Cyanotic congenital heart disease
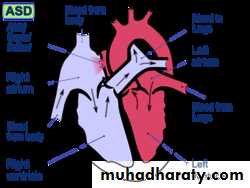
Classification of congenital heart diseases• Group I : Left to right shunts
• Group II: Right to lefts shunts
• Group III: Obstructive lesions
Left to right shunts
Atrial Septal DefectVentricular Septal Defect
Patent Ductus Arteriosus
Right to Left Shunts
• Tetralogy of Fallot• Tricuspid atresia
• Ebstein’s anomaly
• Transposition of Great Vessels
• Truncus Arteriosus
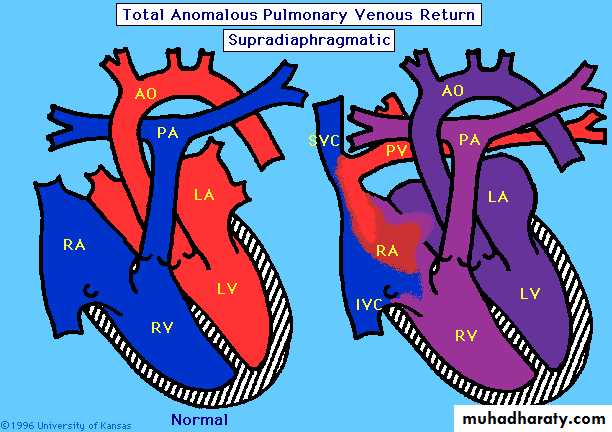
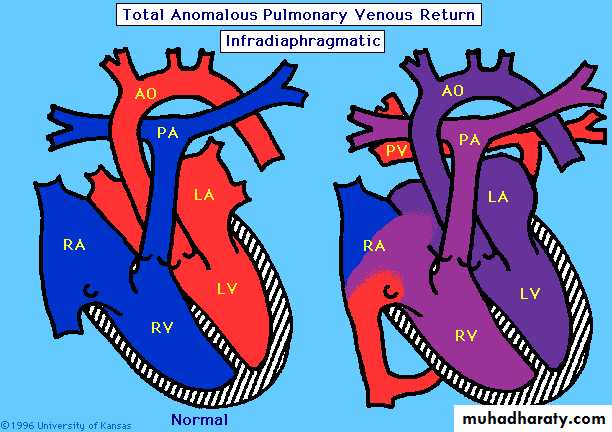
• Total Anomalous Pulmonary Venous Return (TAPVR)
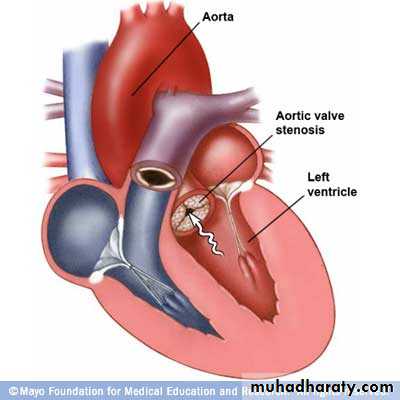
Obstructive Lesions
Aortic stenosisCoarctation of the Aorta
Pulmonic Stenosis
Cyanotic heart disease
Right to Left ShuntCyanotic heart disease
bluish or purplish tinge to the skin and mucous membranes.5 g/dL of unoxygenated hemoglobin in the capillaries
This usually correspond to oxygen saturation of 70-80%
Who is this guy?
ÉTIENNE-LOUIS ARTHUR FALLOT!
a French physician, 1888 Fallot accurately described in detail the four anatomical characteristics of tetralogy of Fallot.Tetralogy OF Fallot
Most common cyanotic heart disease!75%!
TOF
4 component!
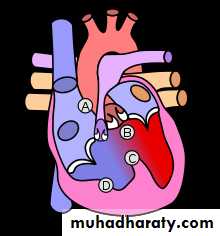
Imagine this is a HEART!
TOF
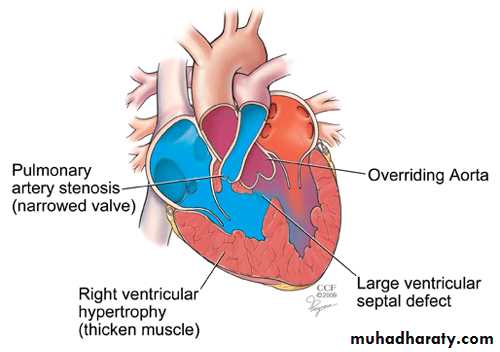
• Vetricular Septal Defect
TOF
• Vetricular Septal Defect
• Pulmonic Stenosis
TOF
• Vetricular Septal Defect
• Pulmonic Stenosis
• Overriding of dextroposed aorta
TOF
• Vetricular Septal Defect
• Pulmonic Stenosis
• Overriding of dextroposed aorta
• Right Ventricular hypertrophy
TOF
• Vetricular Septal Defect
• Pulmonic Stenosis
• Overriding of dextroposed aorta
• Right Ventricular hypertrophy
Concentric R ventricular hypertrophy without cardiac enlargement
TOF
• Vetricular Septal Defect
• Pulmonic Stenosis
• Overriding of dextroposed aorta
• Right Ventricular hypertrophy
Concentric R ventricular hypertrophy without cardiac enlargement
Increase in right ventricular pressure*RV and LV pressures becomes identical
RV and LV pressures becomes identicalThere is little or no L to R shunt
RV and LV pressures becomes identical
There is little or no L to R shuntHence, VSD is silent
RV and LV pressures becomes identical
There is little or no L to R shuntHence, VSD is silent
Right ventricle into pulmonary artery across pulmonic stenosis producing ejection systolic murmur
Hence, the more severe the pulmonary stenosis
Hence, the more severe the pulmonary stenosis
The BIGGER the Left to RIGHT shuntHence, the more severe the pulmonary stenosis
The BIGGER the Left to RIGHT shuntLess flow into the pulmonary artery
Hence, the more severe the pulmonary stenosis
The BIGGER the Left to RIGHT shuntLess flow into the pulmonary artery
Shorter the ejection systolic murmur
Hence, the more severe the pulmonary stenosis
The BIGGER the Left to RIGHT shuntLess flow into the pulmonary artery
Shorter the ejection systolic murmur
More cynosis because of less flow to the lung!
Hence,
Severity of cyanosis is directly proportional to the severity of pulmonic stenosisIntensity of the systolic murmur is inversely related to the severity of pulmonic stenosis
Congestive failure never occur* because…Right ventricle is effectively decompressed because of the ventricular septal defect.
* exception
Congestive failure never occur* because…Right ventricle is effectively decompressed because of the ventricular septal defect.
* exception
• Anemia• Infective Endocarditis
• Systemic hypertension
• Unrelated myocarditis complicating TOF
• Aortic or pulmonary valve regurgitation
Pulmonary obstruction results in delayed P2
Pulmonary obstruction results in delayed P2
Pulmonary artery pressure reducePulmonary obstruction results in delayed P2
Pulmonary artery pressure reduceP2 become soft or inaudible
Pulmonary obstruction results in delayed P2
Pulmonary artery pressure reduceP2 become soft or inaudible
(Second Sound) S2= A2 + P2
Since P2 is inaudible, hence S2 = A2 + P2
[S2 is single sound]Aorta is displace anteriorly too, A2 become LOUD!
Ascending aorta in TOF is large, results aortic ejection click
Diastolic interval is clearNo S3
No S4
Concentric right ventricular hypertrophy reduce the distensibility of the right ventricle during diastole
Concentric right ventricular hypertrophy reduce the distensibility of the right ventricle during diastole
“a” waves become prominent in JVP*
*but not too tallClinical Picture
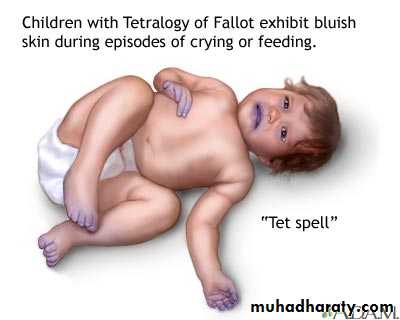
Symptomatic any time after birthParoxysmal attacks of dyspnea
Anoxic spells
Predominantly after waking up
Child cry
Dyspnea
Blue
Lose conscious
Convulsion
Frequency varies from once a few days to many attack everyday
“tet spell”
lethal,unpredictable episodes
The mechanism
spasm of the infundibular septum,which acutely worsens the RV outlet obstruction.
Dyspnea on exertion
Exercise intoleranceSitting posture – squatting
Compensatory mechanismSquatting increases the peripheral vascular resistance,
which diminishes the right-to-left shunt
increases pulmonary blood flow.
Cyanosis during feeding
Poor feedingfussiness, tachypnea, and agitation.
Birth weight is low.
Growth is retarded.
Development and puberty may be delayed.
Rarely, patient remain asymptomatic into adult life.
Physical examination
Clubbing + Cyanosis (Variable)
Squatting position
Scoliosis – Common
bulging left hemithorax
Prominent “a” waves JVP
Normal heart sizeMild parasternal impulse
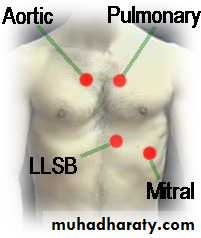
Systolic trill (30%)
S1 normal
S2 singleonly A2 heard
P2 soft & delayed: INAUDIBLE
Murmur
Shunt murmur (VSD) absent
Flow murmur: Ejection systolic, the smaller the flow the shorter the murmur
Ejection aortic click
Retinal engorgement
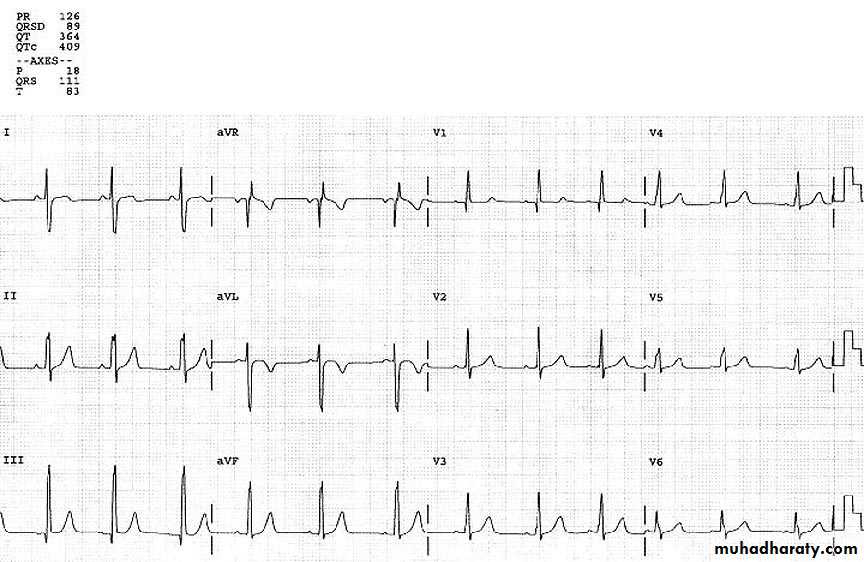
HemoptysisECG
ECG
ECG
ECG
ECG
ECG
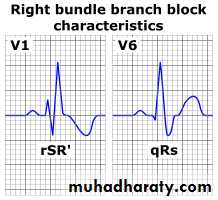
wiLLiam
moRRowECG
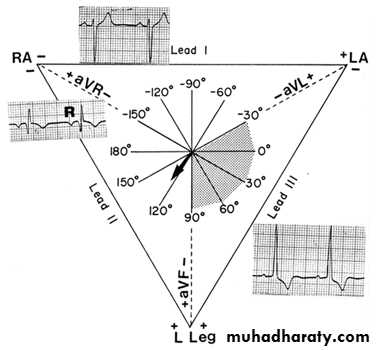
Right axis deviation (+120° to +150°)
Right or combined ventricular hypertrophy
Right atrial hypertrophy
Partial or complete right bundle branch block (especially true of patients after surgical repair)
Coeur en sabot (boot-shaped heart) secondary to uplifting of the cardiac apex from RVH and the absence of a normal main pulmonary artery segment
Normal heart size due to the lack of pulmonary blood flow and congestive heart failure
Decreased pulmonary vascularity
Right atrial enlargement
Right-sided aortic arch (20-25% of patients) with indentation of leftward-positioned tracheobronchial shadowEchocardiography
Reveals a large VSDoverriding aorta
variable degrees of right ventricular outflow tract (RVOT) obstruction
Course and Complication
• Each anoxic spell is potentially fatal
• Polycytemia
• Cerebrovascular thrombosis
• Anoxic infaction of CNS
• Neurological complication
•
• 4) LUNG is an awesome filter.
• Bypassing it may not be a good idea!• TOF, venous blood from gut, peripheral system by pass the lung and re-enter circulation
• Hence TOF can cause:
• Brain Abcess
• Infective endocarditis
• Paradoxical embolism
Management of anoxic spell
• Knee chest position
• Humified O2
• Be careful not to provoke the child
• Especially you are bad at gaining IV access
• Ask for help from someone more experience
• Permit the baby to remain with mother
• Morphine 0.1 -0.2 mg/Kg Subcutaneous
• Correct acidosis – Sodium Bicarb IV
• Propanolol
• 0.1mg/kg/IV during spells• 0.5 to 1.0 mg/kg/ 4-6hourly orally
• Vasopressors: Methoxamine IM or IV drip
• Correct anemia
• GA is the last resort
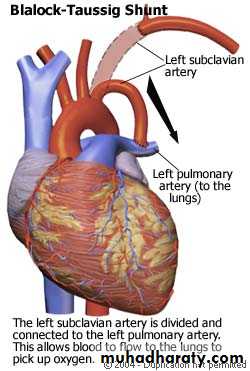
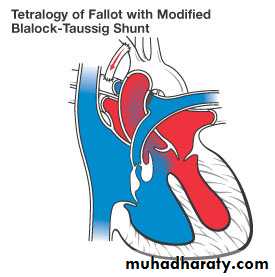
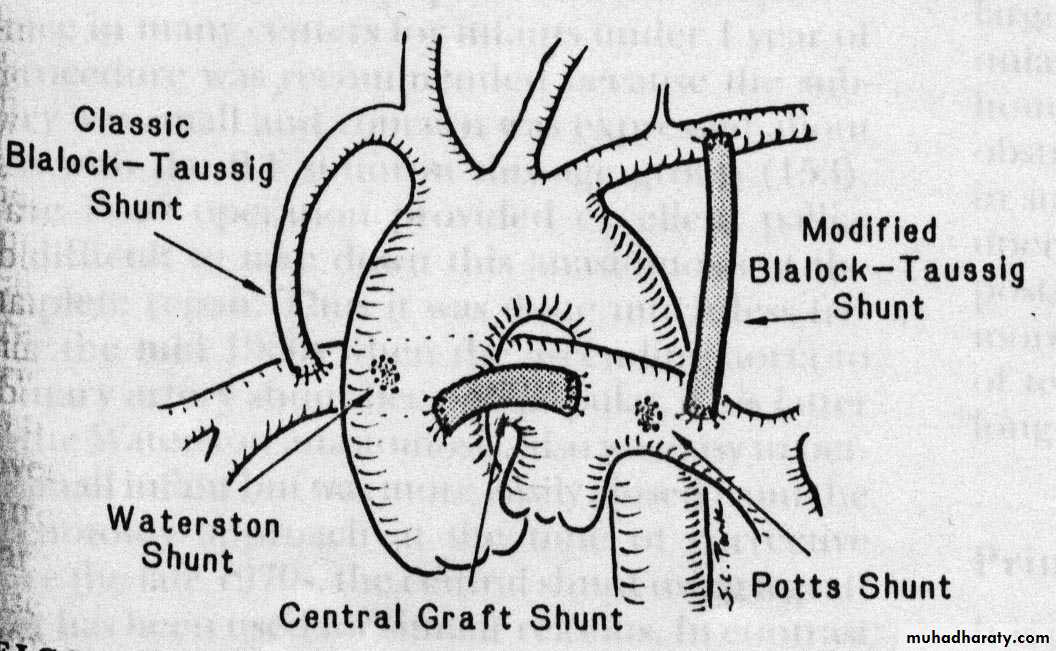
Palliative Surgery
Blalock-Taussig shuntPott procedure
Waterston shunt
Blalock Taussig Shunt
Subclavian artery – Pulmonary artery anastomosis
Modified Blalock Taussig Shunt
Goretex graftSurgical Palliation
Palliative operation prolong life
Increase exercise toleranceDefinitive operation
Closing the VSD
Resecting infundibular
90% can return almost normal life after operation
Complication:
RBBBResidual VSD
Residual Pulmonary stenosis
Pulmonary regurgitation (pulmonary valve excised)
Risk 5%
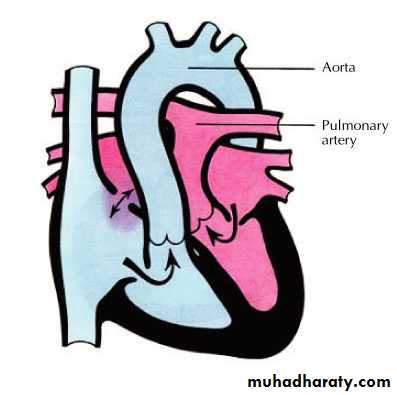
Transposition of Great Areries (TGA)
Aorta originating from the right ventricle, and pulmonary artery originating from the left ventricleAccounts for 5-7% of all congenital heart disease
TGA
Survival is dependent on the presence of mixing between the pulmonary and systemic circulation
Atrial septal defect is essential for survival
50% of patients have a VSD
Usually presents in the first day of life with profound cyanosis
More common in boys
TGA
• Exam :
• cyanosis in an otherwise healthy looking baby• Loud S2 ( aorta is anterior )
• CXR :
• Egg on side
• Narrow mediastinum
TGA .. Acute Management
PGE-1 with no supplemental O2Maintain ductus arteriosus patency, this will increase the effective pulmonary blood flow, and thence increase the left atrial pressure, therefore inhance the left to right shunt at the atrial level
Balloon atrial septostomy
Life saving procedure in the presence of inadequate atrial septal defect
TGA .. Surgical Management
Arterial switchwith re-implantation of the coronary artery to the new aortic site.
Atrial switch :
the old style surgery
Redirecting the pulmonary and systemic venous return to result in a physiologically normal state
The right ventricle remains the systemic ventricle
Rarely needed
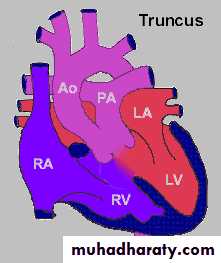
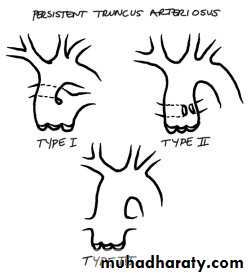
Truncus Arteriosus
The presence of a common trunk that supply the systemic, pulmonary and coronary circulation
Almost always associated with VSD
1.2-2.5% of all congenital heart disease
Truncus Arteriosus
There are different anatomical tupes of truncus arteriosusThis is relevant for surgical repair
Truncus Arteriosus
Generally patients have increased pulmonary blood flowDegree of cyanosis is mild and may not be evident clinically until late stage with pulmonary vascular disease
Presenting feature is congestive heart failure (tachypnia, hepatomegally)
Truncus Arteriosus
Exam is significant forSingle S2
Ejection click of the abnormal truncal valve
Systolic murmur of truncal valve stenosis if present
Diaastolic murmur of truncal valve insufficiency
Gallop
CXR : Cardiomegally , increased pulmonary circulation
Managment
Acute management
No O2 to minimize pulmonary blood flow
Diuretics
Afterload reduction to inhance systemic blood flow
Surgical management: complete repair with VSD closure and conduit placement between the right ventricle and pulmonary arteries
Long term problems :
truncal valve dysfunction
RV conduit obstruction
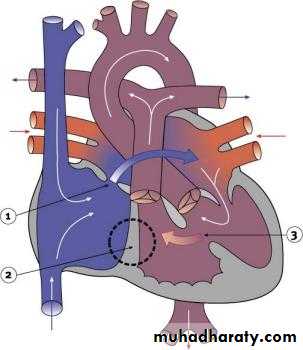
Trcuspid Atresia
Complete absence of communication between the right atrium and right ventricleAbout 3 % of congenital heart disease
Tricuspid Atresia
There is an obligate interatrial communicationUsually associated with VSD
The pulmonary blood flow is dependent on the size of the VSD
Pulmonary blood flow can be increased or decreased causing variable presenting symptoms
If there is no VSD ( also called Hypoplastic right ventricle) the pulmonary blood flow is dependent on the PDA
Tricuspid Atresia- presentation
The presentation will depend on the amount of pulmonary blood flow
If the PBF is decreased, the main presenting symptom is cyanosis
If the PBF is increased the presentation is that of congestive heart failure
CXR will also reflect the amount of pulmonary blood flow
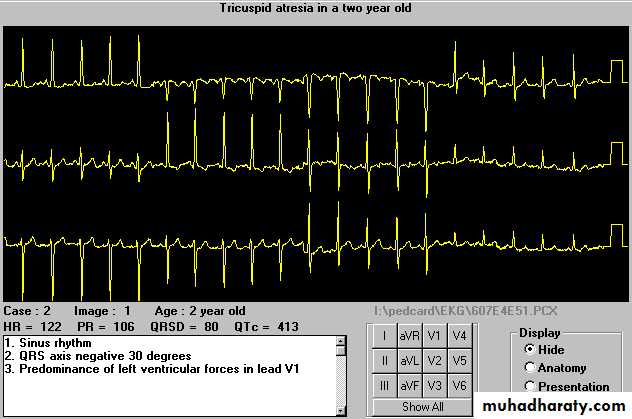
Tricuspid Atresia- EKG
Very characterestic : Left axis deviation
ManagementPBF
Decreased
Increased
PGE-1, and minimal supplemental O2 to maintain ductal patency
No O2
Afterload reduction
Diuretics
Surgical Management
Single ventricle paliationFirst stage : to establish a reliable source of PBF
Aorta to pulmonary artery shunt ( BT shunt)
Pulmonary arterial banding in cases of increased PBF
Second stage: Glenn Anastomosis ( superior vena cava to pulmonary artery
Third stage : Fontan anastomosis ( Inferior vena cava to pulmonary artery