1

2
3
Part:1
Obstetric
Obstetric History
#Identification
Patient: triple name – age – occupation – residence – blood group
Husband: triple name – age – occupation – residence – blood group
Date of marriage
Relationship status
Number of children
Educational background
#Date of admission
#Date of delivery or operation
1. GPA:
G: gravida number of all pregnancies (delivered or aborted).
If the patient is
still pregnant at the time of history taking we can mention the gravida, but if the patient is
already delivered at the time of history taking we not mention the gravida.
P: para or parity number of deliveries after 24 weeks (live or dead)
A: abortion number of expulsions of products of conception before 24
weeks (normal or ectopic حمل خارج الرحمor hydatidiform يدوقنع لمح)
2. LMP: last menstrual period
it is the first day of the last menstrual period
the patient certainty of dates ( )يجب التأكد من صحة التواريخ
ask about the regularity of the cycle
ask about the usage of contraception (type-amount-duration)
3. EDD: expected date of delivery
Calculated by Naegele's rule EDD = LMP + 7 days – 3 months (or +9 months)
this for regular cycle (28 day – not lactating – no use of contraception)
For irregular cycle the date of first Ultrasound is around 20 weeks so we can
calculate the EDD from this information
4. GA: gestational age
Number of weeks from the beginning of pregnancy until the end (whether
normal delivery or C.S or abortion)
Calculated as EDD - real date of delivery or EDD - date of history taking
Pre-term: 36 weeks + 6 days or less
4
Term: from 37 weeks to 40 weeks
Post-date: from 40 weeks to 41 weeks + 6days
Post-term: 42 weeks and more
GA is important to know if the baby is premature so we can support the baby
after delivery
#Date of examination
#Chief complaint
Main complaint (usually one) in patient's own words
Duration of the compliant
#History of present illness
Everything from the start of chief complaint until the delivery
Chronological order
In details
#History of labor
1- During operation
At home or hospital
Difficult or easy
Vaginal delivery, cesarean section, episiotomy, forceps used or not
Duration of operation
Type of analgesia
Catheter
Blood transfusion
I.V fluid
Complications during operation
2- Post-operative
Time of return of consciousness
Blood transfusion
I.V fluid
Analgesia
Catheter
Complications
Nausea, appetite, vomiting
Bowel motion, flatus
PPH
post-partum hemorrhage
Micturition after delivery
Walking after delivery
Breast milk amount
5
#The outcome of delivery
Live or dead
Male or female
Weight of baby
Crying after birth
Infant movement
Cyanosis –jaundice – anemia – blood exchange
Fetal distress
Admission to the neonatal intensive care unit
Feeding (breast or bottle or mixed)
Neonatal care
APGAR score (Appearance – pulse rate – grimace (irritability) – activity –
respiratory effort)
#History of presenting pregnancy
(1, 2, 3 trimester + Systems)
First trimester: ask the patient about:
General health (tiredness – malaise – other non-specific symptoms)
Method of conformation of the pregnancy
Investigations (Ultrasound – blood test – urine test – others)
Vaginal bleeding or discharge
Morning sickness (nausea – vomiting – appetite – constipation)
Micturition (frequency, dysuria, color of urine …….)
ANC ( ante natal care ) go to hospital – take folic acid and vitamins
Drugs (teratogenic drugs - drugs that increased/decreased it's dose in pregnancy)
Back pain
Edema
Abortion
Current disease
Hyper emesis gravidum
Breast tenderness or pain
Second trimester: ask the patient about:
Vaginal bleeding or discharge
Vaccine (like Tetanus toxoid start at 4 month – other vaccines start at 6 months)
Quickening the first feeling of fetal movement by the mother. In parous feel in 16
– 18 weeks. In primi feel in 18 – 20 weeks
Abortion
Weight
هام
هام
6
Bowel motion
Current disease
ANC ( ante natal care )
Drug history
Morning sickness (nausea – vomiting – appetite – constipation)
Back pain
Edema
Micturition (frequency, polyuria …….)
Anemia and pre-eclampsia
Premature contractions
Third trimester: ask the patient about:
Vaginal bleeding or discharge
ANC ( ante natal care )
Weight
Bowel motion
Edema
PIH pregnancy induced hypertension
Pre-eclampsia and eclampsia ( hypertension + proteinuria albumin in urine )
Drug history
Abortion
Current disease
headache
Fit
palpation and chest pain
SOB shortness of breath
UTI urinary tract infection
IUD intra uterine death
Review of other systems: ask the patient about:
CVS
(chest pain, dyspnea, palpitations, edema, syncope, claudication)
Respiratory
(cough, sputum, hemoptysis, chest pain, dyspnea, wheeze, cyanosis, clubbing )
GIT
(dysphagia, dyspepsia, abdominal pain, bleeding ,vomiting, weight loss, diarrhea)
CNS
(headache, fit, weakness, vision ,hearing, tremor, incontinence, paresthesia)
Renal
(urine color, amount, dysuria, hematuria, nocturia, frequency, urgency, pain)
Skin and loco-motor
(pigmentations, discoloration, pain, stiffness, function, swelling)
Genital
(incontinence, impotence, discharge)
#Past obstetric history
(history of previous pregnancies in sequence)
Date of marriage
Age of patient at marriage
هام
7
Age of patient at first pregnancy
Period of infertility (primary infertility – secondary infertility)
Interval between current pregnancy and 1st pregnancy
Past pregnancies in sequence and ask the following questions for each child
o Time of pregnancy
o Duration of pregnancy
o Type of delivery
o Site of delivery
o Gender of baby
o Weight of baby
o Congenital anomaly
o NICV admission
o SOB (shortness of breath) cry immediate
o Any problem to baby
o ANC
o Puerperium ( )فترة النفاس ask about any fever, bleeding, depression, breast
feeding, any complication.
#Gynecological history
Age of menarche first menstrual cycle in life
Menstrual cycle regular – irregular – duration – frequency - amount of blood loss
– any clot or pain with the menstruation - dysmenorrhea – intermenstural bleeding
Vaginal discharge
Contraception pill or IUCD (intra uterine contraceptive device)
Infertility failure of gestation and producing offspring after months of marriage
without using contraception
Gynecological operation Any operation related to gynecological problem - Genital
infections - Date of last cervical smear
#Past medical history
Any serious illness or medical disease or chronic disease like:
D.M and Renal diseases
Hypertension (pre-eclampsia)
Epilepsy, syphilis, rubella, arthritis
Venous thromboembolic disease
HIV, recurrent infections, rheumatic heart disease
Myasthenia gravis – myotonic dystrophy - Connective tissue diseases
In case of +ve finding ask about the time of onset, duration, treatment or not, drugs
taken in pregnancy or not.
8
#Past surgical history
Previous operation (like Caesarian section, appendectomy, cholecystectomy)
Post-operative complications
Anesthesia complications
Blood transfusion
#Drug history
Allergy to any drug
Chronic drug usage like antihypertensive and antiepileptic drugs
Medications taken during pregnancy (like Anti-HT, Anti-DM) and dose
#Family history
Any chronic disease (hypertension – D.M – thromboembolic disease)
Consanguineous marriage
History of pre-eclampsia
History of twin pregnancy or congenital anomalies or cerebral palsy
History of Genetic problems like haemoglibinopathies or fetal inborn error of
metabolism
History of malignancy in family
History of T.B or allergies or Bleeding disorders or psychiatric disorders
#Social history
Occupation - crowding - housing conditions - living environment
Marital status - family problems
Personal (Smoking - alcohol - drug abuse - sleep - diet - bowel habits)
Level of education - income
water supply - animal contact
9
Part:2
Obstetric
Obstetric Examination
#General examination
Like that of medicine, important points for obstetric:
General:
o Age of the patient
o Posture (lying in bed, or sitting)
o Alert or not, irritable or sleepy, oriented
o Any external corrections (cannula, IV fluid, oxygen mask)
o Ill or well? Comfortable or not?
o Built (average build, thin, emaciated, obese)
Face:
o Presence of cyanosis, pale face, pigmentation
o Chloasma: pigments in the face present during pregnancy)
Eye:
o Sclera (yellow or normal)
o Conjunctiva (pale or not)
Mouth:
o Tongue and mucous membrane (anemia, dehydration, jaundice, cyanosis)
o Tooth loss or abnormalities (reflecting a loss of Calcium)
Neck:
o L.N enlargement
o Thyroid gland
o Arterial and venous pulsation
Hand:
o Color: normal, pale, yellow, blue
o Nails: clubbing, swelling
Leg:
o Exposure to the mid-thigh
o Hair distribution
o Color changes, Abnormal pigmentation, Scar
o Calf muscles tenderness
o Edema (pitting, non-pitting) examine for 1 min
o Varicose veins
o Arterial pulsation (like medicine)
o D.V.T examine the pulse , temperature, diameter
Vital signs:
o Pulse: radial pulse (for 1 min) example: 80 bpm, regular, normal volume
Differential diagnosis
of Swelling of fingers:
o Hepatic infection
o Pre-eclampsia
Risks of developing
DVT are: cesarean
section, anemia,
pregnancy, no
movement after labor

11
o Blood pressure: patient in setting or lateral position
o Respirator rate
o Temperature: axillary or oral, fever means infection
Examination of cardiovascular and respiratory systems
Ophthalmoscopy hypertensive/diabetic women
#Abdominal examination
Goals:
Know the size of the uterus (level of the fundus) and whether corresponding to the
gestational age or not
Know the number of fetuses
See the lie, attitude, presentation and position
Assessment of disproportion between size of head and pelvis
Detect any abnormality (Polyhydramnious, ovarian cyst, fibroids)
Inspection:
Shape of the abdomen:
o Distended abdomen: symmetry of the enlarged uterus, general size, shape of the
uterus
o Over distention (girth 100 cm)
indicating twin, polyhydramnious
o Flatting of lower abdomen indicating occiput posterior position
Skin:
o Scars: caesarean scar (Pfannenestiel scar)
o Color and pigmentation
o Stria albicans: of previous pregnancy
o Stria gravidarum: of current pregnancy
o Linea nigra: faint brown line running from the umbilicus to the symphysis pubis
Umbilicus: flat, inverted, everted, round, slit like
Dilated veins and hernia
Fetal movement: can be seen at the moment of examination
Look for scars (women often forget to mention previous surgical procedures if they
were performed long ago). The common areas to find scars are:
o Suprapubic (Caesarean section, laparotomy for Ectopic pregnancy or ovarian
masses).
o Sub-umbilical (laparoscopy).
o Right iliac fossa (appendectomy).
o Right upper quadrant (cholecystectomy).
Inspection of fetal lie transverse uterus, longitudinal uterus

11
Palpation:
Superficial palpation:
o Ask about areas of tenderness
o Gentle palpation is made away from the areas of tenderness
o Look for any superficial mass, soft abdomen, rigid or contraction
Palpation of organs (liver, spleen, kidneys, bladder)
Deep palpation: if indicated by a history of hepatitis or chronic liver diseases
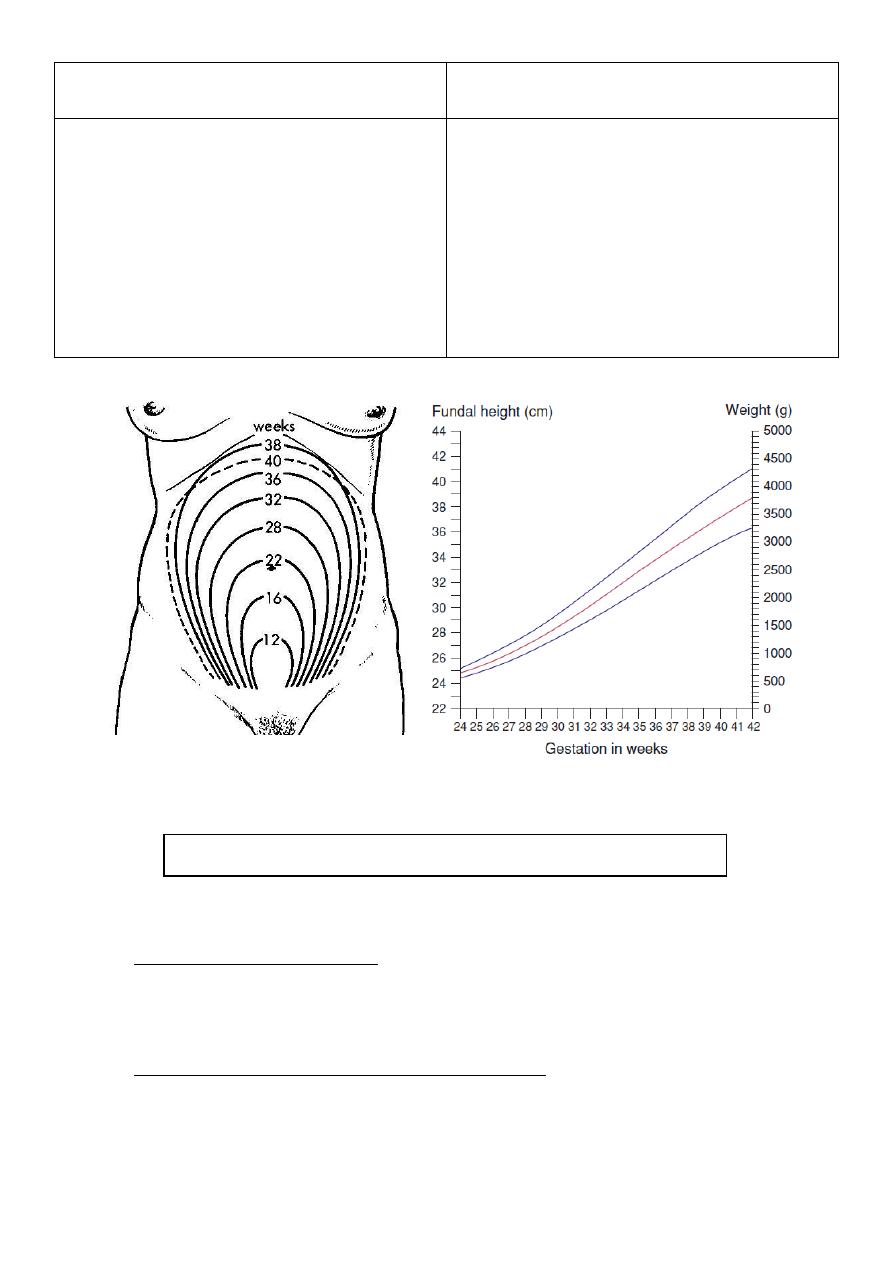
Fundal height:
o Fundal height is generally defined as the distance from the pubic bone to the top
of the uterus measured in centimeters.
o After the first 16 weeks of pregnancy, the fundal height measurement often
matches the number of weeks of pregnancy.(example: 27 weeks of pregnant =
fundal height is about 27 cm)
o Feel carefully for the top of the fundus (by the ulnar border of the left). This is
rarely in the midline. Make a mental note of where it is. Now feel very carefully
and gently for the upper border of the symphysis pubis. Place the tape measure
on the symphysis pubis and, with the centimeter marks face down, measure to
the previously noted top of the fundus. Turn the tape measure over and read the
measurement. Plot the measurement on an SFH chart – this will usually be
present in the hand-held notes.
o If plotted on a correctly derived chart, it is apparent that in the late third trimester
the fundal height is usually approximately 2 cm less than the number of weeks.
o After you have measured the SFH, palpate to count the number of fetal poles. A
pole is a head or a bottom. If you can feel one or two, it is likely to be a singleton
pregnancy. If you can feel three or four, a twin pregnancy is likely. Sometimes
large fibroids can mimic a fetal pole; remember this if there is a history of fibroids.
o Now you can assess the lie. This is only necessary as the likelihood of labor
increases, i.e. after 34–36 weeks in an uncomplicated pregnancy.
o Once you have established that there is a pole over the pelvis, if the gestation is
34 weeks or more, you need to establish what the presentation is. It will be either
cephalic (head down) or breech (bottom/feet down). Using a two-handed
approach and watching the woman’s face, gently feel for the presenting part.
Fundal height at level of umbilicus symphysis pubis 12 weeks
Fundal height at level of umbilicus umbilicus 22 weeks
Fundal height at level of umbilicus xiphosterum 36 weeks
12
Leopold’s Maneuver:
o First maneuver (fundal grip): Using both hands, feel for the fetal part lying in the
fundus.
a.) Cephalic: is more firm, hard, round that moves independently of the body
b.) Breech: is less well defined, moves only in conjunction with the body
o Second maneuver (umbilical grip or lateral grip): Move your hands down the sides
of the abdomen and apply gentle pressure.
a.) Fetal back: is smooth, hard, and resistant surface
b.) Knees and elbows of fetus: feel with a number of angular nodulation
Causes of smaller fundal height
small for date
Causes of larger fundal height
Large for date
Intra-uterine growth retardation (IUGR)
Miscalculation (Wrong LMP)
Oligohydraminous
Genetics
Transverse lie
A baby prematurely descending into the
pelvis or settling into a breech or other
unusual position
Rapid fetal growth
Miscalculation (Wrong LMP)
Polyhydramnious
Multiple pregnancies
Macrosomia (diabetic mother)
Abruption placenta
Multiple uterine fibroids
Edema and Full bladder
See this video http://www.muhadharaty.com/lecture/1686
13
o Third maneuver (Pawlik’s grip): Spread apart the thumb and fingers of the hand.
Place them just above the patient’s symphysis pubis
a.)If descended (engaged): you’ll feel the head fixed
b.)If undescended (not engaged ): you’ll feel less distinct mass mobile
o Fourth maneuver (pelvic grip): Facing foot part of the woman, palpate fetal head
pressing downward about 2 inches above the inguinal ligament. Use both hands.
a.)Good attitude: if brow correspond to the side that contained the elbows &
knees.
b.)Poor attitude: if examining fingers will meet an obstruction on the same side as
fetal back. If brow is very easily palpated, fetus is at posterior position.
Assessing the fetus
o For a pregnancy of >32 weeks gestation you should asses the lie and presentation,
and feel the head.
o Lie (Longitudinal - Transverse - Oblique): this is the position of the long axis of the
fetus in relation to the mother. Palpating the abdomen try to feel the baby’s back
and limbs. The back will feel like smooth curve, whilst the limbs will feel irregular
and usually indistinct
o Presentation (Cephalic - Breech - Shoulder - Face - Brow): this is determined
by the fetal lie and the presenting part
o Position (occipito-Anterior - occipito transverse - Occipito Posterior - Breech
positions - Right sacrum posterior): this describes the position of the fetal head in
relation to the pelvis
o Engagement: In a normal lie and presentation, this assess how far the head has
descended into the pelvis. We describe it by noting how may ‘fifths’ of the head
are palpable, example:
The whole head is palpable – "the head is 5/5
th
palpable"
The jaw only is palpable – "1/5
th
palpable"
In primigravida: the head normally engages by the 37th week. In subsequent
pregnancies, it usually does not engage until labor
The head is 'engaged' when the widest part has passed through the pelvic
brim – thus roughly equal to 2 or 3/5
th
palpable
Percussion:
There isn’t really much to do for percussion. Some may recommend percussing to
determine a rough idea of the amniotic fluid volume. Examine for the fluid thrill
The normal amniotic fluid volume is 500ml – 1L
For more information http://nursingcrib.com/?s=Leopold+Maneuver

14
Oligohydramnios: low volume of amniotic fluid. A normal fetus will drink amniotic
fluid, and urinate back into the fluid, keeping the volume stable. Reduced volume
could be the result of a fetal kidney problem
Polyhydramnious: high volume of amniotic fluid. Associated with maternal diabetes
Auscultation:
If the fetus has been active during your examination and the mother reports that the
baby is active, it is not necessary to auscultate the fetal heart.
If you are using a Pinard stethoscope, position it over the fetal, hearing the heart
sounds with a Pinard takes a lot of practice. If you cannot hear the fetal heart, never
say that you cannot detect a heartbeat; always explain that a different method is
needed and move on to use a hand-held Doppler device.
If you have begun the process of listening to the fetal heart, you must proceed until
you are confident that you have heard the heart. With twins, you must be confident
that both have been heard.
The fetal heart sounds are listened at a point midway between the anterior superior
iliac spine & the umbilicus on the back of the baby (usually in the right if the
presentation is cephalic)
In breech presentations: the heart sounds will often be heard above the umbilicus
In Head (vertex) presentations: the heart sounds will often be heard below umbilicus
Auscultation is either by fetoscope or bell of a stethoscope or best by sonic aid
(heard in case of audible fetal heart sounds) (normal range: 115-150 bpm)
Finishing off:
You could:
Take the BP: checking for pre-eclampsia
Urine dipstick: checking for
o Protein pre-eclampsia
o Leukocytes infection
o Glucose (even ketones) diabetes
Record mother's weight : normal pregnancy has weight gain of about 24lbs
#Vaginal examination
Indications:
o Post-date pregnancy
o Decreased fetal movements (normally 10 movements/12 hours)
o Excessive or offensive discharge
o Vaginal bleeding (in the known absence of a Placenta praevia)
o To perform a cervical smear
o To confirm potential rupture of membranes
15
Contraindications:
o Known placenta praevia or vaginal bleeding when the placental site is unknown
and the presenting part unengaged
o Pre-labor rupture of the membranes (increased risk of ascending infection)
Setting:
o Before commencing the examination, assemble everything you will need (swabs
etc.)
o Ensure the light source works
o Position the patient semirecumbent with knees drawn up and ankles together
o Ensure that the patient is adequately covered
The examination include:
o Inspection of the vulva
o Examination of the vagina
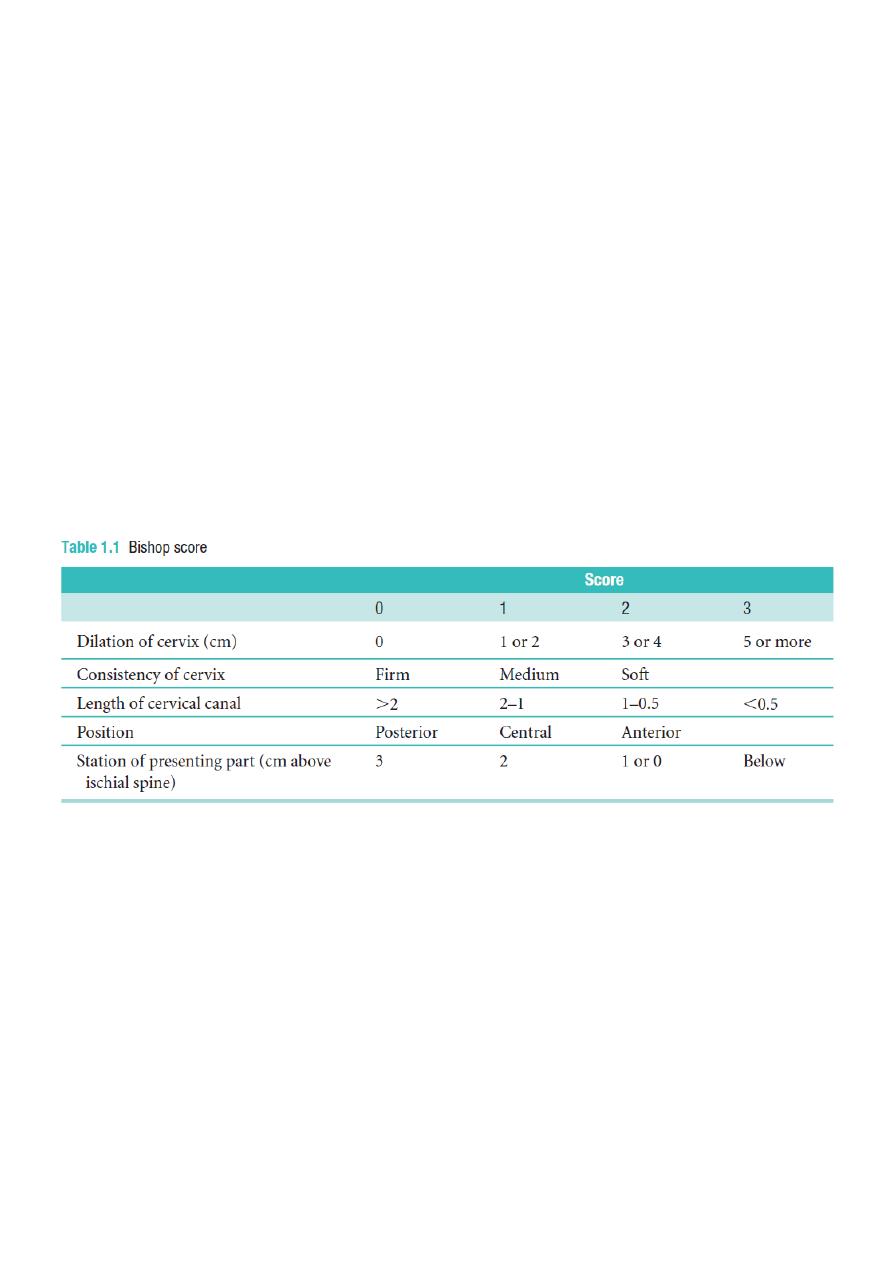
o Palpation of the cervix (cervical dilatation and effacement)
o Feeling the presenting part (late in pregnancy)
o See the station ischial spin = zero, above it +, below it -
o Palpation of the rectovaginal pouch: when deep engagement occur and can detect
abnormality like ovarian cyst
#Assessment of liquor amount
After the pelvic grip, we try to assess the amount of liquor by palpating the abdomen
In polyhydramnious when the fetus pushed by the hands of the examiner, it is felt
that the fetus is pushed to the back and then return to the left hand of the examiner
In oligohydroamnious the baby is stuck to the wall of the abdomen
#Estimation of the fetal weight
Done after assessing the amount of liquor
Fetal weight is estimated by surrounding the fetus between the examiner hands and
predicting the weight of the fetus.
#Assessment of fetal liability
Assessment of fetal movement (kick count) at least 10 movements in 12 hours or 3-4
movements in 1 hour
Doppler U.S
Biophysical profile:
o Fetal tone
o Fetal breathing
o Fetal movements
o Amniotic fluid pocket: normally 4-5 liters (below 5 liters oligo)
o Non-stress test:
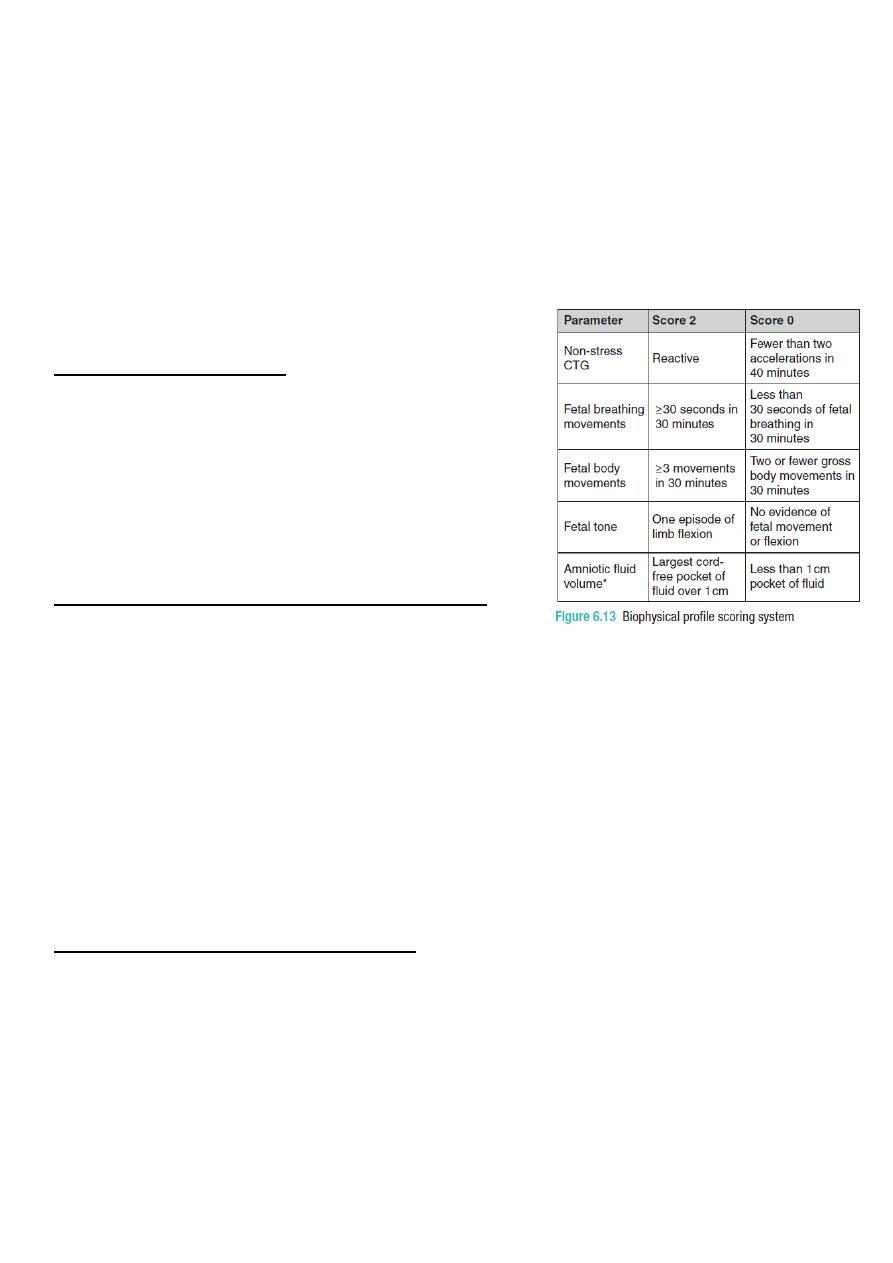
16
Feeling the fetal movements with auscultation of fetal heart (back of baby) at
the same time
Normally there is acceleration of heart rate with fetal movement (increase 15
bpm for 15 sec above the baseline and should be at least 2 accelerations)
The mother lie at left side then put one hand on the abdomen to feel the baby
movements (wait for 20 min) if not feel (put hand for another 20 min) if not
feel it is called equivocal (use Doppler U.S)
Do stress test: by giving oxytocin then use CTG if there is severe deceleration of
fetal heart rate this mean fetal distress.
Do intervertebral test
#Breast examination
Systemic way (setting, inspection, palpation,
examine L.N)
changes in pregnancy (enlargement, secondary
areola)
Nipple (retraction, cracking, discharge)
Breast lump examination
#Assessment of patient before surgery
Take detailed history
Do general examination
Do abdominal examination (fundal height)
Do pelvic examination
Check the fetal well being
If all normal: the patient give trail for vaginal delivery
Induction of oxytocin (start 2 or 5 units)
Do Portogram
Artificial rapture of the membrane (ARM)
Fetal blood sampling (acidosis means fetal distress)
#Examination of post.op patient
It could be caesarean section, episiotomy, or other operations
General examination: vital signs, anemia (anesthesia), cyanosis (intubation), active
internal bleeding can be referred to by a rapid pulse
Leg examination: signs of DVT, unilateral leg edema, dilated veins, shining skin,
tenderness in the calf
Breast examination: inspection, palpation, L.N examination
17
Inspection: observe the dressing (if clean leave it, if not clean open it) – the
indications of removal the dressing are intolerable severe pain and a dressing soaked
with blood
Fundal height examination:(normally below the umbilicus)(finding contracted pelvis)
Deep palpation: can be done before 23 weeks
Grips: are done from 32 weeks and above
Auscultation: for bowel sound, best heard at McBurny's point, heard every 20-30
seconds if negative: give fluid and engorge patient to move
Vaginal examination: bleeding, trauma, episiotomy
Investigations of post.op patient: non-stress test, stress test, CTG, U.S, biophysical
profile, Doppler
Management of post.op patient:
o First day: Vital signs , Sedative, I.V fluid and nothing by mouth (until flatus start) ,
Encourage taking deep breath and cough to get rid of pulmonary edema and to
increase –ve pressure to increase venous return to prevent DVT , Examine for
edema , Examine fore bowel edema, Encourage breast feeding (to prevent PPH)
o Second day: Vital signs, Bowel sound if stop I.V fluid gradually , Laxative if there is
no bowel sound, Check for edema
o Third day: Vital signs, Puerperal pyrexia (chest, UTI, DVT, wound infection, breast
infection, GI infection
o Post.op drugs: prostaglandin, oxytocin, analgesics (opioid, voltarne), Anti-D, flagel,
ceftriaxone
#Presenting
Description of the abdomen after inspection The abdomen is distended, moves
with respiration, showing (no) dilated veins, (inverted, flat or everted) umbilicus,
linea nigra, striae, fetal movement, scars
Description of the uterus after palpation A 36 cm uterus, (longitudinal) lie, with
(the breech) occupying the fundus, and (the head) is the presenting part, (the
engagement), the back is to the (left) and the limbs are to the (right). The amount of
liquor is (good) and the estimated weight is about (3 kg).
Fetal heart rate e.g. was heard - roughly xxx bpm – regular
See this video http://www.muhadharaty.com/lecture/1687
18

19
Part:3
Obstetric
Important Topics
#Abortion:
Definition: expulsion of conception products before 24 weeks of gestation
Occur in First or second trimester
Spontaneous or induced
Causes:
o Fetal diseases: malformation of zygote, defective development of the fertilized
ovum, fatal genetic problem of the fetus
o General diseases of the mother: rubella, syphilis, toxoplasma, malaria, D.M,
hypertension, renal disease, acute emotional disturbance
o Uterine abnormalities: double septate uterus, sub-mucous fibroma, uterine
retroversion and incarceration, incompetent internal os of the cervix
o Hormonal imbalance: progesterone deficiency, thyroid deficiency,
hyperthyroidism
o Irritation of the uterus early in pregnancy
o Drugs: cytotoxic, lead poisoning, oxytocin, ergot, prostaglandins, quinine
o Trauma: insertion of instrument or foreign body through the cervix, surgical
operation (myomectomy), severe trauma to the uterus
o Other causes: immune responses, physical problems in the mother, maternal age,
smoking, drug use, malnutrition, excessive caffeine, exposure to radiation or toxic
materials.
Use of curettage or not ((curettage done in missed or incomplete abortion))
Types
o Complete
1. Less bleeding
2. No pain
3. Closed cervical OS
4. The uterus is normal
5. All contents of the uterus (pregnancy tissue )are expulsed
6. No treatment need
o Incomplete
1. Some of the pregnancy tissue has been expelled while other tissue remains in
the uterus
2. Vaginal bleeding, pain,
3. External cervical os open
4. Products of conception located in cervical os

21
5. Management: blood transfusion , I.M ergometrin, speculum and ring forceps,
evacuation of the uterus under general anesthesia, prophylactic antibiotic
postoperatively
o Missed
1. It is abortion occurs before the 28th week of gestation, after that it is called
intrauterine death or stillbirth
2. Pregnancy test is positive
3. The fetus has not developed or has died
4. Pregnancy tissue has not been expelled from the uterus, with or without pain,
bleeding
5. Uterine size remains stationary or smaller than before
6. Fresh bleeding may become dark or sometimes without bleeding
7. Management: evacuation of the uterus by combination of intra-vaginal
prostaglandins and I.V oxytocin infusion, In early cases do surgery by ring
forceps & dilatation and curettage (DNC)
o Threatened
1. Pregnancy test and fetal heart and quickening are positive
2. Slight or moderate bleeding without clot
3. Little or no pain
4. No dilatation of the cervix (external cervical os close)
5. Uterine size coordinates with the date of gestation
6. Management: bed rest, Ultrasound examination, follow up
o Inventible
1. Irreversible
2. More bleeding with clot
3. Opening cervical OS
4. Painful and rhythmic uterine contractions
5. Membrane may bulge through the internal OS
6. Management: analgesics (pethidine), evacuation of the uterus under G.A with
suction curettage,
7. Differential diagnosis: ectopic pregnancy or follicular mole
o Septic (infected)
1. Infection during pregnancy (fever, weakness, increased pulse rate, broad like
rigidity)
2. Management: broad spectrum antibiotics, blood culture, vaginal swap,
evacuation of the uterus by suction curettage under G.A and antibiotics cover,
oxytocin, vaginal prostaglandins
o Habitual
1. Three consecutive spontaneous abortions
2. Predisposing etiologies: cervical incompetence, progesterone insufficiency,
toxoplasmosis or syphilis

21
3. Dilatation of cervix, bulging membranes
4. Management: cervical circulage (Shirodkhar's operation): insertion of pursest
ring suture of non-absorbable material before 14 week, and remove it at 37
completed weeks or before labor pain.
#Cesarean section:
Definition: it is the operation by which the fetus is delivered by an incision through
abdominal wall and uterus after the 32
nd
week of pregnancy. Before 32
nd
weeks it is
called Hysterotomy
Emergency CS: in which the pregnant woman comes for a reason other than CS, for
example: eclamptic fits at cold weather she needs CS
Elective CS: the pregnant woman comes to the hospital knowing that she will deliver
her baby by CS. The chief complaint for such case is: the patient is admitted for
elective CS (without duration). The history of present pregnancy is: a known case of
previous CS
Indications:
o Faults in the birth canal (passages): cephalopelvic disproportion, pelvic tumor,
cervical or vaginal stenosis or adhesions, double uterus obstruction
o Fetal mal-presentation (passenger)
o Uterine action (power)
o Fulminating pre-eclampsia, hypertension, D.M
o Repeated caesarian section
o Fetal indication: placental insufficiency, cord prolapse, fetal distress (pass of
meconium green color discharge)
o Bad obstetrical history: severe stillbirth or neonatal death
Risks of CS:
o Breathing problems
o Surgical injury (injury to the bladder and uterus)
o Inflammation and infection of the membrane lining the uterus
o Increased bleeding
o Reactions to anesthesia
o Hemorrhage and Blood clots
o Wound infection
o Sepsis, DVT, pulmonary embolism, pain, Adhesions to the intestine
o Increased risks during future pregnancies

22
#Sign & symptoms of pregnancy:
1- Positive signs
Demonstration of the fetal heart beats: by pinard stethoscope or by sonic aid
Quickening: first feeling of fetal movement
Visualization of the fetus and measurements of its diameters: by bi-partial diameter,
femoral length, CRL crown-rump length. >12 weeks of gestation
2- Probable signs
Uterine enlargement: may be due to H.mole or fibroid
Uterine changes in size, shape and consistency:
o Piskacek's sign: when implantation occurs near one of the cornua of the uterus
there will be palpable asymmetrical well defined prominent and soft cornua at the
site of Implantation
o Hegar's sign: palpable softening of the lower uterus starts to appear at 6 weeks
and most evident at 10-12 weeks of gestation
o Palmer's sign: 4-8 weeks regular contractions, occur by manual palpation.
o McDonald's sign: positive when the uterine body and cervix can be easily flexed
against each other.
Cervical changes Goodell's sign: softening of the cervix can be detected by the
second month of pregnancy. In non-pregnant women the cervix is hard like the tip of
the nose. While in the pregnancy the cervix will be soft like the lip.
Palpation of the fetus parts: ballottement of the fetus or fetal part and mapping of the
fetal outline by the palpation
Braxton hick contractions
Endocrine test (pregnancy test): with a possibility of false positive results
3- Presumptive signs
Breast changes: swelling and tenderness
Changes in the skin and mucus membrane:
o Chadwick's sign (violet bluish discoloration of the vulva, vagina, cervix) at 6-8
weeks of gestation
o Increased skin pigmentation (linea nigra, striae gravidarum, chloasma)
o Development of abdominal striae
4- Symptoms
cessation of menses: 8% of pregnancies have some source of bleeding
Nausea with or without vomiting: that occur in half of pregnancies and subsides
within 14 weeks of gestation
Bladder irritability, frequency
Easley fatigability

23
#Polyhydramnious
Definition: this is the excess of amniotic fluid more than 2000 ml
Types:
o Chronic (gradual accumulation noticed after 30
th
week of gestation)
o Acute (earlier and quicker noticed, for example in the uniovlar twins)
Causes:
o Fetal: Multiple pregnancies and Fetal abnormalities: anencephaly, esophageal
and duodenal atresia, spina bifida, skeletal or cardiac or intrauterine infection
(rubella – toxoplasma), fetal tumors
o Maternal: D.M and Rh isoimmunization
o Placental: chorioangioma and circumvallate placenta syndrome
o Idiopathic
Clinical features: unduly enlarged abdomen, usually mobile fetus, chest discomfort,
dyspnea, acute type associated with abdominal pain and vomiting
On examination:
o large for date uterus
o stretched abdominal muscles
o Highly ballotable fetus
o Fluid thrill and malpresentation
o Edema of the abdominal wall and of the vulva
o Very tense uterus especially in the acute phase
Diagnostic tools
o Ultrasound: the deepest pool of the AF that is free of cord and limbs, if it is more
than 8 cm in vertical length is indicative for polyhydramnious
o AFI (amniotic fluid index) if > 23 cm
Differential diagnosis:
o Wrong dating
o Coexisting ovarian cyst
o Multiple pregnancies
o Abruption placenta
Effects on pregnancy and labor:
o Preterm labor
o Risk of placenta abruption and cord prolapse
o Fetal mal-presentation
o PPH
o perinatal mortality
Treatment: termination of pregnancy if there is any gross fetal abnormalities
24
#Involution of the uterus
It takes 6 weeks for the uterus to return to its normal status after the delivery
Postoperatively in a patient with a cesarean section, the fundal height is felt at about
2 cm below the umbilicus
Delayed involution (the fundal height is more than expected) caused by:
o Full bladder
o Infection (endometritis or pancreatitis)
o Fibroids
o Broad ligament hematoma
o Retained pieces of the placenta (the most common cause of sub involution uterus
in a normal vaginal delivery (NVD)
o Loaded bowel (Loaded rectum)
Clinical features:
o Pallor (anemia)
o Fever
o Tachycardia
o Tender abdomen
o Vaginal bleeding with offensive discharge
Investigations:
o Blood culture
o Genera urine examination
o High vaginal swap
Treatment required evacuation, including:
o Dilatation
o Pitocin + ergot: to stimulate uterine contractions and decrease bleeding
o Antibiotics
o Anti-D: in an Rh -ve mother
#Cephalopelvic disproportion (CPD)
Occurs when a baby’s head or body is too large to fit through the mother’s pelvis. It
is believed that true CPD is rare, but many cases of “failure to progress” during labor
are given a diagnosis of CPD. When an accurate diagnosis of CPD has been made, the
safest type of delivery for mother and baby is a cesarean.
Possible causes of cephalopelvic disproportion (CPD) include:
o Large baby due to:
Hereditary factors
Diabetes
Post-maturity
Multiparity
o Abnormal fetal positions

25
o Small Pelvis
o Abnormally shaped pelvis
Diagnosis:
o The diagnosis of cephalopelvic disproportion is often used when labor progress is
not sufficient and medical therapy such as use of oxytocin is not successful or not
attempted. CPD can rarely be diagnosed before labor begins even if the baby is
thought to be large or the mother’s pelvis is known to be small. During labor, the
baby’s head molds and the pelvis joints spread, creating more room for the baby
to pass through the pelvis.
o Ultrasound is used in estimating fetal size but not totally reliable for determining
fetal weight.
o A physical examination that measures pelvic size can often be the most accurate
method for diagnosing CPD.
o If a true diagnosis of CPD cannot be made, oxytocin is often administered to help
labor progression or the fetal position is changed.
Criteria for CPD in nulliparous women Caesarean section for little or no progress
over 2-4 hours with adequate uterine contractions and the cervix at least 3 cm
dilated.
#Fetal Growth Restriction (FGR)
DEFINITION: Fetus whose growth velocity slows down or stops completely because
of inadequate oxygenation or nutrition supply or utilization
AETIOLOGY:
o MATERNAL FACTORS: Nutrition: BMI<19 starvation, Smoking: 460 gm lighter than
fetus with nonsmoker woman, Alcohol and drug abuse, Maternal therapeutic
drugs e.g. B blockers & Anticonvulsant , Maternal diseases (Cardiorespiratory
compromise Sickle cell dis, Collagen vascular disease, Maternal DM, Maternal
chronic hypertension, Abnormalities in the uterus)
o FETAL FACTORS: Fetal abnormalities (Chromosomal, Structural, Cardiac disease,
Gastroschisis) Infection (Varicella, CMV, Rubella, Syphilis, Toxoplasma, Malaria)
o PLACENTAL FACTORS: Placental mosaicisim –16,22 chromosome , PE -- ↓ blood
supply to placental bed
PREDICTION: BMI<19, Smoking, Past history of FGR, Congenital uterine
abnormalities, Big fibroid, Old mother>40 nulliparous, PE, Retro placental
hemorrhage in 2nd & 3rd Trim , Maternal serum screening : 2nd Tim (Alfa Feto
Protein (AFP) , E3 , Human Placental Lactogen , hCG), ULTRASOUND MARKERS
CLINICAL ASSESSMENT: Weight gain in pregnancy, Fundal height, Clinical weight
estimation of the fetus – liquor amount estimation, U/S assessment, Biometrical
measurement of the fetus, Umbilical artery Doppler velocity study

26
PROPHYLAXIS: Small dose aspirin, Protein energy, Stop smoking, Anti malaria, Stop
medications
LABOR: <37wk → C/S because at high risk of hypoxia & academia, If >37wk→
induction – continuous CTG, fetal scalp monitoring
Not all FGR are SGA or all SGA are FGR:
o SGA can be categorized according to the etiology into:
Normal SGA: No structural anomalies, normal liquor, normal Doppler study of
umbilical artery & normal growth velocity.
Abnormal SGA: those with structural or genetic abnormalities
FGR: those with impaired placental function identified by abnormal UADW &
reduced growth velocity.
o SGA is divided into symmetrical or unsymmetrical according to Biometrical
measurement
#Intrauterine death (still birth)
DEFINITION: Baby delivery at 24wk complete with no sign of life
AETIOLOGY:
o MATERNAL FACTORS: Obstetric. Cholestasis, Metabolic disturbances (DM
Ketoacidosis), Reduced oxygen saturation (Cystic fibrosis, Sleep apnea) , Uterine
abnormalities, Ascherman syndrome, Antibodies production (Rh, Platelet)
Alloimmunization, Congenital heart block
o FETAL FACTORS: Cord accident, Fetofetal transfusion, Feto maternal hemorrhage,
Chromosomal and genetic diseases, Structural abnormalities, Infection, Anemia of
fetal origin
DIAGNOSIS: ↓ FM, Routine U/S, Abruption or ruptured membrane, Color Flow
Mapping is definitive
INVESTIGATION: Kleihauer test, Full blood count with platelet, Blood gr, Antibody
screen, Urea & Creatinine, LFT, Uric acid, Bile acid, Syphilis & Parvovirus & CMV &
Toxoplasma serology
HOW TO DELIVER?
o Over 90% of women will deliver spontaneously within 3 weeks, conservative
management is an option that can be offered
o Vaginal delivery is the best option unless there is obstetric indications
o Induction of labor : A standard protocol for mifepristol induction, Prevention of Rh
iso immunization, Contraception, Psychological support, Follow up
27
#Partograph (partogram)
DEFINITION: Is a graph used in labor to monitor the parameters of progress of labor,
maternal and fetal wellbeing, and treatment administration
PRACTICAL VALUE OF USING THE PARTOGRAM:
o Offers an objective basis for overtime monitoring the progress of labor, maternal
and fetal wellbeing.
o Enables early detection of abnormalities of labor
o Prevention of obstructed labor and ruptured uterus.
o Useful in reduction of both maternal and perinatal mortalities and morbidities
COMPONENTS (Parts):
o Patient identification
o Time: It is recorded at an interval of one hour. Zero time for spontaneous labor is
time of admission in the labor ward and for induced labor is time of induction.
o Fetal heart rate: It is recorded at an interval of thirty minutes.
o State of membranes and color of liquor: "I" designates intact membranes, "C"
designates clear and "M" designates meconium stained liquor.
o Cervical dilatation and descent of head
o Uterine contractions: Squares in vertical columns are shaded according to
duration and intensity.
o Drugs and Fluids
o Blood pressure: It is recorded in vertical lines at an interval of 2 hours.
o Pulse rate: It is also recorded in vertical lines at an interval of 30 minutes.
o Oxytocin: Concentration is noted down in upper box; while dose is noted in lower
box.
o Urine analysis
o Temperature record
ADVANTAGES:
o Provides information on single sheet of paper at a glance
o No need to record labor events repeatedly
o Prediction of deviation from normal progress of labor
o Improvement in maternal morbidity, perinatal morbidity and mortality
Lines:
Alert line: means we should do other assessments
Active line: means we should do some actions like dilation of cervix or rapture of
membranes or cesarean section or another things

28
#Ectopic pregnancy
DEFINITION: It is one in which a fertilized ovum implant & being to develop before it
reaches its natural site in the uterus. An extra uterine gestation can develop in the
ovary or in the peritoneal cavity , but 97% of ectopic pregnancy occur in the fallopian
tubes ,most commonly in the ampullary portion
CAUSES: A tubal pregnancy — the most common type of ectopic pregnancy —
happens when a fertilized egg gets stuck on its way to the uterus, often because the
fallopian tube is damaged by inflammation or is misshapen. Hormonal imbalances or
abnormal development of the fertilized egg also might play a role.
SYMPTOMS: Severe abdominal or pelvic pain accompanied by vaginal bleeding,
Extreme lightheadedness or fainting, Shoulder pain
TREATMENT: A fertilized egg can't develop normally outside the uterus. To prevent
life-threatening complications, the ectopic tissue needs to be removed. If the ectopic
pregnancy is detected early, an injection of the drug methotrexate is sometimes used
to stop cell growth and dissolve existing cells.
#Hydatidiform Mole
DEFINITION: This is an abnormal conceptus in which an embryo is absent & the
placental villi are so distended by fluid that they resemble a bunch of grapes. No
trace of an embryo, amniotic sac or umbilical cord is apparent.
CAUSES: A molar pregnancy is caused by an abnormally fertilized egg. Human cells
normally contain 23 pairs of chromosomes. In a complete molar pregnancy, all of the
fertilized egg's chromosomes come from the father. In a partial or incomplete molar
pregnancy, the mother's chromosomes remain but the father provides two sets of
chromosomes. As a result, the embryo has 69 chromosomes instead of 46.
SYMPTOMS: Dark brown to bright red vaginal bleeding during the first trimester,
severe nausea and vomiting, sometimes vaginal passage of grape-like cysts, rarely
pelvic pressure or pain.
TREATMENT: Dilation and curettage (D&C), Hysterectomy, HCG monitoring
#Fetal distress
DEFINITION: Compromise of a fetus during the antepartum period (before labor) or
intrapartum period (during the birth process). The term fetal distress is commonly
used to describe fetal hypoxia (low oxygen levels in the fetus), which can result in
fetal damage or death if it is not reversed or if the fetus is not promptly delivered.
CAUSES: Breathing problems, Abnormal position and presentation of the fetus,
Multiple births, Shoulder dystocia, Umbilical cord prolapse, Nuchal cord, Placental

29
abruption, Premature closure of the fetal ductus arteriosus, Uterine rupture,
Intrahepatic cholestasis of pregnancy, a liver disorder during pregnancy.
SYMPTOMS: Decreased movement felt by the mother, Meconium in the amniotic
fluid, Non-reassuring patterns seen on cardiotocography (increased or decreased
fetal heart rate, decreased variability, late decelerations), Biochemical signs (fetal
metabolic acidosis, elevated fetal blood lactate levels).
TREATMENT: rapid delivery by instrumental delivery or by caesarean section if
vaginal delivery is not advised.
#Changes in pregnancy
Changes in circulatory system:
o ↑ Heart rate (10–20 per cent).
o ↑ Stroke volume (10 per cent).
o ↑ Cardiac output (30–50 per cent).
o ↓ Mean arterial pressure (10 per cent).
o ↓ Pulse pressure.
o Maternal haemoglobin levels are decreased because of the discrepancy between
the 1000 to 1500 mL increases in plasma volume and the increase in erythrocyte
mass, which is around 280 mL. Transfer of iron stores to the fetus contributes
further to this physiological anemia.
o Palpitations are common and usually represent sinus tachycardia, which is normal
in pregnancy.
o Edema in the extremities is a common finding, and results from an increase in
total body sodium and water, as well as venous compression by the gravid uterus.
Renal changes:
o ↑ Kidney size (1 cm).
o Dilatation of renal pelvis and ureters.
o ↑ Blood flow (60–75 per cent).
o ↑ Glomerular filtration (50 per cent).
o ↑ Renal plasma flow (50–80 per cent).
o ↑ Clearance of most substances.
o ↓ Plasma creatinine, urea and urate.
o Glycosuria is normal.
o Urine output increase in first trimester, slightly decreased in the second
trimester and increase again in the third trimester
Hormonal changes: increase of estrogen, progesterone, secretion of hCG and Human
chronic lactogen, increase production of corticotrophin, thyrotropin and prolactin,
while FSH and LH decrease, Increase secretion of glucocorticoids and aldosterone,
and increase secretion of thyroxin, Parathyroid increase, Increase secretion of
vasopressin.

31
#Clinical presentation (sign & symptoms) of gestational diabetes:
Usually there are no symptoms, or the symptoms are mild and not life threatening to
the pregnant woman. The blood sugar (glucose) level usually returns to normal after
delivery.
Effects on fetus: abortion, metabolic upset, increase the incidence of congenital
abnormalities, larger baby
Effects on mother: complications of D.M like UTI, candidiasis of vulva and vagina,
hydramnios, retinopathy, nephropathy
Effects on baby: larger size and organs and skeleton (no edema), immaturity
(neurological and metabolic), respiratory distress syndrome
Complications:
o Macrosomic baby (big baby for his gestational age) macrosomia > 4.5 kg at
birth
o Hypoglycemic baby in the future, so we should give him IV glucose via the
umbilical vein
Symptoms may include:
o Blurred vision
o Fatigue
o Frequent infections, including those of the bladder, vagina, and skin
o Increased thirst
o Increased urination
o Nausea and vomiting
o Weight loss despite increased appetite
31
Part:4
Obstetric
Notes
#The effect of mother age on the pregnancy:
Risk of teenager mother:
1- Increase the incidence of preterm labor
2- Increase the incidence of abortion
3- Increase the incidence of pre-eclampsia
4- Increase the incidence of contracted pelvis
5- Risk of caesarian section
Risk of mother above 35 years:
1- Hypertension
2- Down's syndrome
3- D.M
4- Increase risk of caesarian section
5- Congenital anomalies
6- Contracted pelvis (( increase weight of baby (200gm every pregnancy) and increase
the spondylolisthesis shortenings of pelvic inlet ))
Vaginal bleeding in 20 years old patient may be due to menstruation or may occur in
pregnancy, but in a 60 years old patient it is an abnormal condition
#The effect of occupation on the pregnancy:
Exposure to toxic substances at occupation
Irradiation
Heavy work by the mother may lead to abortion or preterm labor
#Ultrasound during pregnancy
Early ultrasound (in the first trimester):
o Know Site of pregnancy (normal – ectopic)
o Know number of fetuses
o Fetal Viability
o Gestational age (G.A)
o To detect any anomaly
o Polyhydramnious (access of amniotic fluid)
Anomaly ultrasound (18-20 weeks)
o Detection of congenital anomalies
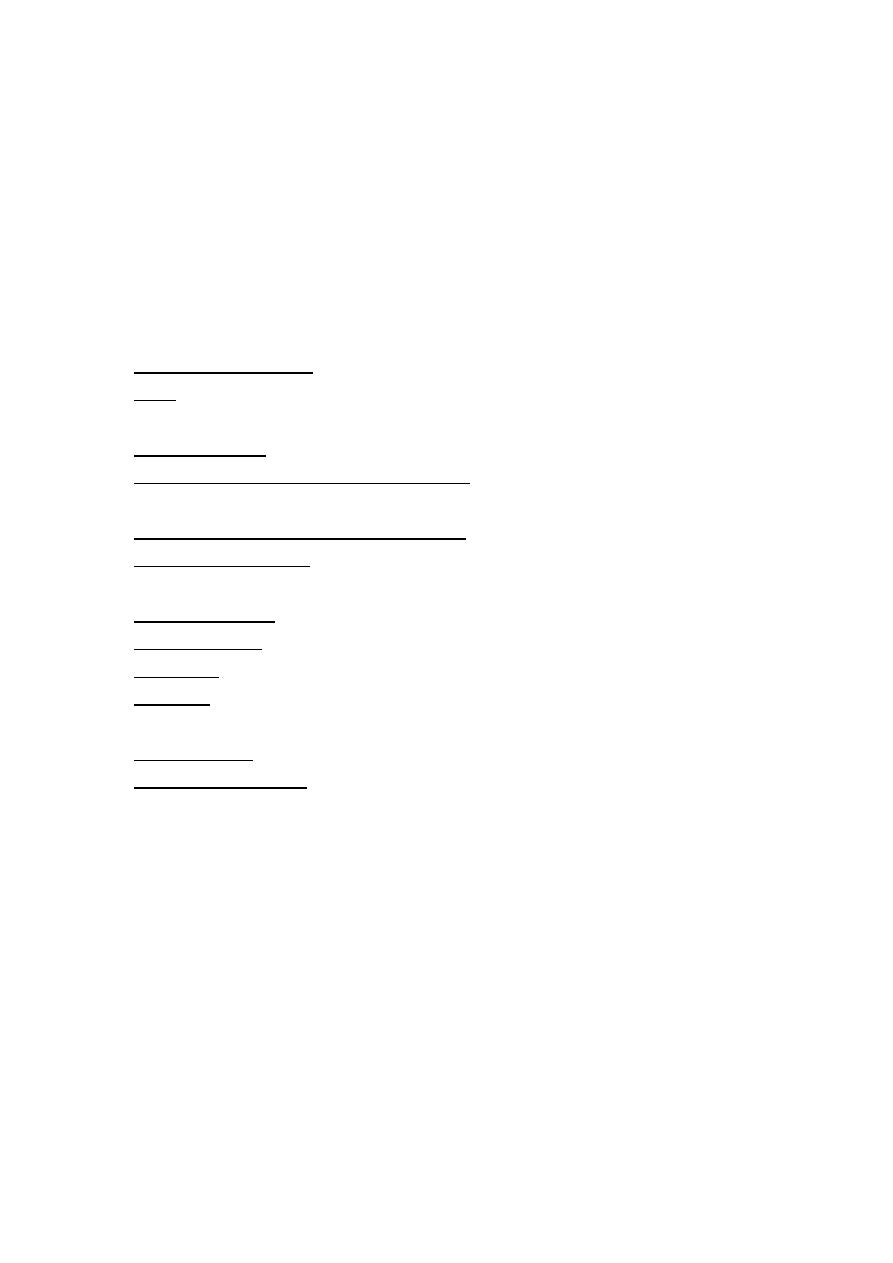
Week
Month
Trimester
4-8 week
1 month
First T.
8-12 week
2 month
12-16 week 3 month
16-20 week 4 month
Second T.
20-24 week 5 month
24-28 week 6 month
28-32 week 7 month
Third T.
32-36 week 8 month
36-40 week 9 month
In gynecology
9
weeks =
2
months
13
weeks =
3
months
Because regular cycle is 28 days

32
o Gestational age
o Twins
Late ultrasound (in the third trimester)
o oligo or poly hydroaminous
o position of the placenta
o fetal well being
#Infertility:
Primary infertility refers to mother who has not become pregnant after at least 1
year
Secondary infertility refers to mother who has been able to get pregnant at least
once, but now are unable.
#Effects of smoking on pregnancy:
Increase incidence of abortion
Intrauterine death
Early post-delivery death
Abnormality in the G.A
#Conditions that may repeated in next pregnancies:
Pre-term
Placenta previa
Placenta abrabeta
Pre-eclampsia
D.M
P.P.H
Ectopic pregnancy
#Efficient uterine contractions:
Number of contractions (normally less than 5)
Duration of contraction (normally 45-60 seconds)
#Management of placenta praevia:
ABC
Catheter
I.V cannula
Resuscitation
Augmentation of the labor
33
#Placenta praevia VS Placenta abruption
Placenta praevia
Placenta abruption
Pain
Painless
Constant pain
Blood
Bright red blood, slight bleeding
at beginning, no hypertension
Dark blood, usually profuse
bleeding, there is hypertension
Obstetric shock
Obstetric shock in proportion to
amount of vaginal loss
The actual amount of bleeding may
be far in excess of vaginal loss
Uterus
Uterus is non-tender and soft
Uterus is tender and tense and
tetanically contract
Fetus
May have abnormal
presentation and/ or lie
Fetal movement is +ve
Normal presentation and lie
The fetal movement is lost
Fetal heart
In general, fetal heart normal
Fetal heart distressed/absent
Protein in urine
Not present
Usually found
Clotting
Normal clotting mechanism
Abnormal and defective
Associated
problems
Small antepartum hemorrhage
may occur before larger bleed
May be a complication of pre-
eclampsia, may cause
disseminated intravascular
coagulation
#Oxytocic agents:
Oxytocin: could be given in early stages of labor
(contraindicated in Hypertension and heart disease)
Methergin: contraindicated in early stages of labor
#Causes of vaginal bleeding for 2 days:
Abortion
Ectopic pregnancy
H.mole
Blood diseases
Incidental (related to cervix and vagina
#Cases that could be encountered in the first trimester:
Repeated vomiting (morning sickness or hyperemesis gravidarum)
Bleeding (Threatened abortion: the fetus is a life and the color is bright red or Missed
abortion: the fetus is dead and the color is dark red)
Pain + bleeding ectopic pregnancy
#Causes that could be encountered in the second trimester:
Threatened abortion (until 24 weeks)
Bleeding (from 24-40 weeks called antepartum hemorrhage)
34
#Causes that could be encountered in the third trimester:
Pain: could be due to uterine contraction or medical condition like UTI
Essential hypertension
The pain could be due to premature labor (24-37 weeks)
#The symptoms of pregnancy with live fetus:
Breast tenderness
Morning sickness
Abdominal pain: mild, lower abdominal, radiate to the back and loins, aggravate by
working, relieved by rest
#Causes of abdominal pain:
In the first trimester: threatened abortion, ectopic pregnancy, UTI
In the second trimester: uterine contraction, threatened abortion, UTI
In the third trimester: uterine contraction, premature labor pain
#Notes on the menstruation:
Duration of the cycle: normally 21-35 days
Poly-menorrhea the cycle is less than 21 day
Oligo-menorrhea the cycle is more than 35 day
Amenorrhea: is the absence of a menstrual period in a woman of reproductive age
Duration of the menstrual phase: 2-8 days average 5 days
Amount of blood lost: normal range 30-80 ml
Inter-menstrual bleeding: this may occur normally at the time of ovulation, where
spotting may occur. Pain at the lower abdomen may accompany this bleeding.
#lochia:
The lochial discharge comes from the placental site
For the first 3 or 4 days the lochia is red in color (lochia rubra)
The become pink then white (lochia alba) at day 12-14 of delivery
#Stages of labor:
First stage (from start of labor until full cervical dilatation 10 cm)
Second stage (from full cervical dilatation until the fetus is born)
Third stage (stage of delivery of the placenta)
Forth stage (from delivery of the placenta to 1 hour)
#Pre-eclampsia and Eclampsia:
Pre-eclampsia (after 20 weeks)
hypertension (frontal headache) + proteinuria
(albumin in the urine) + edema (in the hand and face)

35
Eclampsia (after 20 weeks)
same as pre-eclampsia + fit
Other signs and symptoms of preeclampsia may include:
o
Excess protein in your urine (proteinuria) or additional signs of kidney problems
o
Severe headaches
o
Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
o
Upper abdominal pain, usually under your ribs on the right side
o
Nausea or vomiting
o
Decreased urine output
o
Decreased levels of platelets in your blood (thrombocytopenia)
o
Impaired liver function
o
Shortness of breath, caused by fluid in your lungs
#Signs of placental separation:
Lengthening of umbilical cord
Gush of blood
Fundus becomes globular and more anteverted against abdominal hand
#Controlled cord traction:
The placenta is delivered using one hand on umbilical cord with gentle downward
traction. The other hand should be on the abdomen to support the uterine fundus,
this is the active management of the third stage of labor
Risk factors for aggressive traction is uterine inversion
Normal duration between 0-30 min for both PrimiG and MultiG
#Benefits of catheter during labor:
Drainage of urine
Monitoring the urine output
Monitoring the renal function
#Edema:
Leg edema is normally (physiologically) presented in pregnancy
Face or hand or sacrum edema is pathologic is pregnancy
#Fit in pregnancy:
The frequency of fits will increase
Some drugs of fits will affect the fetus so should be stopped or changed to other
types or change the dose

36
#Fetal presentation and lie:
Presentation: the lower part of the fetus occupying the lower part of the canal in
many presentations like: vertex, breech, shoulder, compound and funic
Fetal lie: relation of the longitudinal axis of the fetus to the longitudinal axis of the
mother, it could be longitudinal, transverse or oblique
Note: management of breech presentation is by external cephalic version or cesarean section
#Blood test
is earlier diagnose the pregnancy than urine test
#ANC (Ante Natal Care):
Pregnant mother should go to the hospital one time every month in the first 6
months
And go one time every two weeks in the 7 and 8 month
And go one time every week in the last (9) month
#Curettage:
Is a procedure to remove tissue from inside your uterus. Doctors perform curettage
to diagnose and treat certain uterine conditions — such as heavy bleeding — or to
clear the uterine lining after a miscarriage or abortion.
Risks: Perforation of the uterus, Damage to the cervix, Scar tissue on the uterine wall,
Infection
#Post-operative paralytic ileus:
Due to hypokalemia& manipulation
Postoperative ileus is thought to result from inflammation, deranged neural input, or
medications taken in conjunction with surgery. Large-volume intraoperative fluid
resuscitation and prolonged procedure time associated with extensive dissection may
contribute to the development of these events.
#Clinical presentation (sign & symptoms) of anemia during pregnancy:
Pale skin, lips, and nails
Feeling tired or weak
Dizziness
Shortness of breath
Rapid heartbeat
Trouble concentrating
#Conditions of Normal vaginal delivery:
1-normal pregnancy without usage of drugs that induced pregnancy
2-not use oxytocin for induction of the labor
3-not use vacuum or forceps in labor

37
4-No vaginal tear
5-No cervical tear
6-No artificial rupture membrane
7-No bleeding after delivery
8-No any compliant to mother
9-No any compliant to baby
#Usually labor pain described as following:
Lower abdominal pain
Radiate to back and upper thigh
Gradual, progressive and intermittent
Increase in frequency and duration
Colicky and so severe
Interrupt other personal activities
Associated with nausea, vomiting and blurred vision
#Types of contraception:
Mechanical: intra-uterine contraceptive device IUCD ( )لولب
Oral contraceptive pills: combined contraceptive pills (estrogen+progesterone) or
progesterone only pills
Injectable drug: hydroxyprogesteron acetate injection
Barrier: vaginal cap or condom
#Maternal bleeding VS fetal bleeding:
Fetal bleeding usually little in volume but can quickly compromises the fetus life,
while maternal bleeding usually more sever.
By adding strong alkaline (APT Test) to the blood, maternal blood will be lysed and
appear as ghost cells, while fetal blood will stay longer (fetal Hb is HbF)
#Differential diagnosis of pain at term:
Labor pain
Accidental hemorrhage
Uterine contraction
Polyhydramnious
Ovarian cyst
Fibroid
UTI
Gastroenteritis

38
#Differential diagnosis of bleeding in early pregnancy:
Miscarriage
Ectopic pregnancy
Molar pregnancy
Cervical lesions (erosion, adenomatous polyp, carcinoma of the cervix)
#Differential diagnosis of vaginal bleeding in late pregnancy:
Placenta Previa
Placental abruption
Cervical lesions (erosions, polyps, cancer)
Trauma
Filamentous insertion of the umbilical cord
#Causes of bleeding and vomiting in early pregnancy:
Hyper-emesis gravidarum
UTI
Appendicitis could cause the vomiting
GIT infection
Rare (bowel obstruction, hepatic disorder, cerebral tumor)
#The risk of ante-Partum hemorrhage:
Lead to shock (hypovolemic shock)
Renal failure
DIC
Fetal hypoxia
Intra-uterine fetal death
#Differential diagnosis for no feeling of fetal movement for one day:
Prolonged fetal sleep
Fetal compromise
Fetal death
#Differential diagnosis of pregnancy
Cessation of menses psychological disorders, endocrine disorders (thyrotoxicosis)
metabolic disorders, chronic illnesses
Nausea and vomiting GIT disturbances, other surgical and medical causes
Polyuria and Frequency UTI, other urinary disorders like tumors and stones
Enlarged uterus abdominal and pelvic tumors like ovarian tumor and fibroid

39
#Contracted pelvis
In android pelvis
Not delivered vaginally, but always by caesarian section
Clinical hints that indicate contracted pelvis:
o Failure of engagement (especially in primi)
o Early rapture of membrane
#Cusses of post-operative sepsis (fever)
Breast engorgement
UTI
GTI
Wound infection
RTI (chest)
DVT
#Wrong dating (LMP) occur in
OCP oral contraceptive pills
Lactational amenorrhea
Hormonal replacement therapy
Irregular cycle
#Causes of puerperal pyrexia
Birth canal infection (puerperal sepsis)
UTI
Breast infection
Thrombophlebitis
Other causes of pyrexia (DVT)
#Booking visit
DEFINITION: is the first official check-up in pregnancy.
INVESTIGATION:
o Blood test: blood group, check for infections (HIV, Rubella, Measles, HBV)
o Urine test: check pre-eclampsia and gestational diabetes
o Blood pressure test: Raised blood pressure, especially later on in the
pregnancy, can be an early warning sign of pre-eclampsia.
o Ultrasound: measures baby size to confirm the gestational age and to
calculate the delivery date
41
#Mixed notes:
Episiotomy
used in fetal distress
instrument
used when the head of fetus is delivered but the shoulder impact
Why CS patient should walk as soon as possible after surgery? To prevent DVT
Why we put Foley's catheter before CS? To evacuate the bladder to prevent its injury
Continuous not treated pain lead to rapture uterus that lead to fetal distress and
death, so doctor should do repair with tubal ligation or partial caesarian
hysterectomy (surgical removal of the uterus)
Bleeding during first month could be threatened abortion
Auscultation of the fetal heart by: Pinard (24-26 weeks) or Sonic aid (12-14 weeks)
If the patient has previous one CS we should give her chance to have vaginal delivery,
but if the patient has 2 previous CS the third pregnancy mostly be CS
In pregnancy joint pain is normal due to relaxin hormone release
