Asthma
DefinitionEpidemiology
Pathology and pathogenesis
Clinical presentation
Laboratory tests
Differential diagnosis
Common asthma types
Diagnostic criteria
Drug therapy
Acute severe asthma
Asthma is “a Chronic Inflammatory Disorder of the Airways” associated with airway hyper-responsiveness that leads to recurrent episodes of :
-Cough
-Chest tightness-Shortness of breath, and
-Wheezing.
Asthma
The Hyper-responsiveness to different types of stimuli usually inhaled is manifested as reversible airway obstruction, either spontaneously or with treatment .
Epidemiology and Natural History
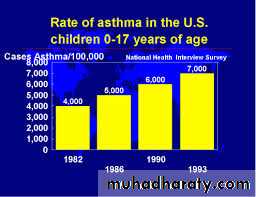
Asthma is one of the most common chronic conditions8.2% of the adult population in the United States are affected.
Asthma is diagnosed most commonly in children where allergy is common, but adult-onset asthma also occurs.
Asthma has a complicated hereditary process with multiple involved genes and likely gene-environment interactions.
The most important environmental factors appear to be airborne allergens and viral infections.
Diet, tobacco smoke, and air pollutants may also contribute to the development of asthma in susceptible persons.
are likely to have asthma.*
On average, 3 children in a classroom of 30*Epidemiology and Statistics Unit. Trends in Asthma Morbidity and Mortality. NYC: ALA, July 2006.
Pathogenesis
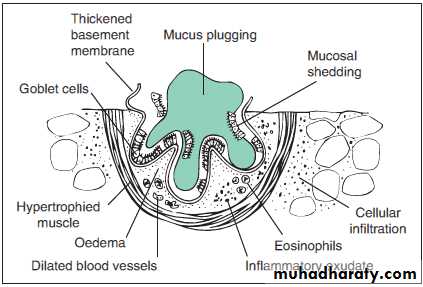
The central features of airway histopathology in asthma include :
Infiltration of inflammatory cells
Edema
Subepithelial fibrosis
Mucous gland and goblet cell hyperplasia and
Increased airway smooth muscle mass
Lymphocytes
During asthma exacerbations, the numbers of lymphocytes increased.Th2 cells predominating.Th2 cells generate higher quantities of IL-4, which is important in the production of IgE, and IL-5, which is essential for promotion of eosinophilic inflammation
Stored mediators (histamine and tryptase) as well as newly generated mediators (leukotrienes and cytokines) from mast cells plays a role in the development of early and late responses to inhaled allergens.
Eosinophils
Are the most commonly detected inflammatory cells in patients with acute active disease specially patients with an allergic component to their disease.Interleukin-5 (IL-5) is involved in the development, activation, and survival of eosinophils
Most patients with sputum eosinophilia respond to treatment with corticosteroids.
Neutrophils
Contribute significantly to the pathogenesis of persistent asthma.If neutrophils are present, the disease tends to be less reversible with inhaled bronchodilators, less responsive to corticosteroid therapy, and associated with reduced lung function.
Macrolide antibiotics may be effective in treating neutrophilic asthma.
Airway remodeling
Structural alteration in the airway, including subepithelial fibrosis, increased muscle mass, angiogenesis, and mucous gland hyperplasia.These changes probably contribute to increased airway obstruction, decreased reversibility, and increased morbidity.
Subepithelial fibrosis may be beneficial as it leads to increased airway stiffness and reduces the tendency toward airway closure.
increased airway obstruction decreased reversibility increased morbidity
Subepithelial fibrosis may be beneficial as it leads to increased airway stiffness and reduces the tendency toward airway closureAirway Remodeling
Airway Structural alteration
Subepithelial fibrosis
Increased muscle massAngiogenesis, and Mucous gland hyperplasia.
Symptoms and Signs
Patients with asthma typically present with recurrent cough, wheezing, chest tightness, and shortness of breath.
The cough is typically productive.
The symptoms of asthma can be intermittent, seasonal, or persistent.
Symptoms vary diurnally, being worse at night and in the early morning.
Precipitating and aggravating factors include exercise, environmental allergens, viral respiratory tract infections, cold air, stress
Most asthma exacerbations resolve spontaneously or in response to therapy, and the response is often complete.
Clinical examination is important for evaluation of associated conditions (nasal polyps, rhinitis, or sinusitis) and to assess the signs of airway obstruction (wheezing, use of accessory muscles and hyperinflation).
Differential Diagnosis of Asthma
Chronic obstructive pulmonary disease Less reversibility of airflow obstruction; associated with a history of tobacco use. May coexist with asthma in adults.Vocal cord dysfunction Abrupt onset of severe symptoms, often with rapid improvement. Monophonic wheezing
Heart failure Wheezing may be a manifestation of heart failure. Consider heart failure when there is not prompt improvement with asthma therapy and in persons with underlying cardiac disease.
Bronchiectasis Voluminous sputum production, often purulent, sometimes blood tinged. Suspect when physical examination shows clubbing or crackles with wheezing .
Pulmonary infiltration with eosinophilia syndromes Wheezing may occur in ABPA, eosinophilic pneumonia, and Churg- Strauss syndrome. Findings of infiltrates, striking peripheral blood eosinophilia, and constitutional symptoms, such as fever and weight loss, suggest chronic eosinophilic pneumonia.
Mechanical airway obstruction Respiratory noises may be more pronounced in the inspiratory or expiratory phase of respiration, depending on location of obstruction.
Cystic fibrosis Associated with thick, purulent sputum containing bacteria and gastrointestinal symptoms due to pancreatic insufficiency.
Pulmonary Function Testing
Spirometry is recommended in the initial evaluation of patients with suspected asthma and during follow-up evaluations.The FEV1/FVC ratio is typically greater than 75% in normal adults; a lower ratio indicates the presence of obstruction.
Significant reversibility of obstruction is indicated by a 12% or greater improvement in FEV1 after administration of a short-acting inhaled β2-agonist
Flowmeter
PEFR(Peak Expiratory flow rate) can be measured simply by flometer and can be used at home for serial measurement of lung function and to assess the relationship of lung function to symptoms.
The highest value of PEFR obtained during a 2-week period of stability is regarded as a patient’s personal best.
Obtaining subsequent values within 20% of the personal best suggests that the disease is stable.
PEFR reduction of 20% to 50% from personal best indicates a moderate increase in airway obstruction
A greater than 50% reduction suggests severe airway obstruction.
Bronchoprovocation
In patients who have symptoms suggestive of asthma but normal spirometry, bronchoprovocation with Methacholine can help establish the presence of airway hyperresponsivenessOccupational Asthma
Asthma related to the work environment can be based on allergic sensitization or nonallergic mechanisms.Resolution or significant improvement in symptoms during weekends and vacations .
Asthma symptoms may not occur during or immediately after exposure to the offending agent.
Cough-variant Asthma
In a subset of patients with asthma, cough can be the predominant or, at times, the only symptom.Must be differentiated from other causes of chronic cough
Patients with cough-variant asthma typically have airway hyperresponsiveness on methacholine challenge testing and can show evidence of obstruction on spirometry, with improvement after inhaled bronchodilators .
Asthma and Gastroesophageal Reflux Disease
Gastroesophageal reflux disease (GERD) is common in patients with asthma and can lead to chronic cough resembling that of cough-variant asthma or may result in worsening asthma control and severity.
Patients with refractory asthma should be evaluated for GERD even in patients with no heartburn.
Allergic Bronchopulmonary Aspergillosis (ABPA)
should be considered in patients with difficult-to-control asthma and a history of recurrent pulmonary infiltratesThe fungus Aspergillus fumigatus does not invade tissue, but it results in immune-mediated allergic inflammation, with subsequent damage to the bronchial wall and development of proximal bronchiectasis that can be best demonstrated on high-resolution CT scan of the chest.
Affected patients typically have eosinophilia, elevated serum levels of circulating IgE (total and specific IgE against A. fumigatus), and a positive skin test for Aspergillus.
The treatment of ABPA is similar to that of asthma with corticosteroids as initial therapy
Exercise-induced Bronchospasm
Exercise-induced bronchospasm (EIB) can develop in most patients with asthma.The more cold and more dry atmosphere is the more to induce bronchospasm.
The symptoms typically occur during or shortly after exercise, peak within 5 to 10 minutes after stopping the activity, and resolve in less than 30 minutes.
15% reduction in FEV1 after intense exercise is compatible with the diagnosis.
Approximately 10% of the athletes on the U.S. Olympic teams in recent years had EIB.
The bronchospasm can be prevented by adequate warm-up before exercise, by wearing a mask or scarf over the mouth in cold weather, or by therapy with short- or long-acting β2-agonists or leukotriene antagonists.
Short-acting β2-agonists given 10 to 15 minutes before exercise can prevent EIB for up to 3 hours.
Asthma-Provoking Drugs
• B blocking drugs even in small does as in patients with asthma who have glaucoma treated with ophthalmic preparations of timolol may experience bronchospasm.• B1-selective blocking agents such as atenolol may also provoke asthma specially with incresing doses
Persons taking angiotensin-converting enzyme inhibitor drugs may develop a chronic cough that can mimic asthma.
This cough may not be accompanied by additional bronchospasm
Asthma, nasal polyposis, and aspirin sensitivity form the “aspirin allergy triad.”
Leukotriene modifiers may be helpful in aspirin-sensitive asthma• Aspirin ingestion can cause acute, severe, and fatal asthma in a small subset of patients with asthma (10-15%).
• The cause of the reaction is unknown but probably involves the generation of leukotrienes.
• Most of the affected patients have nasal polyposis and are steroid-dependent for control of asthma.
• Many nonsteroidal anti-inflammatory drugs can trigger the reaction.
Asthma- Special Considerations
Bone health:Calcium and Vitamin D
Bone density study needed in
1-High dose ICS2-Previous oral steroids
Pregnancy and Asthma
1/3 Improve1/3 deteriorate
1/3 remains the same
Deterioration usually observed at late gestation
Inhaled corticosteroids and inhaled B agonists are the cornerstone in treatment
Other modalities may be needed and there is no strong objection against their use
British Thoracic Society
1- ≥20% difference on at least three days in a week for at least two weeks;
2-≥20% improvement of peak flow following treatment, for example:
1-10 minutes of inhaled β-agonist (e.g., salbutamol);2-six weeks of inhaled corticosteroid (e.g., beclometasone);
3-14 days of 30 mg prednisolone
3-20% decrease in peak flow following exposure to a trigger (e.g., exercise), or methacholine test
Treatment
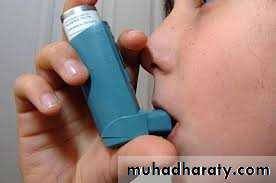
Pharmacotherapy for AsthmaControllers
Inhaled corticosteroidsInhaled long-acting B2- agonists
Inhaled cromones
Oral anti-leukotrienes
Oral theophyllines
Oral corticosteroids
Relievers
Inhaled fast-acting B2-agonists
Inhaled anticholinergics
B-Agonists1-Smooth muscle relaxation
2- Increased clearance of mucus3- Decreased release of mediators from cells
near epithelial surface
4- Decreasing edema
Short Acting B Agonist (SABA)
Long Acting B Agonist (LABA)• Long-term use of B agonist bronchodilators may adversely affect asthma; this also argues for earlier use of inhaled glucocorticoids.
Anticholinergic
Inhibit post-ganglionic efferent vagal fibers decreasing vagal toneGiven as inhalation : Ipratrobium Bromide
Corticosteroids
• Bind Glucocorticoid receptor• Corticosteroids reduce airway inflammation by modulating cytokines.
• Corticosteroids can inhibit the inflammatory properties of monocytes and platelets.
• Corticosteroids have vasoconstrictive properties reducing edema.
• Corticosteroids decrease mucous gland secretion
• • Resistance only in 1:10,000 patients
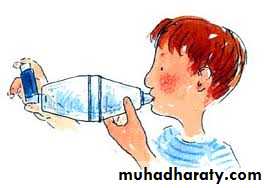
• The most common adverse effects of inhaled corticosteroids are dysphonia and thrush.
• These unwanted effects occur in about 10% of patients and can be reduced by using a spacer device and rinsing the mouth after administration.• Usually, Oral thrush can be treated successfully with oral antifungal agents.
• Dysphonia, when persistent, may be treated by decreasing or discontinuing the use of inhaled corticosteroids.
• The systemic effects of inhaled corticosteroids are very minimal
• There is evidence that high-dose inhaled corticosteroids can affect the hypothalamic-pituitary-adrenal axis , bone metabolism and may increase the risk of future development of glaucoma, cataracts, and osteoporosis.• Inhaled corticosteroids can decrease growth velocity in children and adolescents.
Inhaled glucocorticoids for mild persistent asthma is recommended because of the potential long-term benefits of reducing bronchial hyperresponsiveness and airway remodeling (fibrosis)
Effect of ICS + LABA vs Higher-dose ICS
• Addition of Salmeterol better than doubling the dose of ICS
• Better lung function• Better control of symptoms
• Less rescue therapy
• Less exacerbations
Leukotriene Antagonists
Inhibit Arachadonic acid metabolism into LT synthesis(inhibitors of 5-lipoxygenase)
Zileuton
Inhibit effect of leukotrienes at their receptors
ZafirlukastMontelukast
• Supplement to ICS
• ASA, NSAIDS sensitive patientsIgE Antagonist:Omalizumab
Humanized Ab against IgE (95% human)
Binds circulating IgE
Omalizumab:IgE inert complexes
Omalizumab is approved for use in refractory moderate to severe persistent asthma
Mast cell stabilizers
Sodium CromoglycateNedocromyl sodium
Stabilizes mast cells
Prevents mediator release
Prevents early and late reponses
Exercise induced asthma
Acute severe asthmaRisk factors
1-Previous attacks with A&E admition
2-Three or more drugs used in treatment
3-Large doses of B2 agonist use
4-Brittle asthma
Indicators of Severe Asthma
Anxious & diaphoretic appearance, upright position
Breathlessness at rest and inability to speak in full sentencesPaCO2 normal or increased
PEFR < 200 L/min or <50% predicted
Pulse oximetry < 91% on room air
Tachycardia (HR>120) and tachypnea (RR>30)
Approach to Severe Asthma
Reverse bronchoconstrictionTreat airway inflammation
Correct hypoxemia
Consider differential diagnosis
Monitor for complications
Pneumothorax
Hypotension
Differential diagnosis
1-Left ventricular failure2-Acute exacerbation of COPD
3-Acute pulmonary embolism
4-Severe chest infection
Management
Inhaled B-agonists are the treatment of choice
The optimal dose of inhaled B-agonists varies among patients; dose should be titrated to effect
Safe in patients with underlying cardiac disease
SC B-agonists are an alternative to inhaled B-agonist if the patient is unable to tolerate inhaled B-agonistsAnticholinergics
Multiple doses of inhaled ipratropium bromide in addition to B-agonists lead to a significant improvement in pulmonary function tests, but it may cause dryness of secretionSteroids
All patients with a severe asthma exacerbation should receive steroidsI.V. Hydrocortisone 100-200mg qds
60 – 125 mg IV methylprednisolone
40-60 mg PO prednisone
Maintenance of hydration
Treatment of secondary chest infection with broad spectrum antibioticAssisted ventilation
Intubation and assisted ventilation is very infrequently neededDecision should be based on
1-Clinical deterioration (altered mental status, respiratory fatigue)
2-Rising Paco2 with declining PaO2
3-Cardiovascular collapse
Oxygen
Oxygen administration in high flow and unrestricted concentration may be needed