Diagnosis and treatment planningin Partially Edentulous Arches
Dr. karam AhmedMSc. Operative Dentistry
“Most clinicians also choose an RPD for a partially edentulous patient if they need to restore lost residual ridge, achieve appropriate esthetics, increase masticatory efficiency, and improve phonetics but are unable to do so with dental implants or fixed partial dentures due to financial constraints or patient desires”
- Bohnenkamp DM Removable Partial Dentures : Clinical Concepts, Dent Clin N Am 58 (2014) 69–89
“Problems related to RPDs may be associated with errors in diagnosis and treatment planning, including inadequate mouth preparation “
- McCord JF et al Dent Update 2003; 30: 88–97
Definitions:
Diagnosis : the determination of the nature of a disease
Treatment plan : the sequence of procedures planned for the treatment of a patient after diagnosisPurpose and uniqueness to treatment
The delineation of each patient’s uniqueness occurs through the patient interview and clinical examination process.The ultimate treatment is individualized to address disease management and the coordinated restorative and prosthetic needs that are unique to the patient.
understanding the patient’s desires or chief concerns/complaints regarding his or her condition
ascertaining the patient’s dental needs through a clinical examination,
developing a treatment plan that reflects the best management of desires and needExecuting appropriately sequenced treatment with planned follow-up
Patient Interview
The dentist should follow a sequence that includes:
• Chief complaint and its history
2. Medical history review3. Dental history review, especially related to previous prosthetic
experience(s)4. Patient expectations
Evaluation of the patient ’s psychological status
Personal and psychological factors aresignificant to the success of prosthodontic treatment
House classification
- Philosophical- Exacting
- Hysterical
- Indifferent
- revisited
- Ideal- Submitter
- Reluctant
- Resistant
Clinical examination
The process of clinical examination involves two stages :
Medical examination
Oral examination
A comprehensive medical history includes :
systemic disorders (Chronic degenerative or dysfunctional diseases)
Medication history
Diet
Habits
Systemic disorders include:
HypertensionDiabetes
Pernicious anemia
Vitamin or nutritional deficiencies
Osteoporosis
Chronic pulmonary disease (i.e., emphysema and chronic bronchitis)
• Climacteric (i.e., menopausal changes)
• Parkinsonism• Salivary gland disorders
• TM disturbances
• Post radiation therapy
• Bell ’ s palsy
• Lichen planus
• Fungal infections
Oral examination
An oral examination should be accomplished in the following sequence :
visual examination,
pain relief and temporary restorations,radiographs,
evaluation of abutment and periodontium,
vitality tests of individual teeth,
determination of the floor of the mouth position,
Oral prophylaxis and impressions of each arch.
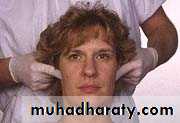
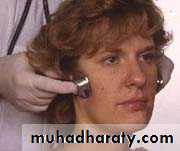
Extra oral examination
This includes : extra oral and intra oral examination.TMJ - tenderness, mouth opening deviation & clicking
Intraoral examination
No of teeth present with their clinical evaluationMalposed teeth
Carious teeth
Existing restoration- sensitivity to percussion
Periodontium
Residual ridges
Saliva
Investing structures
Occlusion and occlusal plane
Oral hygiene index
Pain relief and temporary restorations
to determine the need and management of acute needs and whether a prophylaxis is required to conduct a thorough oral examination.to relieve discomfort arising from tooth defects
the extent of caries and arrest further caries activity
Radiographs
areas of infection and other pathologiesthe presence of root fragments, foreign objects, bone spicules and irregular ridge formations
the presence and extent of caries and the relation of carious lesions to the pulp and periodontal attachment
evaluation of existing restorations : evidence of recurrent caries, marginal leakage, and overhanging gingival margins
the presence of root canal fillings
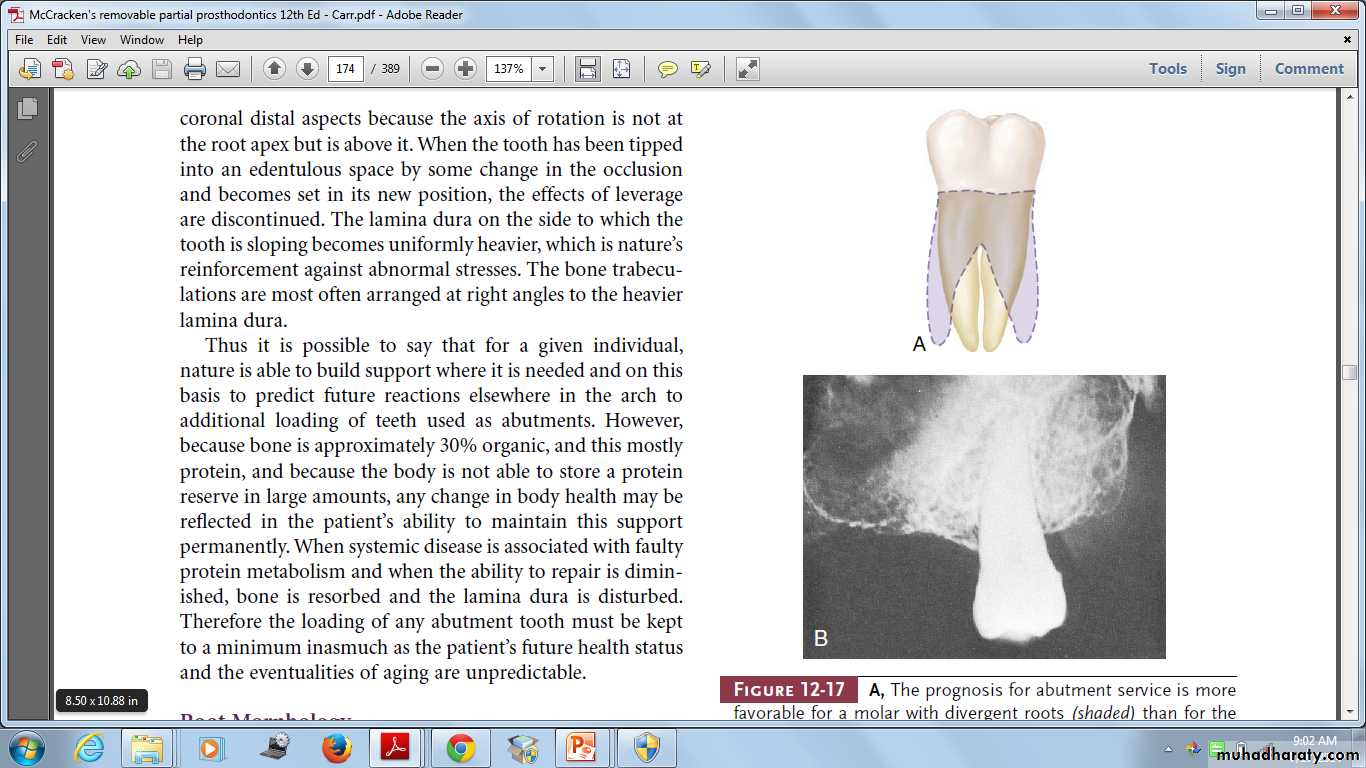
evaluation of periodontal conditions presentto evaluate the alveolar support of abutment teeth, their number, the supporting length and morphology of their roots
the relative amount of alveolar bone loss suffered through pathogenic processes, and the amount of alveolar support remaining
Determination of the floor of the mouth position
To locate inferior borders of lingual mandibular major connectors.Oral prophylaxis & Impression
oral hygiene status before prosthodontic treatment is important.
The impression for the diagnostic cast is usually made with an irreversible hydrocolloid in a stock (perforated or rim lock) impression tray.
Evaluation of abutment
• Anatomic consideration
- Root length, size and form• vitality tests
• caries evaluation
• Periodontal health
• Malpositions
• Analysis of Occlusal Factors
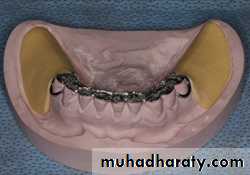
Diagnostic cast
• Supplements oral examination• Permit a topographic survey of the dental arch
• Patient education and motivation
• Custom tray fabrication
• Constant reference
• Patient's record
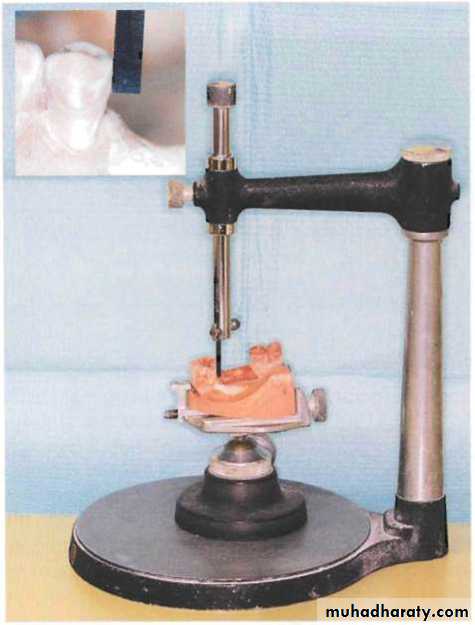
Surveying of the cast
verification of appropriate mouth modifications for a removable partial denture.To determine the most desirable path of placement that will eliminate or minimize interference to placement and removal
To locate and measure areas of the teeth that may be used for retention
To determine whether tooth and bony areas of interference will need to be eliminated surgically or by selecting a different path of placement
To determine the most suitable path of placement that will permit locating retainers and artificial teeth to the best esthetic advantage.
To permit an accurate charting of the mouth preparation to be made including the preparation of proximal tooth surfaces to provide guiding
Mounting of diagnostic cast
• Occlusal plane & relationships• Abutment tooth contours
• Rest seat areas
• Interarch space
• Residual ridge relation
• Tissue contours
Part II
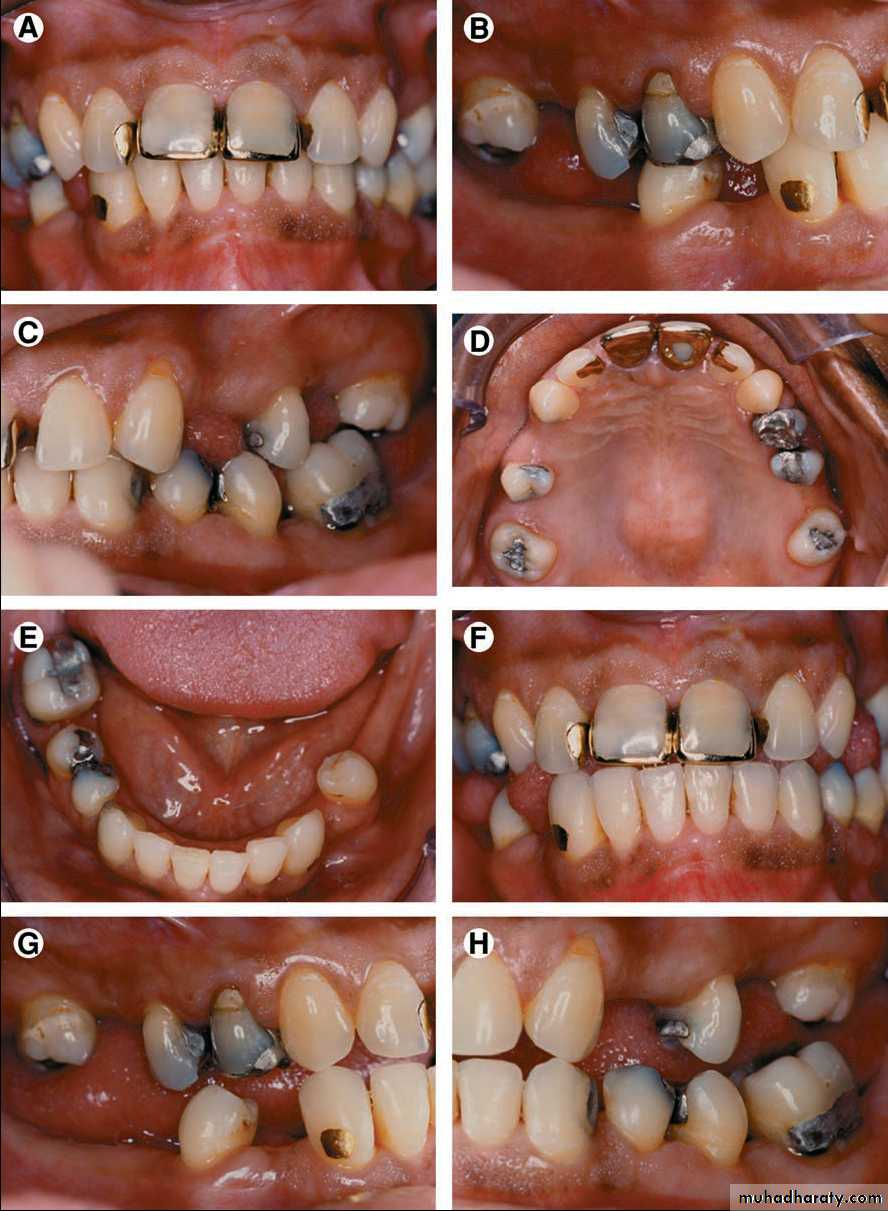
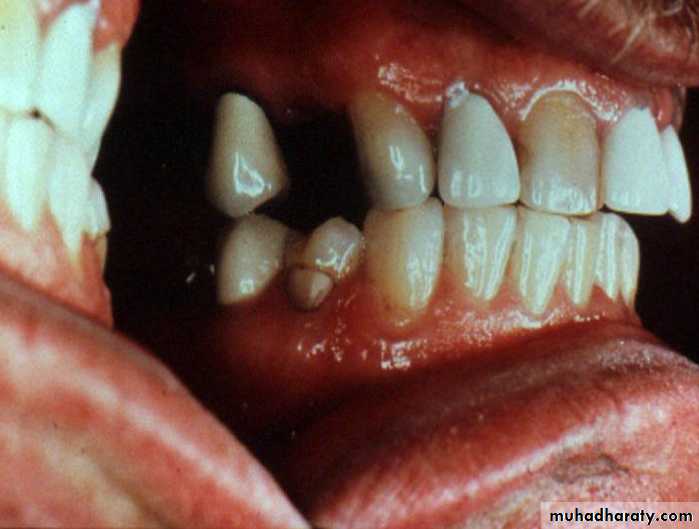
Traumatic Vertical overlap
The objectives of any prosthodontic treatment may be stated as follows:
the elimination of diseasethe preservation, restoration, and maintenance of the health of the remaining teeth and oral tissues
the selected replacement of lost teeth; for the purpose of restoration of function
comfort and in esthetically pleasing manner
Treatment planning
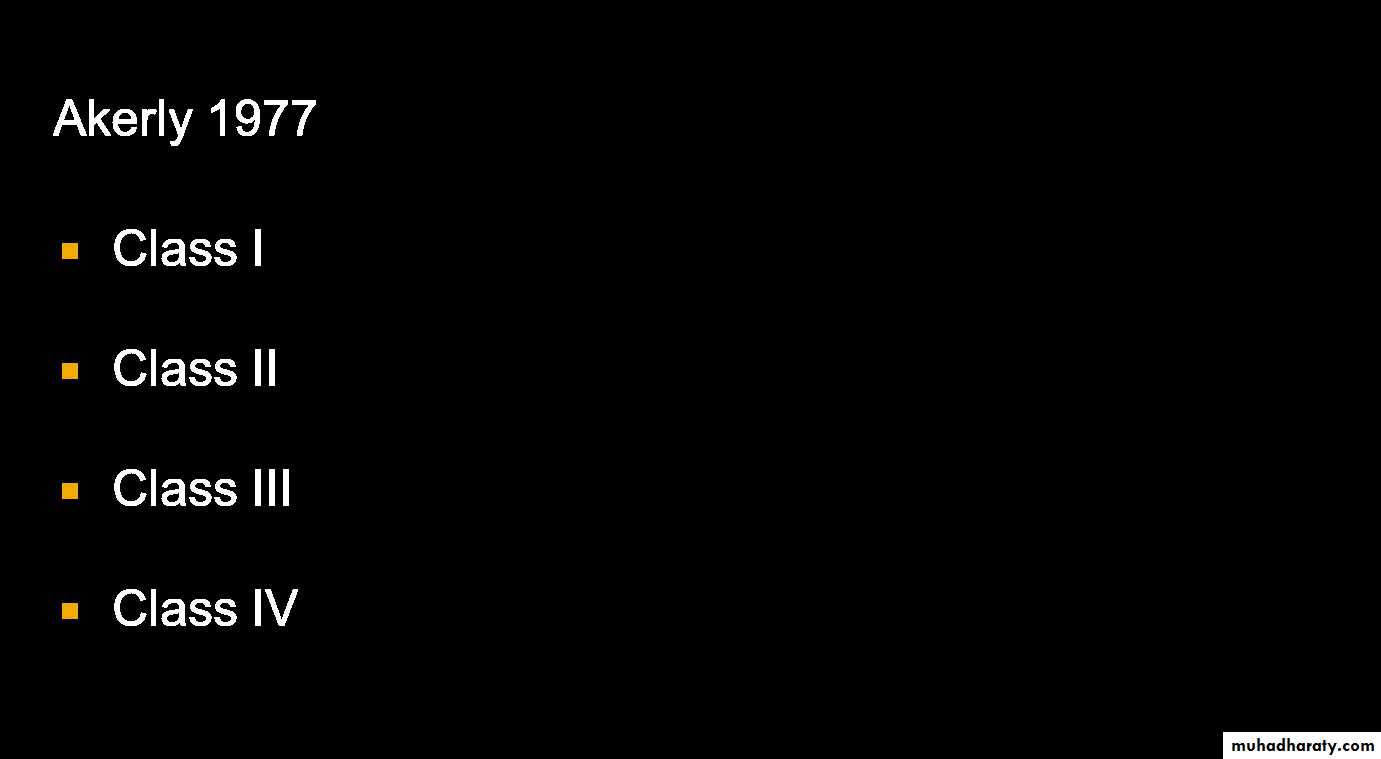
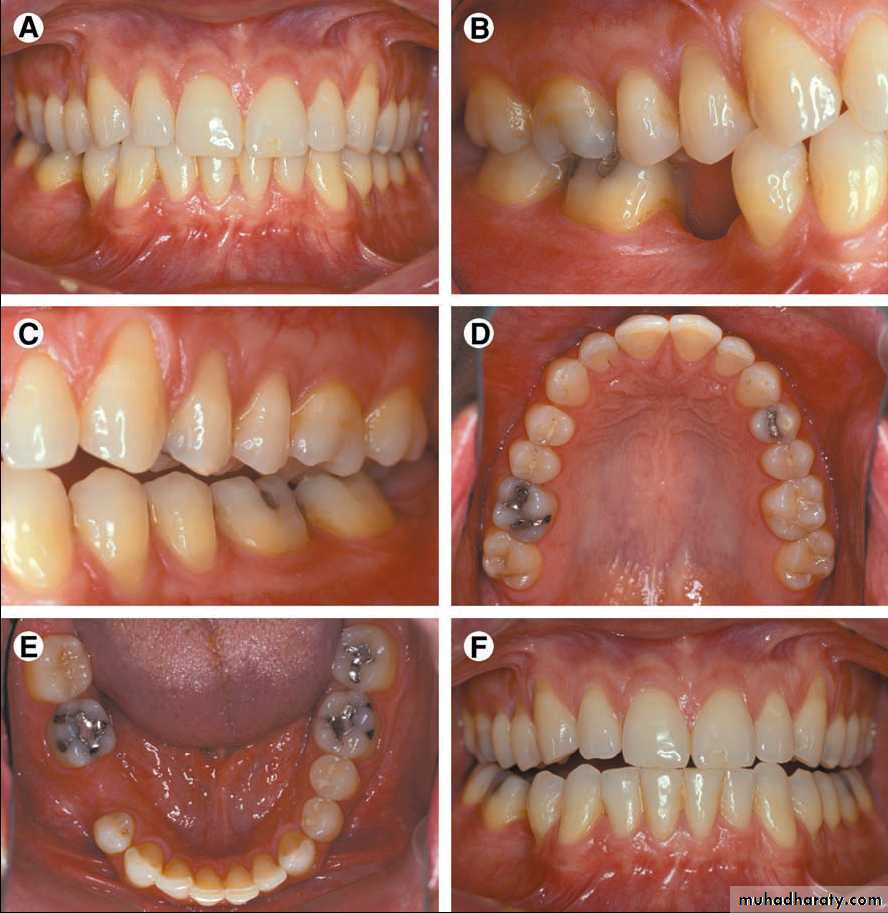
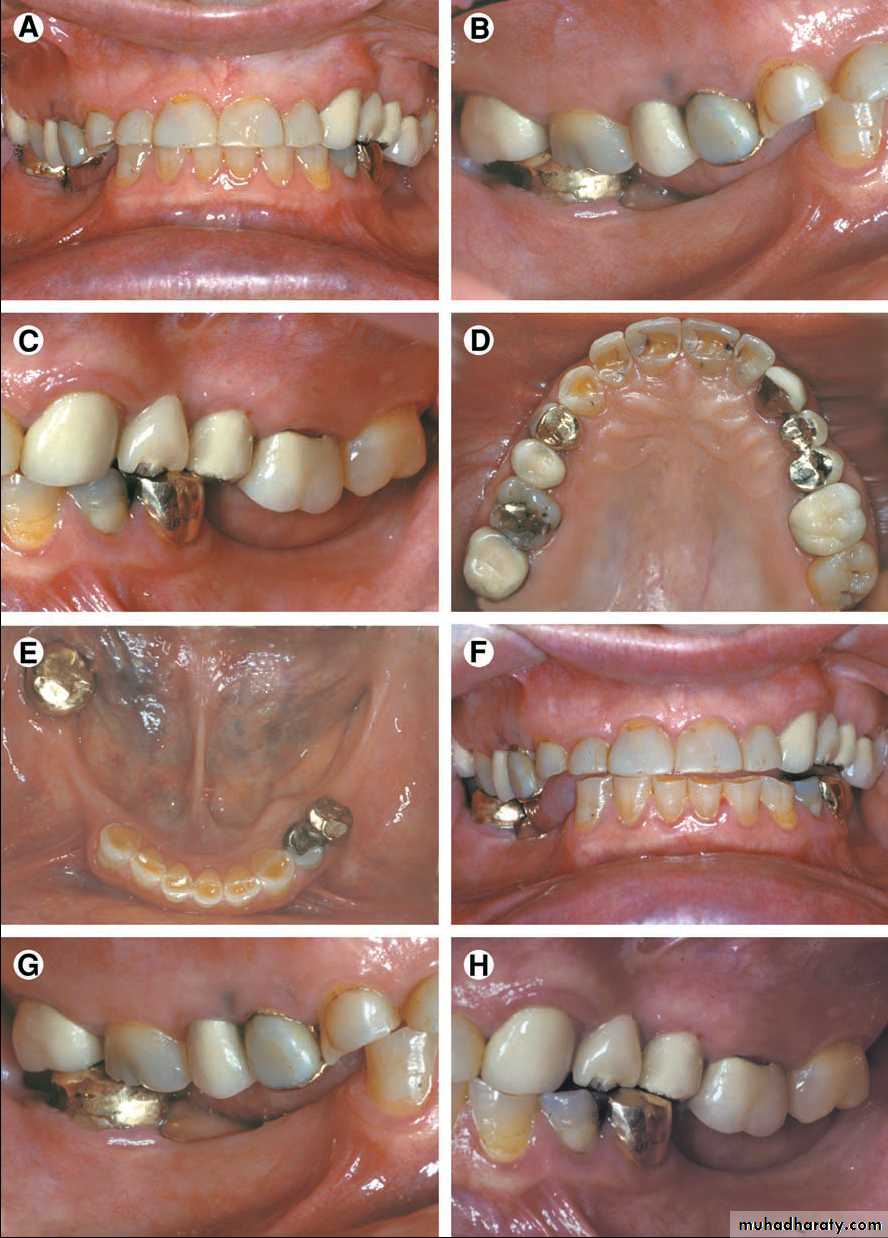
Prosthodontic Diagnostic Index ( PDI )
Based on diagnostic findings, The American College of Prosthodontists (ACP) has developed a classification system for partial edentulismCriteria 1: Location and extent of the edentulous area(s)
Criteria 2: Abutment conditionsCriteria 3: Occlusion
Criteria 4: Residual ridge
Class I
Edentulous area confined to a single archAbutment conditions -No preprosthetic therapy is indicated
Occlusal characteristics- Class I molar jaw relationships are seen
Residual bone height of ≥21 mm
Class II
Edentulous area – Both archesAbutment- Abutments in 1 or 2 sextants have less tooth structure or support intra or extra coronal restorations
Occlusion- Localized adjunctive therapy Class I molar and jaw relationships are seen
Residual bone height of 16 to 20 mmClass III
Any posterior maxillary or mandibular edentulous area greater than 3 teeth or 2 molars. Any edentulous areas including anterior and posterior areas of 3 or more teeth.Abutments in 3 sextants have insufficient tooth structure to retain or support intracoronal or extracoronal restorations.
Entire occlusion must be reestablished. Class II molar and jaw relationships are seen.
Residual alveolar bone height of 11 to 15 mmClass IV
Any edentulous area or combination of edentulous areas requiring a high level of patient complianceAbutments in 4 or more sextants have insufficient tooth structure to retain or support intracoronal or extracoronal restorations.
Entire occlusion must be reestablished, including changes in the occlusal vertical dimension. Class II div 2 and Class III molar and jaw relationships are seen.
Residual vertical bone height of ≤10 mm
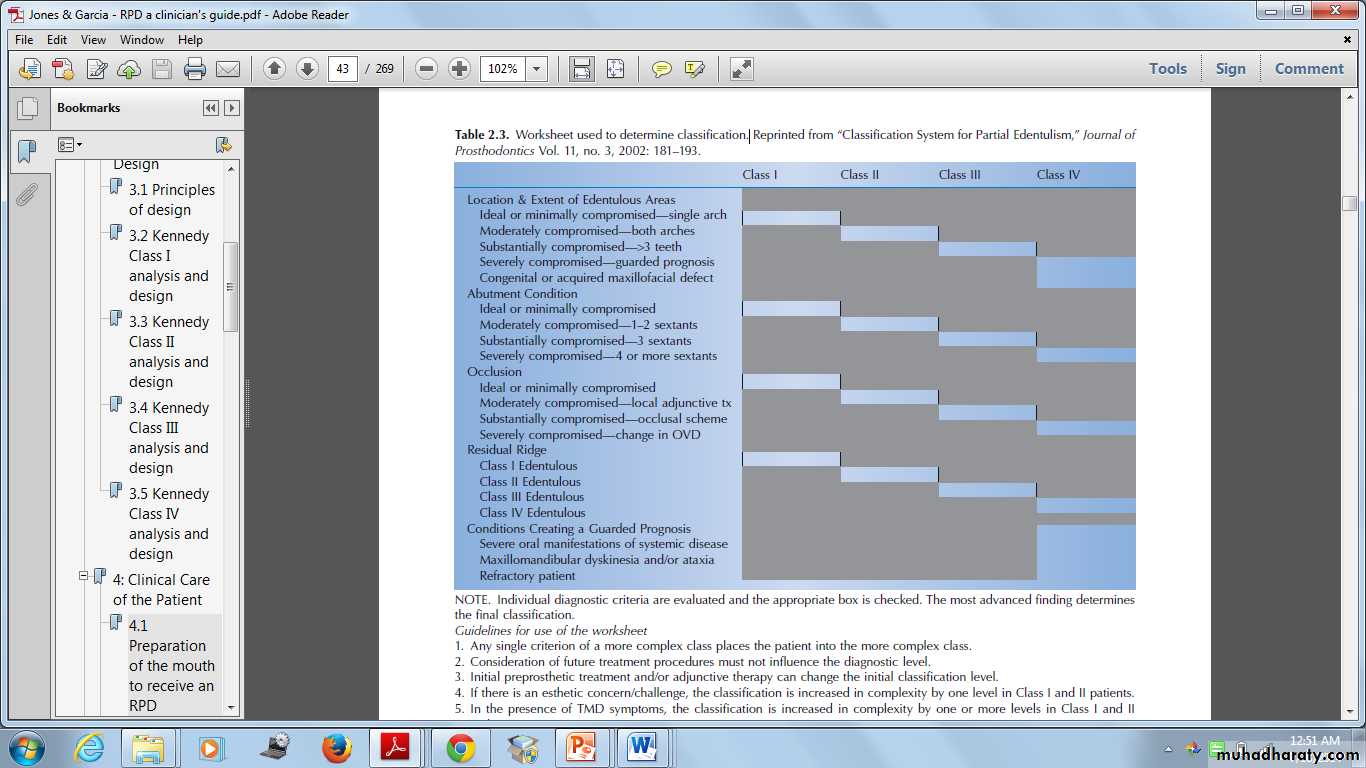
Worksheet used to determine classification
Individual diagnostic criteria are evaluated and the appropriate box is checked. The most advanced finding determines the final classificationClassification System for Partial Edentulism, Journal of Prosthodontics Vol. 11, no. 3, 2002: 181 – 193.
Guidelines for use of the worksheet
1. Any single criterion of a more complex class places the patient into the more complex class.2. Consideration of future treatment procedures must not influence the diagnostic level.
3. Initial preprosthetic treatment and/or adjunctive therapy can change the initial classification level.• 4. If there is an esthetic concern/challenge, the classification is increased in complexity by one level in Class I and II patients.
• 5. In the presence of TMD symptoms, the classification is increased in complexity by one or more levels in Class I and II patients.
• 6. In the situation where the patient presents with an edentulous mandible opposing a partially edentulous or dentate maxilla, Class IV.
Prosthodontic treatment choices
• Implant supported fixed dental prosthesis• Fixed dental prosthesis
• Removable partial denture
• Complete denture
• Combination of the above
• No treatment at all
Indications for removable partial dentures
Distal extension situations
After recent extractions
Long span
Need for cross-arch stabilization
Excessive loss of residual bone
Sound abutment teeth
Abutment with guarded prognosis
Economic considerations
Shared Decision Making
It is a communication modela process where the provider and the patient identify together the best course of care.
it addresses the need to fully inform patients about risks and benefits of care optionsensures that patient values and preferences play a prominent role in the process.
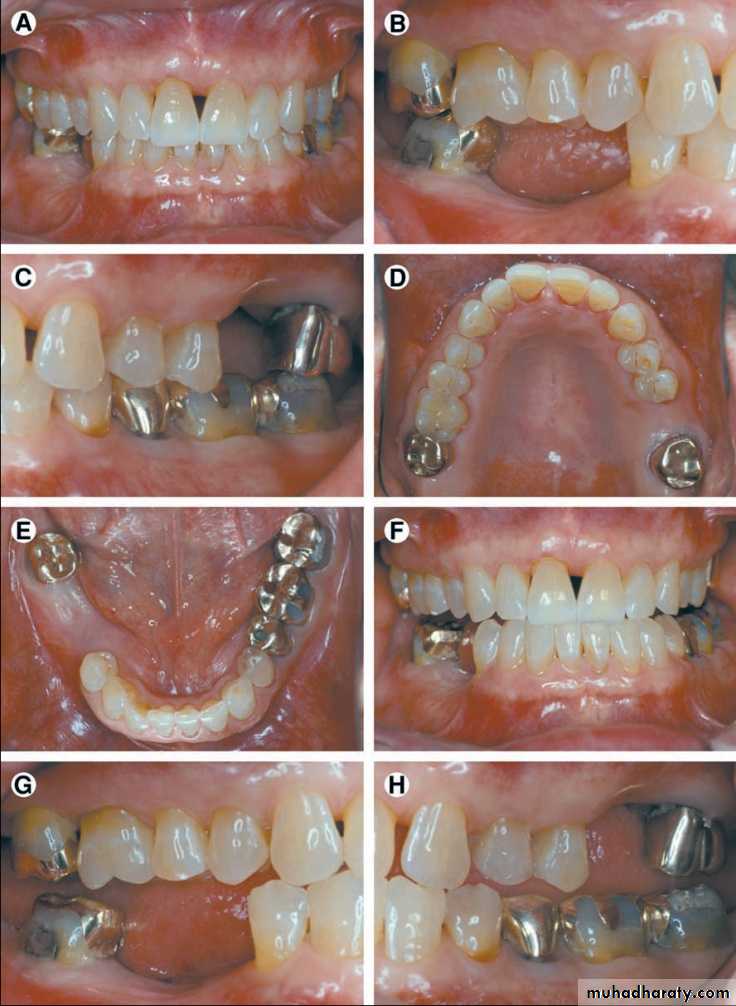
Prosthodontic treatment choices in RPDsComputer-designed polycarbonate RPD framework.
Digital partial design and manufacturing: using 3D printing technology to fabricate RPD frameworks
Valplast RPDs with anterior flexible nylon clasps.
A cast metal framework with metal clasps and flexible nylon polyamide retentive clasps
Bohnenkamp DM Removable Partial Dentures : Clinical Concepts, Dent Clin N Am 2014; 58: 69–89
Mandibular overlay unilateral distal extension RPD with tooth-colored acrylic resin processed to the metal framework
Mandibular overlay RPD metal framework
Bohnenkamp DM Removable Partial Dentures : Clinical Concepts, Dent Clin N Am 2014; 58: 69–89
Implants and RPDs
Minimize rotation about an axis in a Kennedy Class I or II arch, or any long modification spandirect retainers
restsDevelopment of treatment plan
Phase ICollection and evaluation of data
Pain, infection control
Biopsy
Patient motivation
Phase II
Removal of deep caries
Extirpation of necrotic pulp
Extraction of non-retainable teeth
Periodontal treatment
Interim prosthesis
Occlusal equilibrium
Patient education
Phase III
• Preprosthetic surgical procedures• Definitive endodontic procedures
• Definitive restoration of teeth
• Fixed partial denture construction
• Reinforcement of education and motivation of the patient
• Phase IV
• Construction of removable partial denture• Reinforcement of education and motivation of patient
• Phase V
• Post insertion care• Periodic recall
• Reinforcement of education and motivation of patient.
SOAP summary
The four components of a SOAP note are Subjective, Objective, Assessment, and Plan
The SOAP note format is used to standardize medical evaluation entries made in clinical records. The SOAP note is written to facilitate improved communication among all involved in caring for the patient and to display the assessment, problems and plans in an organized format.
Importance of a Written Treatment Plan
Plan the amount of time and appointment scheduleProvides information to the patient.
Estimate the professional fees for the treatment.
Coordinate the schedule for dental laboratory procedures
Meet the legal requirements of informed consent
Conclusion
References• Carr AB, Brown DT, McCracken’s Removable Partial Prosthodontics, 12th edition, Canada, Elsevier Publishers, 2011, pp:150-184
• Stewart, Rudd, Kuebkar, Clinical Removable Partial Prosthodontics, 2nd edition, India, All India Publishers and Distributors, 2001, pp:117-220
• Jones DJ,Gracia LT, Removable Partial Dentures : A Clinician’s guide, 1st edition, Singapore, Wiley-Blackwell, 2009, pp : 11-38
• Garry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR, Koumjian JH, Arbree NS, Classification system for partial edentulism, J Prosthodont 2002;11,3:181-193
• McCord JF, Grey JA, Winstanley RB, Johnson A, A Clinical Overview of Removable Prostheses: 1. Factors to Consider in Planning a Removable Partial Denture, Dent Update 2002; 29: 376-381
• Bohnenkamp DM Removable Partial Dentures : Clinical Concepts, Dent Clin N Am 2014; 58: 69–89
• Gamer et al, M. M. House mental classification revisited: Intersection of particular patient types and particular dentist’s needs, J Prosthet Dent 2003;89:297-302
• Davenport JC, Basker RM, Heath JR, Ralph JP, Glantz PO, The removable partial denture equation, Brit Dent J 2000; 189: 414–424