TUBERCULOSIS
PROF. Dr. ABDUL HAMEED AL QASEERTuberculosis (TB) is one of the oldest disease known to affect humans .
TB is a major cause of death worldwide .TB is caused by mycobacterium tuberculosis complex & usually affected the lungs .
Extrapulmonary TB in up to 1/3 of cases .
If properly treated , TB is curable in the majority of cases .
If untreated the disease may be fatal within 50-65% of cases .
Etiological Agent
M. tuberculosis is a rod-shaped, non-spore-forming, thin aerobic bacterium measuring 0.5 um by 3 um the bacilli cannot be decolorized by acid alcohol; this characteristic justifies their classification as acid-fast bacilli.
Acid fastness is due mainly to the organisms' high content of mycolic acids, long-chain cross-linked fatty acids, and other cell-wall lipids
• M. bovis (the bovine tubercle bacillus)
• M. caprae (related to M. bovis)• M. africanum (isolated from cases in West, Central, and East Africa)
• M. microti (the "vole" bacillus, a less virulent and rarely encountered organism)
• M. pinnipedii (a bacillus infecting seals and sea lions in the southern hemisphere and recently isolated from humans)
• M. canettii
Epidemiology
The WHO estimated that ~ 9.4 million new cases of TB occur worldwide in 2009 ( Asia ~ 5.2 million ;Africa ~ 2.8 million ; Middle East 0.7 million) .About 1.7 million deaths from TB in 2008 .
It had been suggested that ~ 1/3 of the whole world population were infected by TB .
The number of cases of TB increased in industrialized countries ,which may be related to:
1. immigration ;2. HIV ; 3. social problems ; 4.drug abuse .
Factors increasing the risk of TB
TB associated diseases
The incidence of TB per 100000 population (WHO)
Timetable of TBPrimary Disease
Primary pulmonary tuberculosis occurs soon after the initial infection with tubercle bacilli.Inspired air is distributed to the middle and lower lung zones-most commonly involved in primary tuberculosis.
The lesion -accompanied in more than half of cases by hilar or paratracheal lymphadenopathy.
It may be asymptomatic or fever & occasionally pleuritic chest pain( often in children).
Some patients develop erythema nodosum in the legs .
In the majority of cases , the lesions heal spontaneously.
2Progressive Primary Diseases
1)Lymphadenopathy (hilar-often unilateral, Paratracheal,or mediastinal)2)Pleural effusion
3)Endobronchial
4)Miliary
5)Meningitis
6)Pericarditis
Post-primary TB
It is the most important cause of morbidity & mortality of TB .
The onset is usually insidious (over several weeks) .systemic symptoms include fever, night sweats , malaise ,& loss of appetite & weight.
However , in up to 90% cough will develops , which started as dry cough & then may become productive .
Hemoptysis may occurs in 20-30 % of cases & it can be massive .
Physical examination reveals rales in the involved areas during inspiration , especially after coughing .
Occasionally rhonchi & classic amphoric breath sound heard over a large cavity .
The lesion usually localized to the apical & posterior segment of the upper lobes .
The supperior segment of the lower lobes are also more frequently involved .
Clinical presentation of TB
Chronic cough , often with hemoptysis .PUO .
Unresolved pneumonia .
Pleural effusion .
Asymptomatic ( CXR).
Weight loss .
Spontaneous pneumothorax .
CXR OF TB
CXR in TB
CT SCAN OF THE CHEST
Miliary TB• Blood borne dissemination of TB bacilli and characterised by:-
• 2-3 weeks of fever and night sweat .
• Anorexia and weight loss .
• Dry cough .
• Hepato-splenomegaly .
• On auscultation chest may be normal or with crackles.
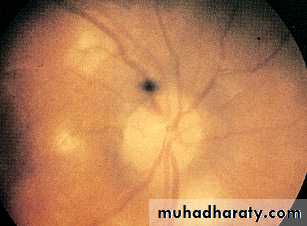
• Fundoscopy may show choroidal tubercle .
• Anaemia and leucopoenia may be present.
• Chest x-ray showed classical appearance of fine 1-2mm lesions distributed throughout the lung fields .
Chest x-ray & Fundoscopyin Miliary TB
Cryptic Miliary TB
This is unusual presentation seen in the elderly and characterised by:-
1)Age over 60 years.
2)Intermittent low-grade fever
3)Unexplained weight loss & general debility.
4)Hepatosplenomegaly in 25-50% .
5)Normal chest x-ray .
6)Negative tuberculin skin test.
7)Blood dyscrasia;leukaemoid reaction,pancytopenia
8)Confirmation by biopsy (granulomas and/or AFB demonstrated) of liver or bone marrow.
Chronic Complications of pulmonary TB
Massive haemoptysisCor-pulmonale
Fibrosis/emphysema
Atypical mycobacterium
Aspergilloma
Lung/pleural calcification
Obstructive lung disease
Broncheactasis
Bronchopleural fistula
Exudative pleural effusion
Spontaneous pneumothorax
Unresolved pneumonia
Extrapulmonary TB
DIAGNOSIS OF TB
1. Clinical features suggestive & high index of suspicion .2. CHEST – X- RAY : The initial suspicion of pulmonary TB based on abnormal radiographic finding in a patient with respiratory symptoms .
Any radiographic pattern-from small nodule to diffuse infiltrate may be seen . Although the ` classic `picture is that of the upper lobe with infiltrate & cavities .
CXR in TB
CXR OF TBDiagnosis of TB
Diagnosis of TB (Cont. )Sputum staining with auramine-phenol fluorescent test is preferred .
Sputum culture on ( Lowenstein- jensen) or Meddlebrook media for 4-6 weeks.
Liquid culture ( Bactec ) need shorter times ( 2-3 weeks ) .
Fibreoptic bronchoscopy wash may be needed when dry cough & no sputum obtained.
Biopsies of pleura , lymph node , or any solid tissue suspected .
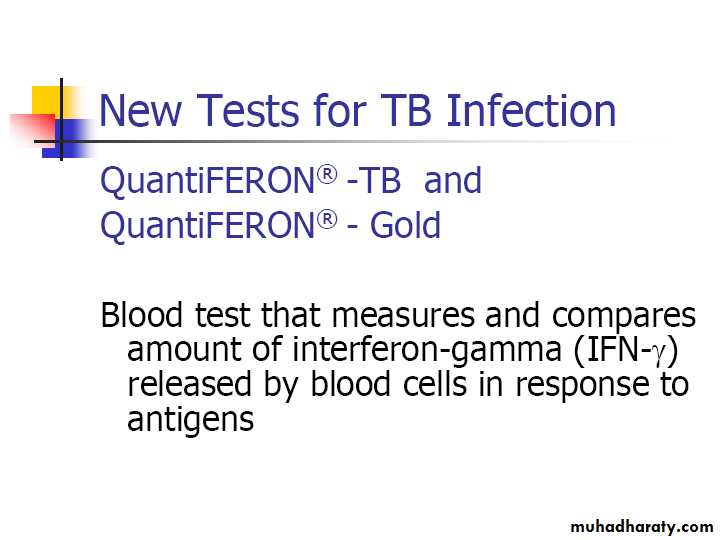
Whole blood interferon – gamma assay .
smear positive sputum
Specimen CollectionObtain 3 sputum specimens for smear examination and culture
Persons unable to cough up sputum, induce
sputum, bronchoscopy or gastric aspiration
Follow infection control precautions during
specimen collection
Drug sensitivity
It is particularly important in :1. those with a previous history of TB .
2. treatment failure .
3. chronic disease .
4. area with high prevalence of resistance .
5. those in contact with multiple drug resistance TB (MDR-TB).
MANANGEMENT OF TB
Four drugs are considered as the first- line of treatment of TB .
Streptomycin formerly used as a first – line drug now it is considered as a second – line drug with other injectable aminoglycosides .
Patients can be assumed to be non-infectious after 2 weeks of appropriate therapy .
The successful treatment of TB is the continuous self- administration of drugs for 6 months .DIRECTLY OBSERVED THERAPY SHORT COURSE (DOTS) in order to improve compliance to attend may be helpful .
Most patients can be treated at home .
Admission to hospital
1 . Uncertain diagnosis .2. intolerance of medication
3. questionable compliance .
4. adverse social conditions
5. significant risk of MDR- TB .
6. comorbidity
7. complication
TREATMENT OF TB WHO recommendation
main adverse reaction to drugs
Corticosteroids uses in TB
1. meningitis2 . Pericardial disease
3. in children with endobronchial obstruction
4. ureteric obstruction
5. pleural disease
6. extensive disease including Miliary TB
7. hypersensitivity drug reaction
Pat. With cavitary disease who do not achieve sputum culture conversion by 2 months require extended treatment .
A sputum specimen should be collected by the end of treatment to document cure.
If mycobacterial cultures are not practical , then monitoring by AFB smear exam. should be undertaken at 2,5 & 6 month.
Smear positive after 5 months are indicative of treatment failure.
CXR
Monitoring of the response to therapy by serial CXR is not recommended.However a CXR may be obtained at the end of treatment .
Monitoring treatment response
Patients with pul. Disease should have their sputum examination monthly until culture become negativeWith the recommended regimen > 80% of pat. Will have negative sputum culture at the end of 2nd month.
By the end of the 3rd month , virtually all pat. Should be culture negative .
When a sputum culture remain positive > 3 months treatment failure & drug resistant should be suspected.
Monitoring for drug toxicity
The most common is hepatitis .
Patients should be educated about signs & symptoms( e.g. dark urine, loss of appetite).
All adult pat. should undergo baseline LFTs (measurement of AST & ALT & bilirubin).
Older pat. ; those with concomitant disease ; alcoholic ; pat. With history of liver disease should be monitor closely ( i.e. monthly).
During initial phase of treatment up to 20% have increase AST &ALT (but < 3 times of normal ).
For elevation > 5 times treatment should be stopped !!!
Other side effects of the drugs
Hypersensitivity reactions usually require the discontinuation of all drugs & rechallenge to determine which agent is the culprit.Autoimmune thrombocytopenia secondary to rifampin should stopped it .
Optic neuritis need permanent discontinuation of ethambutol.
Isoniazid polyneuropathy
It is usually chronic occasionally subacute , sensorimotor (occasionally autonomic).To prevent INH-related neuropathy ; pyridoxine (10-25 mg\d) should be added to a high risk pat.
1. alcoholic 5. CRF
2. malnourished 6. DM
3. pregnant 7. HIV
4. lactating 8. those pat. on high dose.
TB & Renal failure
TB occurs 10 times more in CRF than in normal .INH is acetylated in the liver & excreted in the kidneys , so it is given 2-3 times per week.
E like INH .
INH & E & P should be given after dialysis.
INH & Z should be reduced in severe RF (except those undergo hemodialysis)
Aminoglycosides should be avoided in RF .
Rifampicin not affected by RF. !!
TB & Liver diseases
Pat. With severe liver disease may be treated with E & S .Pyrazinamide (Z) should be avoided .
If required , with INH & R under close supervision.
TB in HIV infected patients
• Mycobacterium tuberculosis :• 1. The incidence reflect background prevalence of TB in the community.
• 2. Most cases are due to reactivation .
• 3. TB may precede AIDS in HIV infections.
• 4. Extrapulmonary TB in HIV is an AIDS- defining Dx .
• 5. Diagnosis may be difficult.
• 6. Threat of MDR-TB .
• 7. Prognosis is poor ; TB accelerate HIV disease.
• 8. Extrapulmonary & disseminated TB is more common ( 60% versus 25%) .
• 9.The clinical presentation depends mainly on immune function .
TB in HIV (cont.)
10. In general response to anti-TB is good ?
11. Rifampicin-induced P450 CYP3A4 activity makes the choice of HAART complicated .
12. Drug reactions are more common in HIV-
infected pat.( esp. hepatitis & skin rashes).
13. Thiacetazone & streptomycin may cause
life-threatening reactions( must be avoided).
14. A syndrome resulting from HAART –induced reconstitution in up to 10% ( 4-6
weeks after anti- TB ; in pats. with CD4<50 cells/ mm3).
• Other Mycobacterial infections
• Mycobacterium avium intracellulare( MAI):• -Before HAART & primary prophylaxis , MAI occur in
• 35% of pats. In late-stage AIDS .
• - The incidence now fallen by 90% .
• -Features of MAI includes ; fever , wt. loss ,chronic
• diarrhea , hepatosplenomegaly , LAP ,anemia .
• - Therapy must consist of combination of ;
• Rifabutin + E + Aztheromycin + Ciprofloxacin
• -Prophylaxis with weekly azethromycin when CD4
• count > 100 cells/ cmm .
Control & prevention of TB
The best way to prevent TB is to diagnose & treat infectious cases rapidly & appropriately.
Detection of latent TB .
Skin testing with tuberculin- PPD (TST) is most widely used in screening for latent TB infection.
An otherwise asymptomatic contact with a positive TST , but normal CXR may be treated with
chemoprophylaxis to prevent infection to progressing to a clinical disease ( R+INH for 3 months
or INH for 6 months )
Vaccination ( BCG) .
In meta-analysis the overall protective efficacy is around 50% .