Interstitial Lung Diseases
A group of disorders affecting primarily the Interstitium but also affects the parenchyma (Alveoli and respiratory bronchioles) and the vascular bed .The ultimate result of these disorders is reduction of pulmonary volumes and capacities
..
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
.
ALVEOLUS
INTERSTITIUM
CAPILLARY
Common clinical features
Symptoms 1-Chronic dry cough2-Exertional dyspnea
Signs 1-Clubbing
2-Basal inspiratory crepitations
Laboratory 1-High ESR
2-Pulmonary infeltrate and reduced lung size
3-Restrictive pattern of pulmonary function tests
Pulmonary Function Tests
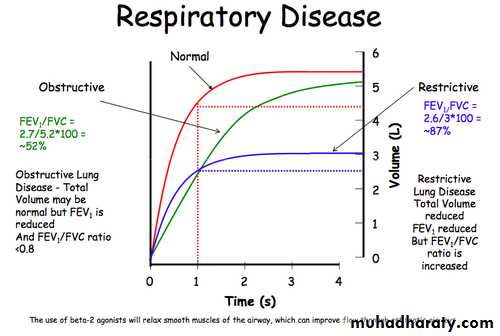
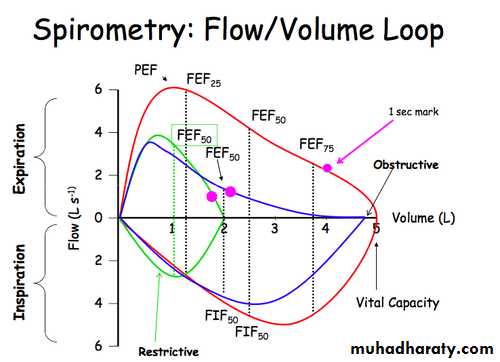
Spirometry 1-Decreased FEV1,FEV(Normal FEV1/FVC)
2-Decreased TLC
3-Mildly Decreased PEF
4-Markedly Decreased DLCO
Blood gasses 1-Hypoxia
2-Hypocapnea
(Type 1 respiratory failure)
Rare features of ILD
1-Excessive sputum and hemoptysis2-Pleurisy
3-Wheezing
4-Chest pain
Blood tests
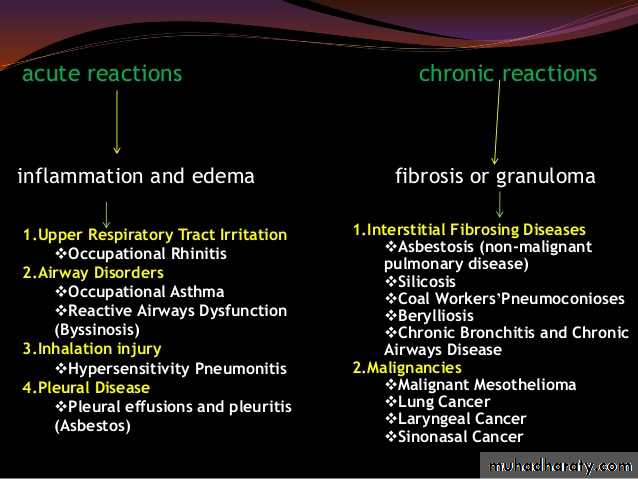
Interstitial Lung DiseaseOccupational
Treatment
related
Connective
tissue disease
Idiopathic
AsbestosisSilicosis
Coal Workers
pneumoconiosisRadiation
Methotrexate
Nitrofurantoin
Amiodarone
Chemotherapy
Sarcoidosis
Hypersensitivitypneumonitis
CFA/IPF
UIP/NSIPDIP
LIP
RB-ILD
BOOP
Immunological
Rh. Arthritis
SLEPolymyositis
Schleroderma
Sjogren’s
PULMONARY FIBROSIS
Localized unilateral fibrosis may result from a destructive pneumonia, trauma, or tuberculosisLocalized bilateral fibrosis may occur in bronchiectasis, tuberculosis, histoplasmosis and other chronic infections
Generalized fibrosis: In end-stage of a range of parenchymal lung disorders where the diffuse inflammatory process ends with diffuse fibrosis .
Idiopathic Pulmonary Fibrosis (Cryptogenic Fibrosing Alveolitis)
The most common of the interstitial lung diseases5-10 per 100 000 people
Men : women (2:1)
Most commonly seen in those over 65 years of age.
Alveolitis Alveolar destruction
Fibrosis Function impairment
The course of the disease
Usually is a progressive disease to end stage lung damage and respiratory failure over yearsMay have a rapid course (Months)
May be a mild disease discovered accidentally
Clinical Presentation
Exertional dyspnea Which increases in severity over months or yearsCough, Dry
Arthralgia even in absence of connective disease.
Clubbing of the fingers
Late inspiratory fine crackles at the lung bases.
Diagnosis
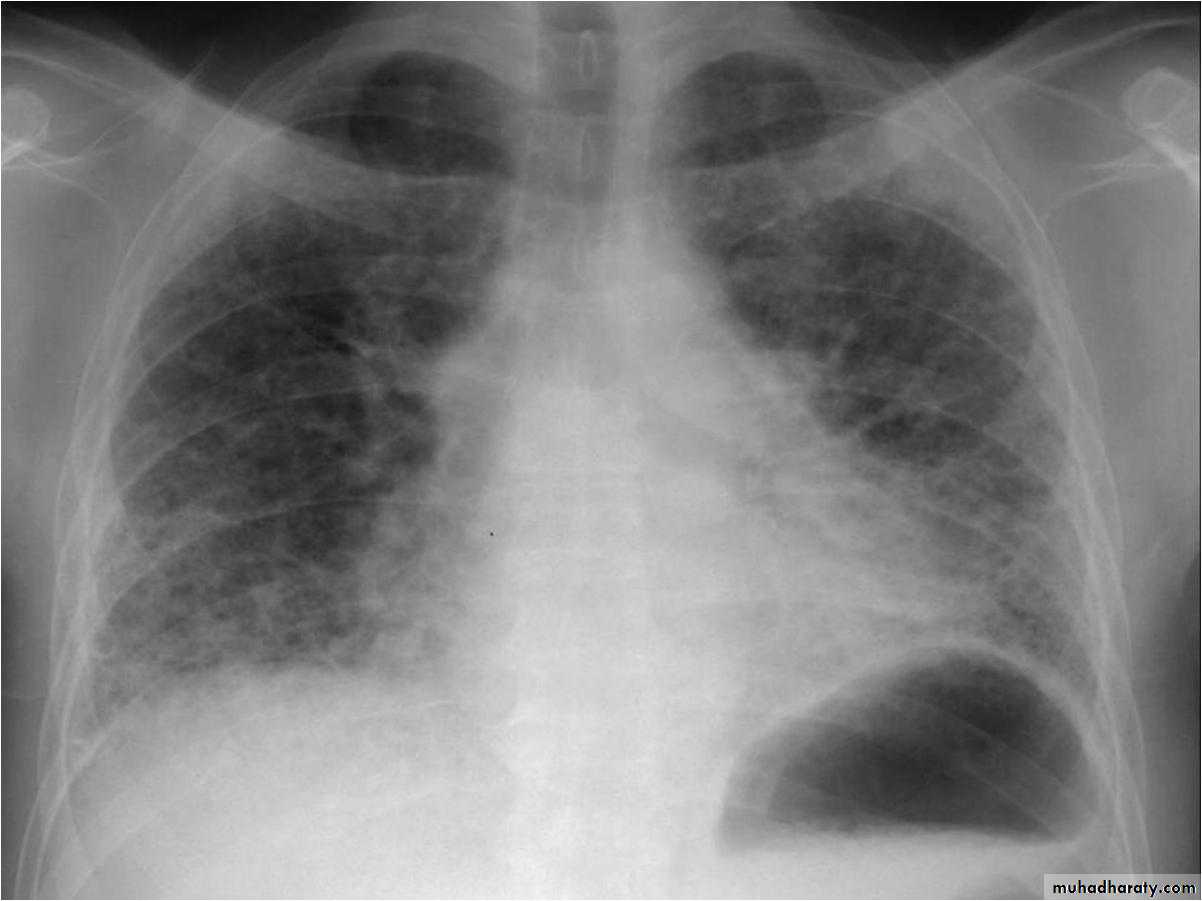
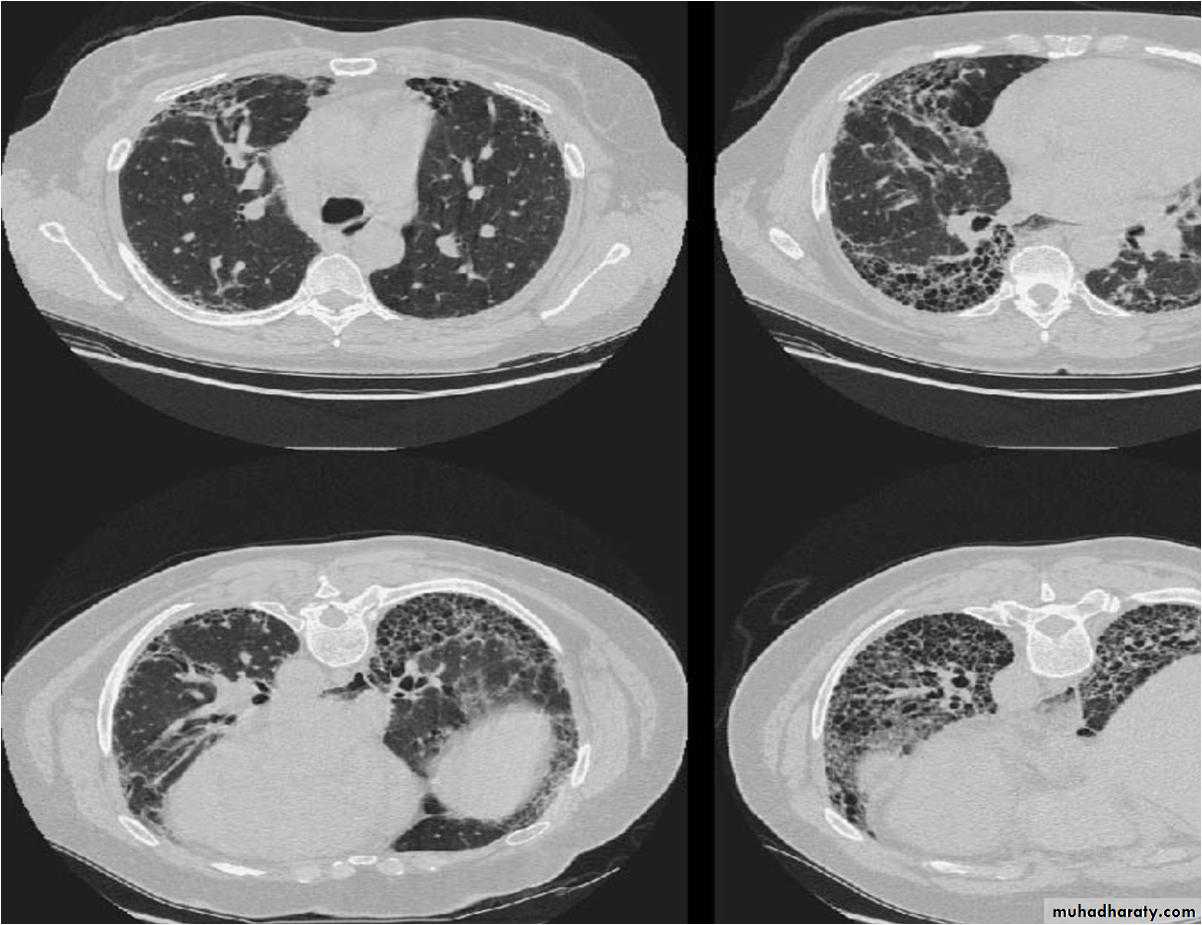
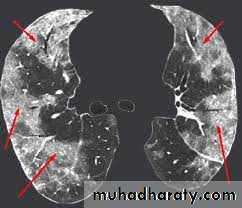
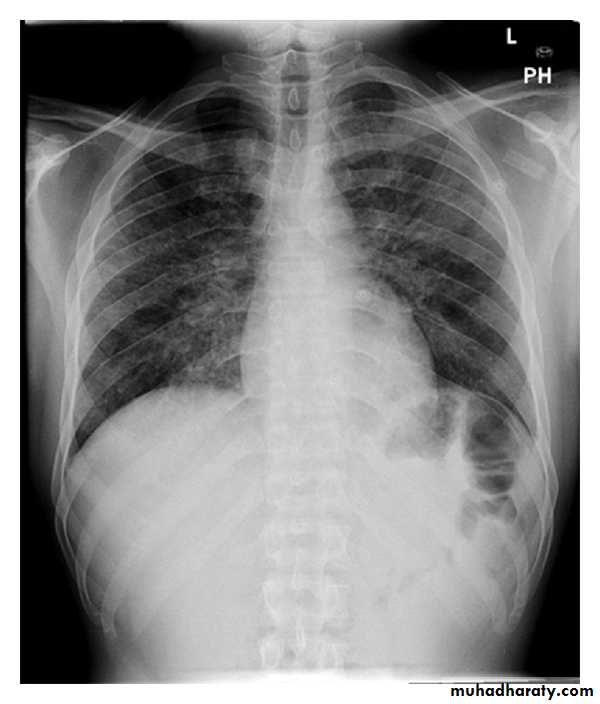
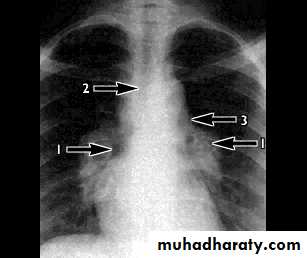
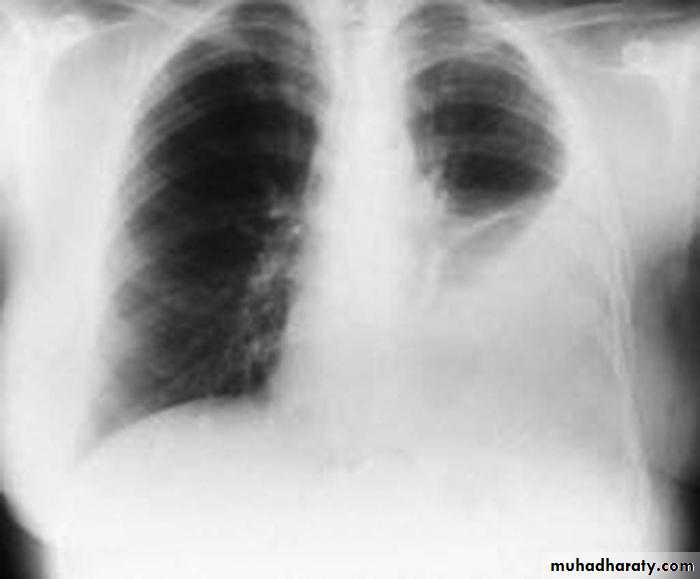
Chest X-rayLower zone shadowing
Decreased lung size
Pulmonary function tests show a restrictive defect, often with a great reduction in transfer factor.
ESR is usually moderately raised.
Positive autoantibodies and there is an association with other autoimmune diseases.
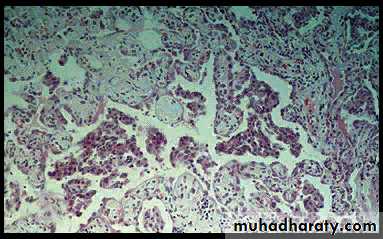
Lung biopsy may be necessary for diagnosis and shows characteristic changes
Pulmonary function tests
Treatment
Systemic corticosteroidsImmunosuppression with cyclophosphamide and azathioprine may be added.
The response to treatment is better if inflammation is more marked than fibrosis in the lung histology.
Prognosis
The long-term outlook is poor with a mean survival of 5 years.The causes of death are supervening infection, cor pulmonale or respiratory failure and bronchial carcinoma.
Younger and otherwise fit patients with severe disease should be considered for heart-lung transplantation.
Extrinsic Allergic Alveolitis(Hypersensitivity Pneumonitis)
A result of a hypersensitivity reaction in the lungs, provoked by a wide range of organic dusts.Repeated exposure of a susceptible individual to the offending antigen leads to the production of circulating precipitating antibodies and immune complexes and ultimately to macrophage activation and epithelioid cell granuloma formation.
Farmer’s lung is the most common cause, accounting for 50% of cases of extrinsic allergic alveolitis.
Bird fanciers lung occur in 5% of bird owners and 20% of pigeon keepers.
SymptomsSymptoms may develop within 6 hours of heavy exposure to the antigen or may appear insidiously over years.
The most common presentation is with breathlessness, dry cough and influenza-like symptoms (malaise, fever and muscle pains).
Investigations
Chest X-rayAcute phase :a fine nodular shadowing
Repeated exposure :fibrotic changes more marked in the upper azones, as with sarcoidosis, than in the lower zones, as with cryptogenic fibrosing alveolitis.
Lung function shows restrictive pattern (reduced TLC and FVC), Plus decreased DLCO
TreatmentThe provoking factor must be identified and removed
Systemic corticosteroids may be required and may accelerate recovery.
Sarcoidosis
A rare multisystem granulamatous disorder of young patients.
The Lungs and its Lymph Nodes are the mostly affectedBut it can involve the skin, eyes, peripheral lymph nodes, gut, liver, bone and CNS.
The pathological process is a granulomatous reaction.
There is a slightly increased incidence within families and in women.In the USA it is much more common in black patients.
clinical presentationThe most common clinical presentation of sarcoidosis is respiratory.
Nonspecific features such as tiredness, weight loss or recurrent fever. The characteristic lesions are
- Bilateral hilar lymphadenopathy , asymptomatic, subside without treatment in about 80-90% of patients
- Pulmonary infiltration and bilateral hilar lymphadenopathy which may cause symptoms such as dyspnoea, cough and fever, but subsides in 40% of patients
- Pulmonary fibrosis with diffuse infiltration, ultimately leading to a restrictive defect on respiratory function testing.
Evidence of the disease should be sought in the skin, eye and peripheral lymph nodes.
Diagnosis
Biopsy of lymph nodes, skin or lung.Lung function tests often show a restrictive defect
Mantoux test is often negative.
TreatmentTreatment of sarcoidosis depends on the extent of the disease and the tissues involved.
Parenchymal lung disease, acute eye involvement and CNS or heart signs require a prolonged course of steroids.
Minor skin or lymph node involvement can be watched over a period of months for spontaneous resolution.
Clubbing
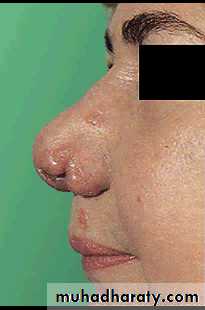
Sarcoid skin lesion
Lupus pernio
Lupus pernio
Pulmonary infeltrate
Hilar adenopathy
Pulmonary Infiltration with Eosinophilia
The association of blood eosinophilia and pulmonary shadowing may occur in a number of situations
Simple pulmonary eosinophilia
Short-lived and usually self-limiting illness with cough and a slight fever are associated with transient pneumonic shadowing and blood eosinophilia.Commonly due to worm infestation or drug therapy
Allergic BronchoPulmonary Aspergillosis (ABPA)
Presents as asthma with poor control and fleeting pulmonary infeltrate with marked blood and sputum eosinophilia
Tropical pulmonary eosinophilia,
Wuchereria bancrofti infectionIATROGENIC LUNG DISEASE
Radiotherapy, usually given for diseases such as cancer of the breast, bronchus, thymus or lymph nodes.The lung damage depends on
Total radiation doseDuration of time over which the dose is given
The number of treatments.
The concomitant use of pulmonary toxic chemotherapeutic drugs
Acute Radiation Pneumonitis
Occurs a few days to some weeks after exposure and presents with a cough, fever and progessive dyspnoea.
Corticosteroids may ameliorate these acute symptoms.
Chronic Radiation Pneumonitis
Fibrosis may develop over many months and there is evidence of a progressive restrictive defect in the pulmonary function tests with a decrease in transfer of carbon monoxide.Examples of drug induced lung damage
A large number of drugs, alone or in combination, may produce a range of respiratory problems that includeAsthma (e.g. b-blockers)
Infiltration or fibrosis (e.g. bleomycin, methotrexate)
Eosinophilia (e.g. nitrofurantoin)
Systemic lupus erythematosus-like syndromes (e.g. hydrallazine)
Respiratory depression (e.g. opiates, barbiturates)
ARDS- opiates , thiazides
Opportunistic infection (e.g. high dose steroids, immunosuppressives).
OCCUPATIONAL LUNG DISEASE
Lung diseases associated with industrial exposure are a common problem.They can be avoided if appropriate occupational regulations are enforced, especially efficient ventilation and individual protection by ventilators or masks..
VASCULITIS
Wegener's granulomatosisClassic Wegener’s granulomatosis consists of the clinical triad of
1-upper respiratory tract granulomas
2-fleeting lung shadows with cavitation
3-necrotizing glomerulonephritis
Allergic granulomatosis (Churg-Strauss syndrome)
Asthma that is difficult to controlhigh blood eosinophilia
lungs, nervous system, skin and heart are often involved
renal involvement is minimal
Pulmonary involvement in connective tissue diseases
Rheumatoid arthritis
Fibrosing alveolitisobliterative bronchiolitis and bronchiectasis
multiple or single pulmonary nodules, which may cavitate, and pleural effusions
Exhudative pleural effusion
Systemic lupus erythematosus
Pleurisy and pleural effusionlung atelectasis in