د بسام ادور/ كلية طب نينوى
1
Endocrine System
Both endocrine & nervous systems provide intercellular communication
which is important for human survival. The endocrine system produces hormones.
Definition of Hormone
Hormone is a substance that synthesized in one organ & transported by the
circulatory system to acts on another tissue. However, this description is too
restrictive because hormones can act on adjacent cells (paracrine action) & on
the cell in which they were synthesized (autocrine action) without entering the
systemic circulation.
Classification of Hormones
Hormones can classified into two main groups:-
1)- Group I: - Includes steroid, retinoid & thyroid hormones. Characterize by
the following:-
1-They are lipophilic.
2- Because they are lipophilic, these hormones after secretion into the blood,
higher concentration of them are transported by plasma carrier proteins as
bound form (inactive) while the remaining little concentration is in the free or
unbound form (active), this protein binding circumvents the problem of
solubility while prolonging the plasma half-life of the hormone (hours to days).
3-Free hormone readily traverses the lipophilic plasma membrane of all cells
& encounters receptors in either the cytosol or nucleus of target cells; therefore
the hormone-receptor complex is directly affecting the genes expression.
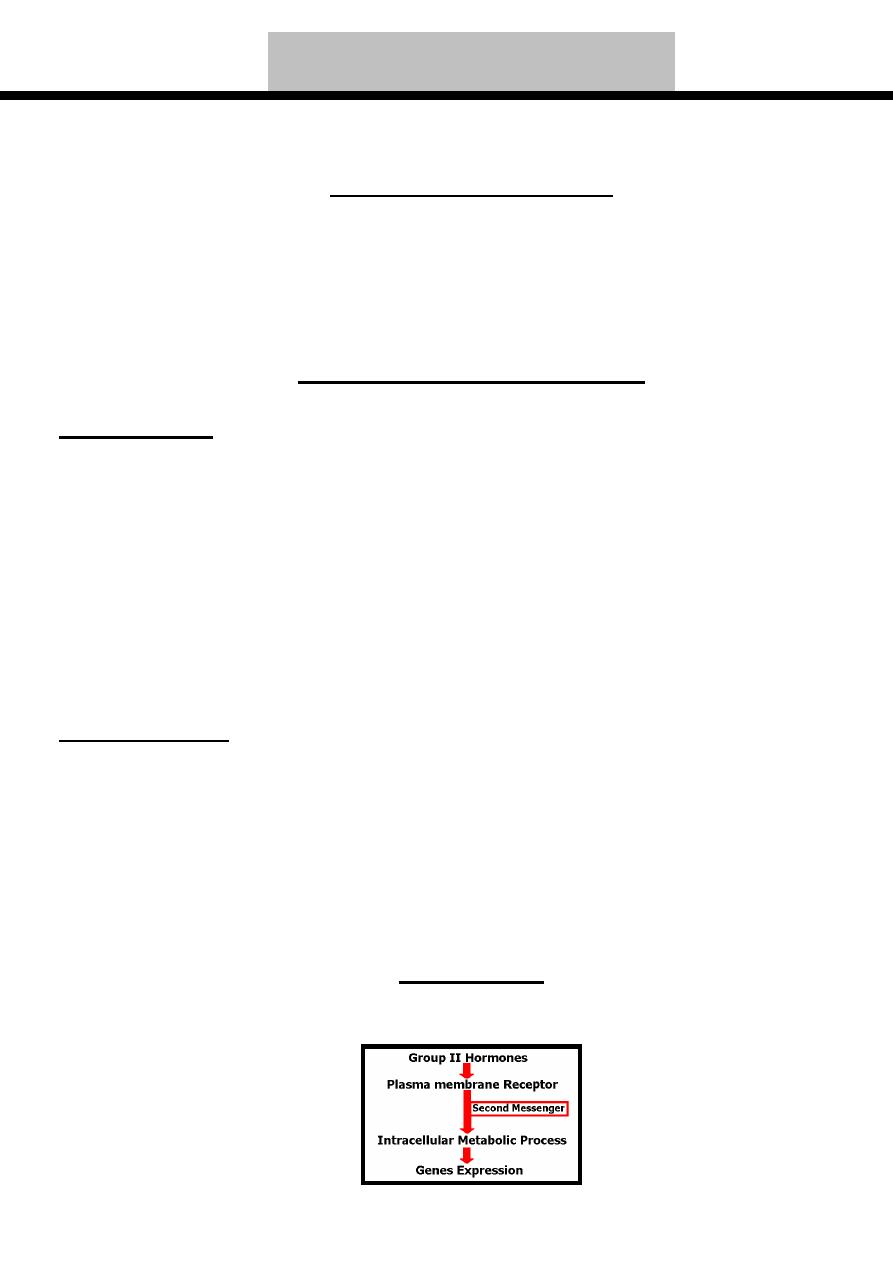
2)- Group II: - Includes polypeptide, protein, glycoprotein & catecholamine
hormones. Characterize by the following:-
1-They are hydrophilic.
2- Because they are hydrophilic, these hormones after secretion into the blood
are not associated with plasma carrier proteins; therefore, they have short
plasma half-life (seconds to minutes).
3- Bind to receptors located in the plasma membrane that affect the genes
expression through the second messengers like cAMP & cGMP.
Target Cell
Target cell include any cell in which the hormone binds to its receptor,
whether or not a biochemical or physiologic response has yet been determined.
د بسام ادور/ كلية طب نينوى
2
Hormones of Adrenal Cortex
Each adrenal gland consist of two separate endocrine organs which are adrenal
medulla (produce catecholamines) & adrenal cortex (produce steroid hormones)
The steroid hormones produced by adrenal cortex are grouped into:-
1-Mineralocorticoids...Produced by zona glomerulosa of adrenal cortex.
2-Glucocorticoids...Produced by zona fasiculata & zona reticularis of adrenal
cortex.
3-Androgens...Produced by zona fasiculata & zona reticularis of adrenal
cortex.
Introduction to Steroid Hormones
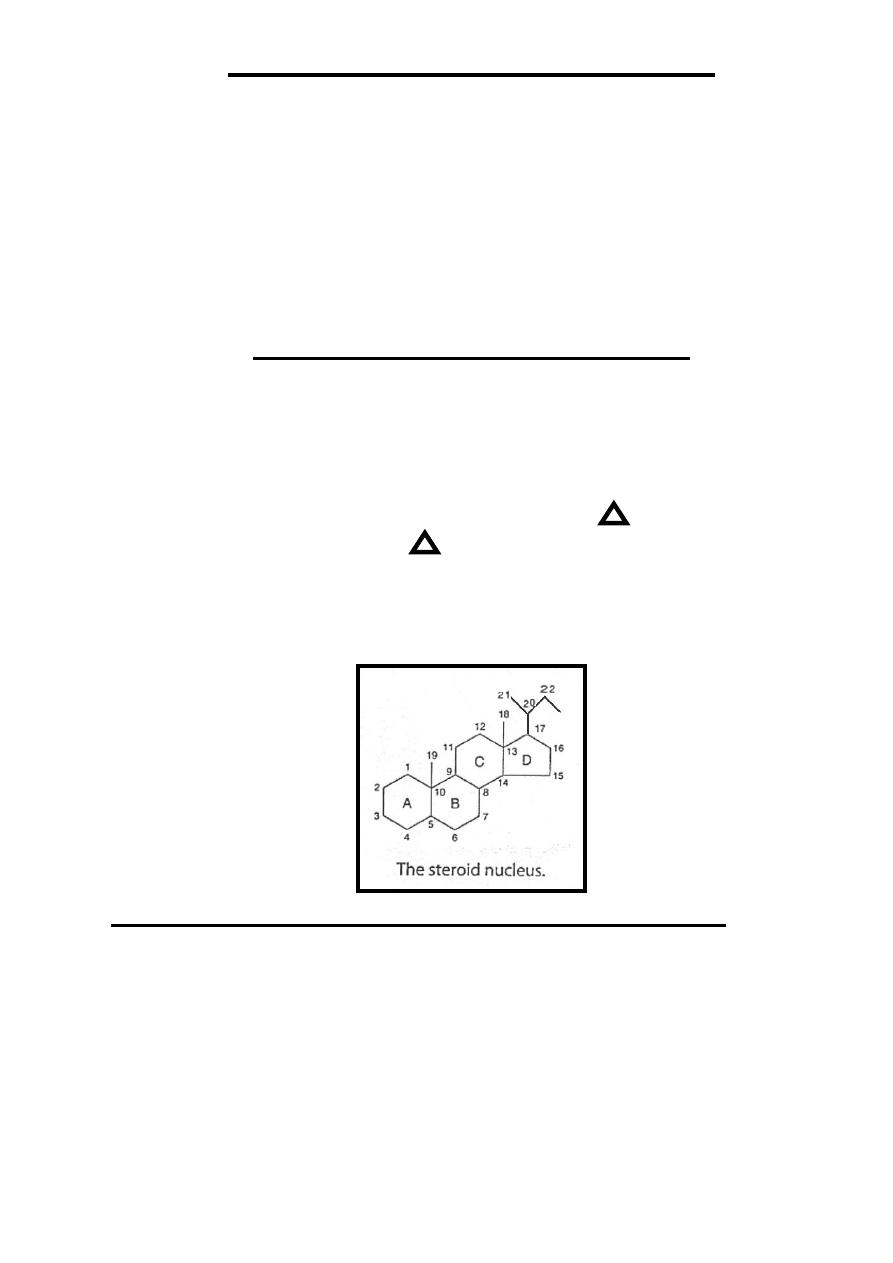
Steroid hormones nucleus are characterize by having four rings ((17- carbon
atoms)) with additional carbon atom at position 13((C
18
)) & at position 10
((C
19
)) & carbon atoms at position 17 ((C
20 ,21
….)).
If the side-chain of steroid hormones above (front) hormone plane it's called β
cis while if it's below (behind) hormone plane its called α trans.
Double-bond in steroid hormones represented by (Delta) with number
of preceding carbon atom (example
5
mean double bond between C
5
& C
6
).
On drawing the structure of steroid, the carbon positions on the steroid
nucleus are numbered. All double bonds shown as such. Methyl side chains
shown as single bonds unattached at the farther (methyl) end. β- bonds are shown
with bold solid lines, whereas α -bonds are indicated with broken lines.
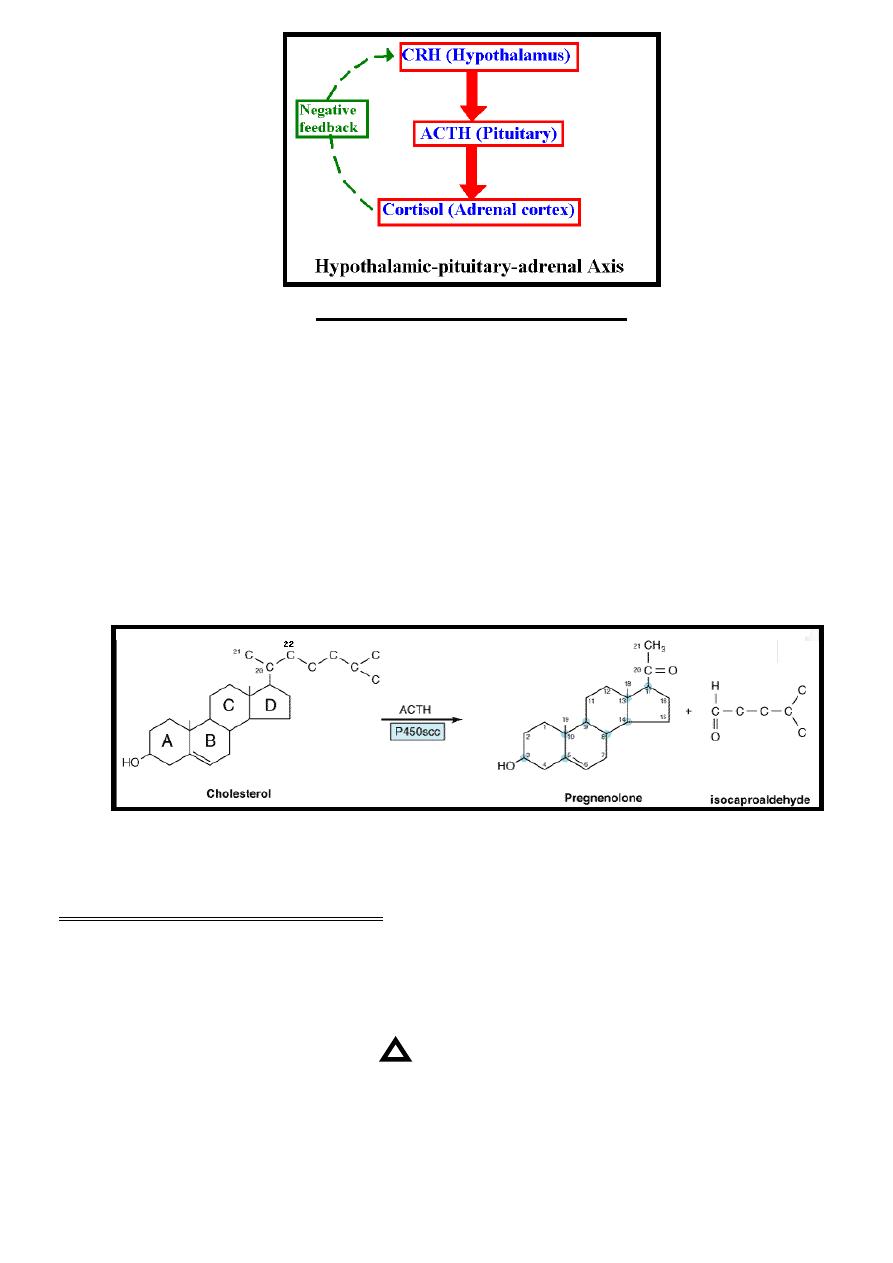
Control of Adrenal Steroid Hormones Secretion
The physiological control of adrenal steroid hormones mainly glucocorticoids
(especially cortisol) occurs through hypothalamic-pituitary-adrenal axis by
production of hypothalamic corticotropin-releasing hormone (CRH) which
stimulate the release of ACTH from the anterior pituitary gland, this ACTH
stimulates the release of adrenal steroid hormones mainly glucocorticoids
(especially cortisol) while mineralocorticoids are stimulated mainly by
angiotensin II & to less extent by ACTH .
Increase free cortisol level cause negative feedback inhibition to this axis
through suppression of CRH mainly.
د بسام ادور/ كلية طب نينوى
3
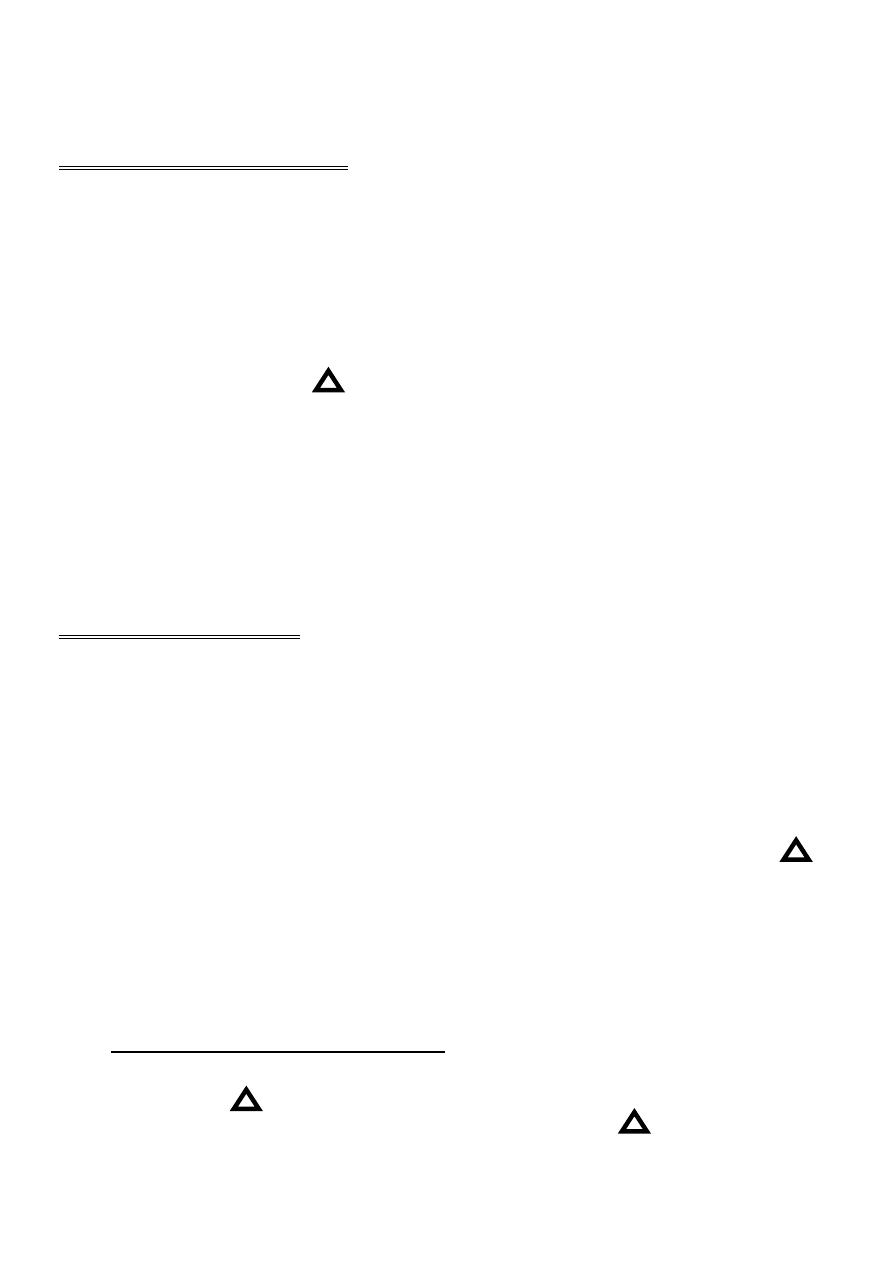
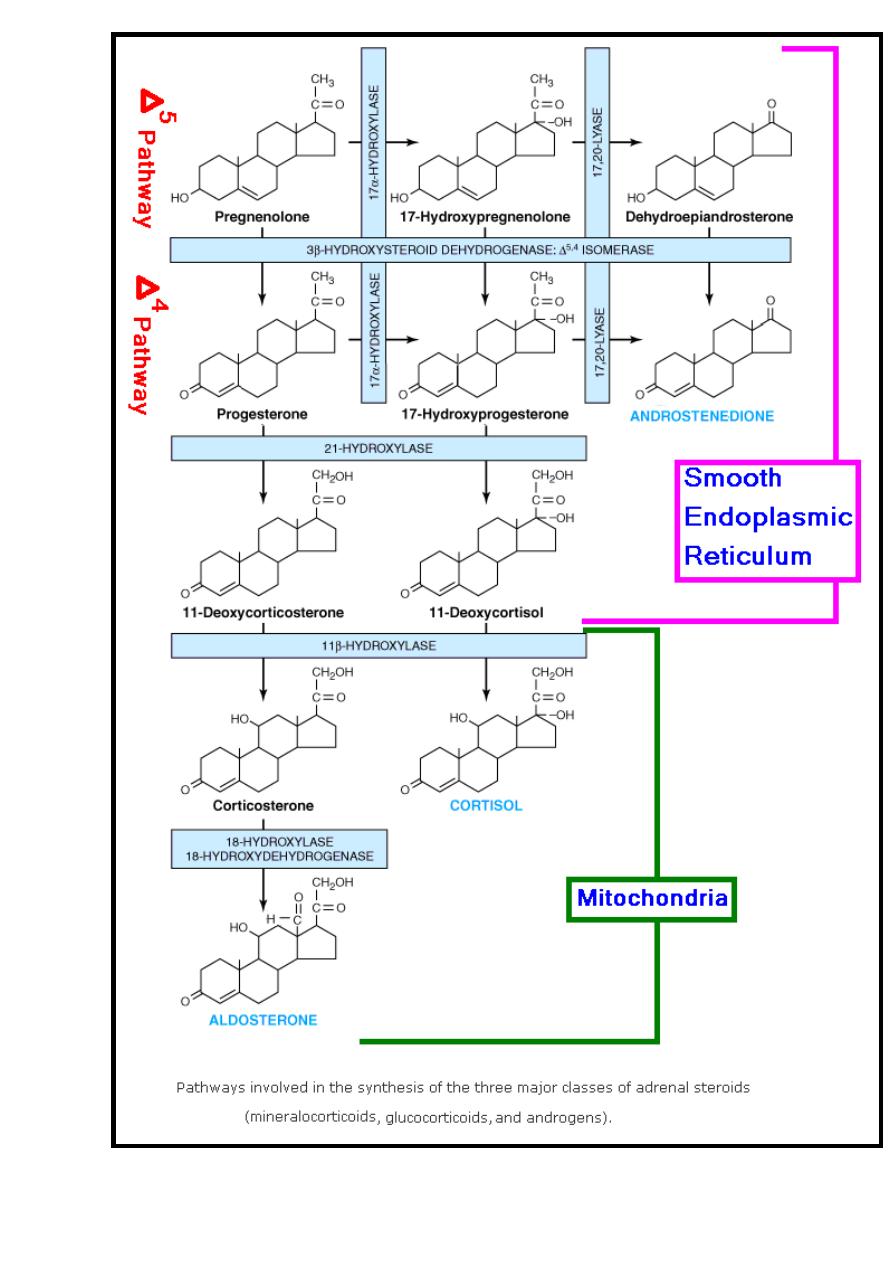
Adrenal Steroidogenesis
The adrenal steroid hormones are synthesized from cholesterol. Much of
cholesterol in the adrenal is esterified & stored in cytoplasmic lipid droplets.
Upon stimulation of the adrenal cortex by ACTH, an esterase enzyme is
activated converting cholesterol ester into the free cholesterol which is
transported into the mitochondria, where a cytochrome P450 side chain
cleavage enzyme (P450scc) converts cholesterol (27-carbons) to pregnenolone
(21-carbons) + isocaproaldehyde (6-carbons), this cleavage occurs between C
22
& C
20
.
An ACTH-dependent steroidogenic acute regulatory (StAR) protein is
essential for the transport of cholesterol to P450scc in the mitochondria, this
step is consider as a rate-limiting step of adrenal steroidogenesis.
Pregnenolone is consider as a common precursor of all steroid hormones,
pregnenolone leaves the mitochondria into the smooth endoplasmic reticulum
where subsequent reactions occur as follow:-
A. Mineralocorticoids synthesis:-This synthesis occurs in zona glomerulosa &
the most potent mineralocorticoides produced is aldosterone, the synthesis
occurs through the following steps:-
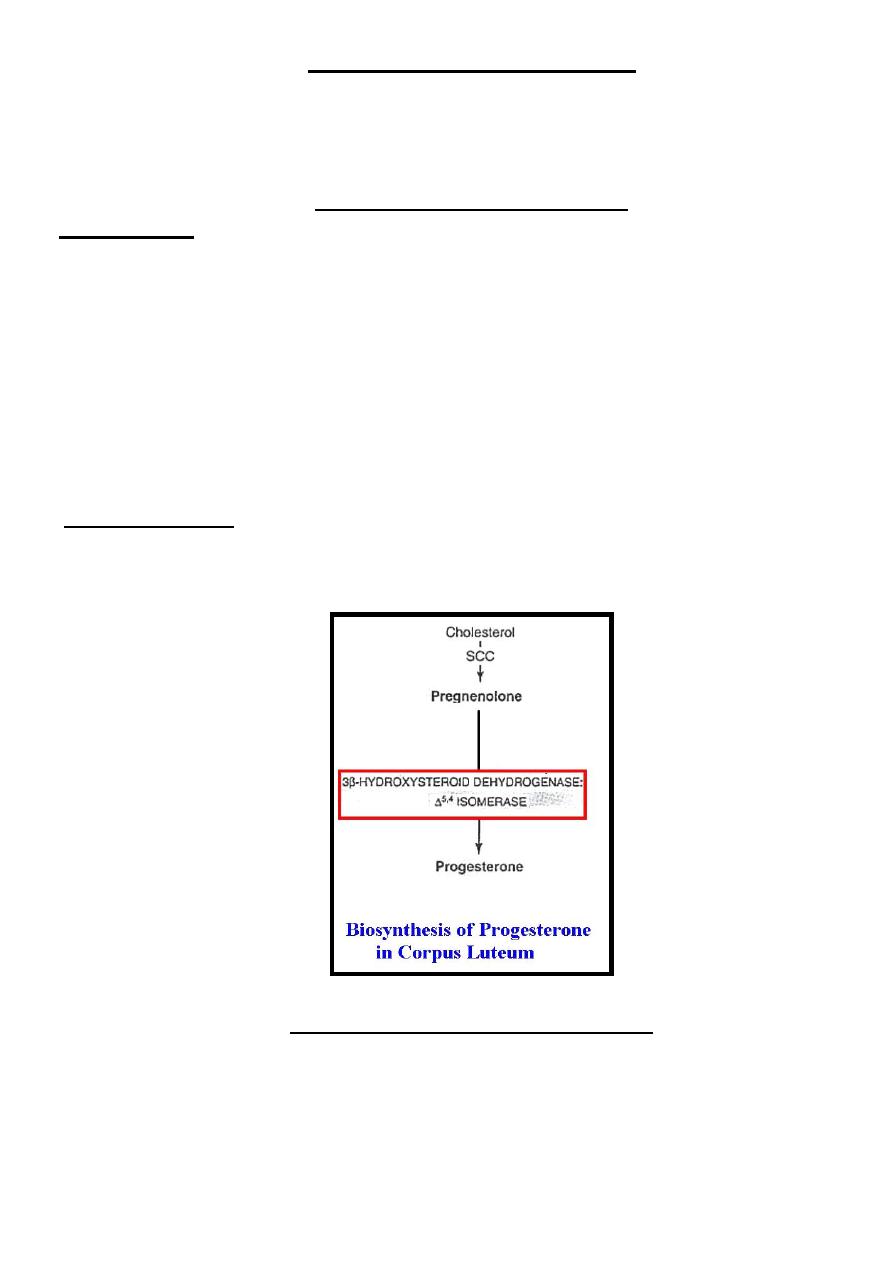
1)- Pregnenolone which present in the smooth endoplasmic reticulum is
converted to progesterone by the action of two enzymes ((3β-hydroxysteroid
dehydrogenase (3 β -OHSD) &(
5
'
4
isomerase).
2)- Progesterone is hydroxylated at C
21
position by the action of 21-
hydroxylase enzyme forming 11-deoxycorticosterone (DOC).
3)- DOC leaves smooth endoplasmic reticulum into the mitochondria where
subjected to another hydroxylation at C
11
by the action of 11 β hydroxylase
د بسام ادور/ كلية طب نينوى
4
enzyme forming corticosterone.
4)- In the zona glomerulosa((not have 17α–hydroxylase enzyme)), there is a
mitochondrial enzyme called 18-hydroxylase (18 hydroxydehydrogenase,
aldosterone synthase) acts on C
18
of corticosterone forming aldosterone.
B. Glucocorticoids synthesis... This synthesis occurs in zona fasiculata & zona
reticularis & the most potent glucocorticoids produced is cortisol.
Cortisol synthesis requires three hydroxylases that act sequentially on the C
I7
,
C
21
& C
11
positions. The synthesis of cortisol occurs through following steps:-
1)- 17α-hydroxylase is a smooth endoplasmic reticulum enzyme located only
in the fasciculata & reticularis zones that acts mainly on pregnenolone
producing
17-
hydroxypregnenolone.
2)- 17-hydroxypregnenolone converted into 17-hydroxyprogesterone by the
action of 3 β-OHSD &
5
'
4
isomerase in addition small amount of 17-
hydroxyprogesterone produced by the action of 17α-hydroxylase on
progesterone.
3)- 17-hydroxyprogesterone is hydroxylated at C
21
forming 11-deoxycortisol by
the action of 21-hydroxylase enzyme which present in smooth endoplasmic
reticulum.
4)- 11-deoxycortisol leaves the smooth endoplasmic reticulum into the
mitochondria where is subjected to another hydroxylation at C
11
by the action of
11 β hydroxylase enzyme forming cortisol.
C. Androgens synthesis…The major androgen produced by the zona fasiculata
& zona reticularis of adrenal cortex is dehydroepiandrosterone (DHEA), the
synthesis of androgens occurs through the following steps.
1)- Most of the 17-hydroxypregnenolone follows the glucocorticoid pathway,
but a small fraction is subjected to oxidative fission & removal of the two-
carbon side chain by the action of 17, 20-lyase enzyme. This enzyme is present
in the smooth endoplasmic reticulum & is important in both the adrenals & the
gonads; the product of this reaction is DHEA.
2)- DHEA is really a prohormone & by the actions of 3 β-OHSD &
5
'
4
isomerase convert the weak androgen (DHEA) into the more potent androgen
called androstenedione (androstene 3,17 dione).
Small amounts of androstenedione are also formed in the adrenal by action of
17,20 lyase on 17-hydroxyprogesterone.
3)- Recently found that small amounts of testosterone (the most potent
androgen) are produced in the adrenal cortex.
Notes on adrenal steroidogenesis
1- The pathway of conversion of pregnenolone into 17-hydroxypregnenolone
& DHEA is called
5
pathway while the pathway of conversion of progesterone
into 17-hydroxyprogesterone & androstenedione is called
4
pathway.
2- All reactions involved in adrenal steroidogenesis are irreversible.
د بسام ادور/ كلية طب نينوى
5
د بسام ادور/ كلية طب نينوى
- 6 -
Function of Glucocorticoids
I-Carbohydrate metabolism... Increase blood glucose by:-
1) - Stimulate gluconeogenesis.
2)-Reduce peripheral utilization of glucose by extrahepatic tissues.
II-Lipid metabolism…
1)-Lipogenic effect on certain places specially the face & trunk.
2)-Lipolytis effect on certain places as extremities.
3)-Elevate FFA (Free Fatty Acid) in blood circulation.
III-Protein metabolism…
1)-Anabolic effect in the liver.
2)-Catabolic effect in the extrahepatic tissues as muscle, bone & skin.
IV-Immune system… reduce immunity & have anti-inflammatory effect.
V-Share in the metabolic response toward trauma.
VI-Minor mineralocorticoid activity.
Function of Mineralocorticoids
The main function of mineralocorticoids (mainly aldosterone) is that it affects
sodium-potassium & sodium-hydrogen ion exchange across all cell membranes.
Transport of Adrenal Steroid Hormones
These hormones are synthesized in the final form & secreted immediately into the
blood circulation (no storage). In the blood circulation:-
*Cortisol is present in two forms:-
1- Unbound (free) cortisol constitutes about 8% of the total plasma cortisol &
represents the biologically active fraction.
2- Bound cortisol represents the biologically inactive & reservoir fraction, the
protein that bind to cortisol is mainly Corticosteroid-binding globulin (CBG) & to
less extent Albumin.
*Aldosterone: It has no specific transport protein but is weakly bind to albumin.
Metabolism of Adrenal Steroid Hormones
It occurs in the liver through two steps:
Step 1:- Reduction of cortisol or aldosterone forming Dihydro or Tetra-hydro cortisol or
aldosterone respectively.
Step 2:- Conjugation of Dihydro or Tetra-hydro cortisol (or aldosterone) at position 3 by
glucuronate or sulphate form Dihydro or Tetra-hydro cortisol (or aldosterone) 3-
glucuronate or sulphate respectively. These metabolites are water soluble so they
excreted through bile duct where majority of them are reabsorbed by enterohepatic
circulation making 70% of them are excreted by urine, 20% by feces & 10% by skin.
د بسام ادور/ كلية طب نينوى
- 7 -
Hormones of Testes
Testes are performing two distinct but closely related functions which are:
1- Production of mature spermatozoa.
2- Testosterone hormone synthesis.
This done by the following types of cells:-
1-Spermatogonia & more differentiated germ cells that present in the seminefrous
tubules under the effect of FSH.
2- Leydig cells which present in the interstitial tissue producing testicular
hormones mainly testosterone under the effect of LH.
3-Sertoli cells which forms the basement membrane lining of seminefrous
tubules providing the media required for germ cells differentiation & maturation
to form mature sperms through the secretion of androgen binding protein (ABP)
under the effect of FSH, this ABP have 100 times affinity to bind testosterone
than other tissues ,therefore, is responsible for sperm maturation.
Therefore, spermatogenesis requires Testosterone, ABP, FSH & LH.
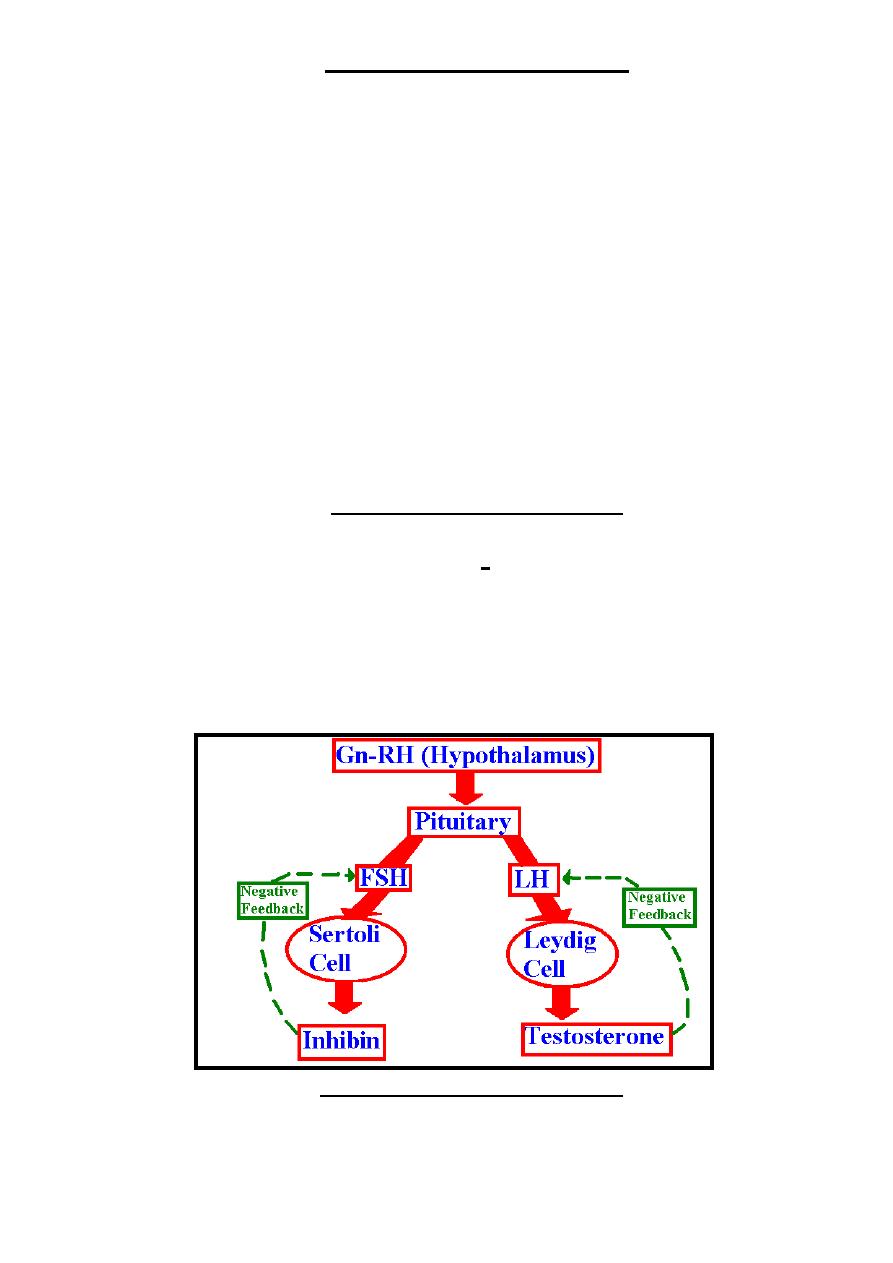
Control of Testicular Function
The physiological control of testicular function occurs through hypothalamic-
pituitary-testicular axis by production of hypothalamic gonadotropin-releasing
hormone (Gn-RH) which stimulate anterior pituitary to produce both FSH & LH.
FSH stimulates differentiation of germ cells & sertoli cells function.
LH stimulates leydig cells to produce testosterone.
Negative feedback inhibition to this axis occurs by:-
1-Increase level of free testosterone causes inhibition to LH secretion.
2-Sertoli cells produce inhibin causes inhibition to FSH secretion.
Testicular Steroidogenesis
Testicular androgens are synthesized by the Leydig cells.
As in adrenal steroidogenesis; the precursor of the testicular steroids is
cholesterol & the rate-limiting step is the delivery of cholesterol to
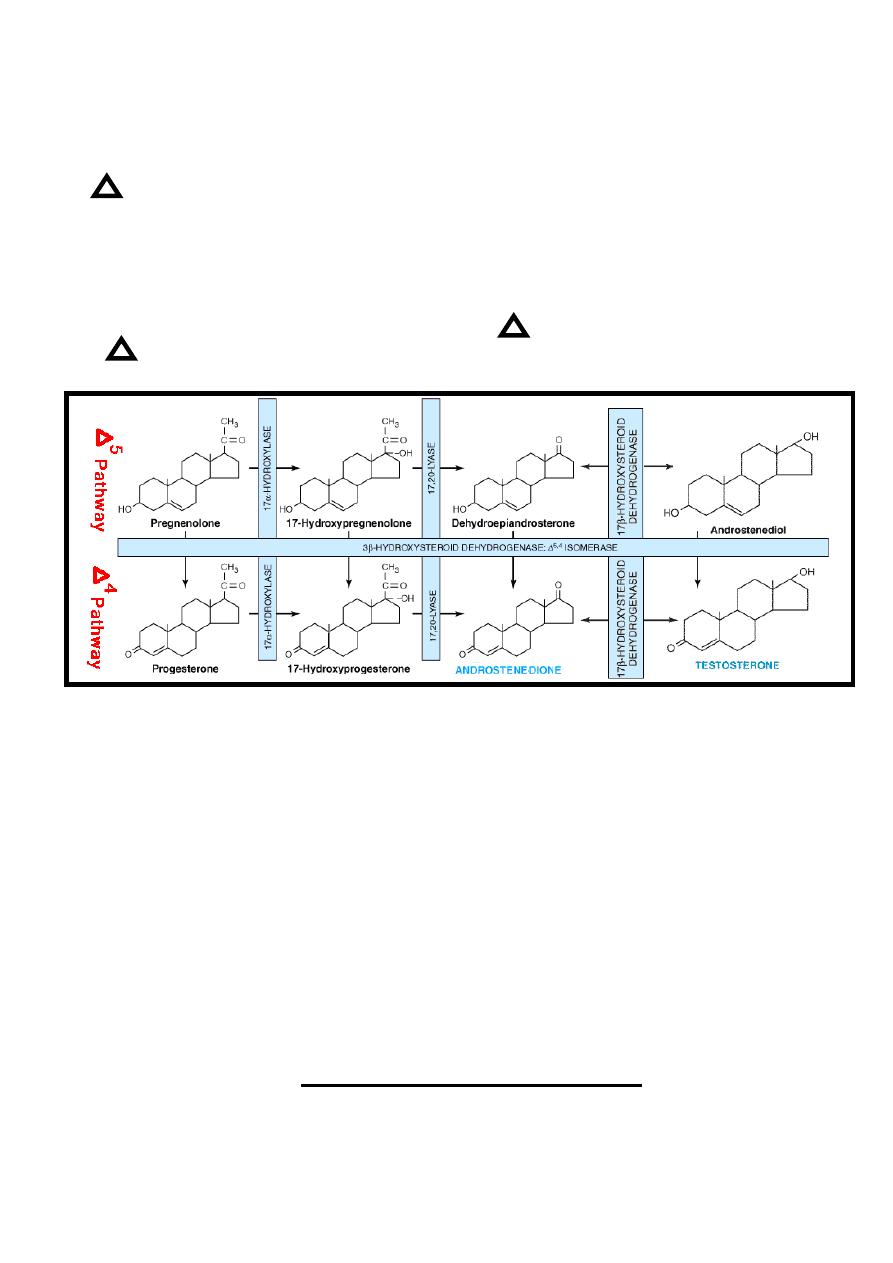
د بسام ادور/ كلية طب نينوى
- 8 -
mitochondria by StAR. The conversion of cholesterol to pregnenolone is
identical to adrenal. However, the reaction promoted by LH rather than ACTH,
which promote the reaction in adrenal cortex.
The conversion of pregnenolone to testosterone occurs in the smooth
endoplasmic reticulum of the leydig cells by two pathways that are-
1)
5
pathway... More common pathway, in which pregnenolone is converted
into 17-hydroxypregnenolone & DHEA (as in adrenal cortex) with additional
reversible reaction in which DHEA is converted into androstenediol by 17β-
hydroxysteroid dehydrogenase (17β -OHSD) enzyme which present in the
smooth endoplasmic reticulum of the leydig cells, then androstenediol is
converted to testosterone by (3 β -OHSD) &
5
'
4
isomerase enzymes.
2)
4
pathway... Conversion of progesterone into17-hydroxyprogesterone &
then into androstenedione which is converted to testosterone by 17β -OHSD.
All reactions involved in testosterone synthesis are irreversible except
reactions catalyzed by 17β -OHSD enzyme.
In addition to testosterone other hormones produced by testes are:-
1)-Dihydrotestosterone(DHT):produce from testosterone in irreversible reaction
catalyzed by NADPH-dependent 5 α-reductase enzyme, this reaction occurs
mainly in the extratesticular tissue & to less extent in the testes.
The plasma concentration of DHT in the adult male is about one-tenth to that
of testosterone, however testosterone considered a prohormone, since it is
converted into a much more potent compound which is DHT. However there
are certain receptors in the body are sensitive to testosterone as spermatogonia,
brain, kidney, muscle & bone while other receptors are sensitive to DHT as
prostate, external genitalia & genital skin.
2)- Estradiol(E
2
) :produced in small amounts mainly from testosterone.
Function of Testicular Hormones
1- Spermatogenesis.
2- Secondary sexual characters.
3- Male sexual characters which requires DHT as enlargement of prostate &
د بسام ادور/ كلية طب نينوى
- 9 -
external genitalia.
4- Male sexual behavior.
5- Anabolic effect.
Transport of Testosterone
Testosterone in male is synthesized in the testes & secreted immediately into blood
circulation (no storage) while in female it produced by the ovary in little amount.
In the blood circulation testosterone present as follow:-
1- Unbound (free) testosterone represents the biologically active fraction
constitutes about 2% of the total plasma testosterone in male & 1% in female.
2- Bound testosterone represents the biologically inactive & reservoir
fraction, the proteins that bind to testosterone are of two forms which are:-
A- Albumin...40% of the total plasma testosterone is bound to albumin in male
& 20% in female.
B-Sex hormone-binding globulin (SHBG) or called testosterone-estrogen
binding globulin (TEBG)... 58% of the total plasma testosterone is bound to
SHBG in male & 79% in female.
Metabolism of Testosterone
Two pathways that are metabolize testosterone:
1-In liver, testosterone oxidized to 17-ketosteroid which is followed by
conjugation at position 3 by glucuronate or sulphate forming 17-ketosteroid 3-
glucuronate or sulphate which is water soluble so it excreted through the bile duct
where majority is reabsorbed by enterohepatic circulation so its final excretion mainly
by urine & to less extent by feces & rarely through the skin.
2-Peripheral conversion of testosterone into the potent metabolite (DHT) & to
less extent into estradiol (E
2
) which thereafter estradiol is metabolized through
estrogen metabolic pathway.
د بسام ادور/ كلية طب نينوى
- 10 -
Hormones of Ovaries
The ovaries perform two related functions that are-
1-Production of female sex hormones, which are estrogens & progesterone.
2- Production of female germ cells which are the ova.
Synthesis of Ovarian Hormones
I- Estrogens: The estrogens are a family of hormones synthesized in a variety of
tissues mainly the ovary & during pregnancy from the placenta, these estrogens
include-
1)- Estradiol (E
2
) which is the main estrogen, synthesized by ovaries & from
peripheral tissues.
2)- Estrone (E
1
) which synthesized by ovaries & from tissues.
3)- Estriol (E
3
) which is synthesized during pregnancy from the placenta & also
synthesized during metabolism of E
2
& E
1
.
These peripheral tissues include mainly adipose cells, liver, skin & other
tissues.
II-Progesterone: Progesterone, a precursor for all steroid hormones, is produced
& secreted by the corpus luteum as an end product hormone because these cells do
not contain the enzymes necessary to convert progesterone to other steroid
hormones, during pregnancy progesterone is produced from the placenta.
Function of Ovarian Hormones
1-Estrogens & progesterone regulate the menstrual cycle.
2-Estrogens & progesterone with placental hormones maintain pregnancy.
3-During pregnancy; estrogens & progesterone with placental hormones &
prolactin help in breast development for lactation.
4-Estrogens help in development of secondary female sex characteristics.
د بسام ادور/ كلية طب نينوى
- 11 -
5-Estrogens have anabolic effect on certain tissues as bone & cartilage.
Transport of Ovarian Hormones
Ovarian hormones are synthesized & secreted immediately into the blood circulation
(no storage)
In blood circulation:-
Estrogens are carried in blood bound to SHBG (TEBG).
Progesterone carried in blood circulation bound to CBG.
Metabolism of Ovarian Hormones
Estrogens metabolism take place mainly in the liver where some of E
2
& E
1
are converted into E
3
, then these three estrogens components (E
1
, E
2
& E
3
) are
conjugated with glucuronate or sulphate to become inactive water soluble
compounds & so excreted in urine & feces.
Progesterone metabolism occurs also in the liver through conjugation with
glucuronate to be excreted in urine & feces.
د بسام ادور/ كلية طب نينوى
- 12 -
Hormones of Adrenal Medulla
Adrenal medulla considers as neuro-endocrine unit because it's a part of
sympathetic nervous system & also produces the catecholamines hormones
which are dopamine, norepinephrine, & epinephrine.
Control of Catecholamines
The release of catecholamines from the adrenal medulla is stimulated by the
low level of catecholamines in the body & vice versa when the level of
catecholamines is elevated it inhibits its release from the adrenal medulla.
Biosynthesis of Catecholamines
Catecholamines (dopamine, norepinephrine & epinephrine) are synthesized in the
final form from the amino acid tyrosine by chromaffin cells of the adrenal medulla
& stored in these cells to be released on need, these cells also present in the some of
the extramedullary tissues such as heart, liver, kidney, gonads, sympathetic fibers
& CNS. However, the main differences between catecholamines produced by
adrenal medulla & that produced by the extramedullary tissues are:-
1- Epinephrine is the main product of adrenal medulla while norepinephrine is
the main product of extramedullary tissues.
2-Catecholamines produced by adrenal medulla are transport by blood
circulation to act on other tissues while catecholamines produced by
extramedullary tissues are act locally.
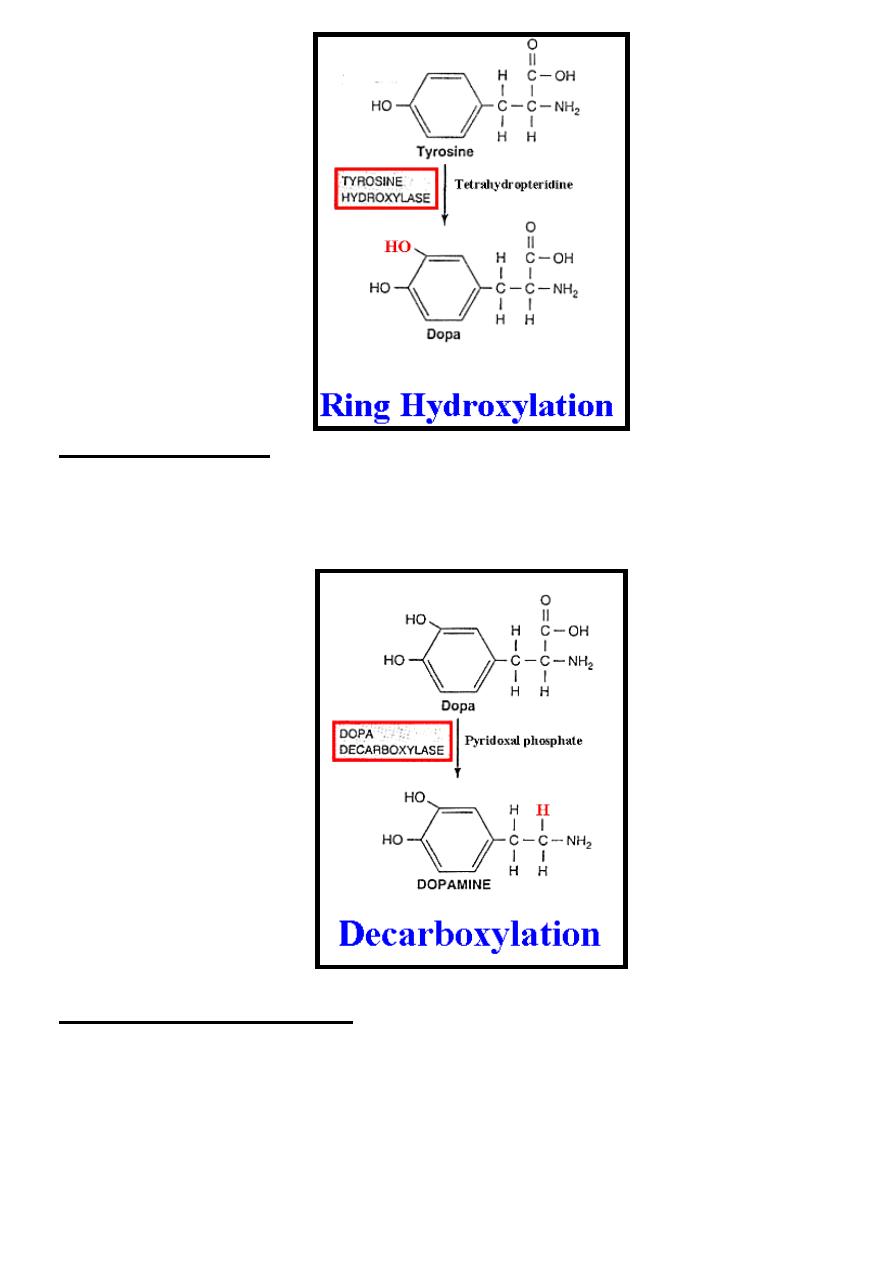
The sequential steps for conversion of tyrosine into epinephrine are:-
(1) Ring hydroxylation.
(2) Decarboxylation.
(3) Side chain hydroxylation
(4) N-Methylation.
(1) Ring hydroxylation:- It occurs in the cytoplasm of chromaffin cells, by this
step ring hydroxylation of L-tyrosine result in the formation of L-3,4-
dihydroxyphenylalanine (L-dopa), this reaction is irreversible & is catalyzed by
tyrosine hydroxylase enzyme in the presence of tetrahydropteridine as a
cofactor. It is the rate-limiting step of catecholamines biosynthesis.
د بسام ادور/ كلية طب نينوى
- 13 -
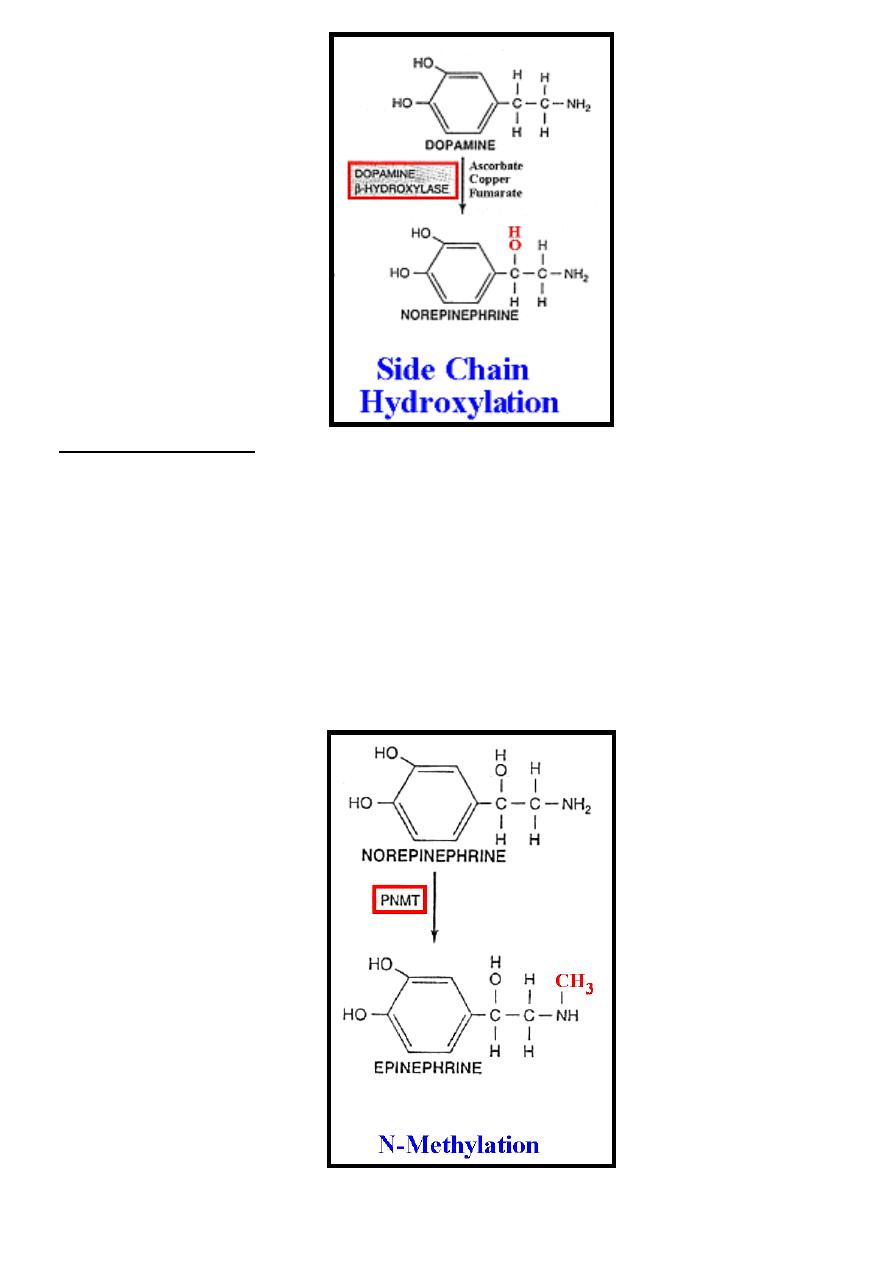
(2) Decarboxylation:- It occurs in the cytoplasm of chromaffin cells, by this step
decarboxylation
of
L-dopa
result
in
the
formation
of
3,4-
dihydroxyphenylethylamine (dopamine), this reaction is irreversible & is
catalyzed by dopa decarboxylase enzyme in the presence of pyridoxal
phosphate as a coenzyme.
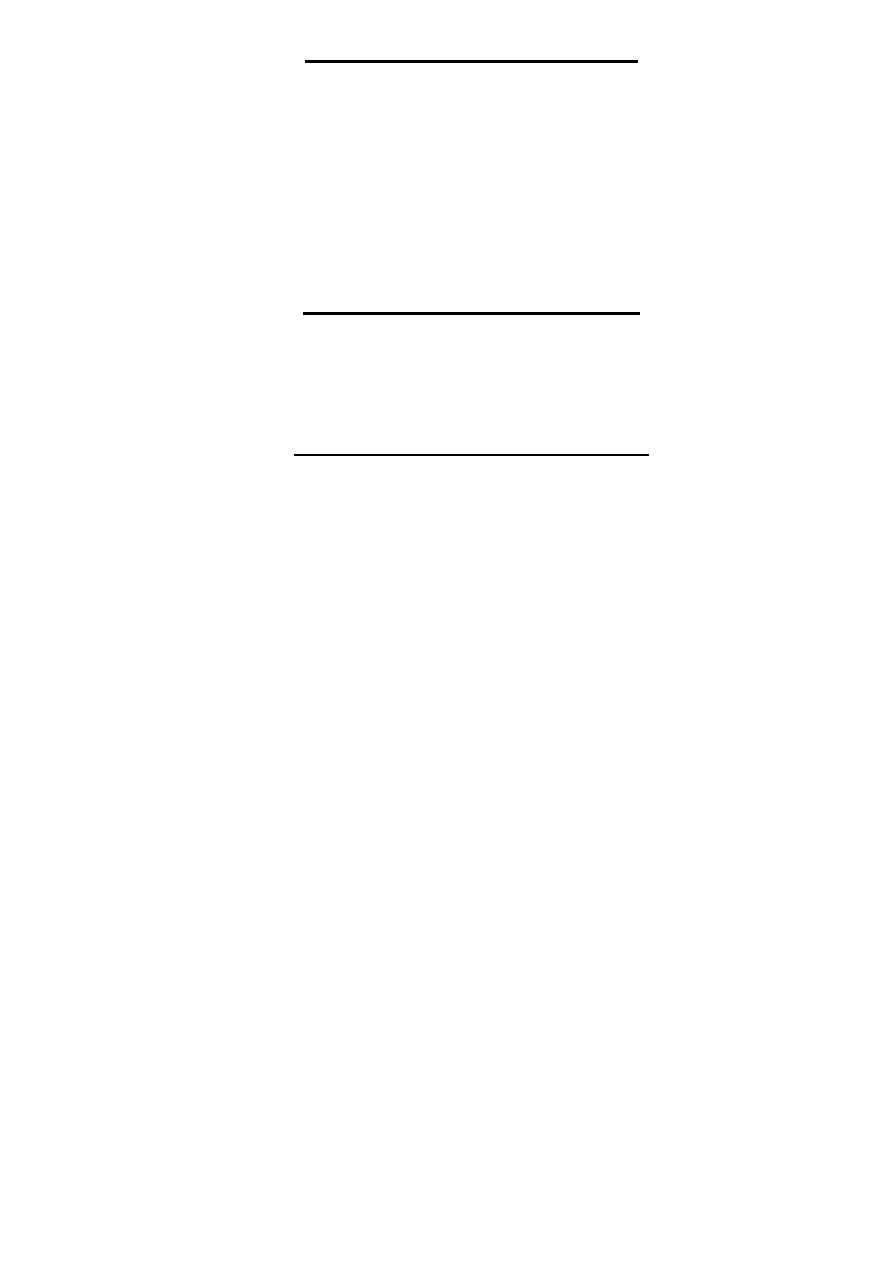
(3) Side chain hydroxylation:- It occurs in the secretion granules of chromaffin
cells, by this step side chain hydroxylation of dopamine result in the formation of
norepinephrine, this reaction is irreversible & is catalyzed by dopamine β-
hydroxylase (DBH) enzyme in the presence of ascorbate ,copper & fumarate as a
coenzyme.
Once norepinephrine is formed it returns back into cytoplasm for further step.
د بسام ادور/ كلية طب نينوى
- 14 -
(4) N-Methylation: - It occurs in the cytoplasm of chromaffin cells, by this step
N-methylation of norepinephrine result in the formation of epinephrine, this
reaction is irreversible & is catalyzed by phenylethanolamine-N-
methyltransferase (PNMT) enzyme.
The synthesis of PNMT requires induction by high glucocorticoid hormones
concentration (100-fold concentration gradient over systemic arterial blood)
which present in the adrenal medulla & this explain why epinephrine is the main
product of adrenal medulla & norepinephrine is the main product of
extramedullary tissues (not contain high glucocorticoid concentration).
After formation of norepinephrine & epinephrine, they stored in secretion
granules of chromaffin cells to be released on need.
د بسام ادور/ كلية طب نينوى
- 15 -
Functions of Catecholamines
The main functions of catecholamines especially norepinephrine & epinephrine
are the followings:-
1- Share in the metabolic response toward trauma.
2-Provide fatty acids as a source of energy.
3-Provide glucose which is important source of energy to brain by:-
A-Increase glucose production.
B-Inhibit insulin release.
Transport of Catecholamines
Since catecholamines are hydrophilic, after secretions are not associated in
plasma with carrier proteins, therefore, they have short plasma half-life (10-30
seconds).
Metabolism of Catecholamines
Metabolism of catecholamines occurs in the liver through complicated
pathways where both norepinephrine & epinephrine are end in the formation of
Vanillyl Mandelic Acid (VMA) while dopamine is end in the formation of
Homovanillic Acid.
Both VMA & Homovanillic Acid are conjugated in the liver with glucuronate
or sulphate to be excreted mainly by the urine.
د بسام ادور/ كلية طب نينوى
- 16 -
Thyroid Hormones
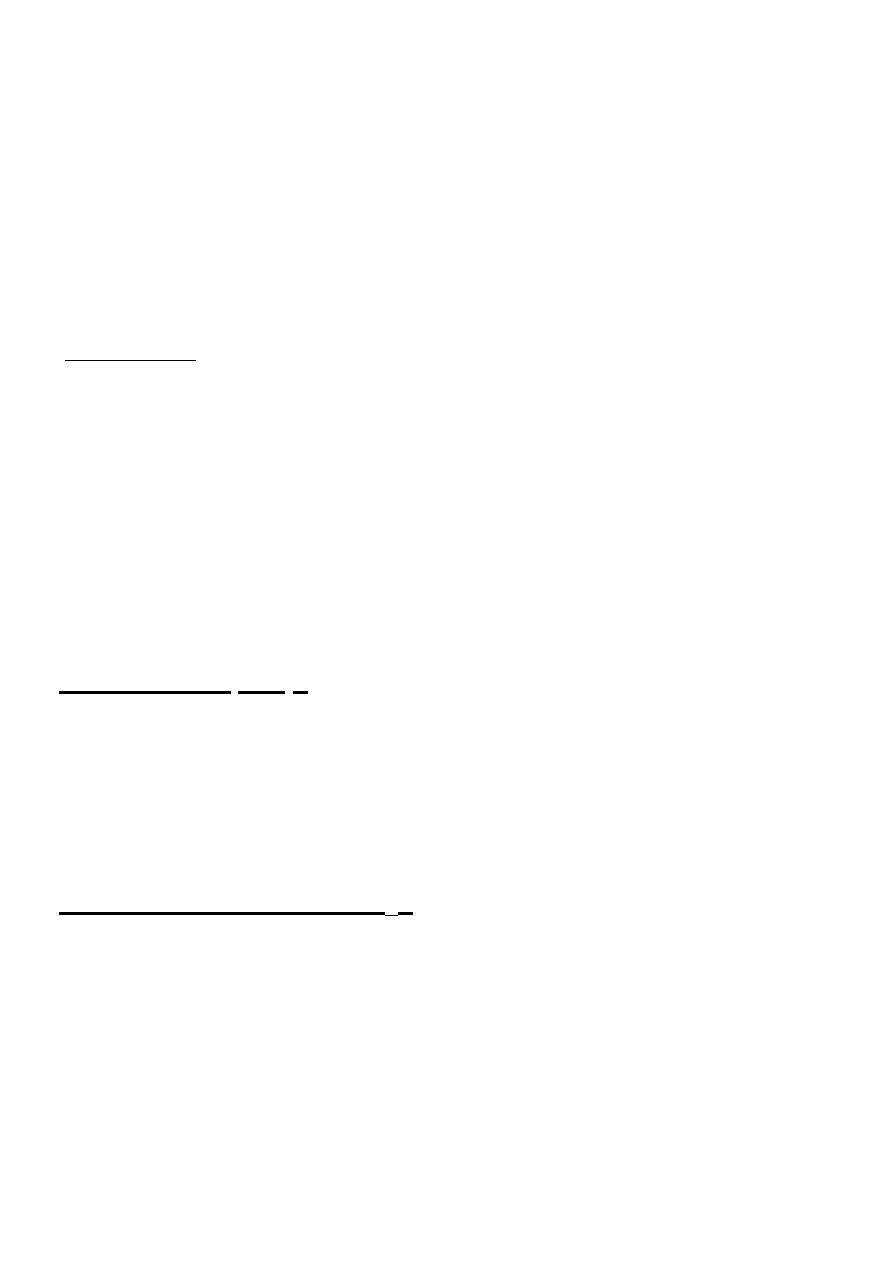
The thyroid gland produces the following hormones:-
1)- 3, 5, 3', 5' tetraiodothyronine (thyroxine, T
4
) & 3, 5, 3' triiodothyronine (T
3
)
produced by thyroid follicles.
2)- Calcitonin produced by C-cells of the thyroid gland.
We study here T
4
& T
3.
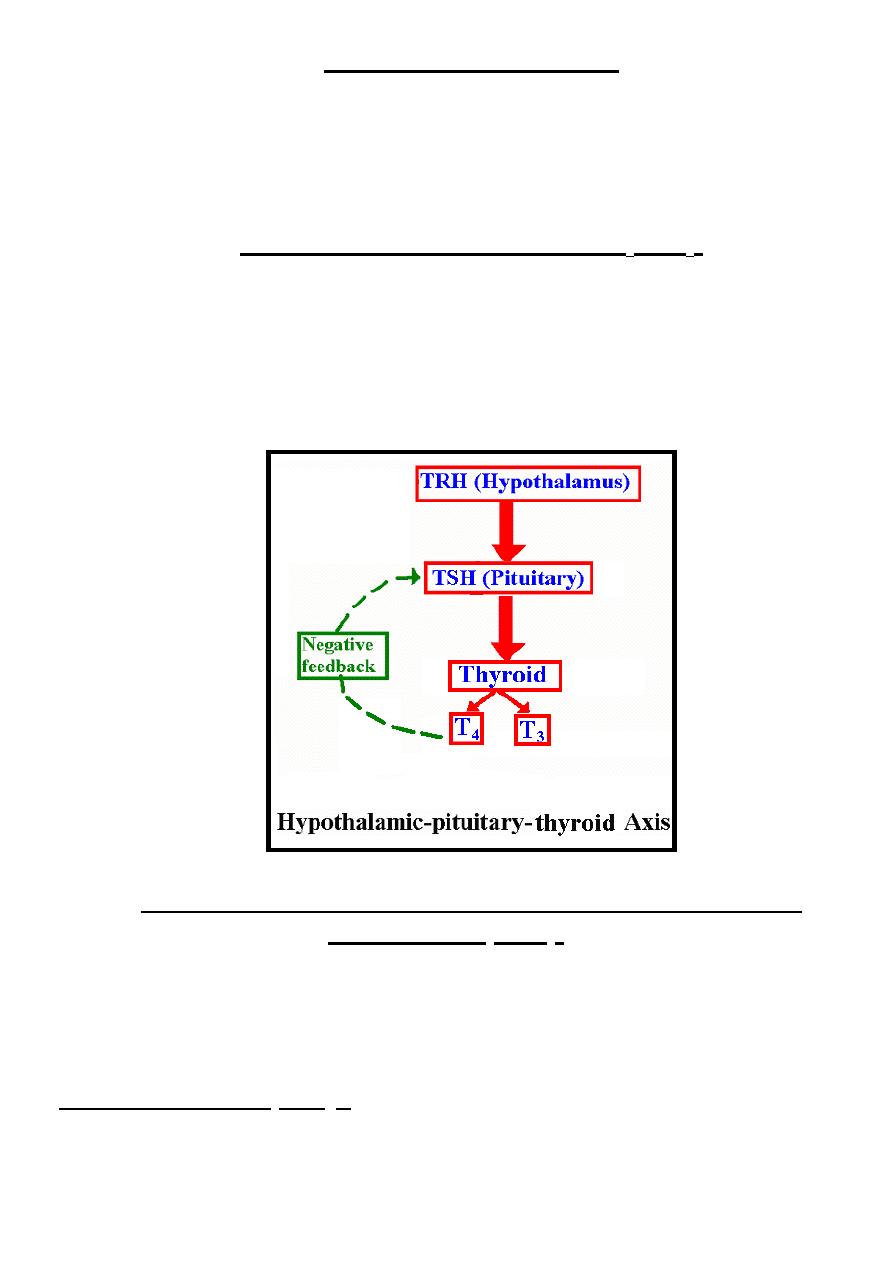
Control of Thyroid Hormones ( T
4
& T
3
)
The physiological control of thyroid hormones (T
4
& T
3
) occurs through
hypothalamic-pituitary-thyroid axis by production of hypothalamic
thyrotropin-releasing hormone (TRH) which stimulates the release of thyroid-
stimulating hormone (TSH) from the anterior pituitary gland; this TSH
stimulates the release of thyroid hormones (T
4
& T
3
).
Increase free thyroid hormones level mainly free T
4
cause negative feedback
inhibition to this axis through suppression of TSH mainly.
Biosynthesis, Release & Peripheral Conversion of Thyroid
Hormones ( T
4
& T
3
)
The thyroid hormones T
3
& T
4
are unique in that the rare element iodide is an
essential component of both; they are synthesized as part of a very large precursor
molecule (thyroglobulin) which stored in the colloid to be released on need & there
is a peripheral conversion of T
4
to T
3
which is a much more active hormone.
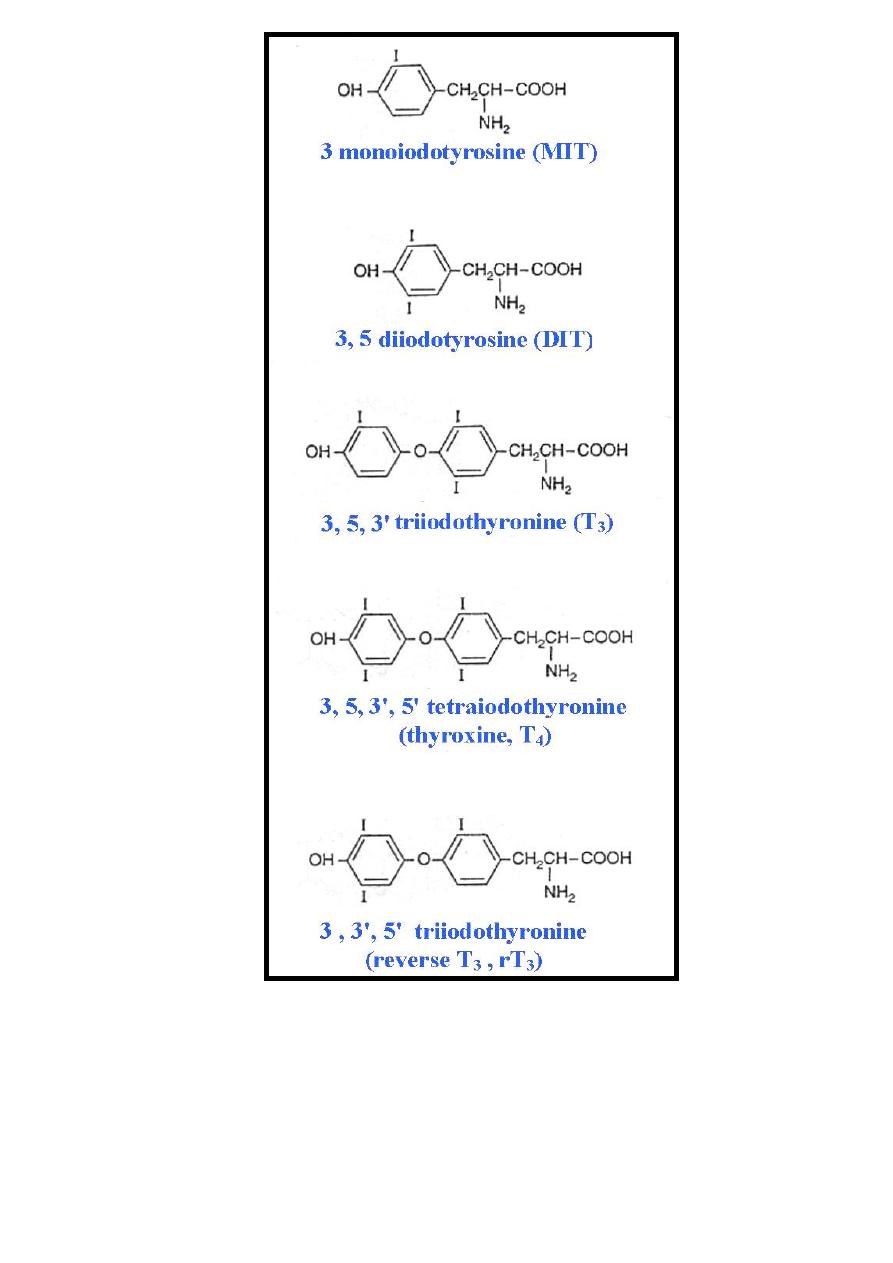
A))-Biosynthesis of T
4
& T
3
:- It occurs through the following steps:-
1-Concentration of iodide by the thyroid:- In most parts of the world, iodide is
present in little amount in the food, therefore, thyroid should have a mechanism for
د بسام ادور/ كلية طب نينوى
- 17 -
acquire & retain this crucial element, this activity is primarily controlled by TSH.
According to this activity, the ratio of iodide in thyroid to iodide in serum is about
25:1.
2-Oxidation of iodide: - The thyroid is the only tissue that can oxidize iodide to
iodine, an obligatory step for synthesis of T
4
& T
3
, this step is catalyzed by
thyroperoxidase enzyme & occurs at the luminal surface of the follicular cell.
Once oxidation occurs, the iodine does not readily leave the thyroid.
3-Iodination of tyrosine (Iodine organification):- Iodination of tyrosine lead to
formation of 3 monoiodotyrosine (MIT) & 3, 5 diiodotyrosine (DIT), this synthesis
takes place in thyroglobulin & catalyzed by the same thyroperoxidase enzyme that
catalyze the oxidation of iodide.
Thyroglobulin is the precursor of T
4
& T
3
. It’s a large iodinated, glycosylated
protein with a molecular mass of 660 kDa. It consists of two large subunits. It
contains 115 tyrosine residues on its surface, each of which is a potential site of
iodination. Thyroglobulin is synthesized in the basal portion of the follicular cell &
moves to the lumen (in the colloid), where iodination occur.
4-Coupling:- The coupling of some of MIT & DIT lead to formation of T
4
if
coupling occurs between
two DIT molecules & formation of T
3
if coupling occurs
between
MIT & DIT, this process occurs within the thyroglobulin molecule which
present in the colloid, this reaction is catalyzed by a coupling enzyme.
Therefore, thyroglobulin which stored in the colloid contain a mixture of MIT,
DIT, T
3
& T
4
in which about 70% of tyrosine present in the form of MIT & DIT &
30% present in the form of T
3
& T
4
with T
4
:T
3
ratio is about 7:1.
B))-Release of T
4
& T
3
:- Within minutes after stimulation of the thyroid gland by
TSH, colloid ( contain thyroglobulin) reenters the follicular cell where
thyroglobulin will phagocytes in the follicular cells & so lysosomal enzymes
hydrolyze the thyroglobulin into its constituent including T
4
, T
3
, MIT & DIT .
T
4
& T
3
are discharged from the follicular cell into the circulation while MIT &
DIT are subjected in the follicular cell to the deiodination process that catalyzed by
deiodinase enzyme & by this process MIT & DIT are hydrolyzed into their
constituents which are tyrosine & iodide to be reused in thyroid hormone synthesis.
C))- Peripheral conversion of T
4
:-. A peripheral deiodinase enzyme in target
tissues such as pituitary, kidney & liver selectively removes iodide from the 5'
position of about 80% of T
4
to make T
3
, which is a much more active molecule.
In this sense, T
4
thought to be a prohormone.
In certain circumstances as starvation, chronic illness, following surgery & in
certain drugs the peripheral deiodinase enzyme in target tissues such as pituitary,
kidney & liver selectively removes iodide from the 5 position of T
4
to make 3 , 3',
5' triiodothyronine or called reverse T
3
( rT
3
)
which is a weak thyroid hormone.
د بسام ادور/ كلية طب نينوى
- 18 -
د بسام ادور/ كلية طب نينوى
- 19 -
Function of Thyroid Hormones ( T
4
& T
3
)
Most of the function attributed to T
3
, which has the following functions:
1-Increase oxygen consumption in all body tissues except brain, gonads &
reticuloendothelial system (RES).
2-Increase activity of Na
+
/ K
+
pump in all body tissues.
د بسام ادور/ كلية طب نينوى
- 20 -
3-Anabolic effect.
4-Modulator effect on certain developmental processes as epidermal tissues,
conversion of HbF into HbA & stimulation of urea cycle enzymes.
Transport of Thyroid Hormones ( T
4
& T
3
)
Nearly all thyroid hormones transported in the circulation as protein-bound while the
remaining small-unbound (free) fraction is responsible for the biologic activity.
Most of thyroid hormones bound to a specific binding protein called thyroxine-
binding globulin (TBG) & to less extent to thyroxine-binding prealbumin &
albumin. Under normal circumstances, TBG binds T
4
with greater affinity than T
3
making:
1- Plasma half-life of T
4
is higher than that of T
3
so the plasma concentration of total
T
4
is higher than that of T
3
.
2- free fraction of T
3
(0.2% of plasma T
3
) is higher than that of T
4
(0.05% of plasma
T
4
) making the plasma concentration of free T
3
is nearly equal to free T
4
concentration & because T
3
is more active than T
4
so that most of the biologic
activity is attributed to T
3
.
Metabolism of Thyroid Hormones ( T
4
& T
3
)
The first step of thyroid hormones metabolism occurs in almost all tissues then in
the liver they are conjugated with glucuronate or sulphate to be excreted in urine
or feces.

د بسام ادور/ كلية طب نينوى
- 21 -
Hypothalamic Hormones
The main hypothalamic hormones are:-
1- Corticotropin-Releasing Hormone (CRH): Stimulates the release of
ACTH from the anterior pituitary gland.
2- Gonadotropin-Releasing Hormone (Gn-RH): Stimulates the release of both
FSH & LH from the anterior pituitary gland.
3-Thyrotropin-Releasing Hormone (TRH): Stimulates the release of TSH from
the anterior pituitary gland.
4- Growth Hormone Releasing Hormone (GHRH): Stimulates the release of
Growth hormone (GH) from the anterior pituitary gland.
5- Growth Hormone Releasing Inhibitory Hormone (GHRIH) or called
somatostatin: Inhibits the release of GH from the anterior pituitary gland.
6- Prolactin Inhibitory Hormone (PRIH): Inhibits the release of prolactin
(PRL) from the anterior pituitary gland.
These hypothalamic hormones reach the anterior pituitary gland through
hypothalamic hypophyseal portal circulation & the secretion of these
hypothalamic hormones usually occur in the pulsatile episodic manner in such a
way that the pituitary gland is sensitive to these pulses.
د بسام ادور/ كلية طب نينوى
- 22 -
Hormones of Pituitary Gland
Pituitary gland consists of three lobes which are:-
1-Anterior lobe which produces many hormones.
2-Intermediate lobe which is usually rudimentary in human except in fetus &
during late pregnancy.
3-Posterior lobe which produces:-
A)-Antidiuretic hormone(ADH) : regulate body water homeostasis.
B)-Oxytocin hormone: initiate & maintain milk ejection from the breast.
Anterior Pituitary Hormones
The anterior lobe of pituitary gland produces many of tropic hormones that
regulate the function of other endocrine glands as well as it produces other
hormones that regulate certain metabolic process in target tissues.
Some of the anterior pituitary hormones are shared structural similarity with
certain placental hormones so that these placental hormones are included with
anterior pituitary hormone classification.
Anterior pituitary hormones can be classified into three groups according to
their structural similarity, these groups are:-
I))- GH, PRL & CS ((Chorionic somatomamotropin)).
II))- Glycoprotein hormones which include FSH, LH, TSH & CG ((Chorionic
gonadotropin)).
III))- Pro-opiomelanocortin (POMC) family which include ACTH, LPH ((Lipotropin
hormone)), MSH ((Melanocyte-stimulating hormone)) & endorphins.
GH, PRL & CS
These three hormones are peptide hormones with some structural similarity between
them; all they have tryptophan amino acid at position 85 in GH & CS & at position 91
in PRL.
Growth Hormone (GH) (Somatotropin)
This hormone is secreted by somatotrope cells in anterior pituitary in pulsatile
episodic manner.
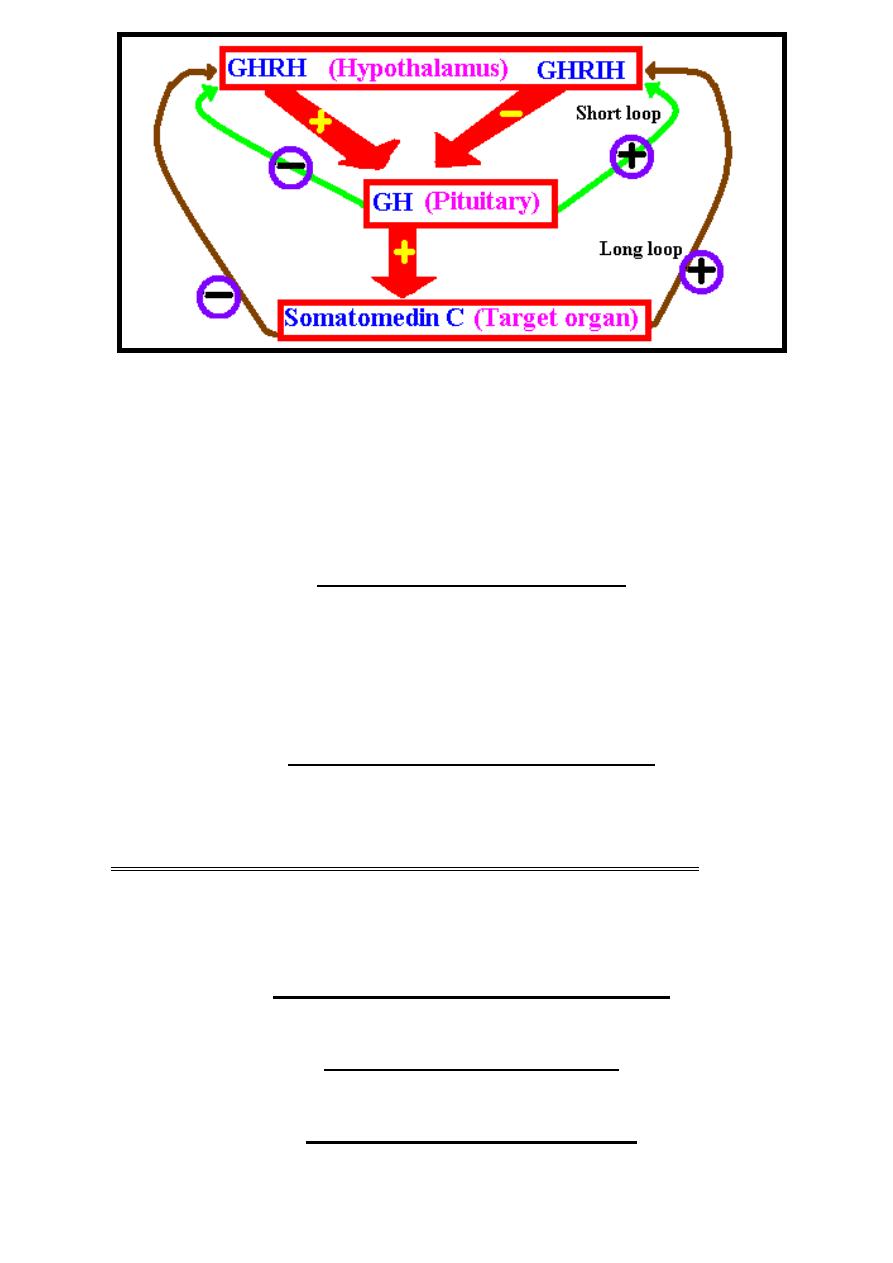
Physiological control of GH secretion by:-
Hypothalamic GHRH which stimulate the release of GH from anterior pituitary
gland until GH reach the desire level where GH by itself cause negative feed back
inhibition to GHRH & stimulation to GHRIH (Somatostatin) this is called (short loop
control).
GH acts on target organ & its effect is mediated by certain mediator that
produced by the liver called Somatomedin C or called Insulin growth factor (IGF) ,
this mediator when reach its desire level it stimulates GHRIH & inhibit the
secretion of GHRH this is called (long loop control).
د بسام ادور/ كلية طب نينوى
- 23 -
The main metabolic function of GH include:-
1-Control of postnatal growth.
2-Its effect on carbohydrate metabolism is opposite to that of insulin (increase
blood glucose).
3-Its effect on lipid metabolism is opposite to that of insulin (stimulate lipolysis
& ketogenesis).
4-Its effect on protein metabolism is similar to that of insulin (anabolic effect).
Prolactin (PRL) (Lactotropin)
PRL secreted by lactotrope cells of anterior pituitary gland.
PRL secretion is inhibited (negative control) by hypothalamic PRIH.
The main function of PRL is stimulation of breast tissue development & milk
production in female while its function in male is still unclear, however, might
have some role in the fertilization process.
Chorionic Somatomamotropin (CS)
Placental hormone responsible for prenatal growth otherwise has the same metabolic
function of GH.
Glycoprotein Hormones (FSH, LH, TSH, CG)
These four glycoprotein hormones consist of two subunits (α & β subunits)
with α-subunit is identical in all these four hormones while the β subunit is
differ according to the type of hormone & so determine its specificity.
Follicle-Stimulating Hormone (FSH)
FSH produced by gonadotrope cells of anterior pituitary gland.
Luteinizing Hormone (LH)
LH produced by gonadotrope cells of anterior pituitary gland.
Chorionic Gonadotropin (CG)
Produced by chorionic villa & has structural similarity with LH & its main
د بسام ادور/ كلية طب نينوى
- 24 -
function is to maintain corpus luteum in early weeks of pregnancy until the
placenta is capable to produce female sex hormones.
Thyroid-Stimulating Hormone (TSH)
TSH produced by thyrotrope cells of anterior pituitary gland. The main function
of TSH is to stimulate thyroid hormone synthesis by thyroid gland.
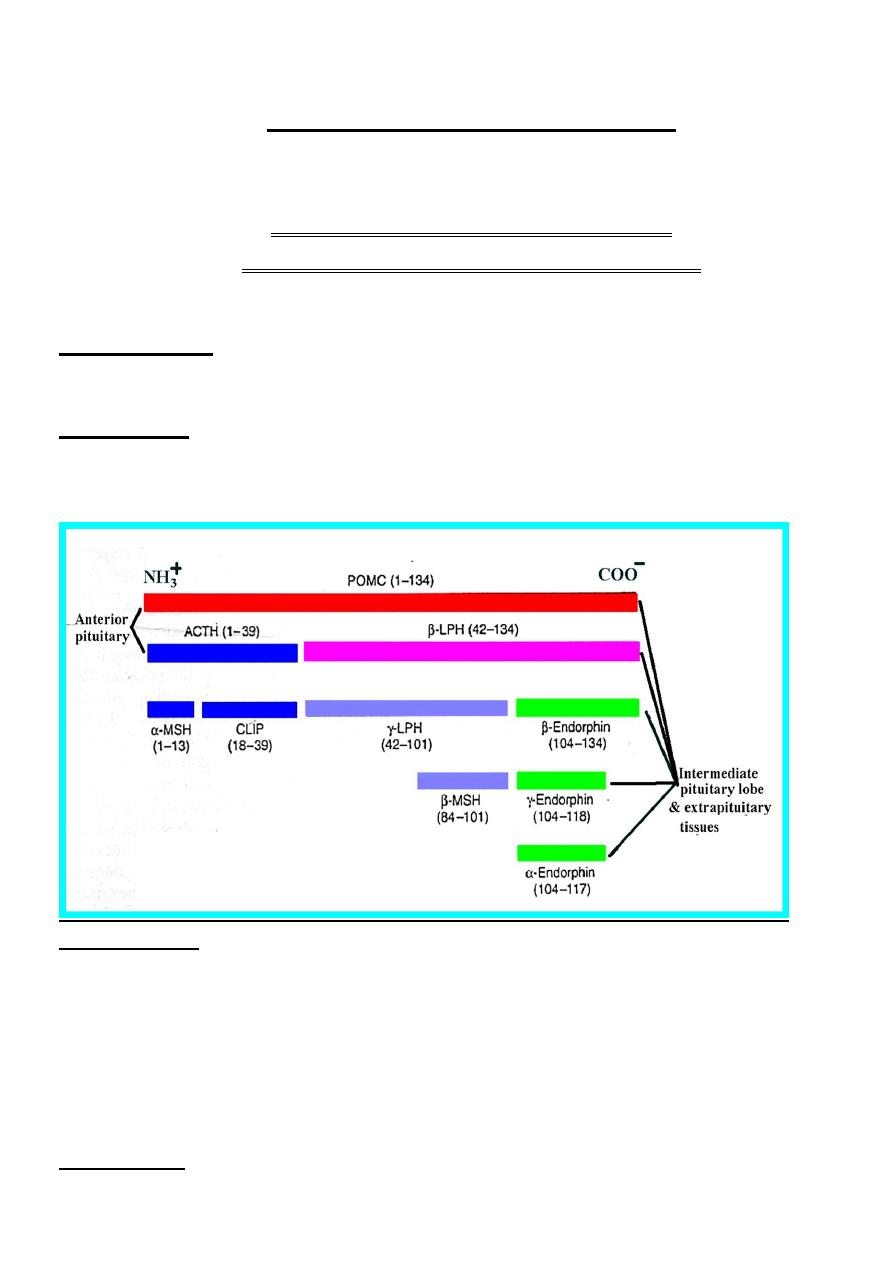
Pro-opiomelanocortin (POMC)
[ACTH, LPH, MSH & Endorphins]
ACTH, LPH, MSH & Endorphins are formed from POMC & have
characteristic distribution, processing, regulation & function.
*Distribution:- POMC are present mainly in anterior & intermediate lobes of
pituitary & to less extent in extrapituitary tissues as brain, GIT, gonads, lung ,
lymphocyte & placenta.
*Processing:- POMC has incomplete processing in anterior lobe of pituitary
while it has almost complete processing in the intermediate lobe of pituitary &
other extrapituitary tissues. The intermediate lobe of pituitary is usually
rudimentary in human except in fetus & during late pregnancy.
*Regulation:-
In anterior lobe of pituitary: They regulated by hypothalamic hormonal
factors & neural factors.
In intermediate lobe of pituitary, this structure is poorly vascularized;
therefore, it has no proper communication with hypothalamic hypophyseal
portal circulation so that hypothalamic hormonal factors have no role in their
regulation; therefore they regulated by neural factors.
In extrapituitary tissues, They regulated by neural factors.
*Function:- POMC is consider as precursor for the following:-
د بسام ادور/ كلية طب نينوى
- 25 -
1-ACTH: It has the following functions:-
A-Stimulates adrenocortical hormone production.
B-Growth promoting effect on adrenal cortical cells.
ACTH consists of 39 amino acids; however, the first N-terminal 24 amino
acids are responsible for full ACTH biological activity, therefore, synthetic
ACTH (synacthen) have only these 24 amino acids.
2-LPH (Lipotropin hormone): Its main function is the stimulation of lipase
enzyme causing the release of FFA.
3-MSH (Melanocyte-stimulating hormone): It stimulates melanin distribution
in melanocyte so it controls darkening process of the skin.
4-Endorphins: Include α, β & γ endorphins, most potent one is β-endorphin.
These endorphins have the following functions:-
A-Act as neurotransmitters by binding the opiate receptors in higher centers so
minimizing the feeling of pain 20-30 times more potent than morphine.
B-Help in contraction of reproductive system musculature so help in delivery,
therefore, intermediate lobe of pituitary developed in late pregnancy.
C-Have limited effect on control temperature & blood pressure.
د بسام ادور/ كلية طب نينوى
- 26 -
Hormones of Pancreas
Pancreas consists of two parts that are-
I-Exocrine (acinar) part: - Produce digestive enzymes.
II-Endocrine part (islet of langerhans):- Contains about 1-2 millions of
the islet of langerhans, it consists of four different cell types each produce
specific hormone as follow:-
1)-α (A) cells: Produce glucagon hormone & constitute 25 % of islet cells.
2)-β (B) cells: Produce insulin hormone & constitute 70 % of islet cells.
3)-δ (D) cells: Produce somatostatin hormone & constitute less than 5 %
of islet cells.
4) - F cells:- Produce pancreatic polypeptide hormone & constitute trace%
of islet cells.
Following secretion of these hormones, they enter the pancreatic vein to
reach the liver through the portal vein; therefore , liver is the first organ for the
action of these hormones specially insulin & glucagon.
Insulin
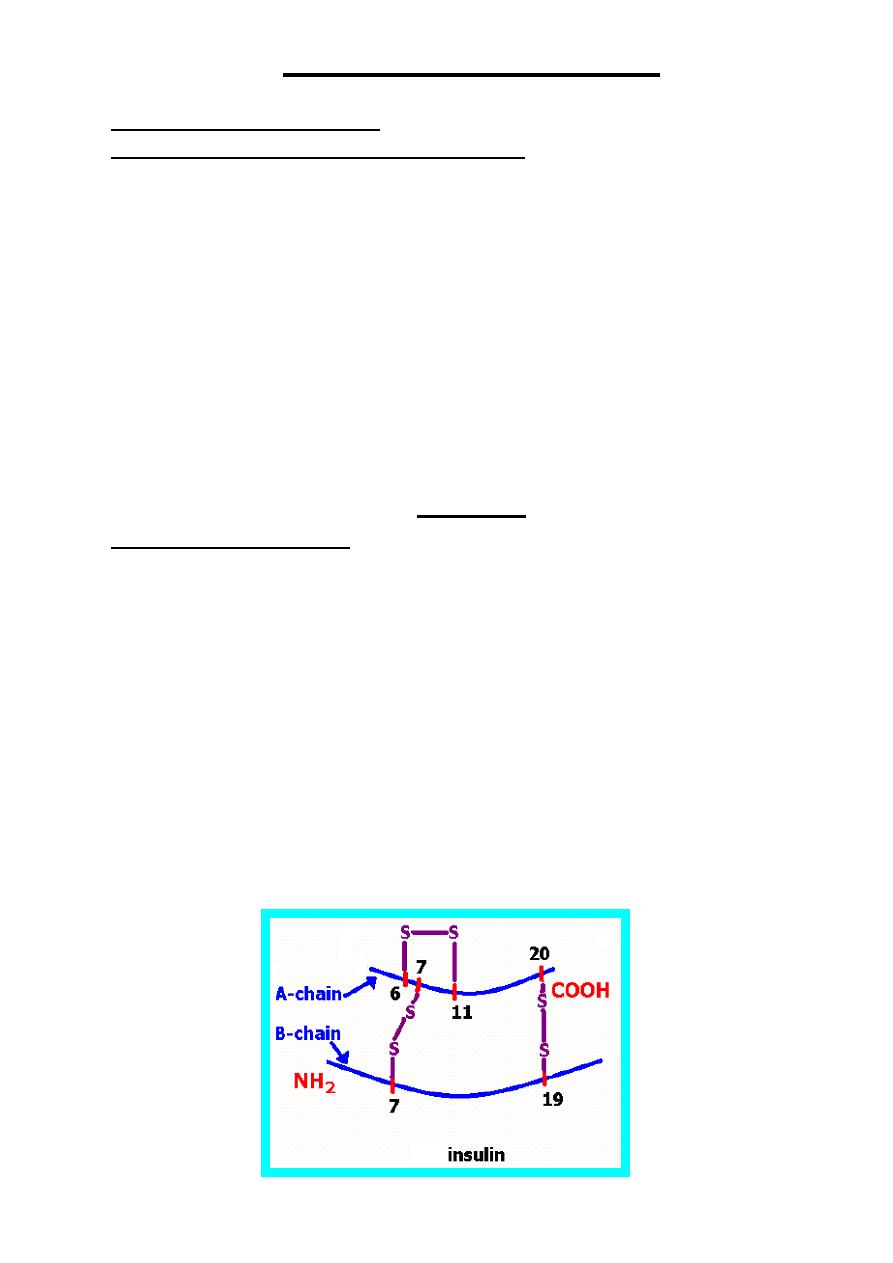
Chemistry of Insulin
Insulin is a peptide hormone synthesized by β (B) cells of islet of langerhans,
it is the first protein hormone discovered & synthesized.
Human insulin consists of two chains (A & B), A-chain consists of 21 amino
acids while B-chain consists of 30 amino acids.
Insulin contains S-S bridges, which are of two types:-
1-Interchain S-S bridges: Two bridges connect the two chains (A & B) of
insulin together as follow:-
*A7-B7: connect amino acid no. 7 of A-chain with amino acid no. 7 of B-chain.
*A20-B19: connect amino acid no. 20 of A-chain with amino acid no. 19 of B-
chain.
2-Intrachain S-S bridge: - One bridge connects amino acid no.6 of A-chain with
amino acid no. 11 of A-chain also (A6-A11).
د بسام ادور/ كلية طب نينوى
- 27 -
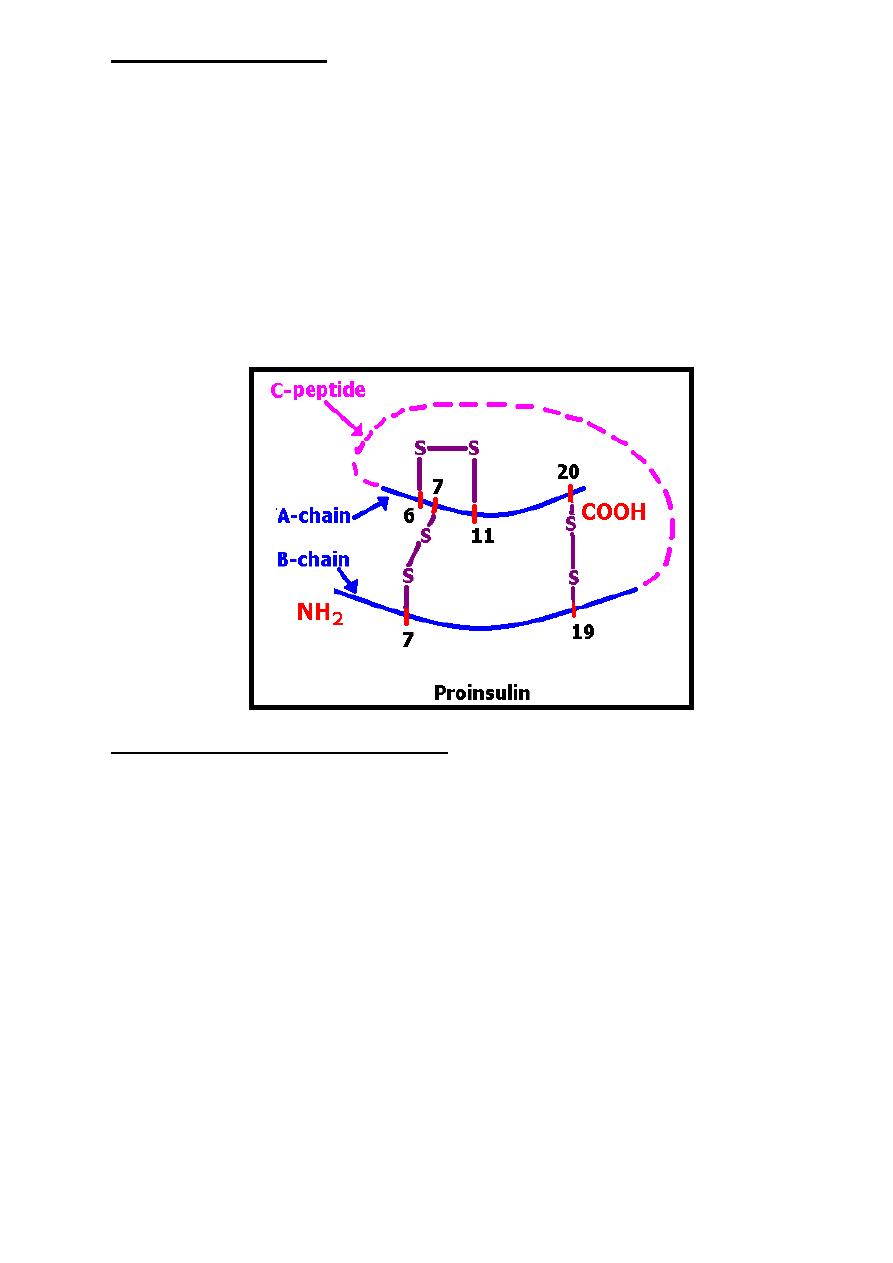
Synthesis of Insulin
In the rough endoplasmic reticulum of B-cells a common precursor
molecule of insulin called preproinsulin (M.Wt about 11500 Dalton) is present,
this structure through sequences of cleavage in rough endoplasmic reticulum
lead to formation of proinsulin with variable amino acids range from 78-86
(M.Wt about 9000 Dalton). This proinsulin is transported into the golgi
apparatus to be stored ,therefore, golgi apparatus consider as storage for insulin
(in the form of proinsulin).
The arrangement of proinsulin, starting from the amino terminal, is B
chain—connecting (C) peptide—A chain.
Upon appropriate stimulation, the proinsulin molecule undergoes cleavages
into equimolar amounts of insulin & C-peptide to be released into circulation
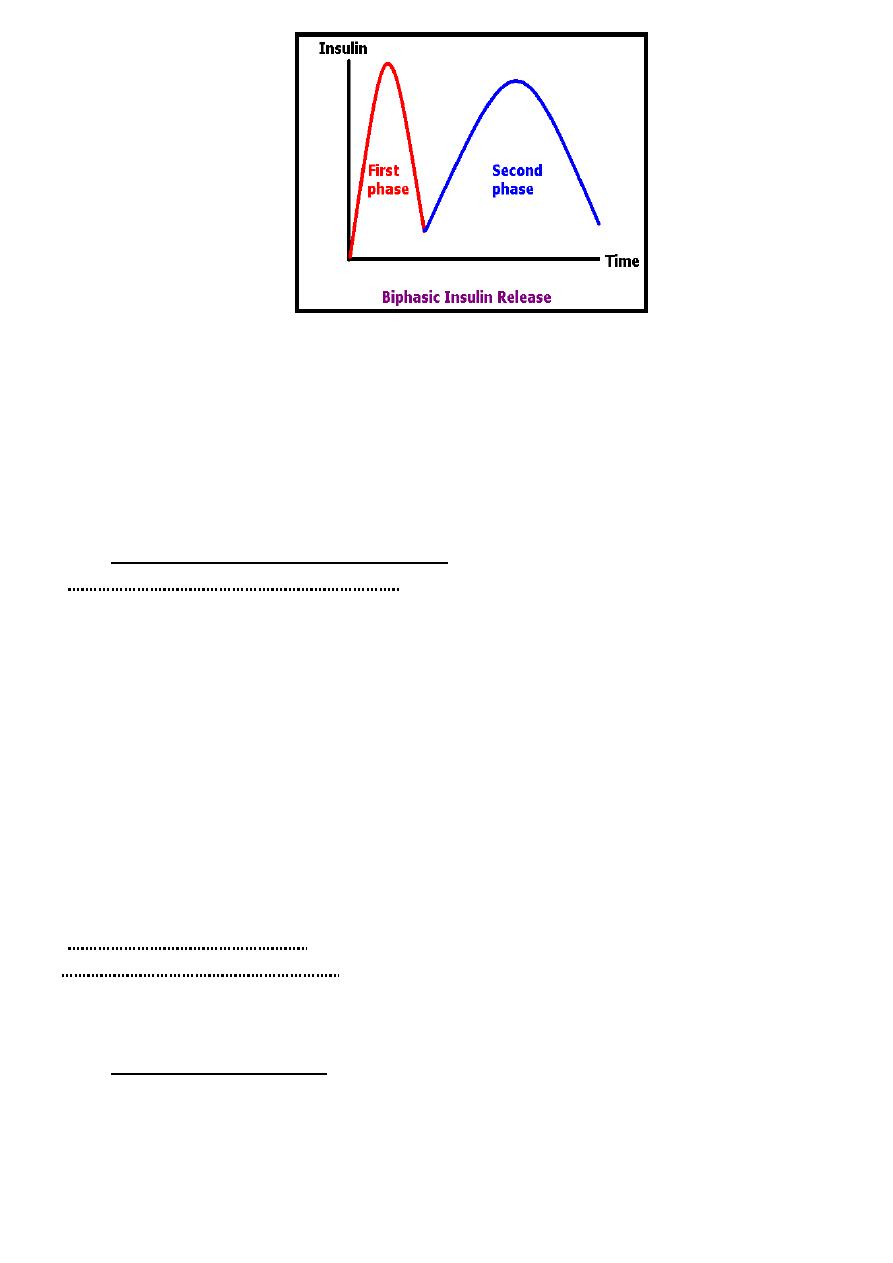
Regulation of Insulin Release
In healthy person about 40-50 units of insulin are released from the
pancreas daily which represent about 15-20% of the daily capacity of pancreas
to release insulin.
The following factors are concerned with insulin release:-
1-Blood glucose: Insulin starts to release when blood glucose
concentration reach 80-100 mg/dl & reaches its maximum level when blood
glucose concentration reaches 300-500 mg/dl.
Insulin release usually occurs in biphasic pattern where by:-
-First phase (acute phase) represents the release of already stored
proinsulin, occurs within 1 minute & last for 5-10 minutes.
-Second phase represents the newly formed insulin pool, occurs within 30
minutes & remains until the blood glucose returns to normal.
د بسام ادور/ كلية طب نينوى
- 28 -
2-Hormones:
*Chronic exposure to excessive levels of certain hormone as cortisol, placental
lactogen, progesterone & GIT hormones mainly GIP (Gastric inhibitory peptide)
or called (Glucose-dependant insulinotropic peptide) increase insulin release.
*Somatostatin inhibits insulin release.
3-Pharmacologic Agents: -Many drugs stimulate insulin secretion as
sulfonylurea compounds.
Metabolic Function of Insulin
1-On carbohydrate metabolism:-Insulin affects carbohydrate metabolism & so
reduce blood glucose through the following mechanisms:
A-Glucose transport: Insulin control the entry of glucose into the
extrahepatic tissues especially adipose tissues & muscles by carrier-mediated
facilitated diffusion. Glucose entry to liver occur by simple diffusion method
where insulin activate hepatic glucokinase enzyme so reduce hepatic
intracellular glucose concentration making a high difference between glucose
concentration in the portal system & the liver so facilitate simple diffusion for
glucose entry into the liver.
Insulin is not required for glucose entry to brain, this facilitate entrance
of glucose to brain even at low blood glucose level (when insulin level is low).
B-Glucose utilization: Insulin stimulates glycolysis & glycogenesis while
it inhibits glycogenolysis & gluconeogenesis
2-On lipid metabolism:- Insulin stimulates lipogenesis in adipose tissue.
3-On protein metabolism:- Insulin considers as a most important anabolic
hormone.
4-Share in metabolic response toward trauma.
Metabolism of Insulin
Since insulin is a peptide hormone, therefore, it has no specific carrier
protein so that its half-life short (3-5 minutes).
About 50% of the released insulin removed by liver after its first passage. Insulin
is metabolized in almost all body tissues specially liver, kidney & placenta.
د بسام ادور/ كلية طب نينوى
- 29 -
Glucagon
Chemistry of Glucagon
Glucagon is a second pancreatic islet cell hormone discovered, it's
synthesized as a precursor molecule (proglucagon) in the α (A) cells of the
pancreatic islets.
Glucagon consists from a single-chain polypeptide containing 29 amino
acids without S-S bridges.
Glucagon shares some immunologic & physiologic properties with
enteroglucagon (glucagon-like peptide) which produced by duodenal mucosa.
Regulation of Glucagon Release
1-Secretion of glucagon inhibited by hyperglycemia.
2-Secretion of glucagon stimulated by hypoglycemia.
3-Somatostatin inhibits glucagon release.
Metabolic Function of Glucagon
The liver is the primary target of glucagon action, metabolic functions of
glucagon reverse that of insulin & can summarized as follow:-
1-On carbohydrate metabolism: Glucagon stimulates glycogenolysis &
gluconeogenesis while it inhibits glycolysis & glycogenesis so that it elevates blood
glucose level.
2-On lipid metabolism: Glucagon stimulates lipolysis & tendency to ketosis.
3-On protein metabolism: - Glucagon consider as a catabolic hormone.
4-Share in metabolic response toward trauma.
Metabolism of Glucagon
Since glucagon is a peptide hormone, therefore, it has no specific carrier protein
making its half-life short (about 5 minutes).
Glucagon is inactivated by the liver.
Somatostatin
Somatostatin has the following tissue distribution:-
1-Hypothalamus: inhibits GH mainly.
2-CNS: act as neurotransmitter.
3-Pancreas: synthesized by δ (D) cells of pancreatic islets as 14 amino acids
peptide hormone. It has an inhibitory local paracrine effect on insulin, glucagon
& pancreatic polypeptide.
4-GIT: decrease delivery of nutrients from GIT into the circulation .
Pancreatic Polypeptide (PP)
PP is a 36-amino-acid peptide produced by F cells of the pancreatic islets.
The function PP is still unknown.
د بسام ادور/ كلية طب نينوى
- 30 -
Parathyroid Hormone (PTH)
Chemistry of PTH
PTH which is an 84-amino acids peptide is formed by parathyroid glands from a precursor
molecule called preproPTH (peptide with 115-amino acids) which form proPTH
(peptide with 90-amino acids), this proPTH then form PTH.
PTH
1-34
has full biologic activity .
Function of PTH
PTH increases the plasma ionized calcium (Ca
++
) concentration by:-
1-Stimulation of osteoclast activity leads to release of calcium & phosphate from the bone
to blood so that increases the plasma concentrations of both calcium & phosphate.
2-Increases renal tubular reabsorption of calcium which further increases plasma Ca
++
concentration & at the same time PTH decreases renal tubular reabsorption of phosphate to
overcome the phosphate elevation that result from the stimulation of osteoclast activity.
Regulation of PTH
The biosynthesis of PTH & its subsequent secretion are regulated by the plasma ionized
calcium (Ca
++
) level where an acute decrease of Ca
++
results in a marked increase of PTH
while increase of Ca
++
results in a marked decrease of PTH.
