
1
L4
Testicular tumors are divided into five general categories:
1. Germ cell tumors (95%) arising from the germinal epithelium of the seminiferous
tubules;
2. Sex cord-stromal tumors;
3. Mixed germ cell-sex cord-stromal tumors; primary
4. Tumors not specific to the testis; and
5. Metastatic tumors
Testicular tumors:
Is the most common cause of firm painless enlargement of the testis.
The causes remain unknown but:
1. Cryptorchidism is associated with increase in the risk of cancer (5-10% associated
with cryptorchidism).
2. Testicular feminization and Klinefelter also increase the risk.
3. The risk is increase in siblings of patients with testicular cancer.
4. The development of cancer in one testis is associated with marked increase risk of
neoplasia in the contralateral testis.
5. Testicular tumors are more common in white peoples than the blacks.
Testicular tumors divided into two major histogenetic groups:-
Germ cell tumors, which represent more than 9%
1. Seminoma (the neoplastic primitive germ cells may differentiated along the gonadal
lines).
2. Embryonal carcinoma (the primitive germ cells transform into totipotential cells
which largely remain undifferentiated).
3. Yolk sac tumor (totipotential cells may differentiated into extraembryonic cell lines).
4. Choriocarcinoma (differentiation of pluripotential neoplastic germ cells along
trophoplastic lines)
5. Teratoma (totipotential cells may differentiated along the somatic cell lines)
Male Tumor
2
Gonadal stromal /sex cord tumors.
Leyding cell tumor
Sertoli cell tumor
֎ Germ cell tumor –presentation
֎ Painless testicular swelling
֎ May become painfull or heavy
֎ Symptom of metastases
֎ Hormonal manifestation eg gynaecomastia
Seminoma:
It represents about half of all germ cell tumors. Peak incidence is the fourth decade and
it’s of three variants:-
Classic seminoma:
About 90% of all seminomas. On gross examination, the tumor is solid, gray-white, poorly
demarcated growth that bulges from the cut surface of the testis. The tumor may replace
the entire testis in more than half of the cases. Histologically: solid nest of proliferating
tumor cells in between there is randomly scattered thin fibrovascular trabeculea. The
tumor cells have well defined borders with clear cytoplasm. The nuclei show limited
pleomorphism and coarse granular chromatine. Typically there is lymphocytic infiltration
is present in the fibrovascular trabeculea. Radiotherapy results in 5- years’ survival in 85-
90%.
Spermatocytic seminoma:
About 5% of all seminomas. It arises in older patients (more than 50 years). On gross
examination the size of the tumor is variable may reach 15 cm. the tumor is poorly
demarcated soft yellow gray, gelatinous with small cystic areas. Histologically:- the tumor
is composed of three population of neoplastic cells
1. small cells,
2. intermediate cells which is the most numerous and similar to tumor cells of classic
seminoma,
3. Scattered large cells with clumped coarse chromatin. All these tumor cells show
poor cohesiveness and lack the lymphocytic infiltration which is characteristic for
classic seminomas.
Siminomas may reach a large size and show late metastases by lymphatic to iliac and
paraortic lymph nodes, while the other germ cell tumors show an early metastases even
in the absence of palpable testicular lesion by both lymphatic and hematogenous routs.
Hematogenous metastases are most common to the liver and the lung.
3
Seminoma
Most common type
Yong men
Curable
Arises from sperm producing cells
Several histologic types.
Lymphocytes
No markers
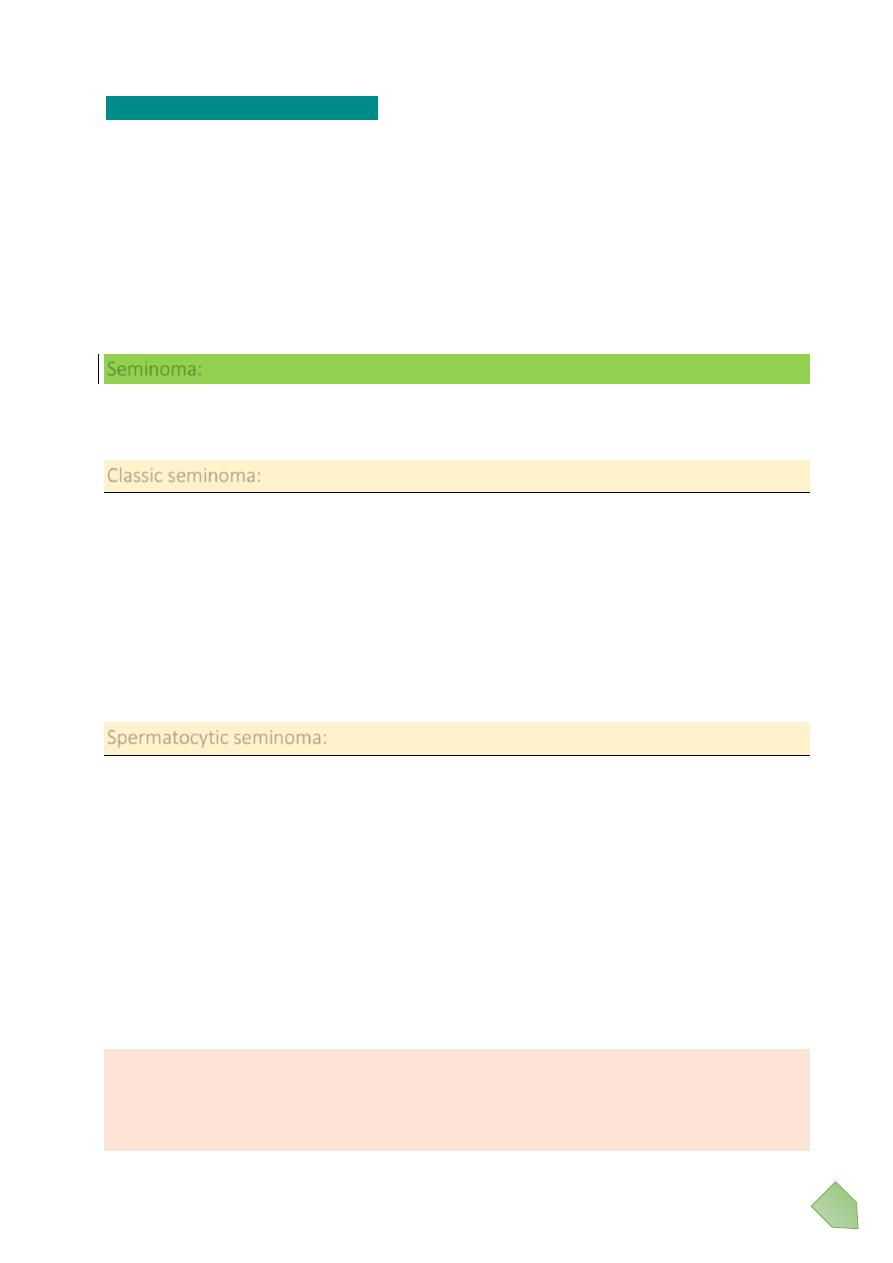
Seminoma testis gross
Histologically: solid nest of proliferating tumor cells in between there is randomly scattered
thin fibrovascular trabeculea. The tumor cells have well defined borders with clear
cytoplasm. The nuclei show limited pleomorphism and coarse granular chromatine.
Typically there is lymphocytic infiltration is present in the fibrovascular trabeculea.
Radiotherapy results in 5- years’ survival in 85-90%.
A small rim of remaining normal
testis appears at the far right.
The tumor is composed of
lobulated soft tan to brown
tissue.
4
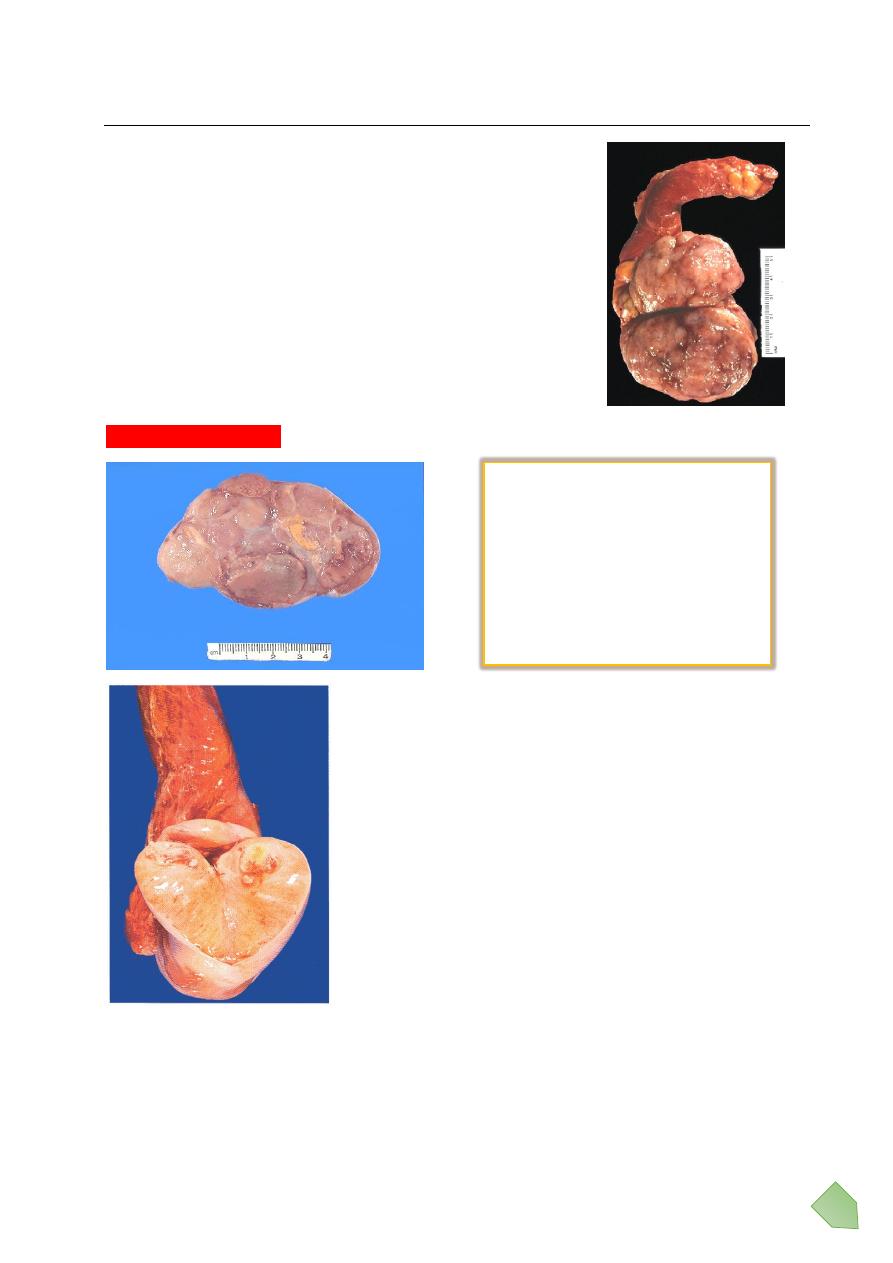
Seminoma
Little fried egg looking cells.
Lymphocytes
No production of Bet-HCG or Alpha-fetoprotein
Seminoma testis mic
Typical seminoma. Lobules of neoplasitic cells have an intervening stroma with
characteristic lymphoid infiltrates. The seminoma cells are large with vesicular nuclei, and
pale watery cytoplasm.
5
Anaplastic seminoma:
About 5% of all seminomas. Has the same gross feature of classic type but histologically
the tumor has more marked nuclear pleomorphism and increased mitoses. This tumor
tends to be at a high stage than the classic seminoma at time of diagnosis.
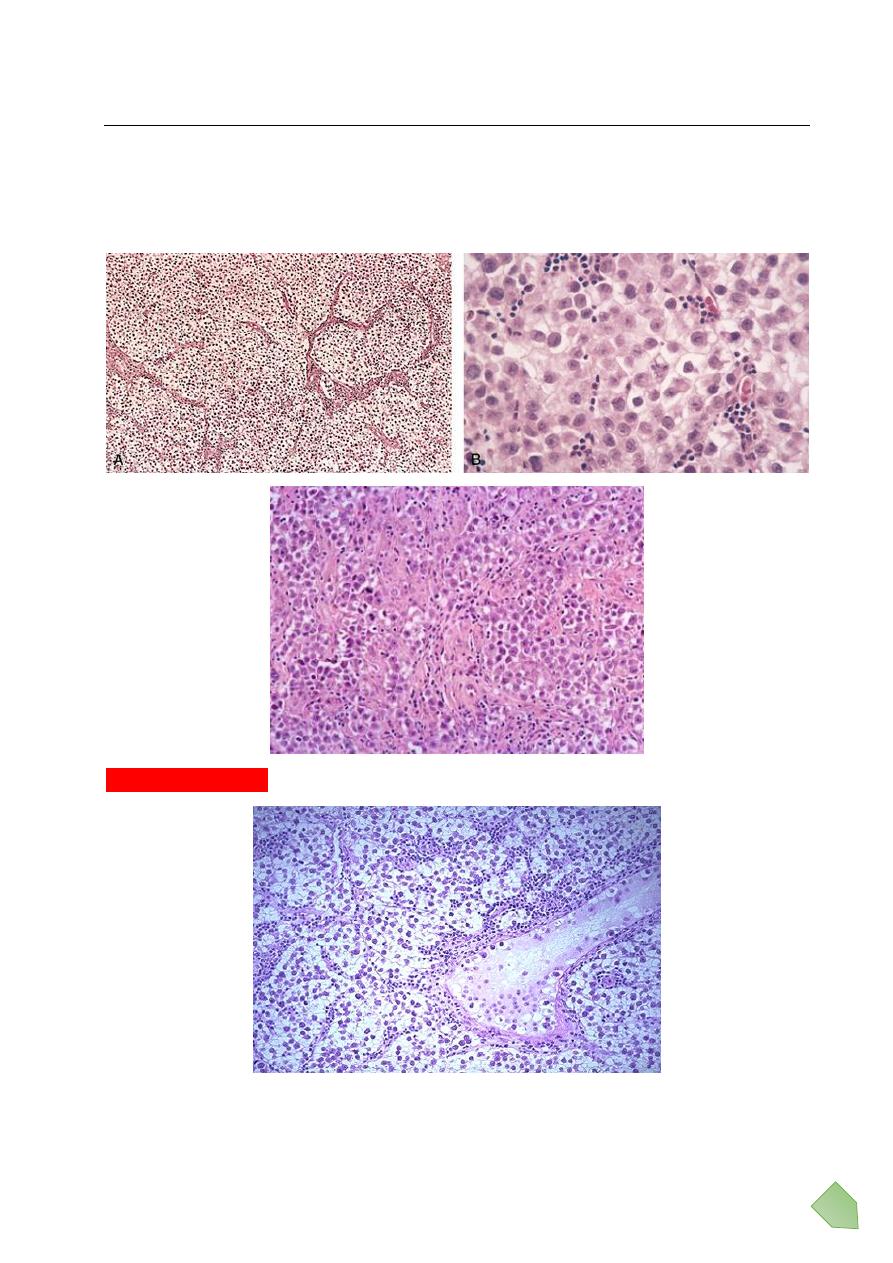
Embryonal carcinoma:
Is the second most common testicular germ cell tumor, account 15-35% of these
neoplasms? It occurs between 20-35 years. Grossly appear as ill-defined invasive masses
containing foci of hemorrhage and necrosis. The primary lesion is small even in-patient
with systemic metastases.
Histologically the tumor cells are large and primitive with basophilic cytoplasm, ill-defined
borders, and large nuclei with prominent nucleoli. The neoplastic cells may arrange in solid
sheet, glandular structures or irregular papillae. In most cases neoplastic cells of yolk sac
carcinoma, teratoma, choriocarcinoma mixed with embryonal areas. Chemotherapy
results in cure rate of 95%-98%.
Embryonal Carcinoma
Aggressive tumor
20-35 years
Areas of hemorrhage and necrosis
Two histologically distinct cell types.
Markers +/-
6
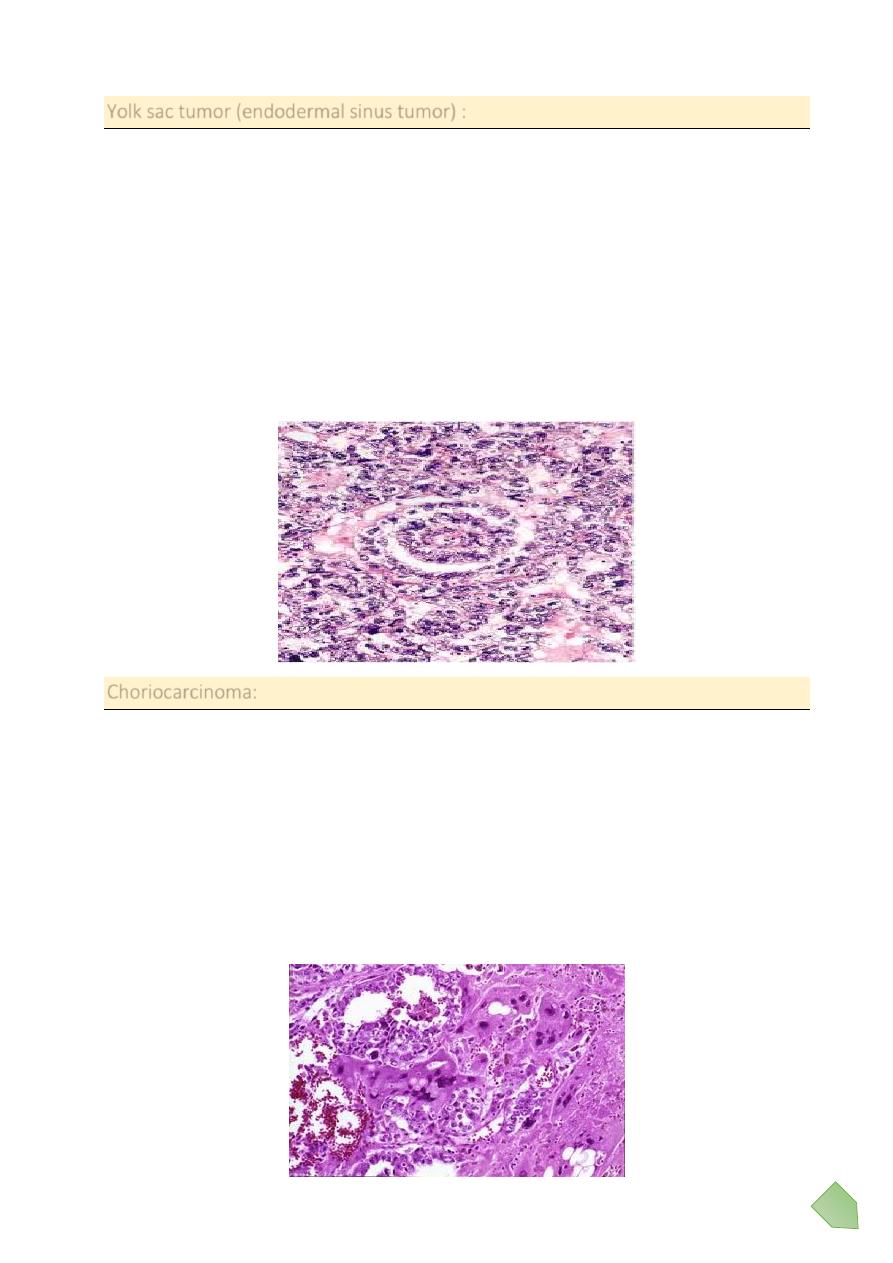
Yolk sac tumor (endodermal sinus tumor) :
Most common primary testicular neoplasm in children younger than 3 years of age, but in
adult this tumor are mostly seen admix with embryonic carcinoma. Grossly this tumor is
typically large and well demarcated.
Histologically:
Show cuboidal or columnar epithelial cells forming sheets, glands, papillae and microcysts
associated with eosinophilic hyaline globules and forming a characteristic feature is the
forming of a primitive structure similar to the glomeruli (Schiller-Duvall bodies.)
By immunohistochemical techniques α- fetoprotein can be demonstrated in the cytoplasm
of the neoplastic cells.
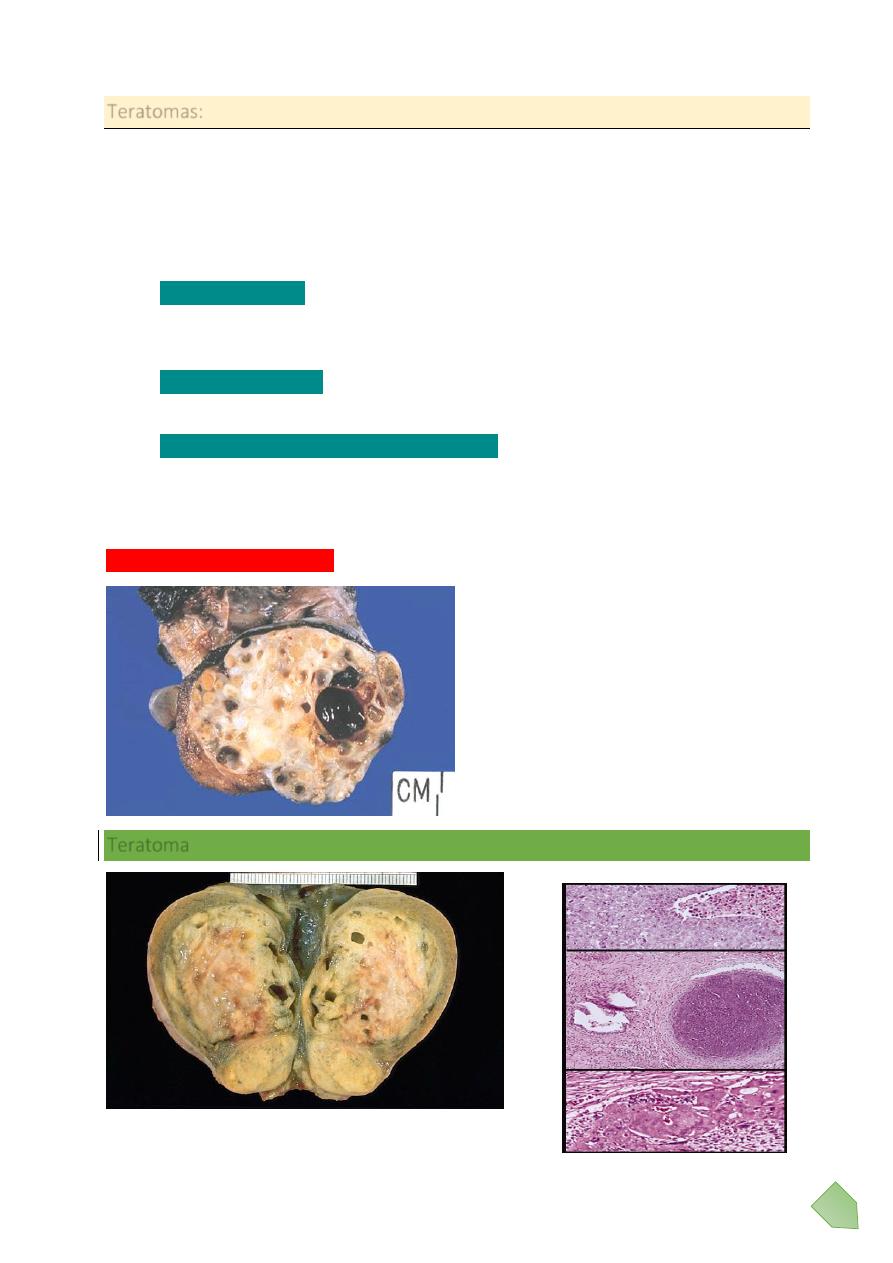
Choriocarcinoma:
Grossly the tumors are very small, nonpalpable lesion even with extensive systemic
metastases.
Histologically:
The tumor is composed of sheets of small cuboidal cells irregularly intermingled with or
capped by large eosinophilic syncytial cells containing multiple dark, pleomorphic nuclei;
these represent cytotrophoblast &syncytiotrophoblastic differentiation respectively. Well-
formed placental villi are not seen. HCG can be identified by immunohistochemical
techniques in the cytoplasm of the syncytiotrophoblastic elements.
7
Teratomas:
Grossly firm masses on cut section show multiple cysts with recognizable areas of cartilage,
bone, hair…
Histologically:
Three variant of pure teratoma can recognize:
Mature teratomas
: contain fully differentiated tissues from one or more germ cell
layers (e.g. cartilage, neural tissue, adipose tissue, bone, and epithelium) in a
haphazard array.
Immature teratomas
: in contrast, contain immature somatic elements resemble to
those in developing fetal tissue.
Teratomas with malignant transformation
: characterized by developing of frank
malignancy in preexisting teratomatous elements such squamous cell carcinoma or
adenocarcinoma. Most cases of malignant transformation occur in adult patients
while pure teratomas in prepubertal male are usually benign.
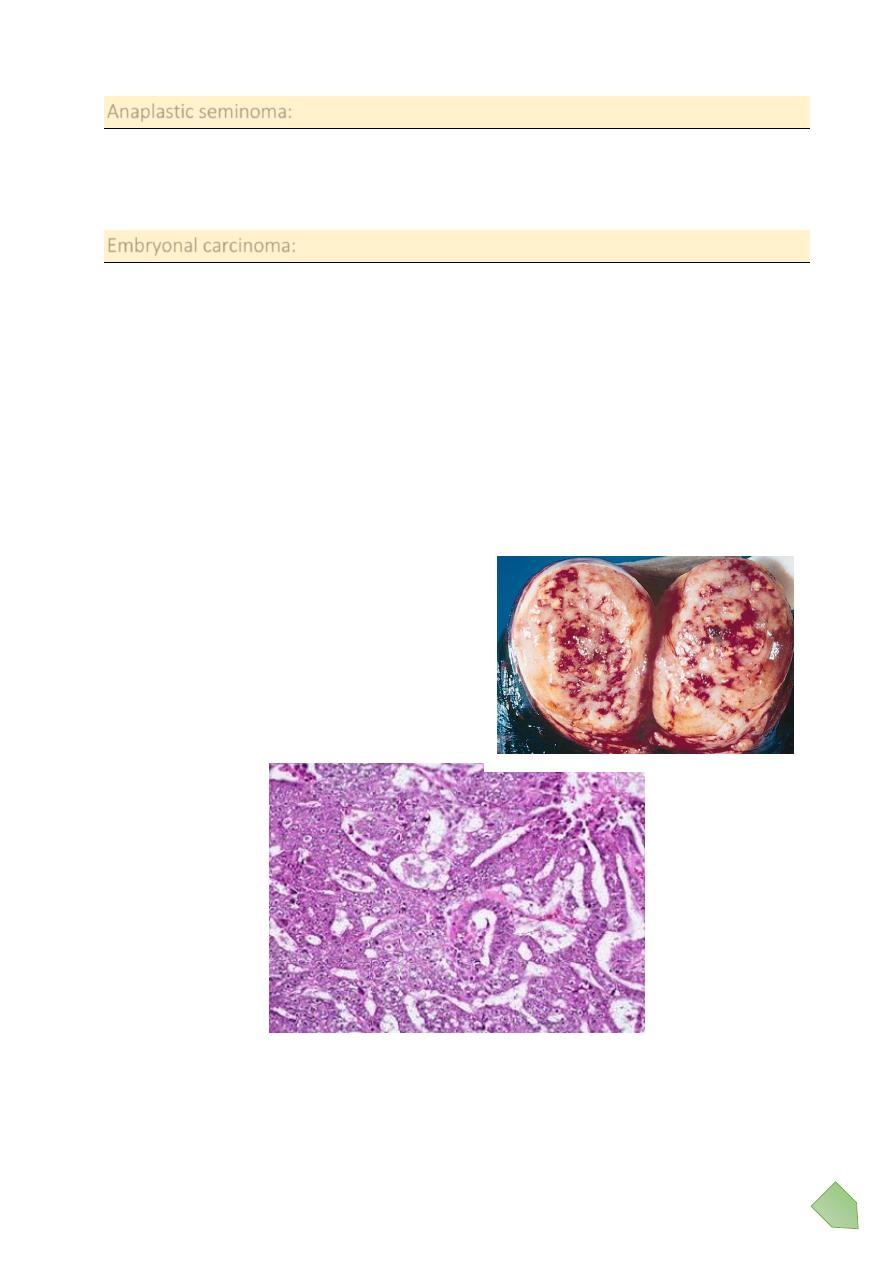
Mature teratoma testis gross
Teratoma
There are multiple cystic
areas, lobules of mature
adipose tissue, and shiny solid
nodules corresponding to
well-differentiated cartilage.
8
Aggressively malignant
Three germ lines
o Ectoderm
o Endoderm
o Mesoderm
Makers +/-
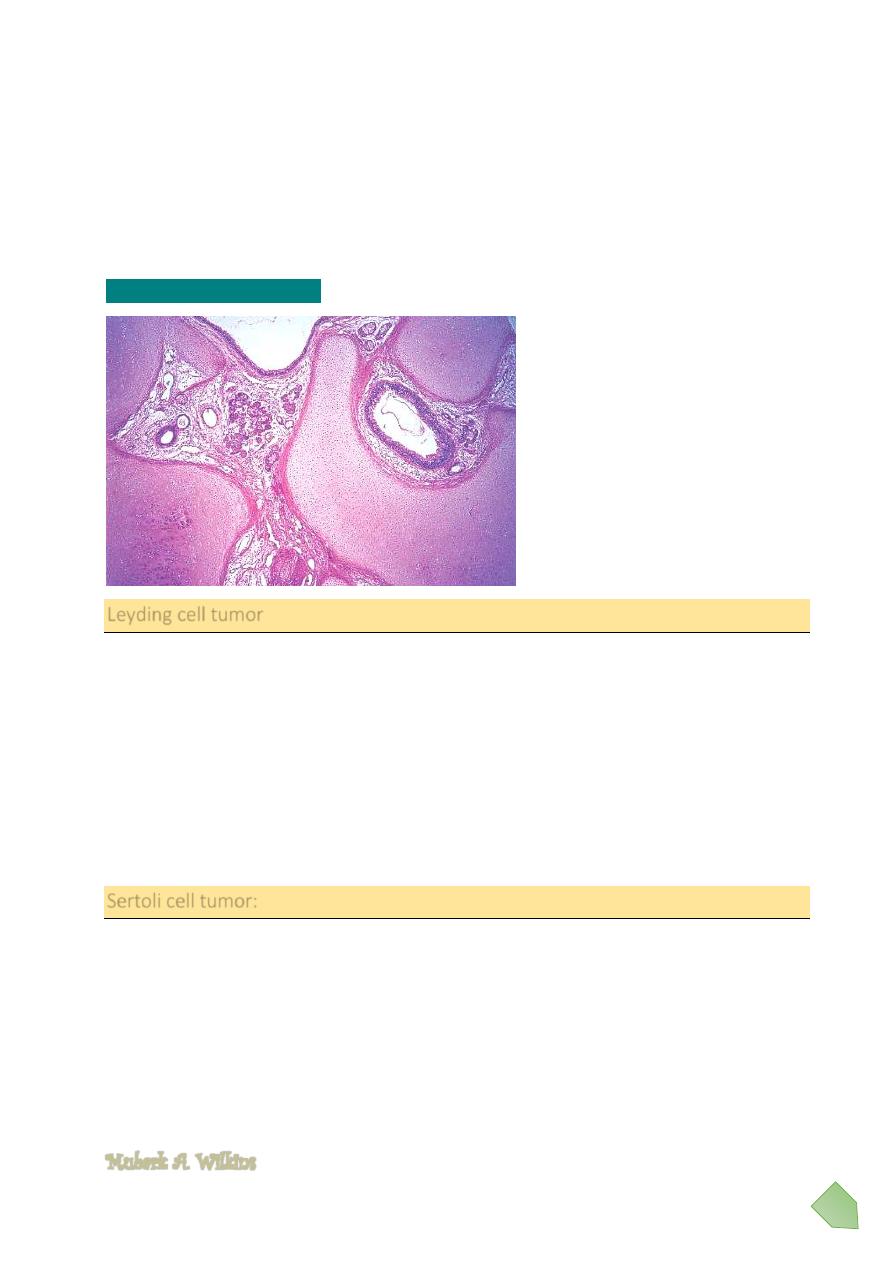
Mature teratoma testis mic
Leyding cell tumor
Rare neoplasm arises from interstitial leyding cells of the testis. This tumor is very
interesting because they are functionally active secreting either testosterone or estrogen
or both of them.
It occurs in two age groups: boys older than 4 years and men in their 3th – 6
th
decades.
Although some boys develope precocious physical and sexual development ,, feminization
with gynecomastia may observed in adult but still there is no characteristic clinical pattern
of this tumor it’s depend on the its endocrinal activity.
Leyding cell tumors are cured by orchiectomy.
Sertoli cell tumor:
Less frequent than leyding cell tumor. 20% of sertoli cell tumors are malignant.
Orchiectomy is curative.
Mubark A. Wilkins
Large islands of cartilage are
seen surrounding well-
differentiated glandular
structures.
