1

2

3
Part:1
Pediatric
History of respiratory & CVS
Pediatric history related to respiratory system
#Ask about
Cough, sputum, Cyanosis, Shortness of breath, Noisy breathing
Sneezing, Expectoration, Hemoptysis, Post-tussive, Nasal discharge
Chest pain, Chest tightness (respiratory and cardiac problems)
Fever, Abdominal distention, Abdominal movement
Daily activity, Difficulty in feeding, Crying
#Cough
Source carina // center medulla oblongata
Onset (sudden, gradual)
Duration:
o < 2 weeks
acute (bronchiolitis, pneumonia, asthma)
o 2 weeks – 2 months
acute prolonged cough (pertussis, chronic sinusitis)
o > 2 months
chronic (foreign body, GERD, Tracheo-esophageal fistula, cystic
fibrosis, bronchiectasis, mucociliary dyskinesia)
Continuous or intractable
Wet or dry?
o If productive (with sputum) ask about: color, amount, consistency, contains blood
or clot
o If productive: mostly lower respiratory tract problem // dry: upper problem
Character:
o Group, LaryngeoTracheoBronchitis barking
o Pertussis paroxysmal post-tussive vomiting
o Bronchiolitis, asthma wheezing
Timing:
o Nocturnal allergy, asthma
o Midnight sinusitis
o Early morning Bronchiectasis, COPD, chronic bronchitis, adenoid, smoking
o Exercise asthma
o All over the day allergy, foreign body
Associated symptoms:
o Feeding may suggest Tracheo-esophageal fistula
o Suffocation, Apnea, Fever, Dyspnea

4
#Cyanosis
Bluish discoloration of skin and mucus membrane
Central or peripheral (lips, tip of tongue, peripheries)
Respiratory causes: T.B, respiratory distress syndrome, asthma, pneumonia,
pneumothorax, bronchiectasis, lung abscess, cystic fibrosis, asbestosis, familial (10%)
Acute cyanosis: pneumonia (respond to O2)
Chronic cyanosis: Tetralogy of Fallot (not respond to O2)
Signs of chronic cyanosis: finger clubbing, polycythemia (due to chronic hypoxia),
gingival hyperplasia
#Shortness of breath
Onset
Duration
Day/night
Feeding – activity – sleeping
Fever
Bluish discoloration
Aggravating and relieving factors
#Fever
High grade fever (in bacterial infection) or low grade fever (in viral infection)
At day time or night
Intermittent or continuous
Associated with sweating, chills, shivering, rigors
DDx: T.B, pneumonia, dehydration, SIADH, others (CNS infection and UTI)
#Noisy breathing
At which level?
Nose snoring "inspiratory", adenoid hypertrophy, common in pediatric
Epiglottis Grunting "expiratory", sign of respiratory distress
Grunting:
o Pulmonary:
Effusion, pneumothorax
Dramatic response to O2 for 10 minutes
o Extra-pulmonary:
Cardiac: e.g. acute heart failure
Metabolic acidosis: e.g. gastroenteritis, diarrhea, diabetic ketoacidosis,
salicylate
Severe blood loss: anemia
o Expiratory phase due to respiratory failure
5
Larynx Strider "inspiratory", e.g. croup
Trachea and major bronchus Crepitation (by stethoscope), Rattling (by ear)
"Inspiratory and expiratory" causes:
o Bronchiolitis: viral (RSV), less than 1 year, peak at 6 months
o Pneumonia: more than 1 year, inflammation of lower respiratory tract
Minor bronchioles wheezing "mainly expiratory", causes: bronchiolitis, asthma,
heart failure, pulmonary edema
#Relation of other systems to respiratory system:
GIT chest infection + frequent bowel motion = adenovirus
GUS chest infection + UTI = adenovirus
CNS chest infection + meningitis = adenovirus / Fit due to hypoxia (anxious or
lethargic)
Skin respiratory infection + rash = meals or as complication of poliovirus vaccine
#Past medical history:
The most important problem that affect the neonate and that 100% ends with
asthma is Broncho-pulmonary dysplasia
#Feeding:
Unfortified milk may lead to rickets – iron deficiency anemia // cow milk allergy
#Family history:
Usually 4 types of atopy
Allergic conjunctivitis
Allergic rhinitis (annual or seasonal)
Asthma
Allergic dermatitis (Eczema)
#Social history:
Type of heating trigger gas irritant for asthma patient
Animal contact irritant for child and asthma patient
Ventilation factory near house, fresh air from trees
Type of house cleaning
#Effects of feeding on respiratory problems:
1st common aspiration pneumonia
2nd common Tracheo-esophageal fistula
3rd common cow milk protein allergy (dyspnea, skin rashes, diarrhea,
microscopically bleeding or rectal bleeding)
6
Respiratory distress:
Mild: flaring of ala nasi and tachypnea
Moderate: use of accessory muscles
Severe: Grunting
More severe: all of above + cyanosis + conscious level (irritability)
Other signs:
o Cyanosed face
o Tachypnea (increased O2 wash alkalosis retention of CO2 acidosis)
o Asymmetrical movement of the chest
o Recession (suprasternal, supraclavicular, intercostal, subcostal)
o Harrison's sulcus permanent indentation of chest wall along the costal margins
where diaphragm inserts, due to chronic dyspnea in asthma, COPD, bronchiolitis
obliterans, heart diseases, also occur in rickets
o Tracheal Tag pulling of thyroid cartilage towards the sternal notch in inspiration
Associated symptoms:
o Nasal discharge (rhinorrhea)
o Sneezing
o Otalgia
o Ear discharge (otorrhea)
o Dysphagia
o Chest pain (if child can explain)
o Pulsus paradoxus fall in systolic BP > 15 mmHg during inspiration
Ask about: activity, sleeping pattern, feeding
General information:
o RDS is a condition that need admission postnatally and its effect is long-lived
o Surfactant formation starts at 28 weeks and complete at 37 weeks
o For maturity of lung of the baby dexamethasone is replaced by betamethasone
(one injection/ 24 hours before delivery)
o Causes of respiratory distress:
Reparatory: pneumonia, bronchiolitis, bronchitis, asthma, plural effusion,
pneumothorax relieved by O2
Cardiac not respond to O2
Metabolic: diabetic ketoacidosis, acute renal failure, dehydration
Neurological, drugs (opioids), severe anemia
Differential diagnosis of chronic cough + respiratory distress syndrome:
o Infections Pertussis (most common), TB
o Asthma, Bronchiectasis
o Sinusitis, Foreign body
o Bronchiolitis, obliteration
o Congenital anomaly

7
Part:2
Pediatric
General examination
General examination related to respiratory system
#General:
Introduce yourself
Name-age-sex-occupation of the patient
Alert or not (Old child oriented// young child alert)
Condition of patient: well, depressed, crying, comfortable, no abnormal posture,
Build obese (steroids), thin (TB, asthma, bronchiectasis, cystic fibrosis),
macrosomia (occur in baby for mother with gestational diabetes)
Environment (cannula, I.V fluid, catheter)
Congenital anomalies
Color of the child: Polycythemia, dusky color, jaundice, pale (physiological anemia,
breast milk not contain high amount of iron, premature baby)
Rapid assessment of dehydration (fontanels, eyes, skin turgor, drinking, urine output)
Rapid assessment of malnutrition (Subcutaneous fat of abdomen and thigh and
buttock, wrinkling, old face baby)
Respiratory problems (Dyspnea, Tachypnea, wheezing)
Anemia conjunctiva, mucus membrane, nail bed, palmer creases
Face: mangolian face, site of ear, eye distance
Mouth: cyanosis, dental carries, mouth breathing, gum hypertrophy (in CHD)
Nose: nasal discharge, nasal obstruction
Ear: otitis media
Neck: tonsils, thyroid, lymphadenopathy (generalized lymphadenopathy 3 groups
of lymph nodes involvement
Hand: drumstick clubbing, cyanosis, pallor, koilonychia, leukonychia
Leg: bilateral edema, cyanosis, sacral edema common in children
Peripheral cyanosis in neonate could be acrocyanosis, due to cold, should
disappear after warming up
Joneway lesions rheumatic fever "red macules in the palm"
#Finger clubbing:
Grading of clubbing:
I: obliteration of angle between nail and nail bed (fluctuation test: +Ve)
II: Parrot beak
III: Drum stick
8
IV: Hypertrophic osteroarthropathy
Causes:
o pulmonary: TB, Cystic fibrosis, bronchiectasis, lung abscess, bronchogenic
carcinoma
o Cardiac: congenital heart disease, infective endocarditis, Tetralogy of Fallot
(severe drum stick), fibrosing arteritis
o Idiopathic - Familial
#Cyanosis:
It is bluish discoloration of skin and mucus membrane due to increased
deoxygenated hemoglobin > 5 g/dl it is not hypoxia (associated with CO2)
Acro-cyanosis: peripheral (hands), normally occur in neonate, newborn, cold
Cardiac cyanosis: central (involves tongue), In central cyanosis there should be
peripheral cyanosis with it
5T cyanosis:
o TOF: tetralogy of Fallot
o TGA: transposition of great arteries D(dextro)type/ L(incompetent with life)type
o Total anomalies pulmonary venous return
o Tricuspid atresia
o Truncus arteriosus
Also: Ebstein's anomaly, pulmonary atresia or stenosis
Cyanosis: From birth it is mostly TGA
Cyanosis: 3-6 months later TOF
Cyanosis: Associated with H.F TGA
Cyanosis: Not associated with H.F TOF
#Vital signs:
1- Temperature:
Tympanic membrane (more common)
Oral
Axillary (+0.5)
Rectal (-0.5)
One degree increase lead to 10 beat increase in the heart rate

9
2- Pulse rate:
Rate
o Tachycardia: Fever, shock, drugs (salbutamol), sinus tachycardia, anemia,
thyrotoxicosis
o Bradycardia: sick sinus syndrome, athletes, cretinism, drugs (propanol), sleeping,
heart block, heart failure
Rhythm:
o Regular – regular
o Regular – irregular (ectopic)
o Completely irregular
o Radio-femoral delay: post ductal coarctation of aorta
o Radio-radial delay: pre ductal coarctation of aorta
o Brachio-femoral delay
Character:
o Jet of pulse: e.g. big and thrusting pulse
o Watson's water hammer pulse
o Gallop rhythm: can be assessed by palpation, we find S1, S2, S3, tachycardia
DDx: heart failure and valvular heart disease
Volume: small volume, normal volume, large volume
Pulsus paradoxus: decrease in systolic blood pressure >15 mmHg with inspiration,
occur in asthma and acute pericarditis
Non-cardiac causes of large volume pulse:
o Thyrotoxicosis
o Severe anemia
o Stress
Cardiac causes of small volume:
o Aortic stenosis
o Coarctation of aorta
o Pericardial effusion
o Cardiac tamponade
Causes of radial pulse absence:
o Arteriovenous fistula
o TAR: Thrombocytopenia-absent radius syndrome Thrombocytopenia, absence
of radial artery, congenital absence of radius bone
Tachycardia + small volume in shock or diarrhea
Water hummer (collapsing pulse) large volume, dorsum of hand
Differential cyanosis: cyanosis present in foot, but not hand coarctation of aorta
By ending of pulse examination: 80 bpm, regular, normal character, good volume, no
radio-femoral delay, normal peripheral pulsation
Post ductal coarctation:
Bluish discoloration of the lower
limbs but not the upper limbs and
head
11
3- Blood pressure:
5 methods:
o Auscultation: cuff = 2/3 of arm circumference
o Palpitory method: only systolic
o Flushing pale red
o Osmometry
o Doppler
There is special chart for blood pressure:
Example: 4 years child BP = 4+90/4+60 = 94/64 mmHg
4- Respiratory rate:
At least for 1 min (because of irregular respiration in childhood)
1-2 months 60/ min
2 months – 1 year 50/ min
> 3 years 20-30/ min
Periodic breathing: occurs when the breath pause for up to 10 seconds at time, there
may be several such pauses close together, followed by series of rapid shallow
breaths, then breathing returns to normal. This is common condition in premature
babies in first few weeks of life. Even healthy full term babies sometimes spells
periodic breathing, usually after sleeping deeply. Home care: supine position, avoid
soft pillows and smoking, never snake your baby to breath brain injury.
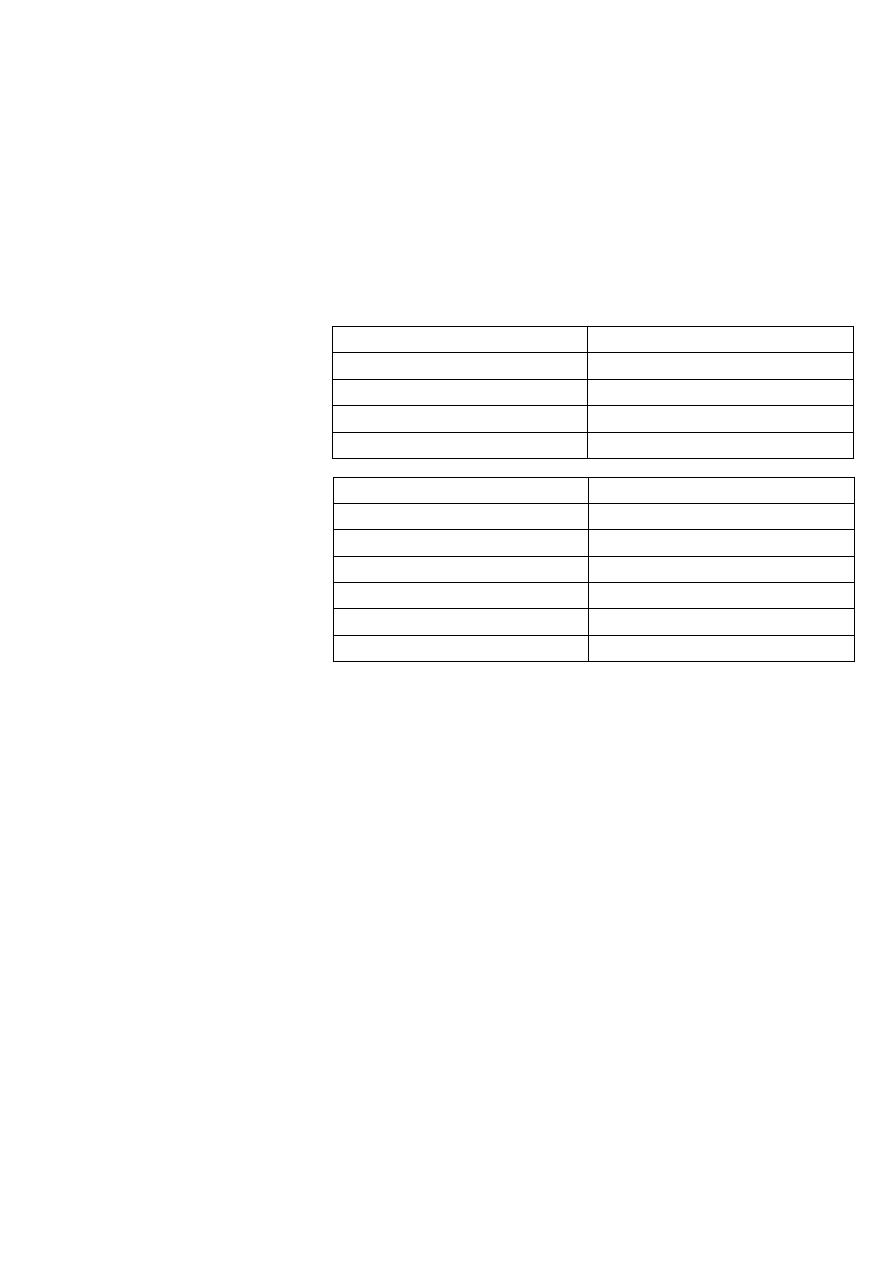
Periodic breathing
Apnea
Breathing stops up to 10 seconds
Stops more than 20 seconds
No
Infant may become limp
No cyanosis
Cyanosis
No change in heart rate
Decrease heart rate
5- Anthropometric measurements
OFC microcephaly, macrocephaly
Wight underweight, overweight
Height short stature, long stature
In acute illness weight is most affected anthropometric measure
In chronic illness length is most affected anthropometric measure
TB and bronchiectasis decrease weight
Asthma increase weight (due to steroids use) and cause short stature
Age in years + 90
Age in years + 60
11
Part:3
Pediatric
Respiratory examination
1- Setting:
Full exposure of the chest
Good light
Take permission
In children < 2 years old the examination includes inspection and auscultation only
2- Inspection:
Shape of the chest:
o Hyper-inflated chest: in bronchiolitis, asthma, emphysema
o Barrel chest: anterio-posterior diameter = transverse diameter normally in
young baby
o Pectus excavatum (Funnel chest)
o Pectus carinatum (Pigeon chest)
Symmetry of the chest
Movement with respiration, and respiratory rate
Type of respiration: abdominal, thoraco-abdominal, periodic respiration // abdominal
breathing is normal in small children
Space between 2 nipples
Scars:
o On left or right side of the chest Thoracotomy
o On sternum cardiac surgery
Abnormalities:
o Polymastia
o Absence of pectorals (Poland syndrome)
o Absence of sternum
o Absence of intercostal muscles (or wasted) starvation
o Hemangioma
o Rachitic rosary: in rickets patient, bead like knobs in the costochondral joint
o Visible pulsation
Hyperoxia test: (give 100% O2)
Used to differentiate between cardiac and respiratory causes of cyanosis
Response (absence of cyanosis after O2) pulmonary
No response (persistent of cyanosis after O2) cardiac (R to L shunt)

12
Posterior inspection for: kyphosis, scoliosis respiratory compression decreased
lung volume right sided heart failure // kyphoscoliosis in COPD and heart failure
3- Palpation:
Areas:
o Anteriorly clavicle (above) + 3 areas (ICS)
o Laterally 2 areas (in axillary region)
o Posteriorly supra-clavicular, inter-scapular, infra-scapular
Palpation for any mass or tenderness
Trachea:
o use one finger (unlike adult) Put index finger in the suprasternal notch
o normally centrally located and slightly deviated to the right
o If you suspect deviation of the trachea palpate the apex beat (could be
deviated)
o Fibrosis, consolidation, collapse pull
o Pneumothorax, hemothorax, plural effusion, emphysema push
o Only trachea deviated upper lobe lesion, neck mass (L.N, Tumor)
o Only heart deviated left ventricular hypertrophy, dextrocardia
Apex beat:
o Under 7 years: normally at 4th ICS at mid-clavicular line
o Above 7 years: normally at 5th ICS lateral to mid-clavicular line
o Shifting of apex beat (cardiac or respiratory cause) plural effusion, pneumonia,
pneumothorax, cardiomegaly (toward axilla)
Chest expansion: by tape measure below the nipple (use tape measure < 4 years //
use hands > 4 years) normally 1-3 cm bilateral
Vocal fremitus:
o Need cooperative child, you could know it from crying in young baby
o Decreased in: emphysema, plural effusion, pneumothorax, collapse
o Increased in: consolidation
o Done at 7 areas
Mitral area
Tricuspid area
Suprasternal area
Left upper and lower sternal border
Right upper and lower sternal border
4- Percussion:
Dull, Resonant, Hyper-resonant normally resonance
Site of percussion:
o Anterior wall one apical over clavicle, three anterior chest wall in ICS
o Lateral wall two at mid-axillary line

13
o Posterior wall one apical, one interscapular, one subscapular
Start from supraclavicular area and same regions of auscultation
Supra-clavicular (apex of lung) important most common site of T.B increase O2
Percuss direct on clavicles – 2
nd
space – anterior and posterior
Dull areas: cardiac (3,5,6 ICS) liver (7
th
ICS)
Resonance normal
Hyper-resonance pneumothorax, emphysema
Dull consolidation, fibrosis, tumor
Stony dull plural effusion
5- Auscultation:
Areas: Mammary region (supra-mammary, mammary, infra-mammary) Axillary
region (superior, inferior) and same sites of percussion
First check the nose patency
Air entry or not? Unilateral or bilateral? Type of respiration? Breathing sounds?
First: expose patient, warm stethoscope, ensure that nostrils are patent
Silent chest:
o No air entry all over the chest
o In status asthmaticus, in severe eczema (or emphysema), in pleural effusion
Bronchial breathing: found normally over trachea, over main bronchus, in neonate //
abnormally hear over lung in pneumonia
Added sounds: wheezes (rhonchi), crepitation (rales, crackles), plural rub
Plural Friction rub:
o Occur at the end of inspiratory phase when pleura become in contact with chest
wall
o Causes: pleurisy, pleural effusion
o friction rub with respiration pneumonia
Neonatal stridor:
o High pitched (harsh), inspiratory, biphasic (in foreign body), upper respiratory
problem (partial obstruction of large airways)
o Infectious strider: viral , bacterial (epiglottitis, croup)
o Non-infectious strider: hypocalcemia, edema, allergy to penicillin, foreign body
o In congenital laryngeomalacia, laryngeal foreign body, infection (like croup),
angioedema, hypocalcemia (stridor, convulsion, spasm)
o If cyanosis occur with stridor emergency
o Most common cause in pediatric is laryngeomalacia
Wheezing:
o Musical, medium pitched or low pitched - transmission of air through narrow
spaces (partially obstructed airway)
o In pediatric = small diameter bronchi mainly expiratory / severe diffuse
expiratory and inspiratory

14
o Differential diagnosis: heart failure (cardiac asthma), pneumonia, foreign body,
infection
o Localized rhonchi: foreign body
o Generalized rhonchi: asthma, bronchiolitis
o Most common cause of wheezing: bronchiolitis (<1 year), asthma (>4 year)
Crepitation:
o High pitched sound (inspiratory)
o Produced by mucus filled alveoli which fill during inspiration and collapse on
expiration
o Fine: inspiratory, occur in pulmonary edema (heart failure), pneumonia, foreign
body
o Course: inspiratory and expiatory, occur in fibrosis, asthma, bronchiolitis
Vocal resonance:
o Heard by stethoscope at same sites of percussion while the patient say 44
o Increase in: consolidation
o Decrease in: plural effusion, collapse
15
Part:4
Pediatric
Examination of CVS
#Cardiac examination
1- Settings:
Take permission
Hand washing
Good light support
Patient in sitting or semi-supine position
Exposure form the neck to the umbilicus
2- Inspection:
General look for:
o Signs of cyanosis or distress
o Continuous O2 administration
o Medication types
o How many pillows below the head of the patient
o Jaundice, hydration status
Any thoracic cage abnormality like Precordium bulging:
o Unilateral bulge: pneumothorax, plural effusion
o Bilateral bulge: massive collapse
Scars: indicates open heart surgery
o Axillary coarctation of aorta
o Femoral catheterization
o Scapular PDA
o Radial A-V shunt
o Middle sternotomy GABG, aortic valve replacement
o Infra-clavicular scar Pacemaker
o Sub-mammary mitral valvotomy
Visible pulsations: at apex, aortic, tricuspid, left side of sternum, epigastric , carotid
Bulged beat cardiomegaly
Apical pulse:
o Apex beat outermost, lowermost
o If you don’t find the pulsation look at the axilla (left side), if you still don’t find
the pulsation see the right side (dextrocardia)
o Causes of absent apex beat: obesity, thick chest wall, pericardial effusion, dextro
Other pulsations: hyperactive dancing pericardium in severe left to right shunt in
patient with VSD
16
Note: Telangiectasia: distributed blood vessels in face and thorax, disappear at
pressure, Ataxia telangiectasia syndrome // doesn't disappear on pressure spider
navi
3- Palpation:
Apex beat:
o Apex beat + character: example apex beat is palpable at 5th ICS mid-clavicular
line with normal character
o Under 7 years: normally at 4th ICS at mid-clavicular line
o Above 7 years: normally at 5th ICS lateral to mid-clavicular line
Thrill (by palmer surface of 4 fingers) suprasternal thrill coarctation of aorta
Heave parasternal or epigastric (right ventricular hypertrophy) apical (left
ventricular hypertrophy)
4- Percussion: only in plural effusion or pericardial tamponade
5- Auscultation:
4 regions in auscultation:
o Mitral (Apex) area 4
th
left ICS in mid-clavicular line or 5
th
ICS in older child
o Aortic area 2
nd
ICS right to the sternum
o Pulmonary area 2
nd
ICS left to the sternum
o Tricuspid area left sternal border in 4
th
ICS or 5
th
ICS in older child
Finding: S1, S2, Added sounds (S3, S4, ejection click), Murmur
1
st
heart sound (S1)
Mitral area (normal, soft, loud)
2
nd
heart sound (S2)
Pulmonary area (normal, splitting, loud, single)
Mitral (apex) area auscultation abnormalities:
o S1, S3, S4
o Mitral regurgitation
o Pan-systolic murmur (presented in first month of life) may be normal in infants
< 7 weeks but always pathological in infants > 7 weeks
o Mitral stenosis: most common cause of opening snap
Aortic area auscultation abnormalities:
o Aortic stenosis head at apex and all over chest and can radiate to neck
o Coarctation of aorta (also heard from the back)
o Innocent murmur
o Ejection systolic murmur (early aortic diastolic murmur) due to aortic
regurgitation and also radiated to pulmonary area
Pulmonary area auscultation abnormalities:
o Pulmonary stenosis
o Pulmonary innocent murmur
o Pulmonary hypertension
o Atrial septal defect (ASD)
17
o Ventricular septal defect (VSD)
o Ejection click systolic murmur in pulmonary area
Tricuspid area auscultation abnormalities:
o Tricuspid regurgitation radiate laterally to mitral area
o Pan-systolic murmur
o Tricuspid stenosis rare condition cause opening snap
5- Murmur:
Abnormal musical heart sound due to abnormal valve or abnormal (turbulent) blood
flow through normal valve
Rolle the patient left lateral bring the heart to the chest wall then sitting hear
back and ask the patient to take inspiration and expiration Murmurs related to
the back (PDA, Aortic regurgitation, coarctation of aorta)
Murmurs:
o Types (systolic-diastolic)
o Time (ejection systolic, pan systolic, early diastolic, late diastolic)
o Site, Intensity, Radiation, Grade, Character
o Relation to respiration: murmur of right side (higher during inspiration like aortic
stenosis) murmur of left side (higher during expiration like pulmonary stenosis)
o Propagation (radiation of pulse)
o Pitch of sound (harsh, soft, high)
o Change with position: mitral (left side), aortic (forward)
Murmur grades:
o G1: fairly heard
o G2: heard without difficulty
o G3: there is thrill
o G4: loud murmur
o G5: heard without stethoscope
Types of murmurs:
o Innocent murmur only systolic, murmur that change or disappear with position
change, change with inspiration and expiration, change in hype-dynamic
condition, diminished with liver decompression
o Ejection click in aortic stenosis
o Opening snap in mitral stenosis / in early diastolic phase with left ventricular
contraction and stenosed valve (soft sound)
Pan-systolic murmur:
o Ventricular septal defect radiate all over the precordium
o Mitral regurgitation (apex) radiate to the axilla
o Tricuspid regurgitation (left lower sternal border) no radiation
o Coarctation of aorta radiate to the back
18
#Diagnosis of VSD by examination
1- Inspection:
Hyperactive precordium (dancing precordium)
In large VSD > 5 mm there is Harrison sulcus, deviated apex beat, dancing, bulging
precordium
Shifting apex beat
2- Palpation:
Shifted apex beat
Epigastric thrill
Apical heave
3- Auscultation:
S1: normal
S2: not splitting, strong, fixed
Murmur: more harsh, less loud in large VSD // less harsh, more loud in small VSD
o Large VSD
> 5 mm
treated surgically, if there is heart failure we afraid of
complications like pulmonary hypertension and cardiac arrhythmias
o Small VSD
< 3 mm
close spontaneously 40% in the first year and 60% in the
followed 4 years
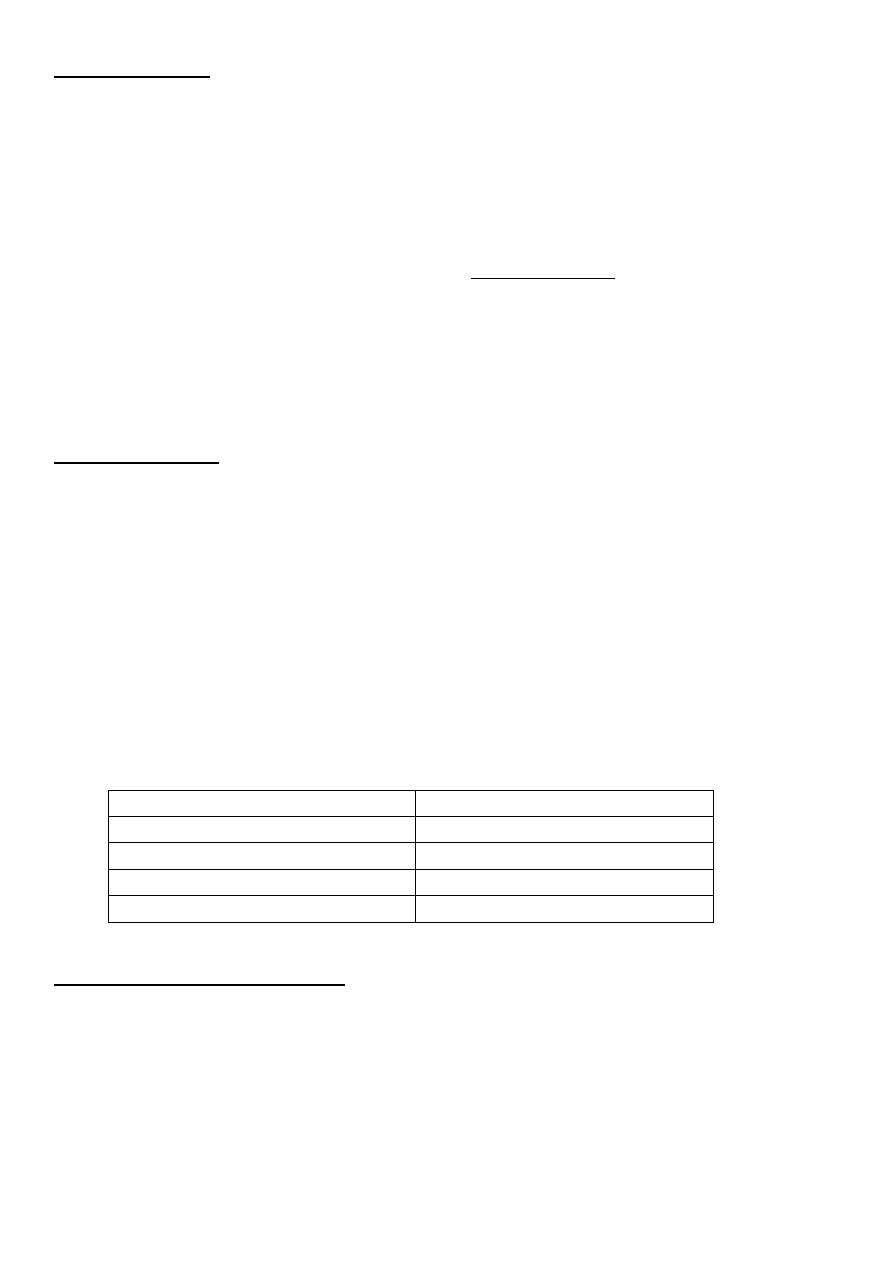
Murmur
Systolic
Ejection systolic murmur Pulmonary stenosis
Aortic stenosis
Atrial septal defect ASD
Pan- systolic murmur
Mitral regurgitation
Tricuspid regurgitation
Ventricular septal defect VSD
Systolic + diastolic Machinery murmur
Patent ductus arteriosus PDA
Diastolic
Early diastolic murmur
Pulmonary regurgitation
Aortic regurgitation
Mid-diastolic murmur
Mitral stenosis
Tricuspid stenosis

19
#Congenital heart disease (CHD)
1- History presentation of CHD:
Acute: cyanosis, dyspnea, cardiogenic shock
Chronic: chest pain, fatigability, sweating
2- Types:
Cyanotic (15%): 6T
o Tetralogy of Fallot (TOF) 65%
o Transposition of great vessels (arteries) TGA
o Total anomalous pulmonary venous return
o Truncus arteriosus
o Tricuspid atresia
o The pulmonary atresia or stenosis
Acyanotic (85%) 90% VSD
3- Patent ductus arteriosus (PDA)
Lead to Machinery murmur (systolic and diastolic)
Normally ductus arteriosus is opened in the 1
st
week and then closed
If not closed treated medically then surgically
Prostaglandins: the opening of PDA is maintained by it, thus given in TGA until
surgery performed, while indomethacin closes it thus given in PDA
4- Atrial septal defect (ASD)
Functioning foramen ovale is closed at 1 week to 1 month
If not closed lead to shunt with pulmonary stenosis usually
After 6 months present as ejection systolic murmur and accidentally discovered
ASD: usually asymptomatic with excellent prognosis
Clinical features of ASD: 1
st
and 2
nd
degree heart failure, arrhythmia, acyanotic
Osteum primum may present at 3 months
Secondum type of ASD can't be seen before 6 months, and my presented at 30
years as arrhythmia and heart failure, hypertension, tachycardia
5- Ventricular septal defect (VSD)
Presented at 1
st
month complex heart lesion + VSD
Presented up to 3 months pan-systolic murmur of VSD
Recurrent admission to hospital because of Congenital heart defect indicated large
VSD
6- Tetralogy of Fallot (TOF)
Presented up to 9 months during activity (as feeding)
21
Pink TOF when pulmonary cyanosis is not severe enough to cause bluish
discoloration, presented during 2-3 months due to feeding
May present at one year with right ventricular hypertrophy (boot shaped heart)
Surgical treatment is preferred but may treated medically
Decrease lung vascularity Tetralogy of Fallot TOF (Don't DROP the baby)
o Defect (VSD)
o Right ventricular hypertrophy
o Overriding aorta (aorta over interventricular septum)
o Pulmonary stenosis
Pulmonary stenosis determines the severity of Tetralogy of Fallot
Clinical features:
o Central cyanosis (1-2 months after birth) usually aggravated by sulking and crying
o Hyper-cyanotic spells: deep cyanosis aggravated by crying, infection, iron
deficiency anemia, followed by weakness, sleep, convulsion, unconscious
o Finger clubbing (before 1-2 years)
Signs:
o Left parasternal pulsation due to right ventricular hypertrophy
o Systolic thrill at 2nd left intercostal parasternal spaces
o Single S2 and loud at pulmonary area
o Ejection (mid systolic) murmur: usually heard over pulmonary area due to
pulmonary stenosis
o Heart failure is unusual
7- Left to right shunt clinical features:
Frequent chest infection
Cardiomegaly
Left axis dilation
Pericardial bulge
No cyanosis or clubbing
Easy fatigability and sweating
Chest lead on left ventricle
Plethoric lung in chest x-ray (increase lung vascularity)
occur in Patent ductus
arteriosus PDA, Transposition of the Great Arteries TGA
8- Right to left shunt clinical features:
Polycythemia
Cyanosis
Clubbing
With or without cardiomegaly
Oligemic lung

21
9- Congenital heart conditions without shunt:
Patent ductus arteriosus
Aortic stenosis and regurgitation
Pulmonary stenosis and regurgitation
10- How to differentiate between congenital/ aortic problem:
Time of appearance of clinical features
Failure to thrive (FTT)
Easy fatigability
Psychological problem
Notes:
Right ventricular hypertrophy (on palpation):
o Apex don’t shift
o Thrusting (diffuse pulsation)
o Heave
o May find murmur
Left ventricular hypertrophy (inside the chest):
o Apex has shifted to the axilla
Both right and left ventricular hypertrophy:
o Precordium bulging
o Diffuse pulsation
o Shifting apex beat
Ejection click + innocent murmur found in:
o Aortic stenosis
o Pulmonary stenosis
o Pulmonary hypertension
o Atrial septal defect
Ejection click is not found in:
o Coarctation of aorta
o Aortic regurgitation
Cyanosis stat from the beginning in:
o Mitral condition
o Tricuspid condition
o Transposition of great vessels
Sever pulmonary atresia and TGA without VSD 1
st
day, 1
st
hour, severe cyanosis
2-3 months nearly most cyanotic heart diseases

22
> 3 months supra-ventricular tachycardia, Intra-uterine event that mimic
condition of CHD and causes heart failure (give intrauterine adenosine during
pregnancy)
> 2-3 years Rheumatic fever (rheumatic carditis), aortic stenosis and mitral
regurgitation
Infective endocarditis rare in children because of insidious progression (diagnosed
by culture only)
Patient with myocarditis have enlarged heart, muffled S1 and S2, low voltage
Any lesion in the right side of the heart increase with inspiration and in the left side
of the heart increase with expiration
If baby diagnosed as one of these anomalies or other, mention that at the beginning
of history with time.
Infective endocarditis risk for lifelong 2%
all chronic heart diseases do not interfere with patient activity except aortic stenosis
in which patient is exhausted with any activity
In osteom secundum ASD and PDA of 6 mm close after 2 weeks if not, it need
surgical correction
squint
CVA
bad hygiene of mouth
endocarditis
Congenital heart defect ((1- CVA < 4 years // 2- Abscess > 4 years)) associated with
CNS history
History of heart failure in 2 months old baby is: feeding difficulty + sweating
Investigations in CVS: CXR, Echo, ECG, Catheterization
ASD there is fixed splitting S2 and functional pulmonary stenosis with it.
Murmur in aorta:
o Aortic stenosis: hear everywhere in the chest, occur suddenly
o Coarctation of the aorta: hear better in the back, not suddenly, there is difference
in the upper and lower limb
Non-pathological murmur:
o Functional murmur in fever, thyrotoxicosis, anemia, increased metabolic rate
o Innocent murmur characteristics (10S)
S1 = systolic
S2 = small area
S3 = short duration
S4 = Symptoms free
S5 = signs free
S6 = severity G1 or G2
S7 = study (investigations) like ECG, Echo, CXR => are normal
S8 = sternal depression
S9 = sitting standing variation
S10 = smooth
23
Part:5
Pediatric
Important Topics
#Presentation of respiratory system
Super-acute:
o Short attack within minutes
o May be due to: aspiration, poisoning with CO or Kerosin, Foreign body inhalation
Acute:
o Within hours
o May be due to acute respiratory infection (upper or lower as in strider, croup,
bronchial asthma)
Sub-acute:
o Within several weeks
o May be due to pertussis, TB
Chronic:
o May be due to T.B, COPD, Bronchiectasis, Asthma
#Asthma
#General information
Asthma is disease of small and large airways, but mostly of small airways
Definition: it is recurrent episodes of dyspnea respond to bronchodilators and there
is family history
Chronic inflammatory airway disorder, characterized by:
o Airway obstruction: that is reversible either spontaneously or by medications
o Airway hypersensitivity to variety of stimuli (most commonly in children are viral
infections)
Recurrent disorder, characterized by:
o Chest tightness
o Wheezing
o Breathlessness
o Cough
Deferential diagnosis:
o 1st attack pneumonia, heart failure, bronchiolitis
o 2nd attack allergic bronchitis
o 3rd attack asthma
Epidemiology :
o Most common health problem in children
24
o 80% of them have symptoms < 5 years
o High in African American than white
Asthma needs acute (rescue) treatment and chronic management (if asthma not
treated sufficiently complicated as fibrosing alveolitis)
#Etiology
Not well understood
Family history: Genetic factor (chromosome 15)
Environmental factors (viral infection)
Atopy (atopic dermatitis) or type I hypersensitivity reaction (Exposure to allergens or
chemicals)
Increase risk in (Low Body Weigh < 2.5 Kg) and (Meconium aspiration)
Diet: protective Chinese food // aggravative egg- banana – fish – Cow's milk
#Environmental risk factors
Perinatal asthma: male, maternal smoking, passive neonatal illness, Low body weight,
meconium aspiration
Early childhood: Lower respiratory tract infection (adenovirus, pneumonia,
bronchiolitis), Food allergy, Low socio-economic status, Exposure to household mites
Later childhood: diet, air pollution, mites and pets
#Why common at night?
Anatomically: diameter of bronchioles at night less
than at day
Exposure to antigens at bed and pillows
Decrease secretion of cortisol
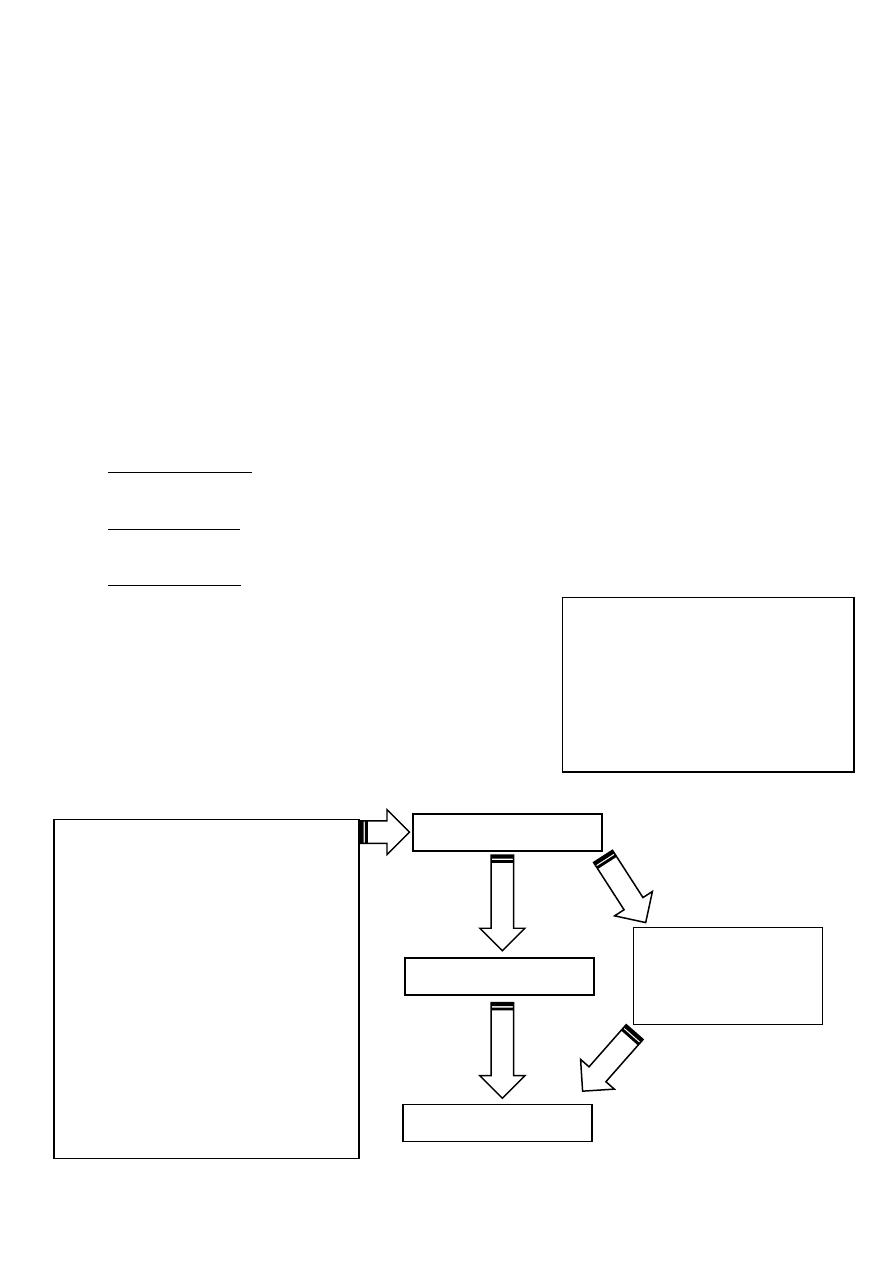
#Pathophysiology
Triggers of asthma
Viral and bacterial infections
Chemical; irritants (industrial,
household)
Air pollutants (CO, O3)
Tobacco smoking
Dust mites / cockroaches
allergens
Animal dander, urine
Exercise, cold weather,
emotion, stress
Inflammation
Acute
hypersensitivity
reaction
Asthma symptoms
Obstruction
Q: Why immunosuppressive
agents not very effective in
treatment of asthma in
pediatric age? Because most
common triggers in children is
viral infection
25
#Models of inflammatory response leading to asthma
Phase I
Sensitization of immune system
Repeated exposure to allergen
Production of IgE by immune system bronchospasm
Treatment: bronchodilators
Lasts 6 hours
Phase II
immediate hypersensitivity to subsequent exposure
IgE recognize and binds to allergen inflammatory mediators released by immune
cells (eg: histamine)
Histamine: smooth muscles contraction, increase secretion of mucus from airway
tract glands, fluid leakage (edema) in airway wall
Treatment: corticosteroids
Lasts 24 hours
#Types
Intermittent:
o More than 2 attacks (at day)/ month and 1 or more attacks (at night)/ month
o Treatment: No daily treatment (only on demand inhaler or nebulizer)
Mild persistent:
o More than 2 attacks (at day)/ month and more than 2 attacks (at night)/ month
o Treatment: low dose of steroid inhaler
Moderate persistent:
o Daily attack mostly / month and more than 4 attacks (at night)/ month
o Treatment: low or moderate dose corticosteroids + aminophylline or
bronchodilator
Severe persistent:
o More daily attacks and frequent attacks at night
o Treatment: low dose of oral corticosteroids or long acting beta agonist (LABA)
Note Mild: low dose inhaler, Moderate: systemic steroids, Severe: high dose
corticosteroids
Note With frequent monitoring and ask about school performance
#Clinical manifestations
History:
Airway limitation in asthma:
1- Mucus plug
2- Airway edema
3- Bronchospasm
4- Airway remodeling
Bronchiolitis has same
pathophysiology except:
airway remodeling
26
o Wheezing, cough, chest tightness, breathlessness
o Worsening at night
o Provoking factors, relieving factors
o Risk factors: allergic rhinitis, atopy, family history
Documented airway obstruction: PEF (peak expiratory flow) or spirometry (FEV,VC)
{>5years}
Demonstration of reversibility of obstruction and symptoms: by giving
bronchodilators
improved?
asthma
Exercise test
#Differential diagnosis
Bronchiolitis
Bronchitis
Pneumonia
Cystic fibrosis
Tracheal stenosis
Laryngeal stenosis
Laryngeal webs
Uvula disease
Lymphadenopathy
Foreign body
Pulmonary embolism
Viral infection
GERD
Congestive heart failure
Pulmonary eosinophilia
#Lung Function Test
1- Spirometry:
Air flow limitation: low FEV1 FEV1/FVC < 0.8
Response to bronchodilators: B2 agonist > 12% of FEV1
Exercise challenge : worsening in FEV1 > 15%
2- Peak expiratory flow meter: the difference between morning and night is > 20%
3- Exercise test:
Stop treatment for 24-72 hours
At early morning and dry weather
Exercise for 15 minutes
First 6 hours accompanied by bronchodilators due to cholinergic stimulation
Before-After exercise worsening: FEV1 > 15% diagnostic
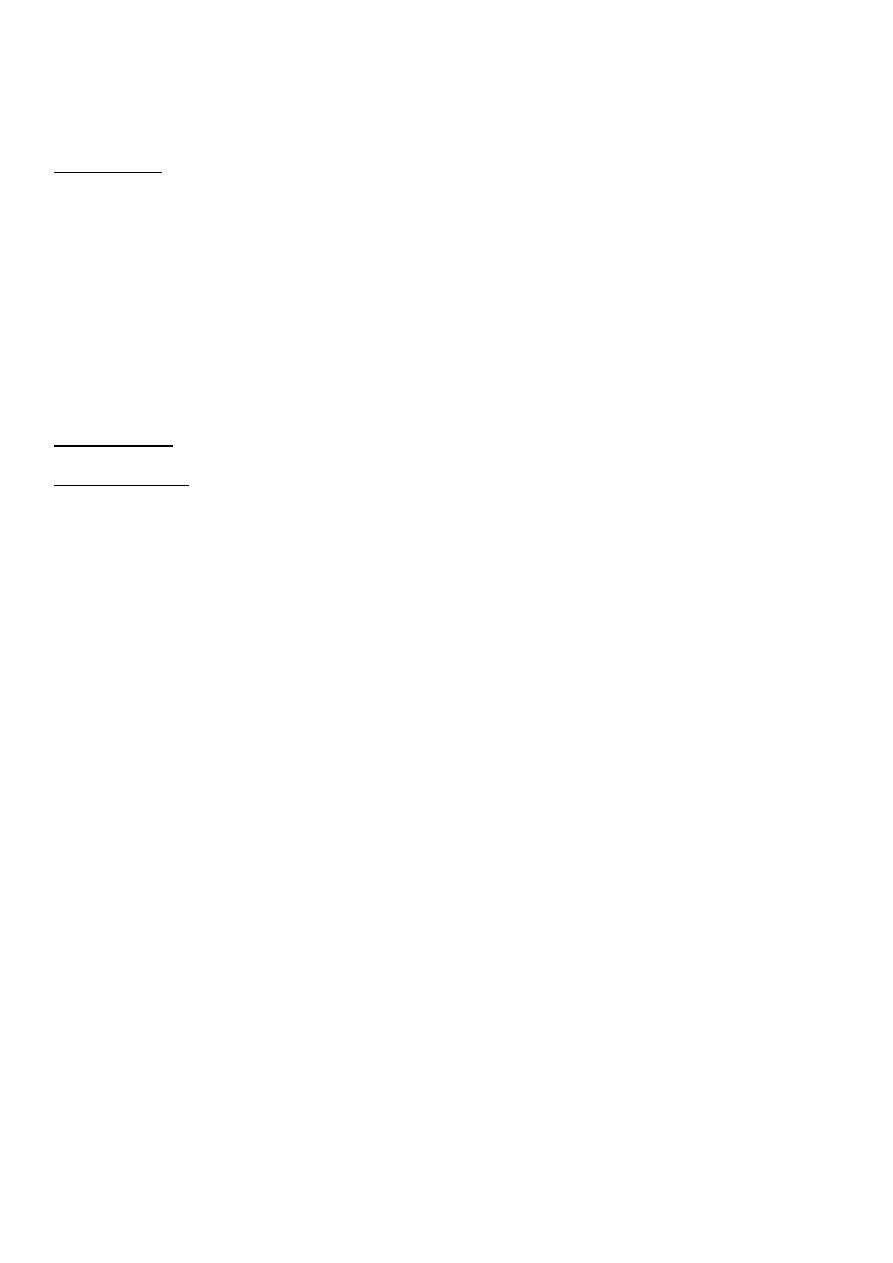
Asthma
Allergy
Recurrence
May but less
Response to bronchodilator
No
Eosinophilia
No
+ve family history
No
Asthma
Bronchiolitis
Recurrent attacks
1
st
attack
Positive family history
Negative family history
Respond to bronchodilators
Not respond
Older children
Small children
Over all year
Winter and early spring
Eosinophilia
No

27
Give bronchodilators: if there's improvement > 15% diagnostic
Needs cooperative child (5 years old or more)
4- Other tests:
Eosinophils
Allergic test 'Chest x-ray
Diffusing capacity
Broncho provocation (give patient histamine bronchospasm risk of status
asthmaticus)
Blood gases:
o Hypoxia + hypocapnia
o Hypoxia + normal capnia
o Hypoxia + hypercapnia
#Reliving factors of asthma
Reduce activity
Give bronchodilators
Give Antibiotics
Avoid allergens
#Notes:
Criteria of asthma dry cough (respond to bronchodilators), positive family history, no
strider, presence of wheezing or rhonchi
FVC normal in asthma so FEV1/FVC decreases
In fibrosis FVC decreased, FEV1 decreased, normal FEV1/FVC
PEFM (peak expiratory flow meter):
o Green Asthma in good control
o Yellow Liable to develop asthma
o Red patient has asthma
Rhonchi:
o Mild asthma expiratory rhonchi
o Moderate asthma expiratory and inspiratory rhonchi
o Severe asthma silent chest
#Acute respiratory infection
Patient come with cough or dyspnea
Acute < 30 days (4 weeks)
Age < 5 years
Assessment:
o Ask fever, feeding, fit, sleeping disturbance
28
o Look respiratory rate, chest indrawing, malnutrition
o Listen strider, wheezing
Respiratory rate:
o < 2 moths (60/min), 2 moths – 1 year (50/min), 1 year – 5 year (40/min)
o Periodic respiration because of immature brain center
Chest indrawing:
o Intermittent lower chest movement due to acute dyspnea
o Movement of chest inward during fetus breathing in (inspiration)
o Occur in acute illness
Sulci permanent indrawing of lower chest (most lower ribs) due to chronic dyspnea
occur in rickets, COPD
Sub-costal recess one line of indrawing of muscles below the ribs immediately
Malnutrition:
o Wasting loss of muscle bilk (thigh and buttocks)
o Thinning loss of subcutaneous fat (skin of thigh)
Strider: harsh noise due to upper respiratory tract obstruction, either inspiratory or
biphasic (in severe obstruction) never be expiratory alone
Wheeze: musical sound due to lower respiratory tract obstruction, either expiratory
or biphasic and never be inspiratory alone
Categories from 2 months – 5 years
Category 1:
o When patient come with cough or dyspnea with any of dangerous sign of the
following:
Fit
Sleeping disturbance
Feeding disturbance
Strider in calm child (and wheezing)
Malnutrition
o Diagnosis: very severe illness
o Treatment: 1st dose antibiotic refer urgently to hospital
Category 2:
o Patient come with cough or dyspnea with no dangerous sign but tachypnea or
chest indrawing
o Diagnosis: sever pneumonia
o Treatment: 1st dose antibiotic refer urgently to hospital
Category 3:
o Patient come with cough or dyspnea with tachypnea only
o Diagnosis: pneumonia
o Treatment: oral antibiotic (5days) then reassess after that then return within 2 days
if no response
Category 4:
29
o Patient come with cough or dyspnea with nothing
o Diagnosis: coryza (cold + cough)
o Treatment: at home clear nose + keep child warm + enhance breast feeding +
give soft home remedies
Categories from 0 – 2 months
Category 1 and category 2 like above
Category 2:
o Patient come with cough or dyspnea with nothing
o Diagnosis: coryza
o Treatment: at home clear nose + keep child warm + enhance breast feeding
Types of drugs used:
o Oral antibiotics: Trimethoprim – sulfamethoxazole
o Injection antibiotics: Penicillin – Benzathine – Ampicillin + Amoxicillin
o For wheezing we use oral salbutamol
o For fever we use paracetamol (oral)
#Pneumonia
It is disease of parenchyma (once parenchyma affected sleeping feeding activity not
well)
Pneumonia inflammation with consolidation // pneumonitis inflammation without
consolidation
Causes:
o Newborn (0-30 days): Streptococcus pneumonia, Listeria monocytogens, E.coli,
Klebsiella pneumonia
o Infants and toddlers: mostly viral RSV, para-influenza virus
o Pre-school (5 years): Mycoplasma pneumonia
o Other causes: osteomyelitis (hematological spread), foreign body, aspiration, viral,
hematological spread (leukemia)
Organisms:
o Pneumococcus pneumonia most common
o Staphylococcus pneumonia most serious, lead to lung abscess and sepsis
o Streptococcus pneumonia
o Para-influenza virus
o Mycoplasma pneumonia atypical pneumonia, peri-school age, afebrile
paroxysmal, spasmodic, not toxic, Investigations (CXR lobar pneumonia / Serology
+ve agglutination test), treated by erythromycin
o Viral low grade fever/ mild toxicity/ CBP lymphocytosis/
o Bacterial high grade fever/ high toxicity/ CBP neutrophilia, increased ESR & CRP
Types of pneumonia:
o Lobar pneumonia bacterial, one lobe, unilateral in chest x-ray, bronchial
breathing, increased vocal resonance

31
o Interstitial pneumonia (acute bronchiolitis) viral, granular, pattern
o Broncho-pneumonia small foci of consolidation along distribution of bronchioles,
bilateral, fine crepitation, expiratory wheezing, multiple small patches on chest x-
ray, Causes:
Viral mild fever, high paroxysmal cough, involve the bronchi (granular
interstitial small foci), lymphocytosis, negative culture of blood
Bacterial toxic, less episodes of mild cough, lobar CXR, leukocytosis, increased
ESR, increased protein, positive culture of blood
Indications of hospitalized patient in pneumonia:
o Age: < 6 months
o Immune compromised
o Vomiting and dehydration
o Patient with chronic disease
o Congenital heart diseases CHD
o Non-competent / not educated parents
Recurrent pneumonia:
o 2 attacks of pneumonia/6 months or 3/1 year, with complete resolution between
attacks
o Causes:
Cardiovascular CHD
pulmonary kartagener syndrome (dextrocardia and immotile cilia), Tracheo-
esophageal fistula, GERD, hernealocele, cystic fibrosis, bronchiectasis
Immunodeficiency
Others: croup, asthma
o Recurrent lobar pneumonia at same site DDx: foreign body
Stages of pneumonia:
o Congestion
o Red hepatization
o Gray hepatization
o Resolution (crepitation)
Signs and symptoms of consolidated lung (like in lobar pneumonia)
o Decease air entry and bronchial breath
o Dull percussion
o Decrease chest expansion
o Increase vocal fremitus
o Increase vocal resonance (while decease vocal fremitus and resonance in plural
effusion e.g. atelectasis)
Neonatal pneumonia usually bacterial
mostly staphylococcus
Aspiration pneumonia bad feeding practice (especially in neonate), at right apical
area

31
Pneumonia always with fever except in: immunocompromised patient or atypical
pneumonia caused by mycoplasma
Mycoplasma pneumonia:
o School aged children
o Causes lobar pneumonia
o Diagnosis: cold agglutinin
o Complications of M.Pneumonia:
Erythema multiforme
Steven-Jensen syndrome (sloughing of skin)
Hemolytic anemia (may produce jaundice)
Management of pneumonia:
o IV fluid if there is vomiting because it causes dehydration
o Oxygen due to hypoxia
o Antibiotics mostly macrolides or antiviral or anti-TB
o Chest drainage if there is para-pneumonic effusion
o Steroids
Indication for hospital admission in pneumonia:
o Signs of respiratory distress
o Less than 6 months
o Fever, vomiting, chronic disease
o Poor response to oral treatment
o Poor family situation
Complications of pneumonia:
o Para-pneumonic effusion
o Respiratory failure
o Myocarditis
o Paralytic ileus
o Meningisum (neck rigidity without other features of meningitis)
#Common clod (Nasophyrangitis)
Rhinorrhea (watery discharge from nose) if greenish give antibiotics
Low grade fever (High fever suggests complications such as: sinusitis, otitis media)
Simple infrequent cough
No disturbance of sleeping
Post nasal drip cough
Not need hospital admission
Doing well (activity + feeding + sleeping)
#Pharyngitis (Oropharyngitis)
Include Tonsillitis
32
Most common microorganism Group A beta-hemolytic streptococci
Dysphagia but no dyspnea
Fever, sore throat, vomiting, abdominal pain, mouth breather, adenoid, malaise
Not well
Why abdominal may develop in tonsillitis? due to involvement of mesenteric lymph
nodes
Tonsillectomy not resolve (Rheumatic fever) problem due to involvement of pharynx, so
prophylaxis of rheumatic fever is antibiotics not tonsillectomy
#Laryngitis
Mostly viral, mild in bacterial
High pitched sound (teacher, singer) dysphonia, aphonia (management rest)
Cough: stellate cough
Irritating
Cold exposure
Low grade fever
No malaise
Affect old age
#Laryngeo-Tracheo-Bronchitis
Viral benign // bacterial serious and emergency
Viral:
o Mostly para-influenza, 1-3 years of age, low grade fever, no dyspnea, moderate
activity
o Barking cough (caw sound) due to dryness of the area (no moister due to: croup,
foreign body) at late night increase dryness so increase severity
o Dramatic response to hot path vaporation and hot soup
o Note: strider sound with inspiration sign of upper respiratory tract problem
Bacterial :
o Haemophilus influenza most common cause
o Specific dangerous site epiglottis suffocation
o Barking cough, stride, fever, dyspnea, cyanosis, open mouth, extended neck,
dysphonia, even aphonia, drooling of saliva
o You shouldn't exam mouth especially tongue depressor
o At causality unit: cannula, I.V fluid, antibiotics, tracheostomy
#Croup
Affect infants, in winter,
Barking cough + well activity + stridor at night + low grade fever
Para-influenza virus, Respiratory syncytial virus
33
Haemophilus influenza, Diphtheria, Staph.aureus, Strept.pneumoniae
Complications of RSV: acute respiratory distress syndrome, bronchiolitis obliterans,
congestive heart failure, myocarditis, chronic lung disease
Management of croup: epinephrine, mist therapy, steroids (dexamethasone 0.4
mg/kg/day to decrease edema)
#Epiglottitis
Toxic and dangerous and patient not well
Nasal discharge (within 6 hours)
Fever, extended neck, drooling saliva, air hunger, barking cough, suffocation, dyspnea
Under general anesthesia in surgical room for investigation
In chest x-ray thumb printing
Acute epiglottitis may be caused by H.influenza
Epiglottitis and foreign body (cause sudden strider) are emergency conditions
Need hospital admission oxygen + IV line (fluid and antibiotics) + assessment of
circulation, monitor of urine output + not use tongue depressor + ay need tracheostomy
#Otitis media
High grade fever
Unexplained crying
Rubbing ear
#Sinusitis
High grade fever
Nasal discharge is purulent > 10 days
#Pertussis
It is infection of the respiratory system caused by bordetella pertussis
Signs and symptoms:
o Common cold: running nose, sneezing, mild cough, low grade fever
o After 1-2 weeks: the dry irritating cough evolves into coughing spells (the child may
return red or purple) then the child make a characteristic whooping sound when
breathing in or may vomit (post-tussive) // cyanosis // reddish discoloration
o Between spells the child usually feels well
At first patient come with burst gum cough then continuous cough then cyanosis then
whooping cough
Paroxysmal cough > 5-6 times accompanied by post-tussive emesis, repeated episodes,
if more than 8 times DDx: pertussis
34
Not all patients come with whooping cough especially young babies, because it requires
strong contraction
Baby come with immature respiration so can't produce enough force to produce
whooping
Pertussis at any age from birth or at 2 months or 4 months age due to its relation
with cellular immunity
Definitive diagnosis: culture, atypical lymphocytosis
Treatment: antibiotics for 2 weeks, mist therapy, rest
#Bronchitis
Acute bronchitis usually viral in origin // bacterial occur in infants & malnourished
Not common in pediatrics, but small trees (bronchiolitis) is common {in adult بالعكس}
because length of tree shorter in pediatrics
Common especially < 2 years – winter – viral
All lower respiratory infection dyspnea
Mostly it is precede by nasopharyngitis
Cough: firstly dry then productive
Fever, spasm, looks like asthmatic patient, recurrent episodes
Signs: rhonchi and moist crepitation
It is not associated with respiratory distress
#Bronchiolitis
0 month – 2 years (usually 2-6 months)
Viral causes RSV, adenovirus, para-influenza virus
During winter and early spring
Diagnosis: wheezy cough, acute respiratory distress in infant around 6 months old
Clinical features: begins with high grade fever and nasal discharge and then with cough
and severe dyspnea, patient not well, no barking cough, no strider
Auscultation: Fine crepitation, expiratory wheezing, decreased air entry
Bronchiolitis may lead to decease urine output due to dehydration with yellow color
(Tachypnea, poor feeding, fever, SIADH)
In bronchiolitis: after first diagnostic CXR for evaluation of the child we use oximetry and
respiratory rate instead of CXR
Q: how to differentiate between bacterial Broncho-pneumonia and bronchiolitis? by
leukocytosis and C-reactive protein in pneumonia
To differentiate between bronchiolitis and heart failure:
o Murmur
o Enlarged left or right ventricle (apex beat)
o On abdominal examination if palpable liver: do liver span because bronchiolitis
may push liver downward or hepatomegaly due to heart failure
35
Management: steroids (no benefit), beta-agonist (no benefit), albuterol, only O2 therapy
improves the condition
Serious condition called bronchiolitis obliterans
Viral cause low grade fever – less toxic – ESR & CRP normal – normal X-ray – Elevated
lymphocytes
Bacterial cause High grade fever – more toxic – ESR & CRP elevated – patchy
consolidation in X-ray - elevated neutrophils and leukocytosis
Important conditions to know:
Laryngeomalacia short neck, the patient come with stridor due to congenital atrophy
of the larynx
Tracheo-esophageal fistula the patient come with history of respiratory tract
infection
Cystic fibrosis the patient come with repeated chest infection and diarrhea
because patient can't spit up sputum and cause chest infection
Meconium ileus abdominal distention due to cystic fibrosis
#Diagnosis of:
Left side heart failure:
o Percussion: normal
o Vocal fremitus: Normal (resonant)
o Breath sound: normal
o Added sounds: crepitation, wheeze
Plural effusion:
o Percussion: stony dull
o Vocal fremitus: decreased (diminished)
o Breath sound: decrease in site of effusion
o Added sounds: no
Pneumonia (consolidation):
o Percussion: dull
o Vocal fremitus: increased
o Breath sound: bronchial
o Added sounds: rales
Emphysema (COPD in late stage):
o Percussion: hyper-resonant
o Vocal fremitus: decreased
o Breath sound: decrease vesicular breathing
o Added sounds: no
Pneumothorax:
o Percussion: hyper-resonant
36
o Vocal fremitus: absent
o Breath sound: absent
o Added sounds: no
Atelectasis (obstruction):
o Percussion: dull
o Vocal fremitus: decreased or absent
o Breath sound: decreased or absent
o Added sounds: no
#Drugs:
Vancomycin most frequent antibiotics used to treat patient with chest infection
given as slow drip (over 1 hour) because it may cause cardiogenic shock
Nebulizer:
o Nebulizer administration after 2 months (not before 2 months) because smooth
muscles of bronchioles are not well developed and also the receptors of
bronchodilator is not mature
o Nebulizer distilled water is replaced by normal saline because the tonicity of the
later is similar to that of the blood
o Ventolin (Salbutamol) 1 ml contains 5 mg we give 0.15 mg/kg If 10 kg baby
we give 10 x 0.15 = 1/5 mg/kg thus give about 1/2 cc for 10 kg
Steroid harmful in adenovirus oblitrance bronchiolitis
Notes:
Upper respiratory tract (nasal cavity, pharynx, larynx) Lower respiratory tract (Trachea,
bronchi, Lungs)
Clinical features of: Upper respiratory tract (Rhinorrhea, Barking cough, Normal feeding,
Normal activity) Lower respiratory tract (Irritable, significant dyspnea, significant cough,
poor feeding)
Nasopharynx (nasopharyngitis, tonsillitis, pharyngitis)(no dyspnea, no cyanosis)
Lymphoma (common malignancy in children) clinically: abdominal mass, dyspnea,
wheezing (compression), CXR (mediastinal widening)
NTD: affects lower limbs and bladder sphincter at lower level and affect phrenic nerve
(c3,4,5) at upper level
Cystic fibrosis: lethal inherited (autosomal recessive) disease, affect exocrine glands,
90% respiratory tract, also affect the pancreas and multiple organs.
Vesicular breathing is bronchial, but due to septae it will change, thus in consolidation
and congestion bronchial not heard
Tachypnea part of dyspnea, but dyspnea not synonymous with tachypnea
Neonatal sepsis Group b beta-hemolytic streptococci, listeria, E.coli

37
Group A beta-hemolytic streptococci lead to scarlet fever (red skin rah – sore throat-
fever) , tonsillitis, rheumatic fever
alpha-hemolytic streptococci in oral cavity lead to infective endocarditis
Examine membrane cover the tonsils or pharynx:
o Diphtheria gray - toxic – fever – membrane cover the whole nasopharynx
tonsils even may include soft and hard palates, difficult to be removed – when
remove cause blood oozing, diphtheria could lead to myocarditis
o Beta-hemolytic streptococci covers pillers and tonsils, gray to red, easily
removed, doesn't reach the hard palate
o Infectious mononucleosis
Staphylococcus (fist 2 months) / Mycoplasma pneumonia (in school age)
Fever: viral (sudden, less severe) bacterial (gradual, more severe)
Chronic cough > 1 months trachitis
Toxic infant + drooling saliva epiglottis
Pneumonia + severe cough with sudden deterioration may indicate pneumothorax
How can we know the patient's condition is stable? assessment of vital signs (especially
respiratory rate), skin color, feeding, urine output // if not stable and become worse
suggest abscess development (developing of sepsis) indicators of infection (patient in
shock, with high fever, tachypnea, increase O2 demand, poor oxygenation, decreased
mentality and stability) do investigations (see cytokines, leukocytopenia suggest
overwhelming infection)
While measles for example After 6 months due to its relation with humoral immunity
from mother
Congenital rubella microcephaly + cardiac disease
Viral infection (with adenovirus) sticky eyes, conjunctivitis, dry cough, febrile,
frequent bowel motion, chest infection / treatment by cold exposure to relieve spasm
and inflammation
The only virus that cause fever after dyspnea adenovirus
Nasal discharge without cough, without fever common cold
Watery nasal discharge green thick (nasopharyngitis)
Fever + nasal discharge + pain pharyngitis
Fever + dysphonia laryngitis
Chest x-ray vertebrae adjacent to costocondrial junction are the only visible, when all
vertebral column is shown bad exposure
Over inflated chest: flat diaphragm or more than 8 ribs on CXR
Congenital diaphragmatic hernia on left side more common due to site of liver
Diaphragmatic hernia: cyanosis, dyspnea, scaphoid abdomen
Cow milk may cause: diarrhea, allergy (wheezing, rhonchi)
Acute tracheitis caused by S.aureus
Children < 1 month may have hypothermia

38
Edema may occur because RSV may cause inappropriate secretion of ADH
How would you know that the infant have sputum with cough? usually if there is
sputum, you can see that with vomiting
Causes of irritability associated with breathlessness? dehydration, hypoxia
Infectious mononucleosis: it is viral infection caused by EBV and causes suppurative
pharyngitis (rare below 2 years) called glandular fever, may involve trochlear lymph
nodes.
Ampicillin and amoxicillin may cause skin rashes
Q: when the child swallow organic particle or inorganic one, which of them is more
dangerous? organic substance is more dangerous because the body immune response
rapidly develop (more rapid than inorganic particle)
DDx of cough + fit febrile convulsion, hypoxia, severe dyspnea caused by rotavirus
CVS relation with environmental cold peripheral cyanosis (acrocyanosis)
Respiratory problem + deceased urine output: SIADH, asthma, cystic fibrosis, dilution
hyponatremia
Neonate with heart failure have neither ankle edema nor raised JVP because of small
neck
Rule of 60 in neonate: 60 breath/min, 160 mmHg, cardiothoracic ratio is 60%, PCV = 60%
White sputum seen in: viral infection, asthma, other types of allergy
Infantile colicky occurs in first 3 months because of overfeeding
Poor ventilation and crowding TB and other communicable diseases
The optimal interval between feedings is about 2-3 hours, because gastric emptying in
pediatrics lasts about 2-3 hours
Normal oxygen saturation is from 94 to 100 % ((SpO2))
Signs of poor circulation increase heart rate, cyanosis, pale face, cold skin, decrease
in the BP and temperature and urine output and capillary refill and O2 saturation
In pediatrics there is no tracheitis alone, in adult yes
Dyspnea occur in asthma, pneumonia, bronchiolitis
High grade fever with shivering pus anywhere / UTI
Low grade fever with sweating and rigor rickettsia / TB
Traveler fever flu like illness
Persistent fever chronic infection
BCG look for scar
Breath holding attack benign condition, psychological cause, baby not cry, become
cyanosed, disappear after the age of 5 years
Down's syndrome congenital heart disease and recurrent pneumonia
Hypocalcaemia strider, convulsions, carpopedial spasm
Wheezing chest + GIT problems:
o Seen in parenteral infection (rotavirus), cystic fibrosis, cow's milk allergy (cause
eosinophilia because it is IgE mediated allergy)

39
o Clinical features: failure to thrive, dyspnea, wheezy chest, diarrhea, colicky
abdominal pain, abdominal distention
Diagnosis of hypertrophy without ECG:
o PMI = point of maximal impulse = apex beat normally in the mitral area but not
necessarily be in mitral area
o Left ventricular hypertrophy if we feel apex beat displaced downward the
cause mostly is congestive HF
o Right ventricular hypertrophy if we feel apex beat displaced upward the
cause mostly is TOF
Diagnosis of pneumonia without X-ray:
o Hear bronchial breathing with added sound, but bronchial breathing without added
sound is plural effusion
Hyper-dynamic circulation PDA, Aortic regurgitation, HF, thyrotoxicosis, anemia
Dilated cardiomyopathy 30% return normal, 30% have restrictive myocarditis, 30%
will die.
Most common causes of H.F in children: VSD, PDA, ebstein anomaly, common AV
channel (in Down's syndrome)
Timing table in heart diseases in pediatric:
o 12 hours all cyanotic CHD like TGA and tricuspid atresia (presented as tricuspid
stenosis)
o 1 – 2 weeks PDA discovered as Heart failure
o 8 – 12 weeks VSD
o 6 months Secondum ASD
o 6 – 9 months TOF
