Chronic Obstructive Pulmonary Disease
An important cause of chronic morbidity and mortality among patients over 55 yearsThe Global Initiative for Chronic Obstructive Lung Disease(GOLD)
A common preventable and treatable disease characterized by persistent and progressive airflow limitationThe presence of airflow limitation is established by spirometry:
If (FEV1) /(FVC) is less than 0.70 after administration of a bronchodilator, airway obstruction is indicated
SMOKING
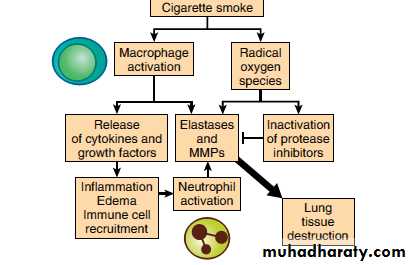
COPD is mostly related to extensive cigarette smoking.Smoking
Pathophysiology of COPDThe results of the lung tissue damage are mucus hypersecretion, airway narrowing and fibrosis, destruction of the parenchyma and vascular changes.
Airflow limitation is the end result
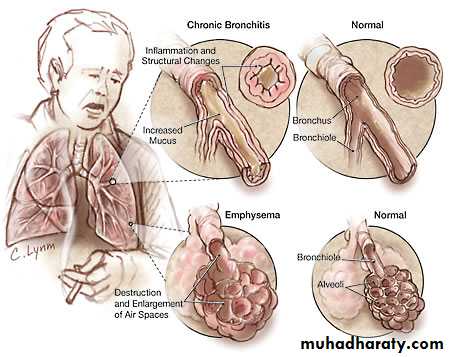
Chronic bronchitis is defined a cough and mucus production on most days for at least three months a year during at least two successive years
Emphysema is abnormal and permanent destruction and dilatation of the airspaces distal to the terminal bronchioles, resulting in loss of capillary-alveolar units
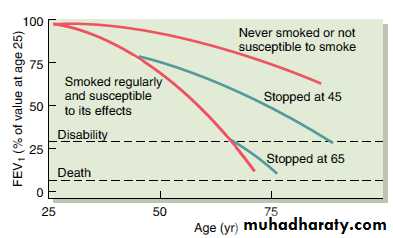
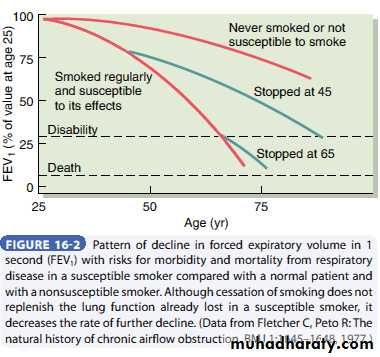
The non-smoking population shows a decline in FEV1 of approximately 20 ml/ year
Compared with an annual FEV1 decrease of 50–60 ml/year in smokersThe inflammation in COPD is markedly different from that in asthma.
Since inflammation is a feature of COPD, anti-inflammatory therapies may have beneficial effects in controlling symptoms, preventing exacerbations, and slowing disease progression.However, the response of inflammation to corticosteroids is poor in COPD, contrary to their effectiveness in asthma
However, asthmatic airway hyperreactivity can be seen in patients with COPD , the inflammation in their lungs may show characteristics of both diseases.
The functional results
Inflammatory narrowing and remodelling of the bronchi and bronchioliProteolytic digestion of the connective-tissue framework of the lung
Lung hyperinflation caused by loss of lung elastic recoil and air trappingImpaired mucociliary clearance
Loss of alveolar surface area and capillary bed
Increased pulmonary vascular resistance caused by vasoconstriction ( as a response to chronic hypoxia) and loss of capillary bed.
Risk factors
The disease arises from an interaction between host factors and environmental exposure.Cigarette smoking is the main risk factor
Additional risk factors for COPD.Heavy exposure to occupational dust (e.g. farming).
Indoor pollution including Passive smoking.
Low socioeconomic status.
Inherited α-1 antitrypsin deficiency, is responsible for approximately 2% of all cases of emphysema in the United States .
Respiratory infections.
Airway hyperresponsiveness may also contribute .
Prevalence
In the United Kingdom COPD affects 6% of men and 4% of women aged over 45
Clinical Assessment
Dyspnea : Exertional increasing over yearrCough, initially at morning with sputum
Wheezes
Sputum production
Recurrent respiratory infections.
Physical examination
Lung hyperinflationIncreased respiratory rate
Prolonged expiration, expiratory +_ inspiratory wheezes and coarse crepitations
Signs of R sided Heart failure
1-
2-
3-
4-
Concomitant diseases such as coronary heart disease, peripheral vascular disease , renal disease and Diabetes has to be looked for in COPD patients as co morbidities
Pulmonary function testing
Reduction in FEV1(<80%) and in the ratio of FEV1 to forced vital capacity (FVC) (<70%)Increase in total lung capacity and residual volume and with
Reduction in diffusing capacity for carbon monoxide, which correlates with the degree of emphysema.
Arterial blood gas analysis should be performed in patients with an FEV1 <50% predicted or clinical signs of right heart failure.
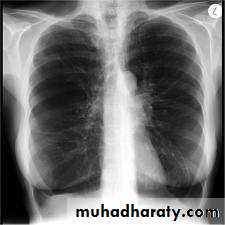
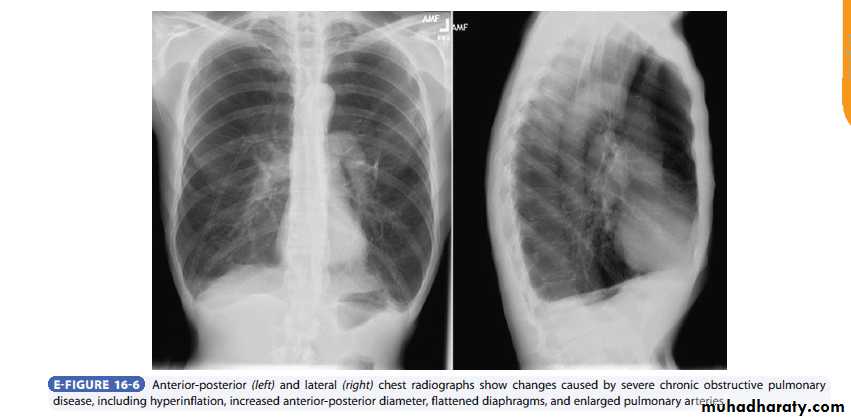
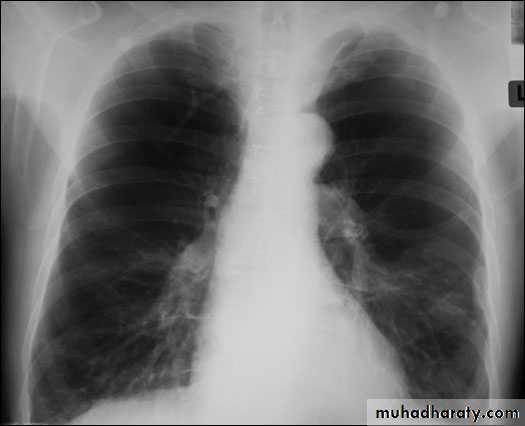
Radiology
Chest x-rayHyperlucency
Vascular attenuationHyperinflation (emphysema).
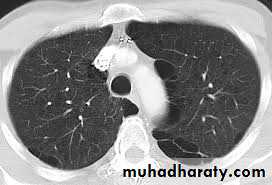
High-resolution CT is the most sensitive and specific technique for detection of pulmonary emphysema and grading of its severity.
It is not recommended for routine clinical assessment of COPD, it may be used to evaluate the feasibility of lung volume reduction surgery.
Polycythemia suggest chronic hypoxaemia.
ECG changes may be observed.Serum α-1 antitrypsin is indicated in patients with early manifestations of emphysema.
Six-minute walking distance may be used to quantify global functional impairment.
Emphysema
CT scan in Emphysema
Chronic obstructive bronchitis
Management of COPD
Relief of symptomsImprovement of exercise tolerance
Improvement in health status and quality of life
Prevention of disease progression
Prevention and treatment of complications and exacerbations
Reduction in mortality due to respiratory illness
Bronchodilators
Decrease shortness of breathBut they don’t modify the decline of lung function or improve the prognosis of the disease
Inhalation is the best way of administration
β2-agonists alone or in combination with anticholinergics can be used.
Long-acting inhaled β2-agonists may be the most convenient for continuous symptomatic relief.
Slow-release xanthines are effective in COPD but are a second-line choice due to their potential toxicity, they may be added to regular inhaled bronchodilators in more severe COPD.
Besides bronchodilatation, theophylline shows various physiologic actions such as increased central respiratory drive, mucociliary clearance, respiratory muscle endurance, cardiac output, and dilatation of pulmonary arteries
Anticholinergics: Inhibition of vagal stimulation of the bronchial tree is associated with reduced smooth muscle tone and bronchial gland secretion, these drugs are very safe.
Tiotropium, is a new long-acting anticholinergic bronchodilator which is inhaled only once daily
Combining drugs whose mechanisms and duration of action differ increases the degree of bronchodilatation and lessens the probability of side effects
Glucocorticosteroids
The effects of glucocorticosteroids on airway inflammation in COPD are much less pronounced than in asthma.Prolonged treatment with inhaled glucocorticosteroids does not modify the long-term decline in FEV1 in patients with COPD
Short course steroid
Short course systemic steroids are of great importance in acute exacerbationsShorten recovery time
Restore lung function more quickly,Decrease the need for hospitalizations, and shorten hospitilization time
Steroid trial
The response to the trial should be assessed by spirometry to identify patients with significant reversible airways obstruction (i.e. an increase in FEV1 >200 ml and >12–15% from prebronchodilator baseline measurements) to detect a component of associated bronchial asthma .This trial should be done on a stable phase of the disease, at least 6 weeks after an exacerbation
Antibiotics
The use of antibiotics, other than to treat infectious exacerbations, is not recommendedVaccination
Influenza vaccination Yearly Influenza vaccination reduces serious illness and death in COPDPneumococcal vaccine: about 50% of invasive pneumococcal infections could be prevented by the vaccination.
Haemophilus influenzae vaccine Oral vaccination, in the autumn
Long-term oxygen therapy (LTOT)
Survival of patients with COPD-induced hypoxaemia is improved by long-term O2 therapy, and the benefit is greatest if the treatment is administered for at least 15–18 h/day .
Long-term oxygen therapy (LTOT) is indicated if
1-PaO2 is ≤55 mm Hg) with or without hypercapnia
2-Between 55 and 59 mm Hg if symptoms or signs of right heart failure and or polycythemia are present.
The primary goal of oxygen therapy is to increase the baseline arterial partial pressure (PaO2) to at least 8.0 kPa (60 mm Hg) or to achieve arterial oxygen saturation equal to or above 90%.
Nasal catheter for Oxygen
Alpha-1-antitrypsin replacement ; Patients with documented severe deficiency and established emphysema who have stopped smoking may be considered candidates for this therapy.
Surgical approaches
Bullectomy i.e. the removal of large bulla compressing the adjacent lung structures is effective in reducing dyspnoea and improving lung function .Lung volume reduction surgery (LVRS) is a palliative procedure improves pulmonary function , exercise capacity and quality of life for several years
Lung transplantation In appropriately selected patients with very advanced COPD and an estimated life expectancy below 6–18 months