Post Mortem Pathology / Equine Diseases / Dr. Saevan Saad Al-Mahmood
1
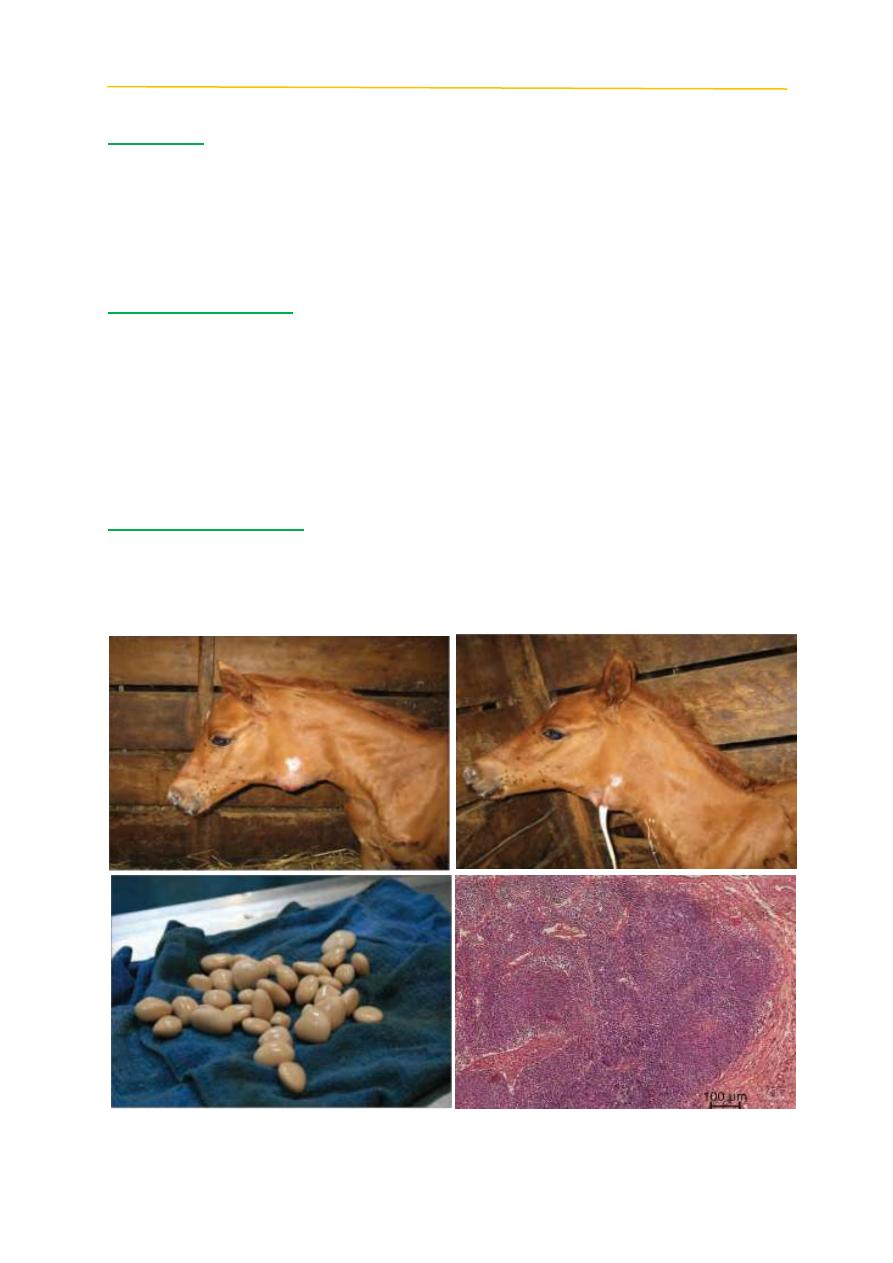
Strangles
Definition:
Worldwide acute upper respiratory infection in horses resulting in high
morbidity low mortality caused by gram-positive coccus Streptococcus equi
subspecies equi, infection is characterized by fever, lethargy, purulent nasal
discharge, and regional lymph node abscessation, and complications include
purpura hemorrhagica and metastatic abscessation.
Post mortem findings
Strangles is typically characterized by formation of abscesses of lymph
nodes of the head and neck 7-10 days following exposure. The most common
lymph nodes affected are those under the jaw. These abscesses may open and
produce a thick yellow drainage which may also be seen as a nasal discharge. The
symptoms of the disease following exposure to a group of horses can vary from
severe lymph node enlargement with difficulty breathing to no outward signs with
a slight nasal discharge.
Differential diagnosis:
1- Glanders.
2- Epizootic Lymphangitis.
3- Ulcerative Lymphangitis.
Post Mortem Pathology / Equine Diseases / Dr. Saevan Saad Al-Mahmood
2
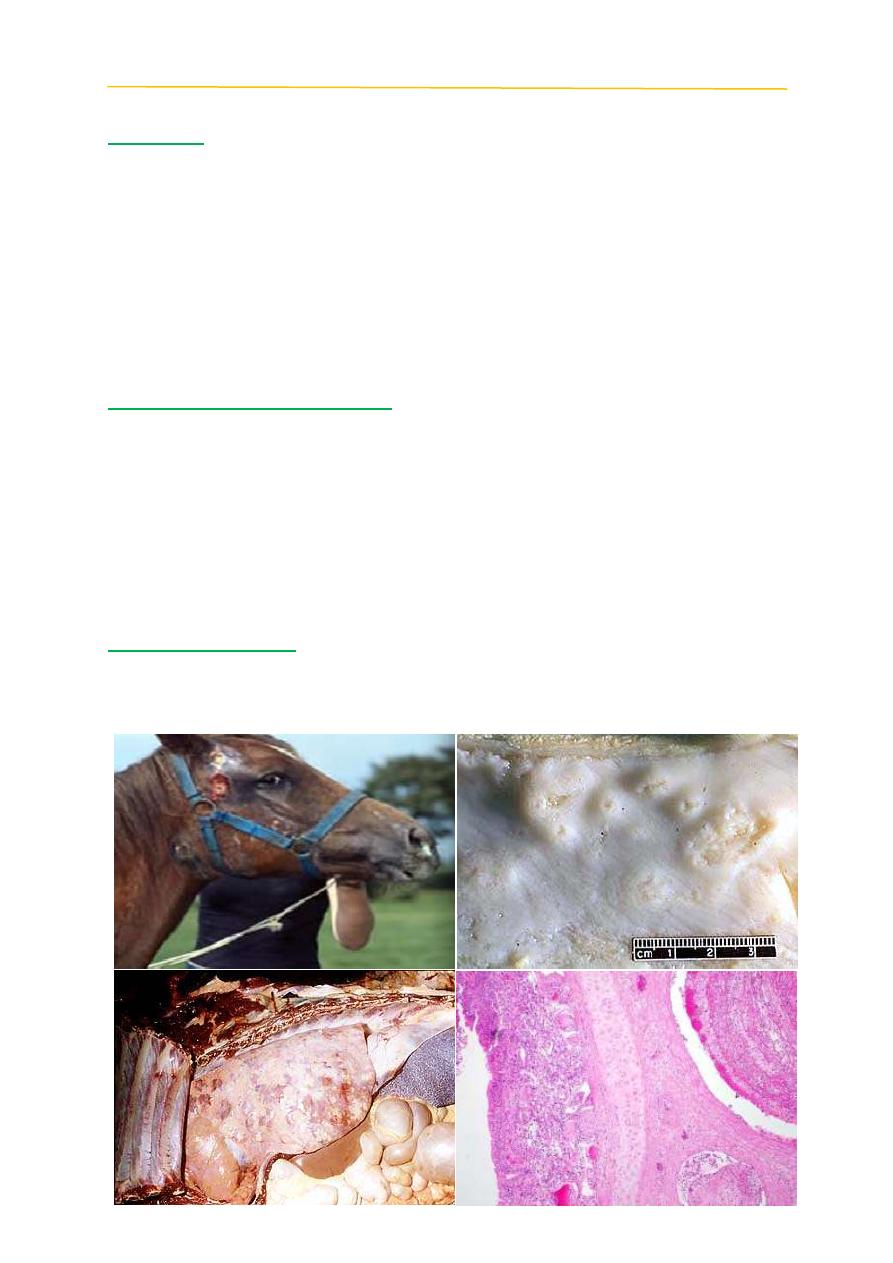
Glanders
Definition:
Highly contagious, zoonotic, fatal disease of horses, donkeys, and mules,
caused by infection with the
Burkholderia mallei
, characterized by ulcerating
granulomatous lesions of the skin and mucous membranes, also known as
equinia
,
malleus
,
droes
, and
farcy
.
Farcy
is an ancient term for a particular cutaneous manifestation of glanders
that before 1882 was believed to be a separate disease of horses. With this
cutaneous manifestation of glanders, nodular abscesses (farcy buds) become
ulcerated, and regional cutaneous lymphatic pathways become thickened (farcy
pipes) and ooze a glanders typical yellow-green gelatinous pus (farcy oil).
Clinical and Post Mortem Signs:
1-Cutaneous: It consists of nodules, pustules and ulcers that occur over any part
of the body but are most frequently observed on the legs. These nodules usually
appear in chains along the course of the lymphatic vessels.
2- Pulmonary: It is characterized by the formation of round, greyish, firm,
encapsulated nodules embedded throughout the lung tissue.
3- Nasal: Appears in the form of nodules or ulcers in the upper air passages. A
bloody mucopurulent nasal discharge appears when those nodules rupture.
4- Asymptomatic: Develops after a period of illness of some months.
Differential diagnosis
1- Epizootic lymphangitis.
2- Ulcerative lymphangitis.
Post Mortem Pathology / Equine Diseases / Dr. Saevan Saad Al-Mahmood
3
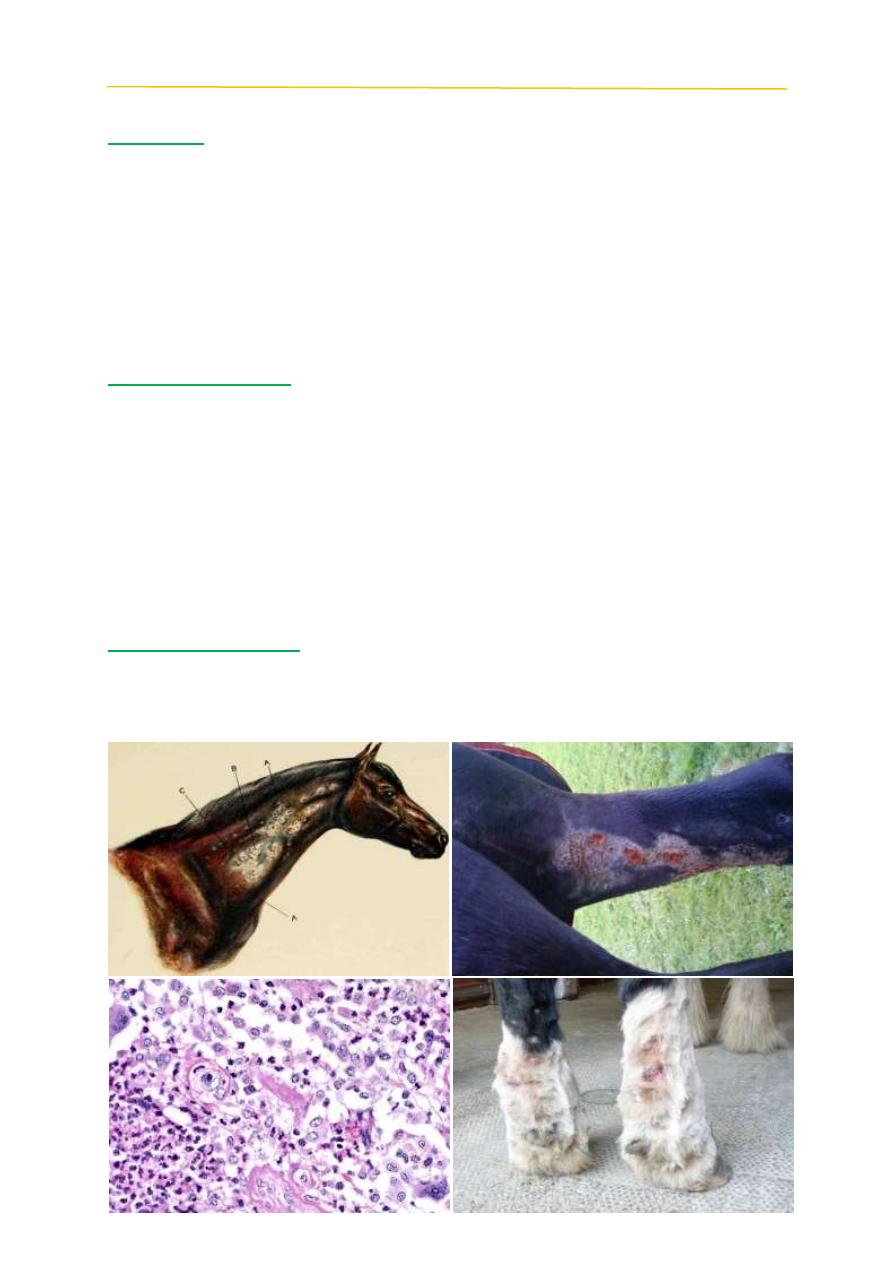
Epizootic lymphangitis
Definition:
Epizootic lymphangitis is a debilitating, contagious, chronic disease of
horses and other Equidae characterised clinically by a spreading, suppurative,
ulcerating pyogranulomatous dermatitis and lymphangitis. This is seen
particularly in the neck, legs and chest. It can also present as an ulcerating
conjunctivitis, or rarely a multifocal pneumonia. Transmission is by contact of
infected material with traumatised skin. Epizootic lymphangitis results from
infection by a dimorphic fungus,
Histoplasma capsulatum
var.
farciminosum
this
organism has also been known as
Histoplasma farciminosum
.
Post Mortem Lesions
At necropsy, areas of the skin and subcutaneous tissue are thickened, and
the skin may be fused to the underlying tissues. The regional lymph nodes may
be enlarged and inflamed. Nodules in the skin have a thick, fibrous capsule and
the affected lymphatic vessels are usually thickened or distended. Both nodules
and lymphatics contain purulent exudates. Multiple, small, gray–white nodules
or ulcers with raised borders and granulating bases may be apparent on the nasal
mucosa, and lesions may be found on the conjunctiva and cornea. The lungs,
spleen, liver, testes and other internal organs may also contain nodules and
abscesses.
Differential diagnoses
1- Glanders (farcy) caused by Burkholderia mallei.
2- Ulcerative lymphangitis due to Corynebacterium pseudotuberculosis.
3- Strangles.

Post Mortem Pathology / Equine Diseases / Dr. Saevan Saad Al-Mahmood
4
Ulcerative lymphangitis (pigeon fever)
Definition:
Highly contagious bacterial infection of lymphatic vessels of skin in horses
characterized by skin abscesses that present in limbs caused by Corynebacterium
pseudotuberculosis is the classical cause of the disease however, other pathogens
such as Staphylococcus aureus have been isolated.
Clinical signs
Diffuse or localized swellings, ventral pitting edema, ventral midline
dermatitis, lameness, draining abscesses or tracts, fever, weight loss, and
depression. A marked or prolonged fever, anorexia, or weight loss indicates
untoward sequelae such as deep or recurring abscesses, internal abscessation, or
systemic infection with abortion.
Post Mortem Findings
Ulcerative lymphangitis appears as a severe cellulitis in one or more limbs
with draining ulcerative lesions. Skin abscesses were present around the hock
joints on the hind limbs, on the chest, and on abdominal and neck skin ranging
from 0.5 to 6 cm in diameter which drained there contained to the surface of the
skin and contained bright green purulent discharge, the exudate is odorless, thick,
tan, and blood tinged.
Differential diagnosis:
1- Glanders (farcy).
2- Epizootic lymphangitis.
3- Strangles.
Post Mortem Pathology / Equine Diseases / Dr. Saevan Saad Al-Mahmood
5
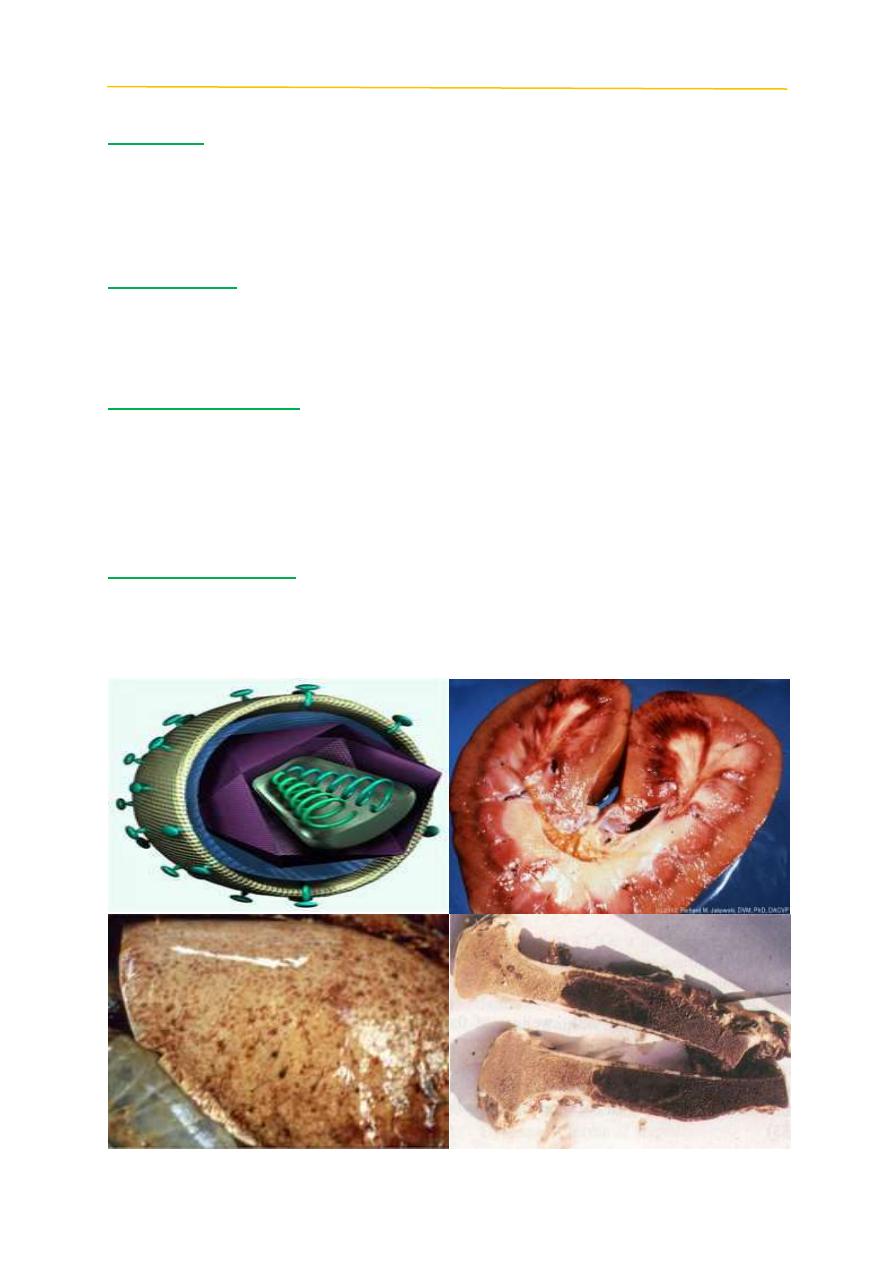
Equine infectious anemia (EIA)
Definition:
Retroviral disease of equids that may be characterized by acute and/or
chronic recurring clinical signs including fever, anemia, edema and cachexia. It
is caused by equine infectious anemia virus (EIAV), a lentivirus in the family
Retroviridae (subfamily Orthoretrovirinae).
Clinical Signs:
The clinical signs of acute EIA are often nonspecific. In some cases, in
horses the only sign is a fever, which is sometimes accompanied by transient
inappetence.
Post mortem findings:
The spleen, liver and abdominal lymph nodes may be enlarged, and the
mucous membranes can be pale. In chronic cases, emaciation may also be noted.
Edema is often found in the limbs and along the ventral abdominal wall. Petechial
hemorrhage observed on spleen and kidney. Mucosal and visceral hemorrhages
and blood vessel thrombosis have also been reported.
Differential diagnosis
1-Equine viral arteritis.
2-Purpura hemorrhagica.
3-Leptospirosis.
