
PROTOZOAL DISEASES
1. In the blood
Malaria
Trypanosomiasis
2. In the gut
Amoebiasis
Giardiasis
3. In the tissues
Toxoplasmosis
Leishmaniasis
AMOEBIASIS
It is caused by Entamoeba Histolytica which spread between humans by its cysts.
PATHOGENESIS
Cysts of E. Histolytica are ingested in contaminated water and food.
In the colon, vegetative trophozoite emerge from the cysts where they may invade
the mucous membrane producing flask shaped ulcers.
Localized granuloma (( AMOEBOMA)) is a rare complication
amoebic ulcers may cause severe hemorrhage but rarely perforate the bowels.
CLINICAL FEATURES
Incubation period from 2 weeks to many years
Abdominal pain
Diarrhea with mucous and blood & offensive odoure
Tenderness over the line of the colon
Diarrhea alternating with constipation is common
DIAGNOSIS
Clinical
GSE: motile trophozoites containing RBCs
Sigmoidoscopy: typical flask shaped ulcers,
In endemic area one third of the population are symptomless (( cyst passer ))
TREATMENT
Oral metronidizole 800 mg/8hr. for 5 days. OR
Tinidazle 2 gm / day for 3 days
Diloxanide furoate 500 mg /8 hr. for 10 days to eliminate luminal cysts.
Amoebic Liver Abscess:
50% has no history of recent diarrhea
Trophozoites may enter the portal venous radicale and carried to the liver causing
an amoebic abscess.
The liquid content at first pinkish colure which may later change to chocolate
brown colure.
Usually single and mainly in the right lobe.
Asymptomatic, local discomfort, malaise, later swinging temperature and
sweating but the patient not toxic.
Enlarged tender liver, cough, right shoulder

Large abscess may penetrate the diaphragm and rupture into the lung or to the
pleural cavity, peritoneal cavity or rarely to the pericardial sac.
DIAGNOSIS:
Clinical
High WBC count ( predominantly neutophilia )
CXR shows elevated right dome of diaphragm
Abdominal ultrasound
Aspirated pus shows characteristic appearance and rarely amoeba
Antibodies detected by IFAT in 95% of the cases.
TREATMENT:
Early:
metronidazole 800mg / 8hr. for 5 days or
tinidazole 2 gm / day for 3 days.
If the abscess is large or threaten to burst or if
not responding to medical therapy, aspiration is
required
Rupture to the pleura, peritoneal cavity or
pericardial sac necessitates immediate aspiration
or surgical drainage.
GIARDIASIS
It is caused by Giardia Lamblia
The cysts remain viable in water for up to 3 months
and infection usually occur by ingestion of
contaminated water.
The flagellate attach to the mucosa of the
duodenum and jejuenum.
CLINICAL FEATURES:
Incubation period 1 – 3 weeks
Diarrhea, abdominal pain, weakness,
anorexia, nausea and vomiting.
O/E there may be abdominal distention and
tenderness
Some patients run in chronic phase with
lethargy, flatulence and loss of weight &
malabsorption.

INVESTIGATIONS:
GSE for the cyst ± flagellate
Duodenal or jejunal fluid exam for the parasite
Jejunal biopsy may shows partial villous atrophy and
may shows Giardia on the surface of the epithelium
TREATMANT;
Single dose of tinidazole 2 gm OR
Metronidazole 2 gm once daily for 3 days OR
Metronidazole 400mg/ 8 hr. for 10 days. OR
Albendazole 400mg / day for 5 days.
MALARIA
It is caused by Plasmodium vivax, P. ovale, P. malariae and
P. falciparum
It is transmitted by the bite of female anopheline
mosquitoes
LIFE CYCLE:
The female anopheline becomes infected when it feed on
human blood containing gametocytes which develop in the
mosquito over 1 – 3 weeks into sporozoites which are
transmitted to another persons via mosquito bites and then
enter the liver to form merozoites which leave the liver and
invade RBC where multiplication occurs forming schizont
which rupture to release more merozoites into the blood
and causes fever.
The periodicity of the fever and rigor depend on the species
of the parasite (( Tertian, Quartian, Aperiodic ))
P. vivax and P. ovale may persist in the liver as dormant.
PATHOGENESIS:
The pathology of Malaria is due to hemolysis of the
infected red cells and there adherence to capillaries.

Anemia may developed and it worse by
spleenomegaly
P. Falciparum cause wide spread organ damage.
CLINLCAL FEATURES:
P. vivax & P. ovale
Continuous fever for several days then classical
boats of fever on alternated days (( cold phase and
rigor for ½ - 1 hour, hot phase with flushing for
several hours and gives a way to profuse sweating
– wet phase- )) the cycle is repeated every 48 hr.
Hepatospleenomegaly
Anemia
Herpes simplex is common
Relapses are frequent in the first two years.
P. Malariae
It is usually associated with mild symptoms
boats of fever every third day
it may cause GN and nephrotic syndrome
P. Falciparum
insidious onset with malaise, headache and vomiting
( Flu – like )
cough and diarrhea are also common
The fever has no particular pattern
Jaundice is common
Hepatospleenomegaly and anemia developed rapidly
Cerebral Malaria is a grave complication manifested
by coma or confusion, no localizing sign and death
Other complication: hypoglycemia, pulmonary
oedema, acute renal failure, severe anemia, metabolic
acidosis, aspiration pneumonia and shock

DIAGNOSIS:
Thick blood film for diagnosis to show the blood stage
of the parasite.
Thin blood film to identify the species of the parasite.
TREATMENT:
P. vivax, P. ovale and P. malaiae:
Chloroquine 600 mg fallowed by 300 mg in 6 hours then
150 mg 12 hourly for 2 more days.
In P. vivax and P. ovale, radical cure and prevention of
relapses can be achieved with primaquine 15 mg daily
for 14 days to destroy the hypnozoite phase in the liver.
P . falciparum:
Because of chloroquine resistance, Quinine is the drug of
choice given 600 mg /8 hr. for 5 days fallowed by single
dose of (( sulfadoxine 1.5 gm with pyrimethamin 75 mg
)) 3 tab. Of fansidar.
In pregnancy, 7days course of quinine should be given
alone
In quinine resistant area, Malarone , 4 tab. Once daily for
3 days
Severe malaria is a medical emergency and cerebral
malaria is the most common cause of death in malaria.
Quinine should be given i.v until the patient can take
orally, active treatment of complication with fluid and
electrolyte correction.
Steroid has no role in treatment.
PREVENTION:
1. Avoiding mosquito bites:
Long sleeves and trousers should be worn
Use of mosquito nets

Repellent creams and sprays
Impregnation of bed nets with ppermethrin
2. Chemoprophylaxis:
Chloroquine sensitive area:
Chloroquine 2 tab./ week & proguanil 1 tab.
/day.
Moderate Chloroquine resistant arteas:
Chloroquine 2 tab./ week & proguanil 2 tab.
/day.
High chloroquine resistant areas:
Mefloquine I tab. Weekly or
Doxycycline 100 mg daily or
malarone 1 tab. Daily
3. Vaccination: still under trial.
AFRICAN TRYPANOSOMIASIS
SLEEPING SICKNESS
It is caused by trypanosomes conveyed to
human by bites of infected tsetse flies.
Two types of trypansomes affect human in
Africa:
1. T. Brucei Gambianse: mainly at the riverside
where the fly rests in the shade of trees and
no animal reservoirs have been identified.
2. T. Brucei Rhodesiense: it has a large
reservoir in numerous wild animals.
CLINICAL FEATURES:
A bite by the fly is painful and
commonly inflamed and it again
become painful and swollen about 10

days later (( Trypansomal chancre )) and
the regional lymph node enlarge ((
Winterbottom᾿s sign))
2 – 3 weeks later, it will invade the
blood stream
The disease characterized by early
heamatolympatic stage and late
encephalitic stage.
RHODESIENSE INFECTION:
The disease is more acute and severe
and usually the patient is severely ill
May developed pleural effusion,
myocarditis or hepatitis.
The patient may die before CNS
involvement.
GAMBIANSE INFECTION
Slow course over months or years with irregular boats
of fever and enlarged lymph nodes mainly in the
posterior triangle.
The spleen and the liver may become palpable
CNS involvement after few months, headache,
change in behavior, insomnia by night and sleepiness
at day, confusion, coma and death.
INVESTIGATIONS:
1. thin and thick blood film to demonstrate
Trypanosome
2. puncture of the primary lesion and lymph node to
demonstrate Trypanosome
3. serology by simple rapid card agglutination
trypanosomal test (( CATT )).

4. if CNS is affected, CSF will shows ↑ cells and protein
and ↓ glucose.
TREATMENT
early treatment carry good prognosis
for T. Rhodesiense: Suramin
for T. Gambiense: Pentamidine
for CNS involvement in both: Melarsoprol
AMERICAN TRYPANSOMIASIS
(( CHAGAS DISEASE ))
It is caused by T. cruzi transmitted to human from
the faeces of the reduvidd bug
Infected faeces are rubbed in through the
conjunctiva, mucosa of the mouth or nose or skin
abrasion.
CLINICAL FEATURES
Acute phase:
At the site of entrance, red, dusky firm
swelling and enlargement of the regional
lymph nodes
Conjectival lesion cause unilateral firm
reddish swelling of the lid may close the eye ((
Romana᾿s sign ))
In few patients : skin rash, fever,
lymphadenopathy and hepatospleenomegaly
In few patients, acute myocarditis, heart
failure or neurological features.
Chronic phase:
Normal life span, asymptomatic, natural reservoir for
the disease .

After several years, 10 – 30 % develop low grade
myocarditis and damage to the conducting fibers
leading to cardiomyopathy characterized by cardiac
dilatation, arrhythmias, heart block and sudden death.
In 10 % , damage to Auerbach᾿s plexsus result in
dilatation of the alimentary tract mainly the
oesophagus and colon so called (( Mega disease ))
INVESTIGATIONS:
Blood film
Serology
TREATMANT:
Acute and early chronic (( 10 years )) : nifurtimox
Cardiac or GIT : symptomatic, no specific treatment
Mega disease: surgery may be useful.
LEISHMANIASIS:
It comprises several diverse clinical syndromes which
can placed into 3 broad groups
1. Visceral leishmaniasis (( Kala – azar )), caused by L.
donovani
2. cutaneous leishmaniasis caused by L. tropica and L.
mexicana
3. mucosal leishmaniasis caused by L.brasiliensis
it is zoonotic disease transmitted to human through
phlebtomine sandfly vectors.
LIFE CYCLE:
Flagellar promastgotes are introduced by the feeding
female sandfly and they taken by the human macrophage
where they lose their flagellae and transform into
amastigotes. These will multiply causes lysis of the
microphage and infection of other cells. Sand fly pick up

amastigote when feeding on infected patient or animal.
In the sand fly, the parasite transform to flagellar
promastigoites which multiply in the gut.
VISCERAL LEISHMANIASIS:
Kala – azar
It is caused by L. donovani complex
CLINICAL FEATURES:
it is predominantly a disease of childhood.
Malnutrition and HIV infection increase the
susceptibility to the visceral disease.
Incubation period: weeks – months.
At first high fever, rigor and chills then fever
intensity will decrease and may present with double
spike fever and afebrile in between.
Spleenomegaly developed quickly and become
massive as the disease progresses and hepatomegaly
occurs later.
Lymphadenopathy may be seen ( generalized ).
Blackish discoloration of the skin is a feature of
advanced illness and now seen rarely.
Moderate to severe anemia that may lead to
congestive heart failure.
Bleeding tendency from retina, GIT and nose.
Hypoalbuminemia lead to leg edema , ascites and
anasarca.
Immune suppression and secondary infectionare
common and include TB, pneumonia, dysentery,
herpes zoster, chicken pox, otitis media and skin
infection.

Without adequate treatment, most of the patients
with clinical VL are likely to die.
INVESTIGATIONS:
1. Pancytopenia with granulocytopenia and
monocytosis
2. Hypergammaglobulinemia chiefly IgG.
3. Hypoalbuminemia
DIAGNOSIS:
1. Demonstration of amastigotes (( Leishman –
Donovan bodies )) in splenic smear is the most
efficient mean of diagnosis but it carry a risk of
serious hemorrhage.
2. Bone marrow or lymph node smear are more save
but less sensitive.
3. PCR for DNA detection from the peripheral blood.
4. Serodiagnosis by ELISA or IFAT.
5. Direct agglutination test of stained promastigot.
6. Rapid immunochromographic strip test.
DIFFRENTIAL DIAGNOSIS:
1.Malaria
2. Typhoid fever
3. Tuberculosis
4. Schistosomiasis
5. Blood diseases
6. Leukemia
TREATMENT:
1. Antimony compound (( Sb )): pentavalent antimony
– Sodium stibogluconate – is the drug of choice at a
dose of 20 mg / kg/ day given i.m or i.v for 28 – 30
days.

S/ E : arthralgia, myolgia, elevated liver enzymes,
ECG will show T inversion, ST segment elevation,
prolonged QT interval, ventricular ectopi, VT, VF
and death.
2. Amphotericin B: 1mg/kg/day for 15 – 20 days used
in Sb failure or resistance.
S/E: renal,hepatic and cardiac toxicity.
3. Miltifosine: oral drug, 100 mg/ day for 28 days butr
it is teratogenic drug.
RESPONSE TO TREATMENT:
A good response result in abatement of fever,felling of
well being, gradual decrease in splenic size, weight
gain and recovery of the blood count.
Follow up for 6 – 12 months because some will
relapse in form of enlargement of the spleen, return of
fever,weight loss and decline in blood counts.
Re- treatment with Sb or amphotericin B indicated.
HIV – VL Co-infection:
HIV increase the risk of contracting VL 100 –
1000 times.
Atypical presentations are common, GIT
involvement, Ascitis, plwural effusion,
pericardial effusion or oral mucosa involvement.
Diagnosis and treatment are the same but
relapses are common.
POST- KALA – AZAR DERMAL
LEISHMANIASIS (( PKDL ))
After treatment and recovery from VL, some
patients develop dermatological
manifestations seen as macules, papules,
nodules and plaques especially at the area
around the chin
The diagnosis is clinical supported by slit
skin smear to demonstrate the parasite or
serological tests
Treatment is difficult and may prolonged for
2 – 4 months.
PREVENTION:
1. sand flies are extremely sensitive to
insecticides and vector control through
insecticides spray is very important.
2. use of mosquito net treated with insecticide.
3. early diagnosis and treatment of human
infection.
CUTANEOUS LEISHMANIASIS
((oriental sore )) (( Baghdad boil ))
causative agent: L. Tropica major
L. Tropica minor
incubation period: 2 – 3 months
papules which ulcerated later with raised
borders usually at the site of the bite
forming nodule.
Regional lymphadenopathy, pain,
pruritus and secondary infection.
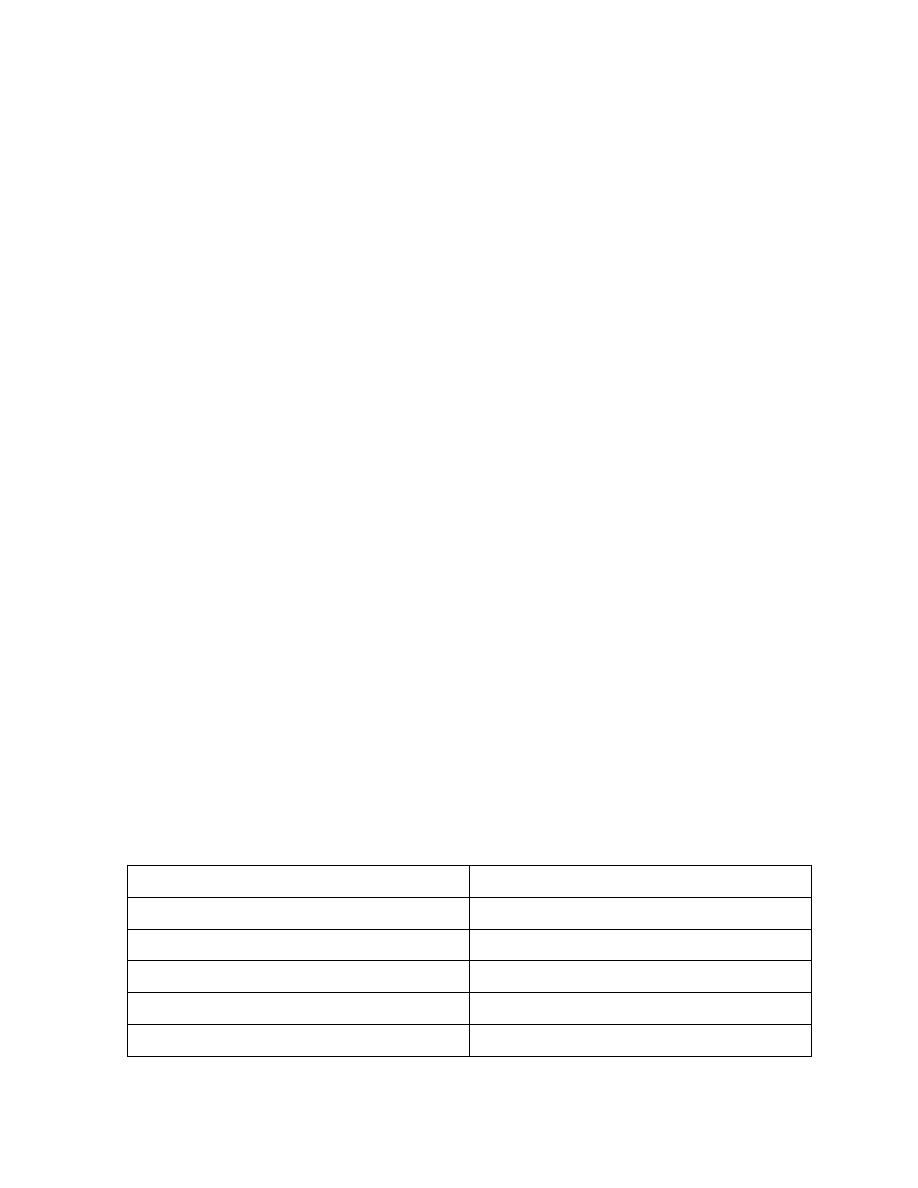
L. tropica
L. major
Usually multiple
Usually single or few
Small size
Large 2 – 10 cm
Slow evolution, less severe
Rapid necrosis
Dry lesion
Wet lesion
No or minimal scars
Heal with scar
No immunity
Give immunity for both
MUCOSAL LEISHMANIASIS:
It is caused by L. brasiliensis complex,
cutaneous lesion may be fallowed by mucosal spread,
metastatic lesions in the mucosa of the nose or mouth
it characterized by thickening and erythema of the
nasal mucosa at the junction of the nose and the upper
lip, later ulceration will developed.
No spontaneous healing and death may result from
severe respiratory tract infection due to massive
destruction of the pharynx
INVESTIGATIONS
For cutaneous and mucosal leishmaniasis:
1. usually the diagnosis made on clinical characteristic of
the lesion
2. Amastigotes can be demonstrated by slit skin smear
stained by Giemsa stain.
3. Leishmanin skin test is +ve except in those with
diffuse CL.
4. PCR is useful in both CL & ML.
TREATMENT of CL & ML
Small cutaneous lesion may heal spontaneously ((
self – heal )) or by
Freezing with liquid nitrogen.
Topical paromomycin and methyl benzathonium
chloride is beneficial in CL.
When the lesions are multiple or at disfiguring
site, treatment with Sb 20mg/kg/day for 20 days.
Interalesional antimony 0.5 ml is rapidly
effective, well tolerated and save.

Fluconazole 200mg/day for 6 weeks reduce the
healing time and cure 80% of CL caused by L.
major.
ML are treated with 28 days systemic Sb or 8
injections of pentamidine on alternated days
regiem.
Refractory CL or ML should be treated with
amphotercin B .
PREVENTION:
Personal protection against sandfly bites
Use of insecticides
No vaccine yet available.
TOXOPLASMOSIS
Causative organism:
Toxoplasma Gondii
Congenital Tox.
From infected mother during pregnancy to her fetus.
Acquired Tox.
From the ingestion of cyst excreted in the faces of
the infected cats or from eating undercooked beef ((
oöcysts and cysts ))
PATHOLOGY:
In congenital form, the parasite widely
spread in the CNS, eyes, heart, lung and
adrenals.
If the infant survive, the parasite disappear
from most organs except the brain (( CNS ))
and retina.

In acquired form, the organism invade the
LN, spleen and less commonly; liver and
myocardium.
CLINICAL FEATURES:
Congenital Toxoplasmosis:
The main features are cerebral with
hydrocephalus, microcephaly,
convulsion, tremor or paralysis.
Microphthalmos, nystagmus and
choroidoretinitis are common.
Hepatomegaly, thrombocytopenia and
purpura may occurs.
Severe forms are usually fatal and if the
child survive, he will be disabled and
blind.
Mild cases presented with only
choroidoretinitis.
Acquired Toxoplasmosis:
Many of them are asymptomatic.
In the acute form:
Fever, cough, myalgia, malaise, maculopapular rash
and rarely jaundice & myocarditis.
In the chronic form:
Generalized lymphadenopathy, particularly cervical
lymph nodes,may be spleenomegaly.
Some pf them may developed encephalitis,
myocarditis, pneumonia, hepatitis and even
choroidoretenitis.
INVESTIGATIONS:

1. in congenital Tox., skull X – ray may shows
calcifications.
2. blood film will shows atypical lymphocytosis.
3. serology
antibodies detected by DYE test.
Rise in Ig M antibody titer indicate acute
infection.
significant levels of Toxoplasma Ig M –
antibody by double sandwich IgM ELISA
and Ig M Immunosorbent agglutination
assay ISAGA.
TREATMENT:
Most of the patients not require treatment.
Sulphadiazine 2gm/day, Pyrimethamin 25mg/day and
folinic acid 15mg/day. For 4 weeks.
In pregnancy with recent infection, Spiramycin
3gm/day until term.
