synthesized in the body in limited amounts from the amino acid tryptophan.
Deficiency – pellagra
Pellagra was formerly endemic among poor people who
subsisted chiefly on maize, which contains niacytin, a
form of niacin that the body is unable to utilise. Pellagra
can develop in only 8 weeks in individuals eating diets
that are very deficient in niacin and tryptophan. It
remains a problem in parts of Africa, and is occasionally
seen in alcoholics and in patients with chronic small
intestinal disease in developed countries. Pellagra can
occur in Hartnup’s disease, a genetic disorder characterised by impaired absorption of several amino acids, including tryptophan. It is also seen occasionally in carcinoid syndrome ,when tryptophan is consumed in the excessive production of 5-hydroxytryptamine (5-HT).
Pellagra has been called the disease of the
three Ds:• Dermatitis. Characteristically, there is erythema
resembling severe sunburn, appearing symmetrically over the parts of the body exposed to sunlight, particularly the limbs and especially on the neck, but not the face (Casal’s necklace). The skin lesions may progress to vesiculation, cracking, exudation and secondary infection.
• Diarrhoea. This is often associated with anorexia, nausea, glossitis and dysphagia, reflecting the presence of a non-infective inflammation that extends throughout the gastrointestinal tract.
• Dementia. In severe deficiency, delirium occurs acutely and dementia develops in chronic cases.
Treatment is with nicotinamide, given in a dose of
100 mg 3 times daily orally or parenterally. The responseis usually rapid. Within 24 hours, the erythema diminishes,
the diarrhoea ceases and a striking improvement
occurs in the patient’s mental state.
Toxicity
Excessive intakes of niacin may lead to reversible
hepatotoxicity. Nicotinic acid is a lipid-lowering agent,
but at doses above 200 mg a day gives rise to vasodilatory symptoms (‘flushing’ and/or hypotension).
Pyridoxine (vitamin B6 )
Pyridoxine, pyridoxal and pyridoxamine are different
forms of vitamin B6 that undergo phosphorylation to
produce pyridoxal 5-phosphate (PLP). PLP is the
co-factor for a large number of enzymes involved in the
metabolism of amino acids. Vitamin B6 is available in
most foods.
Deficiency is rare, although certain drugs, such as
isoniazid and penicillamine, act as chemical antagonists
to pyridoxine. Pyridoxine administration is effective
in isoniazid-induced peripheral neuropathy and some
cases of sideroblastic anaemia.
Large doses of vitamin B6 have an antiemetic effect in radiotherapy-induced nausea.
Although vitamin B6 supplements have become
popular in the treatment of nausea in pregnancy, carpaltunnel syndrome and premenstrual syndrome, there is
no convincing evidence of benefit.
Very high doses of vitamin B6 taken for several months can cause a sensory polyneuropathy.
Biotin
Biotin is a co-enzyme in the synthesis of fatty acids,isoleucine and valine and is also involved in gluconeogenesis.
Deficiency results from consuming very large
quantities of raw egg whites (> 30% energy intake)
because the avidin they contain binds to and inactivates
biotin in the intestine. It may also be seen after long
periods of total parenteral nutrition.
The clinical features of deficiency include scaly dermatitis, alopecia and paraesthesia.
Folate (folic acid)
Folates exist in many forms. The main circulating form
is 5-methyltetrahydrofolate. The natural forms are prone
to oxidation. Folic acid is the stable synthetic form.
Folate works as a methyl donor for cellular methylation
and protein synthesis. It is directly involved in DNA
and RNA synthesis, and requirements increase during
embryonic development. Folate deficiency may cause three major birth defects (spina bifida, anencephaly and encephalocele) resulting from imperfect closure of the neural tube, which takes place 3–4 weeks after conception. Women who have experienced a pregnancy affected by a neural tube defect should take 5 mg of folic acid daily from before conception and throughout the first trimester.
The UK Department of Health advises that All
women planning a pregnancy are advised to includegood sources of folate in their diet, and to take folate
supplements throughout the first trimester. Liver is the
richest source of folate but an alternative source (e.g.
leafy vegetables) is advised in early pregnancy because
of the high vitamin A content of liver . Folate deficiency has also been associated with heart disease, dementia and cancer. There is mandatory fortification of flour with folic acid in the US and voluntary fortification of many foods across Europe. There are now concerns that this may contribute to the increased incidence of colon cancer through promotion of the growth of polyps.
Hydroxycobalamin (vitamin B12 )
Vitamin B12 is a co-factor in folate co-enzyme recyclingand nerve myelination. Vitamin B12 and folate are particularly important in DNA synthesis in red blood cells.
Vitamin B12 , but not folate, is needed for the integrity of myelin, so that vitamin B12 deficiency is also associated with neurological disease.
Neurological consequences of vitamin B12 deficiency
In older people and chronic alcoholics, B12 deficiency arises from insufficient intake and/or from malabsorption. Several drugs, including neomycin, can render vitamin B12 inactive. Adequate intake of folate maintains erythropoiesis and there is a concern that fortification of foods with folate may mask underlying vitamin B12 deficiency.
In severe deficiency there is insidious, diffuse and uneven demyelination. It may be clinically manifest as peripheral neuropathy or spinal cord degeneration affecting both posterior and lateral columns (‘subacute combined degeneration of the spinal cord’), or there may be cerebral manifestations (resembling dementia) or optic atrophy. Vitamin B12 therapy improves symptoms in most cases.
Vitamin C (ascorbic acid)
Ascorbic acid is the most active reducing agent inthe aqueous phase of living tissues and is involved
in intracellular electron transfer. It takes part in the
hydroxylation of proline and lysine in protocollagen to
hydroxyproline and hydroxylysine in mature collagen.
It is very easily destroyed by heat, increased pH and
light, and is very soluble in water; hence many traditional
cooking methods reduce or eliminate it. Claims
that high-dose vitamin C improves immune function
(including resistance to the common cold) and cholesterol
turnover remain unsubstantiated.
Deficiency – scurvy
Vitamin C deficiency causes defective formation of collagen with impaired healing of wounds, capillary haemorrhage and reduced platelet adhesiveness (normalplatelets are rich in ascorbate) . Precipitants and clinical features of scurvy are shown in Box.
A dose of 250 mg vitamin C 3 times daily by mouth should
saturate the tissues quickly. The deficiencies of the
patient’s diet also need to be corrected and other vitamin
supplements given if necessary. Daily intakes of more
than 1 g/day have been reported to cause diarrhoea and
the formation of renal oxalate stones.
Scurvy – vitamin C deficiency
Scurvy.
A Gingival swelling and bleeding.B Perifollicular hyperkeratosis.
Other dietary organic compounds
There are a number of non-essential organic compoundswith purported health benefits such as reducing risk of
heart disease or cancer. Groups of compounds such as
the flavonoids and phytoestrogens show bioactivity through their respective antioxidant and oestrogenic or
anti-oestrogenic activities.
Flavonoids (of which there are a number of different classes of compound) are found in fruit and vegetables, tea and wine; phytoestrogens are found in soy products (with higher intakes in parts of Asia compared to Europe and the US) and pulses.
Caffeine from tea and coffee and carbonated
beverages affects the nervous system and can improvemental performance in the short term, with adverse
effects seen at higher intakes. Intake of non-carbonic
organic acids (which are not metabolised to carbon
dioxide), e.g. oxalates, may be restricted in individuals
prone to kidney stones.
Vitamin deficiency in old age
Inorganic micronutrientsA number of inorganic elements are essential dietary
constituents for humans . Deficiency is seen
when there is inadequate dietary intake of minerals or
excessive loss from the body. Toxic effects have also
been observed from self-medication and disordered
absorption or excretion. Examples of clinical toxicity
include excess of iron (haemochromatosis or haemosiderosis), fluoride (fluorosis), copper (Wilson’s disease) and selenium (selenosis, seen in parts of China). For most minerals, the available biochemical markers do not accurately reflect dietary intake and dietary assessment is required.
Summary of clinically important minerals
Calcium and phosphorusCalcium is the most abundant cation in the body and
powerful homeostatic mechanisms control circulating
ionised calcium levels . WHO’s dietary guidelines for calcium differ between countries, with higher intakes usually recommended in places with higher fracture prevalence. Between 20 and 30% of calcium in the diet is absorbed, depending on vitamin D status and food source. Calcium requirements depend on phosphorus intakes, with an optimum molar ratio (Ca : P) of 1 : 1. Excessive phosphorus intakes (e.g. 1–1.5 g/day) with a Ca : P of 1 : 3 have been shown to cause hypocalcaemia and secondary hyperparathyroidism .
Calcium absorption may be impaired in vitamin D
deficiency and in malabsorption secondary
to small intestinal disease. Calcium deficiency
causes impaired bone mineralisation and can lead to
osteomalacia in adults. Too much calcium can lead to constipation and toxicity has been observed in ‘milk-alkali syndrome’.
Dietary deficiency of phosphorus is rare (except
in older people with limited diets) since it is present
in nearly all foods and phosphates are added to a
number of processed foods.
Phosphate deficiency in adults occurs:
• in patients with renal tubular phosphate loss• due to prolonged high dosage of aluminium hydroxide
• sometimes when alcoholics are fed with highcarbohydrate foods
• in patients receiving parenteral nutrition if inadequate phosphate is provided.
Deficiency causes hypophosphataemia and
muscle weakness secondary to ATP deficiency.
Iron
Iron is involved in the synthesis of haemoglobin, and isrequired for the transport of electrons within cells and
in a number of enzyme reactions. Non-haem iron in
cereals and vegetables is poorly absorbed but makes the
greater contribution to overall intake, compared to the
well-absorbed haem iron from animal products.
Fruits and vegetables containing vitamin C enhance iron
absorption, while the tannins in tea reduce it.
Dietary calcium reduces iron uptake from the same meal, which may precipitate iron deficiency in those with borderline iron stores.
There is no physiological mechanism for excretion of iron, so homeostasis depends on the regulation of iron absorption .This is regulated at the level of duodenal enterocytes by hepcidin.
The expression of hepcidin (a peptide secreted by
hepatocytes in the duodenum) is suppressed when body
iron is low, leading to enhanced efflux of iron into the
circulation. The normal daily loss of iron is 1 mg, arising
from desquamated surface cells and intestinal losses. A
regular loss of only 2 mL of blood per day doubles the
iron requirement. On average, an additional 20 mg of
iron is lost during menstruation, so pre-menopausal
women require about twice as much iron as men (and
more if menstrual losses are heavy).
The major consequence of iron deficiency is anaemia.
This is one of the most important nutritional causes of ill health in all parts of the world. In the UK, it is estimated that 10% women are iron-deficient.Dietary iron overload is occasionally observed and
results in iron accumulation in the liver and, rarely, cirrhosis.
Haemochromatosis results from an inherited
increase in iron absorption.
Iodine
Iodine is required for synthesis of thyroid hormones.It is present in sea fish, seaweed and most plant
foods grown near the sea. The amount of iodine in soil
and water influences the iodine content of most foods.
Iodine is lacking in the highest mountainous areas of the
world (e.g. the Alps and the Himalayas) and in the soil
of frequently flooded plains (e.g. Bangladesh).
About a billion people in the world are estimated
to have an inadequate iodine intake and hence are at
risk of iodine deficiency disorder.
Goitre is the most common manifestation, affecting about 200 million people
In those areas where most women have endemic
goitre, 1% or more of babies are born with cretinism
(characterised by mental and physical retardation).
There is a higher than usual prevalence of deafness,
slowed reflexes and poor learning in the remaining population.
The best way of preventing neonatal cretinism
is to ensure adequate levels of iodine during pregnancy.
This can be achieved by intramuscular injections with
1–2 mL of iodised poppy seed oil (475–950 mg iodine)
to women of child-bearing age every 3–5 years, by
administration of iodised oil orally at 6-monthly or
yearly intervals to adults and children, or by providing
iodised salt for cooking.
Zinc
Zinc is present in most foods of vegetable and animalorigin. It is an essential component of many enzymes,
including carbonic anhydrase, alcohol dehydrogenase
and alkaline phosphatase.
Acute deficiency has been reported in patients receiving prolonged zinc-free parenteral nutrition and causes diarrhoea, mental apathy, a moist, eczematoid dermatitis, especially around the mouth, and loss of hair. Chronic zinc deficiency occurs in dietary deficiency, malabsorption syndromes, alcoholism and its associated hepatic cirrhosis. It causes the clinical features seen in the very rare congenital disorder known as acrodermatitis enteropathica (growth retardation, hair loss and chronic diarrhoea).
Zinc deficiency is thought to be responsible for one-third of the world’s population not reaching their optimal height. In the Middle East, chronic deficiency has been associated with dwarfism and hypogonadism. In starvation, zinc deficiency causes thymic atrophy, and zinc supplements may accelerate the healing of skin lesions, promote general wellbeing, improve appetite and reduce the morbidity associated with the under-nourished state, and lower the mortality associated with diarrhoea and pneumonia in children.
Selenium
The family of seleno-enzymes includes glutathione peroxidase, which helps prevent free radical damage tocells, and monodeiodinase, which converts thyroxine to
triiodothyronine .
North American soil has a higher selenium content than European and Asian soil, and the decreasing reliance of Europe on imported American food in recent decades has resulted in a decline in dietary selenium intake.
Selenium deficiency can cause hypothyroidism,
cardiomyopathy in children (Keshan’s disease) and
myopathy in adults.
Excess selenium can cause heart disease.
Fluoride
Fluoride helps prevent dental caries, since it increasesthe resistance of the enamel to acid attack. It is a component of bone mineral and some studies have shown
anti-fracture effects at low doses, but excessive intakes
may compromise bone structure.
If the local water supply contains more than 1 part
per million (ppm) of fluoride, the incidence of dental
caries is low. Soft waters usually contain no fluoride,
whilst very hard waters may contain over 10 ppm. The
benefit of fluoride is greatest when it is taken before the
permanent teeth erupt, while their enamel is being laid
down. The addition of traces of fluoride (at 1 ppm) to
public water supplies is now a widespread practice.
Chronic fluoride poisoning is occasionally seen where
the water supply contains > 10 ppm fluoride. It can also
occur in workers handling cryolite (aluminium sodium
fluoride), used in smelting aluminium.
Pitting of teeth is a result of too much fluoride as a child. Sodium, potassium and magnesium
Western diets are high in sodium due to the sodium chloride (salt) that is added to processed food. In the UK, it is suggested that daily salt intakes are kept well < 6 g.
Other essential inorganic nutrients
These include chloride (a counter-ion to sodium andpotassium), cobalt (required for vitamin B12), sulphur (a
constituent of methionine and cysteine), manganese
(needed for or activates many enzymes) and chromium
(necessary for insulin action).
Deficiency of chromium presents as hyperglycaemia and has been reported in adults as a rare complication of prolonged parenteral nutrition.
Copper metabolism is abnormal in Wilson’s disease.
Deficiency occasionally occurs but only in young children, causing microcytic hypochromic anaemia, neutropenia, retarded growth, skeletal rarefaction and dermatosis.