1
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
SYSTEMIC PATHOLOGY OF CENTRAL NERVOUS SYSTEM
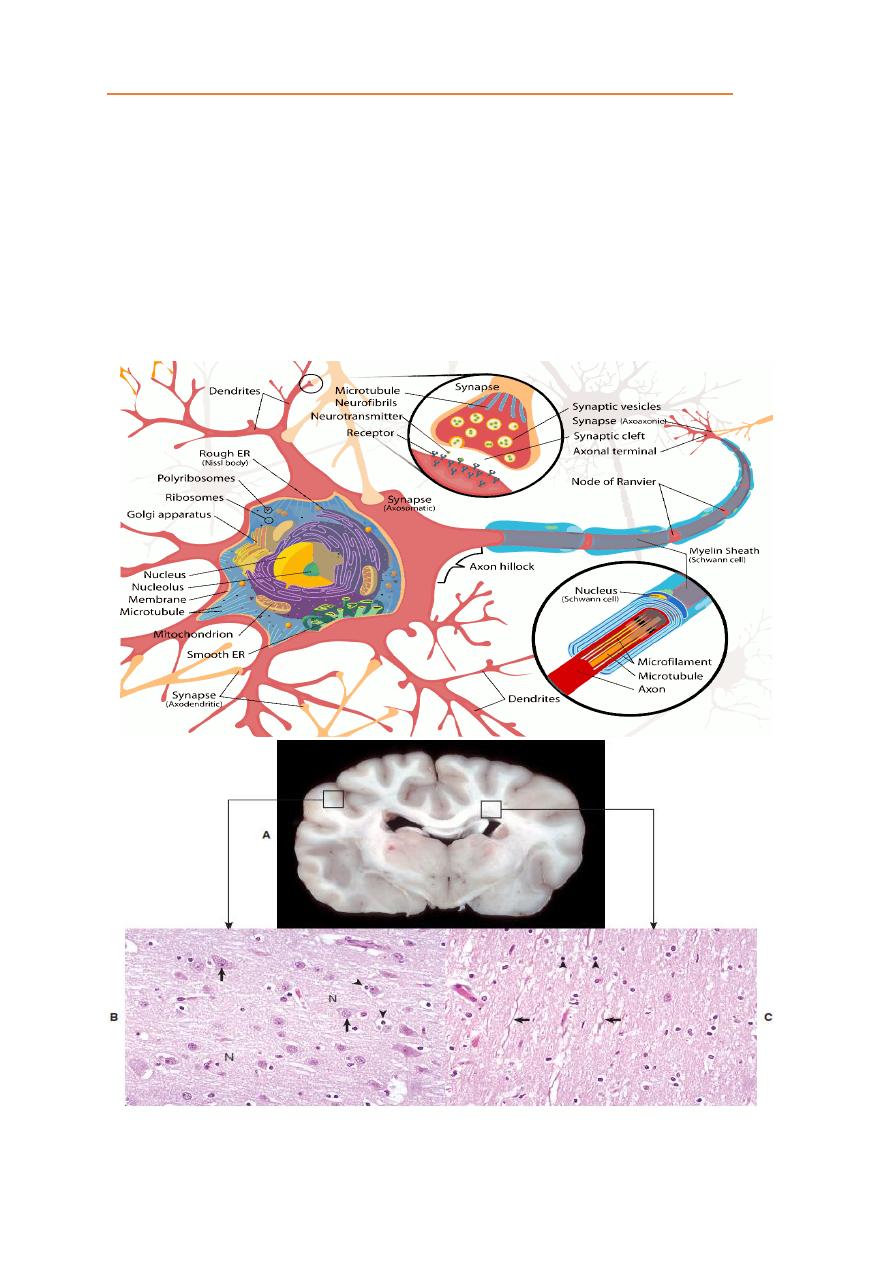
The central nervous system (CNS) brain, spinal cord and meninges. The
CNS is arranged to form two basic parts: the gray and white matter. In the CNS,
gray matter is found in the cerebral cortex, the gray matter is composed from
neuronal cell bodies. The white matter consists of neuronal axons that arise from
neuronal cell bodies in the gray matter and terminate distally. In the spinal cord,
white matter is located peripherally surrounding the gray matter.
The exterior of the CNS is covered by the meninges. The meninges consist
of three layers named from out to in layers as the dura mater, arachnoid, and pia
mater. The arachnoid and pia enclose the subarachnoid space.
Brain: White and Gray matter (Grossly and Microscopically)
2
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Spinal Cord: White and Gray matter (Grossly and Microscopically)
CNS Meninges: 1) Dura mater, 2) Arachnoid, 3) Pia mater.

3
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Apoptotic Cell Death (Programmed Cell Death)
Apoptosis is a single cell-initiated, gene-directed cellular, self-destructive
regulatory mechanism that leads to “programmed” cell death. This mechanism is
used:
(1) During the development of the nervous system to ensure proper migration and
orientation of cell layers and removal of excess embryonic cells.
(2) To remove “aged” cells (i.e., cell turnover).
(3) To maintain cell number homeostasis in organ systems that have regenerative
capacity.
Necrotic Cell Death
Necrosis is a process that usually affects groups of cells in contrast to single
isolated cells as observed in apoptosis. Necrosis is characterized by the following
sequence: hydropic degeneration, swelling of mitochondria, pyknosis and
fragmentation of the nucleus, and eventual cell lysis caused by cell membrane
damage and the inability of the plasma membrane to control ion and fluid
gradients. Cellular debris associated with necrotic neuronal death will illicit an
inflammatory response in contrast to apoptotic neuronal death.
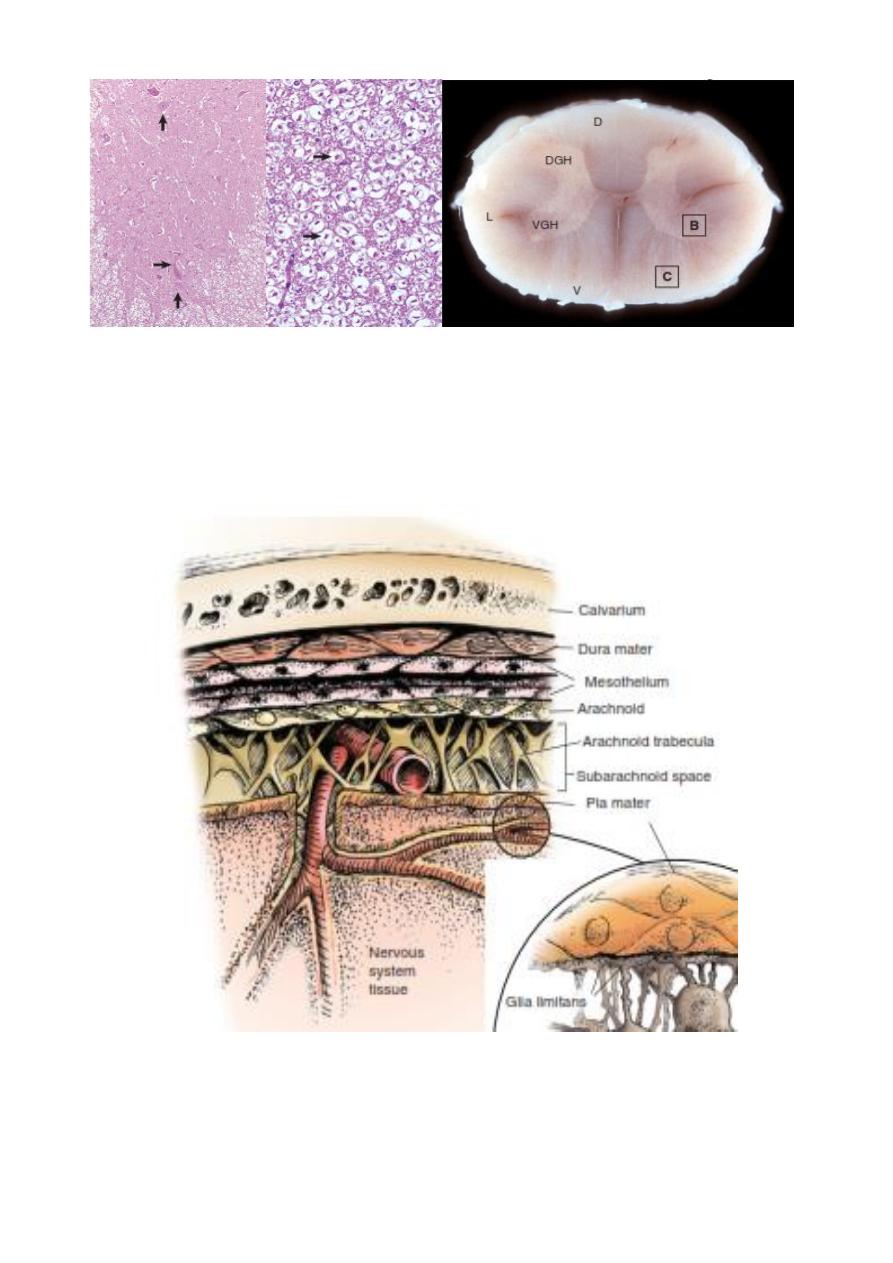
Wallerian Degeneration
Injury to axons of the CNS can result from a variety of causes such as:
(1) traumatic transection leading to Wallerian degeneration;
(2) compression and crushing;
(3) therapeutic neurectomies;
(4) nerve stretching injury; and
(4) intoxication.
The sequence of Wallerian degeneration includes the following:
1. Degeneration and fragmentation of axon and myelin within several days.
Proximal segment degenerates back to the next node of Ranvier, but all the
distal segment dies.
2. Removal of axonal and myelin debris by phagocytosis. Some phagocytes are
from the blood and some phagocytosis is by Schwann cells. All of the debris
is cleared out tube within a few weeks.
3. Regeneration of axon if the endoneurium is intact to allow the axon of the
proximal segment to enter and slide down the tube.
4. Remyelinization by Schwann cells.
4
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Wallerian Degeneration in
Neurons
5
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
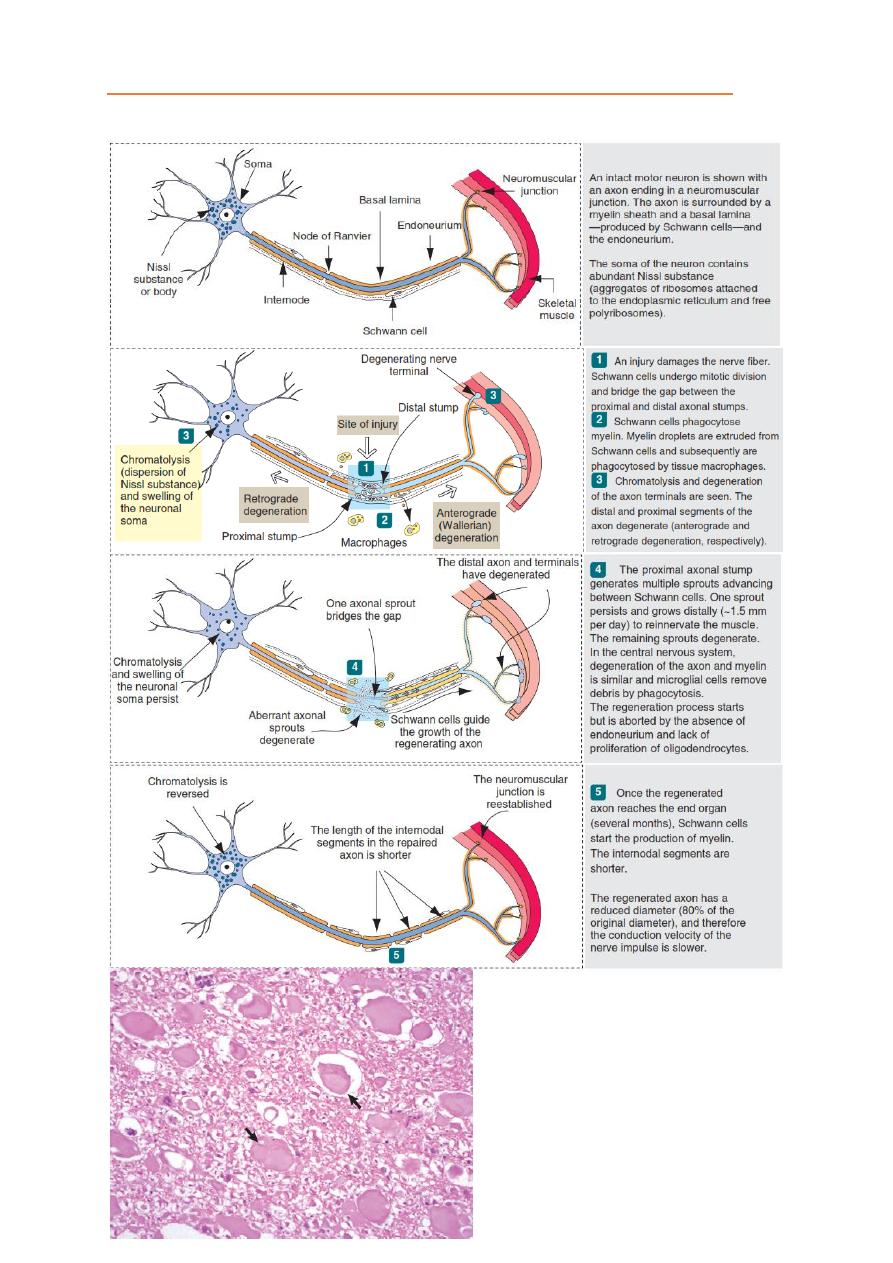
Astrocytes (Gimestocytes)
Microglial cell nodule.
Gitter cells (monocytes)

6
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
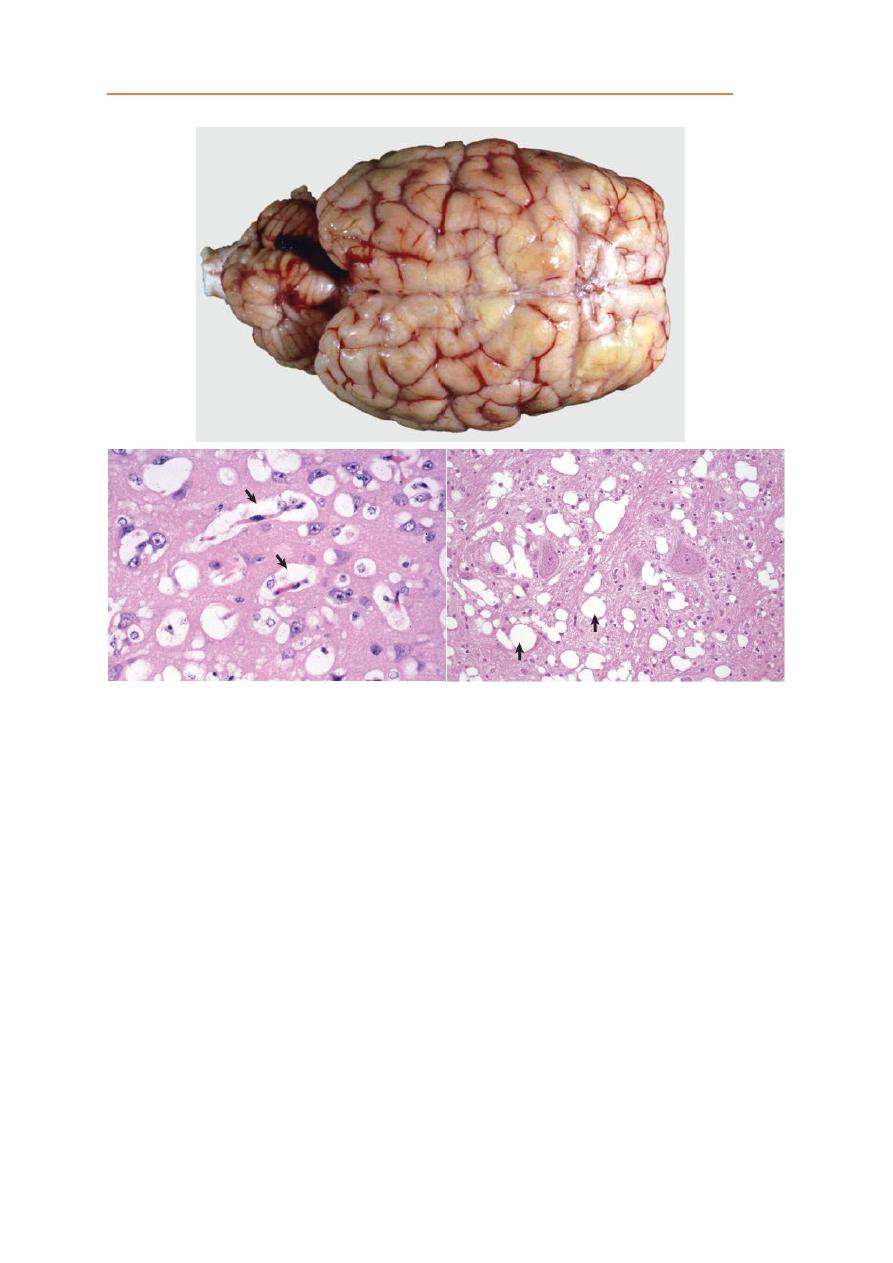
CNS Infarction
Infarction means necrosis of a tissue following obstruction (ischemia) of its
arterial blood supply. The rate at which ischemia occurs in the CNS determines
the degree of injury that follows. The more rapid the onset of ischemia, the more
severe the lesion. If the obstruction is sudden, as caused by an embolus, many of
the neurons can die within minutes and other components within hours. This
outcome also applies to compressive injuries to the CNS that produce a sudden
reduction in blood flow, such as can happen with sudden compression, but if the
blood flow through an artery is gradually reduced (as in arteriosclerosis) there is
sufficient time for anastomotic vessels to dilate and compensate.
The gross appearance of infarction may also differ according to location.
Lesions affecting the gray matter tend to be hemorrhagic, whereas infarction of
the white matter is often pale.
Cerebral Edema
There are two distinct types: (1) cytotoxic edema or cell swelling caused by
increased intracellular fluid with normal vascular permeability and (2) vasogenic
edema or tissue swelling caused by increased extracellular fluid resulting from
increased vascular permeability.
Vasogenic Edema:
is the most common type of edema in the CNS. It occurs
following vascular injury often adjacent to inflammatory foci, hematomas,
contusions, infarcts, cerebral hypertension, and neoplasms.
Cytotoxic Edema:
Cytotoxic edema is characterized by the accumulation of fluid
intracellularly in neurons, astrocytes, oligodendroglia, and endothelial cells
(called hydropic degeneration in other cells of the body) as a result of altered
cellular metabolism, often due to asphyxia.
7
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Encephalitis:
inflammation of cerebral.
Meningitis:
inflammation of meninges.
Encephalomeningitis:
inflammation of cerebral and meninges.
Cerebillitis:
inflammation of cerebellum.
Myelitis:
inflammation of spinal cord.
Encephalomyelitis:
inflammation of cerebral and spinal cord.
Ventriculitis:
inflammation of brain ventricles.
Medullitis:
inflammation of medulla oblongata.
Mesoneuritis:
Inflammation of a nerve without involvement of its sheath.
8
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Encephalitis:
It’s inflammation of cerebral part of brain. Depending on the type of antigen
and the pathogenicity of the infectious agent, the inflammatory response will
resolve (heal) or progress to a chronic or granulomatous phase with attempts at
resolution and clearance of the infectious agent. In the CNS, the type of
Inflammatory response can vary with the cause.
1. Serous to suppurative or purulent responses can be due to several species of
bacteria.
2. Eosinophil responses occur in salt poisoning and parasitic larval migration.
3. Lymphocytic, monocytic/macrophage, nonsuppurative, lymphomonocytic,
and lymphohistiocytic responses can be due to viruses and certain protozoa.
4. Granulomatous response can be due to fungi, certain protozoa, and some
higher-order bacteria, such as the Mycobacterium spp.

9
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Cerebellar Hypoplasia
In animals the most common causes of cerebellar hypoplasia are
parvoviruses, panleukopenia virus, canine parvovirus, pestiviruses, diarrhea
virus.
Grossly the size of the cerebellum is reduced; the reduction in size varies in
severity depending on the age and developmental stage of the brain when the
fetus or neonate is infected. Microscopically there is necrosis and loss of the
external granular layer and degeneration and loss of Purkinje cells.
10
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
Hydrocephalus
The most common congenital malformations and developmental anomalies,
hydrocephalus is the anomaly most likely to be caused in utero injury following
viral infection of the developing fetus. The type of hydrocephalus is depending
on where the occlusion is occurring:
1. Blockage of the interventricular foramen between a lateral and third ventricular
leads to unilateral dilatation of that lateral ventricle.
2. Blockage of both interventricular foramina leads to bilateral dilatation of both
lateral ventricles.
3. Blockage of the mesencephalic duct leads to bilateral dilatation of both lateral
ventricles, the third ventricle, and the segment of the mesencephalic duct
proximal to the blockage.
4. Blockage of the lateral apertures of the fourth ventricle leads to bilateral
dilatation of lateral ventricles, the third ventricle, the mesencephalic duct, and
the fourth ventricle.
5. Blockage of reabsorption leads to bilateral dilatation of lateral ventricles, the
third ventricle, the mesencephalic duct, the fourth ventricle, and the
subarachnoid space.
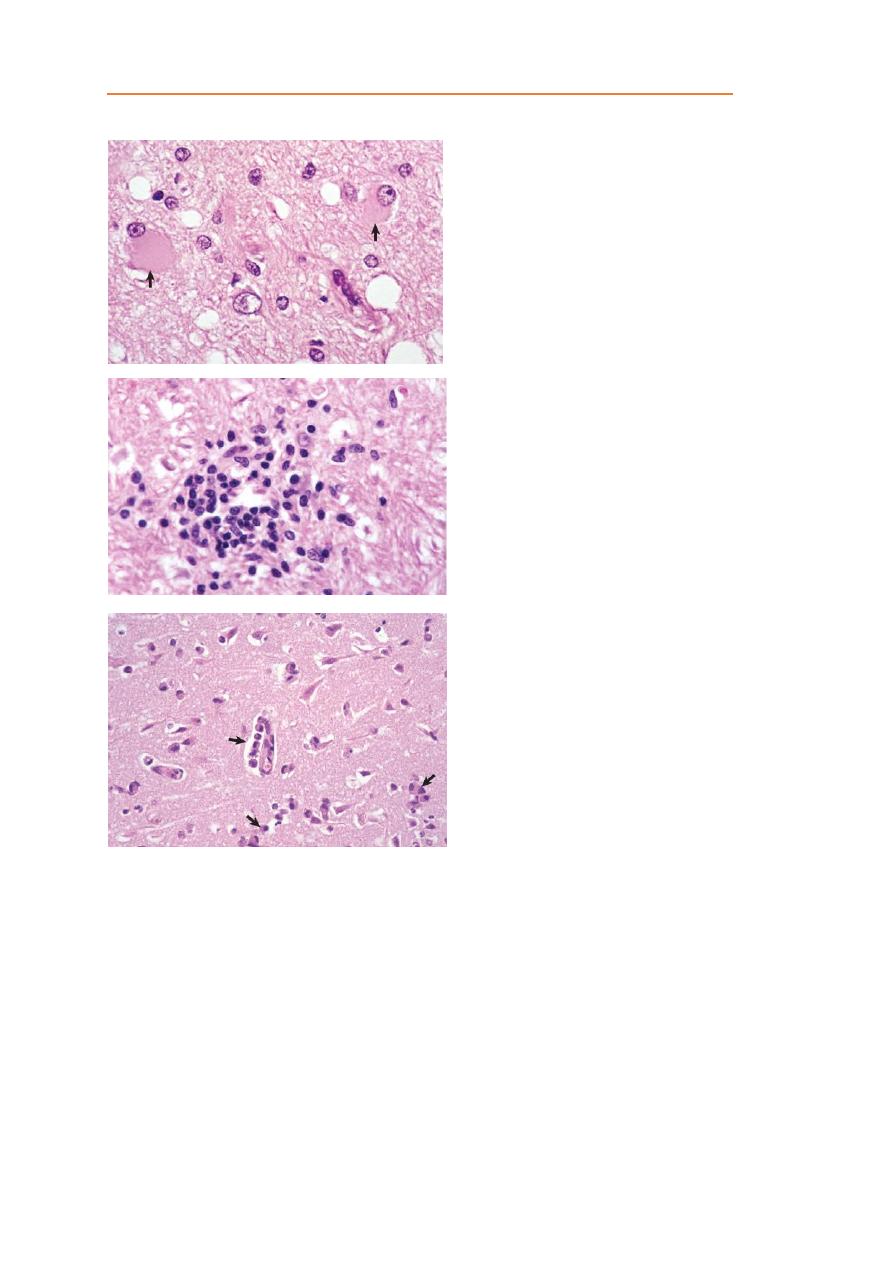
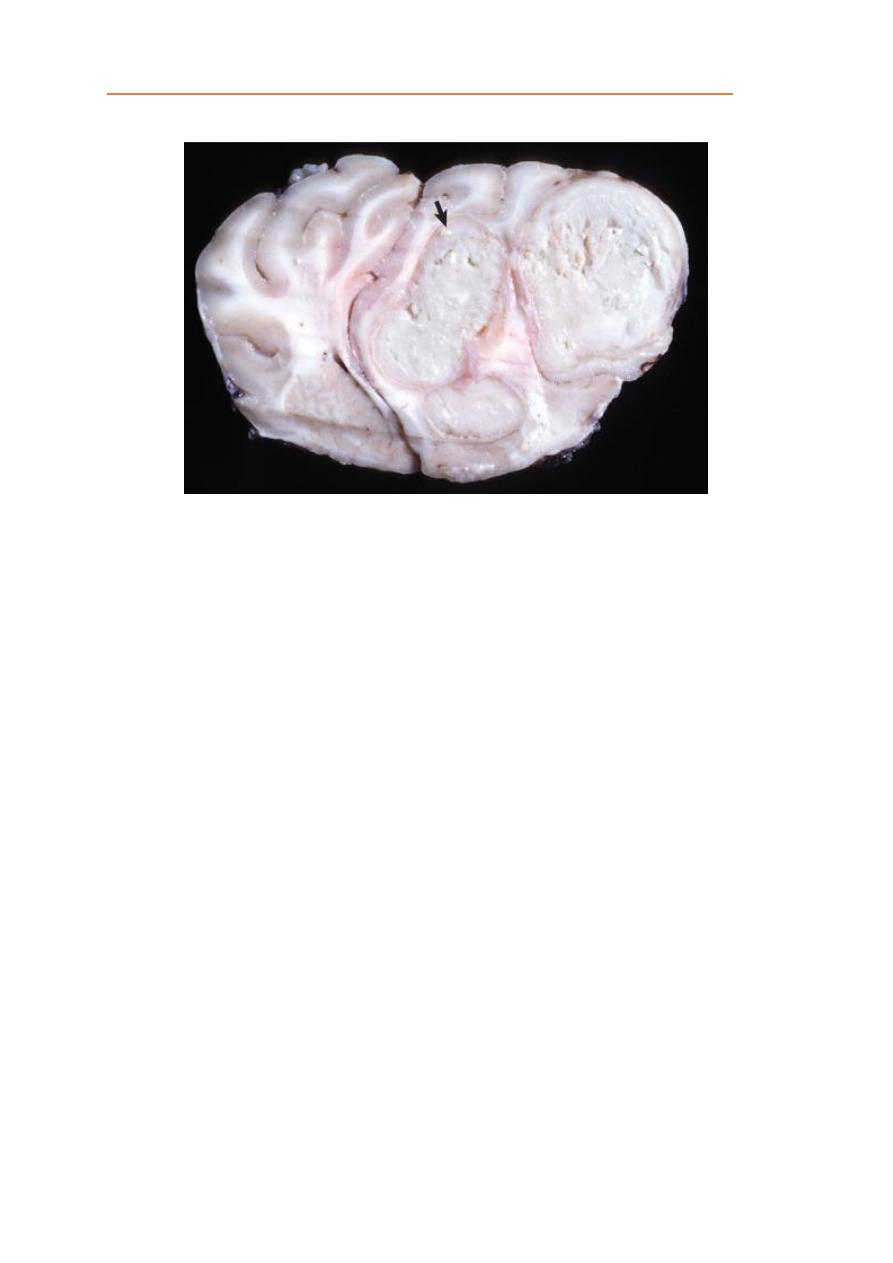
Brain Abscesses
Cerebral abscesses in animals are relatively uncommon but arise following
entry of bacteria into the CNS. This may occur either from direct extension or
hematogenously. With direct extension, abscesses occur following penetrating
wounds, such as calvarial fractures, or from spread of infection from adjacent
tissues such as the meninges, paranasal sinuses, and internal ear.
Grossly, brain abscesses can be single or multiple, be discrete or coalescing,
and have varied sizes. Abscesses consist of a white to gray to yellow, thick to
granular exudate. The color of the exudate can be influenced by pyogenic
bacteria. The borders of abscesses are often surrounded by a red zone of active
hyperemia induced by inflammatory mediators. With chronicity, abscesses may
be walled off by processes of astrocytes and fibrous connective tissue from the
pia mater, especially when the abscess results from a penetrating wound.
Streptococcus, Staphylococcus and Corynebacterium produce a pale-yellow to
yellow and watery to creamy exudate. Escherichia coli and Klebsiella produce a
white to gray and watery to creamy exudate. Pseudomonas produce a green to
bluish-green exudate.
Microscopically, early lesions consist of clusters of microglial cells. With
time, these lesions enlarge and contain variable numbers of neutrophils, but in
some foci macrophages can be the principal cell type. Necrosis and accumulation
of gitter cells can be prominent. Numerous gram-positive bacilli can be detected
in some lesions.
11
Systemic Pathology /
CNS System
/
Dr. Saevan Saad Al-Mahmood
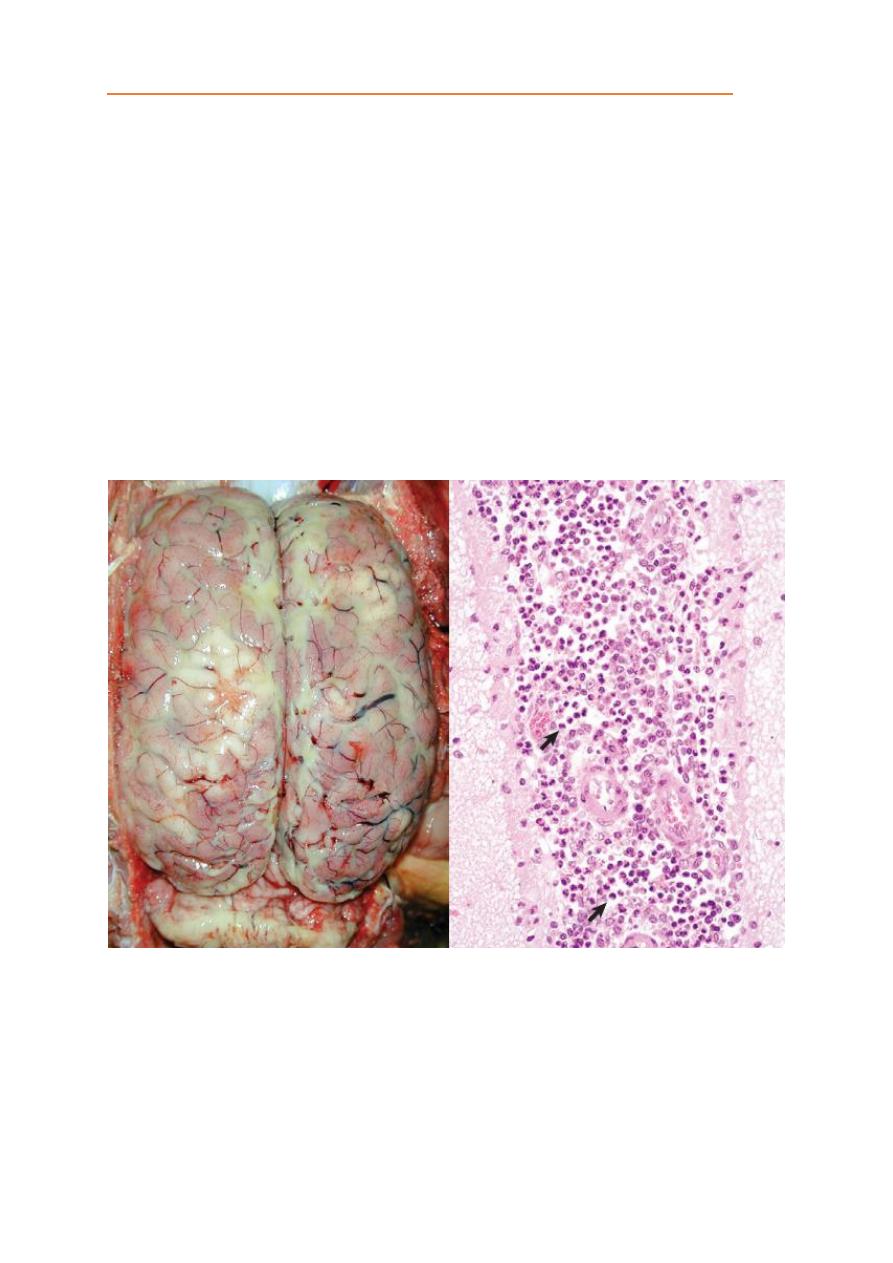
Meningitis
Meningitis refers to inflammation of the meninges. In animals, meningitis is
most commonly caused by bacteria such as Escherichia coli and Streptococcus
that traverse to the leptomeninges and subarachnoid space. The term meningitis
generally refers to inflammation of the leptomeninges (the pia mater,
subarachnoid space, and adjacent arachnoid mater) in contrast to inflammation of
the dura mater, which is referred to as pachymeningitis.
