١
Fifth stage
Pediatrics
Lec-
د
.
أ
ﺛل
29/2/2017
Management of DM1
Aims of treatment:
To maintain a balance between tight glucose control and avoiding
hypoglycemia.
To eliminate polyuria and nocturia.
To prevent ketoacidosis.
To permit normal growth and development with minimal effect on lifestyle.
Minimize the risk of long-term microvascular & macrovascular
complications.
Constituents of Treatment:
Basic Education:
Education is fundamental to diabetes management & metabolic control. Teaching about
diabetes is best handled by a diabetes management team, including a physician, nurse,
educator, dietitian, & mental health professional.
The family of diabetic patient must be taught the following basic of treatment:
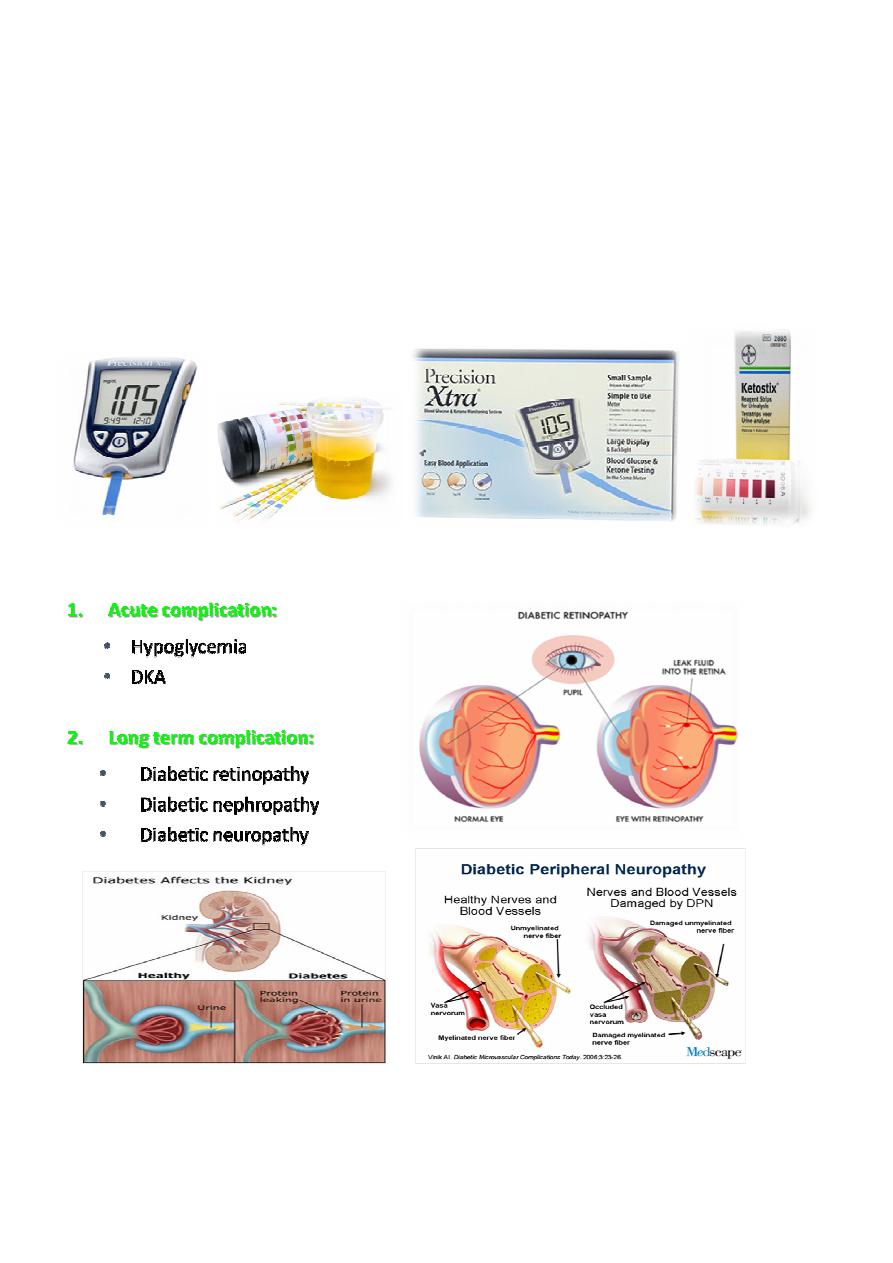
1. monitoring the child's blood glucose and urine ketones.
2. preparing and injecting the correct insulin dose subcutaneously at the proper
time.
3. recognizing and treating low blood glucose reactions.
4. having a basic meal plan.
٢
Insulin Therapy:
The dose of insulin needed over 24 hours varies according to the pubertal
development of the patient:
Prepubertal 0.7U/kg/day
Mid puberty 1 U /kg/day
Late puberty 1.2U/kg/day
At time of the diagnosis of diabetes, patient have some residual B-cells, thus, there is
o en a temporary decrease in insulin requirements 1-3 months a er diagnosis (the
honey moon period) & this period may last in some cases up to 12 months or more.
In this period, is needed about 60-70% of the full replacement dose based on
pubertal status.
The optimal insulin dose can only be determined empirically, with frequent self-
monitored blood glucose levels & insulin adjustment by the diabetes team.
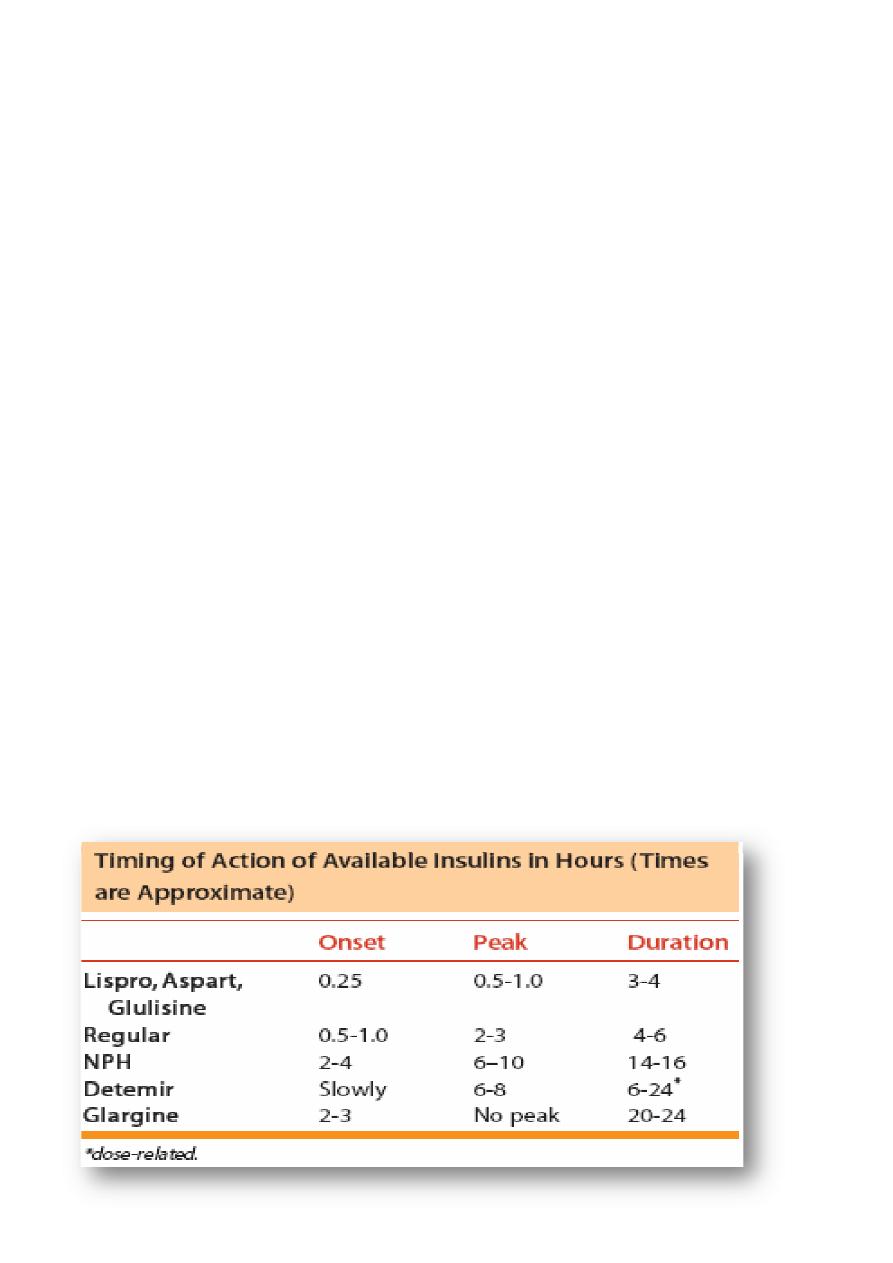
Types of insulin:
Recombinant DNA technology is used to manufacture all currently available types of insulin
and based on the amino acid sequence of human insulin.
1. Rapid acting insulin: e.g. lispro, aspart.
2. Short acting insulin: e.g. regular
3. Intermediate acting insulin: e.g. NPH, detemir, lente
4. Long acting insulin: detemir, glargine
5. Several different mixes are available which combine different percent of short or
rapid acting insulin with intermediate acting insulin e.g. mixtard.
*Detemir can be cosidered either intermediate or long acting, its time of action is dose related.
٣
Insulin Regimens:
I.
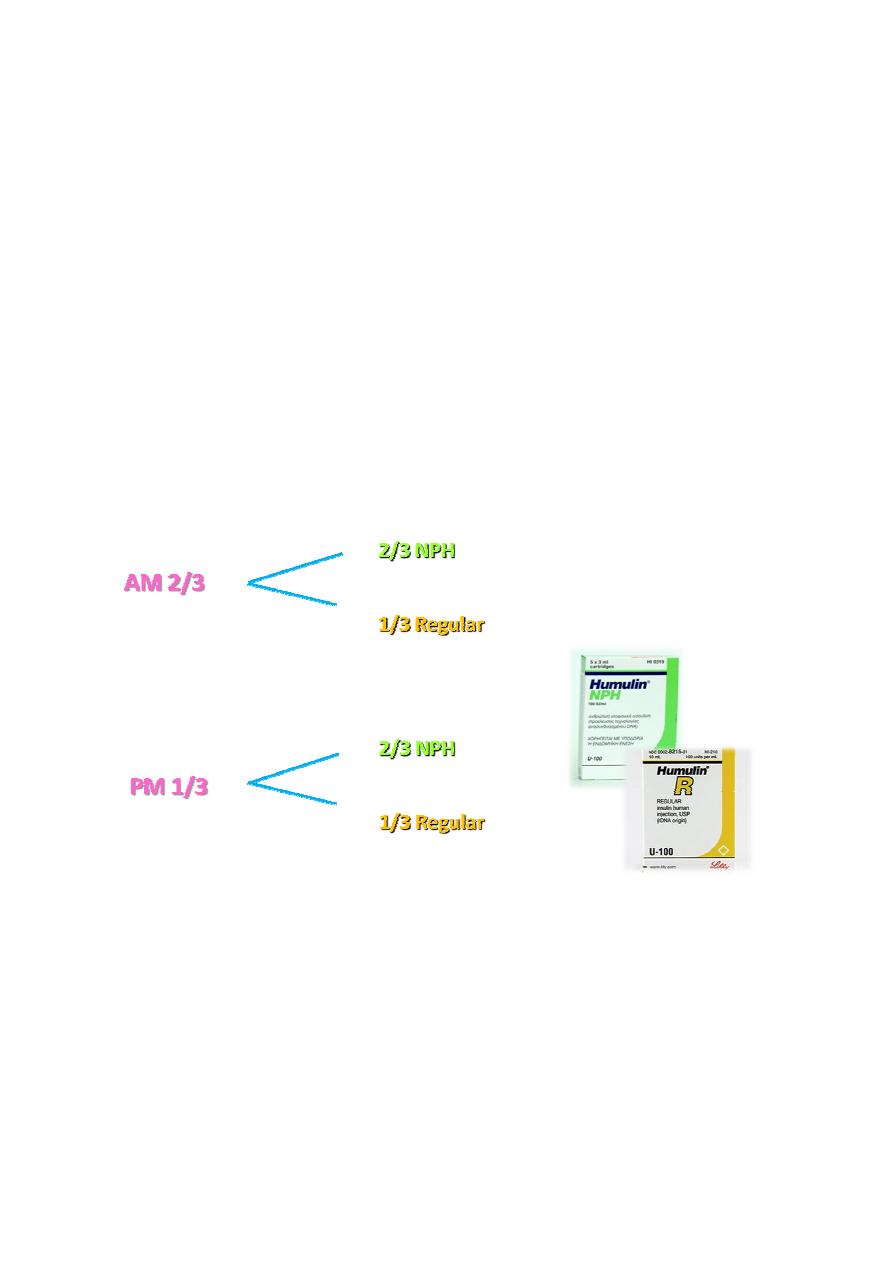
NPH-based regimen:
two doses of NPH are given, per day: one in the morning shortly before breakfast &
2
nd
in the evening, either at dinner or at bed time. Then either regular or rapid acting
insulin is given at breakfast and dinner.
This regimen may use NPH and regular together at breakfast and again at dinner.
The total daily dose is split into two shots and each shot is a mix of NPH and regular
which may be given in the same syringe. With one variation, the evening dose is
divided so regular insulin is given at dinner & NPH at bedtime. This allows the NPH to
last until morning.
The use of rapid acting insulin decrease the problem of between- meal insulin peaks
when regular is used.
The Intermediate acting 70% of the dose & the short or rapid acting 30%.
٤
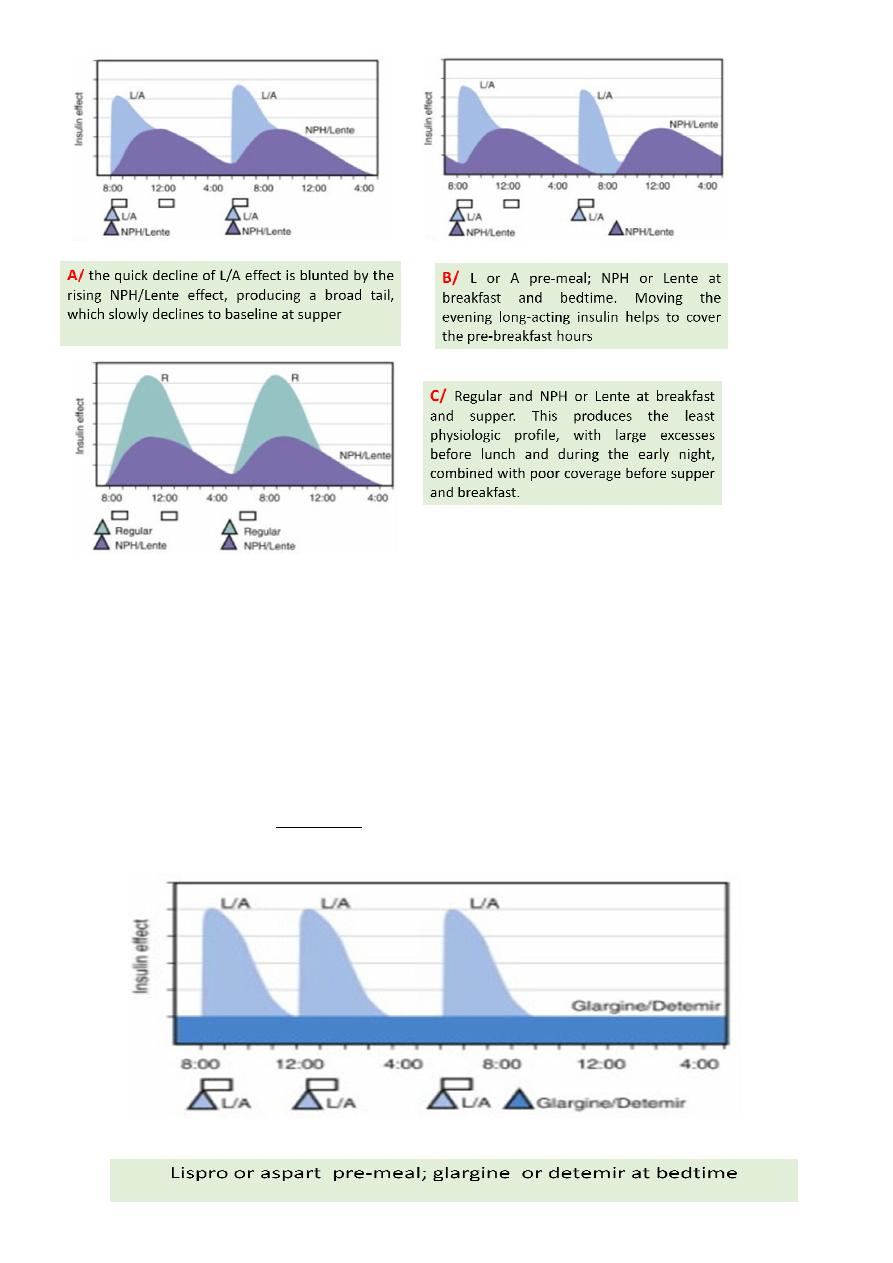
II. Basal/bolus regimens:
The basal insulin component provides baseline, between meals, or fasting insulin
needs.
The bolus component provides insulin to cover food requirements & to correct
hyperglycemia.
The basal component may be provided by either rapid acting insulin given by the
basal rate using an insulin pump, or with once or twice daily injection of detemir or
glargine.
detemir or glargine cannot be mixed with any other insulin.
Usual basal requirments are about 50% of the total daily insulin requirements.

٥
III. Inhaled insulin regimen:
Premeal inhaled insulin combined with once daily long acting insulin at bed time
giving a promising result.
How inject insulin
Insulin may be injected into the subcutaneous tissue of the upper arm, the anterior
and lateral aspects of the thigh, the buttocks and the abdomen.
Rotation of the injection sites is essential to prevent lipohypertrophy or, more rarely,
lipoatrophy.
The skin should be pinched up and the insulin injected be er at a 45° angle in young
child to avoid injection of insulin in muscle.
Using a long needle or an injection technique that is 'too vertical' causes a painful,
bruised intramuscular injection. Shallow intra-dermal injections can also cause
scarring and should be avoided

٦
Nutritional Management:
It is important for children and adolescents with type 1 diabetes to have a
nutritionally balanced diet with adequate calories and nutrients for normal growth.
The caloric mixture should comprise approximately:
• 55% carbohydrate.
• 30% fat.
• 15% protein.
The total daily caloric intake is divided to provide:
• 20% at breakfast.
• 20% at lunch.
• 30% at dinner.
• 10% for each of the midmorning, mida ernoon, and evening snacks, if they
are desired. In older children, the midmorning snack may be omitted and its
caloric equivalent added to lunch.
• Approximately 70% of the carbohydrate content should be derived from
complex carbohydrates such as starch; intake of sucrose and highly refined
sugars should be limited.
• Diets with high fiber content are useful in improving control of blood glucose.
• High-protein intakes may contribute to diabetic nephropathy.

٧
Exercise:
Physical fitness and regular exercise are to be encouraged in all children with type 1
diabetes.
Regular exercise improves glycemic control through
increased utilization of glucose by muscles.
increased rate of absorption of insulin from its injection site.
increasing insulin receptor number.
In patients who are in poor metabolic control, vigorous exercise may precipitate
ketoacidosis because of the exercise-induced increase in the counter-regulatory
hormones.
No form of exercise, including competitive sports, should be forbidden to the
diabetic child. But in order to avoid hypoglycemia that may develop during or after
exercise, an additional carbohydrate exchange should be taken before exercise & a
source of glucose like juice, sweets or candy should be available during & after the
exercise.
An appropriate regimen for regularly planned exercise that is frequently associated
with hypoglycemia as follow:
The total dose of insulin may be reduced by about 10-15% on the day of the
scheduled exercise.
Prolonged exercise, such as long-distance running, may require reduction of as
much as 50% or more of the usual insulin dose.
Monitoring
More frequent monitoring of blood glucose has been shown to correlate with
improved glycemic control.
Blood glucose traditionally is monitored before meals, at bedtime, and overnight.
Ideally, the blood glucose concentration should range from approximately 80 mg/dL
in the fas ng state to 140 mg/dL after meals.
Any significant elevation of blood glucose level above the upper limit of the range or
bellow the lower limit mandates changing the corresponding dose of insulin by 10-
15% accordingly.

٨
In the NPH based regimen:
Fasting blood glucose--- corresponds to the NPH insulin of the night dose.
Noon blood glucose --- corresponds to the regular insulin of the morning.
Presupper blood glucose --- corresponds to the NPH of the morning.
Prebed time glucose --- corresponds to the regular insulin of the night.
A continuous glucose monitoring system (CGMS) records data obtained from a
subcutaneous sensor every 5 min for up to 72 hr and provides the clinician with a
continuous profile of tissue glucose levels. The interstitial glucose levels lag 13 min
behind the blood glucose values at any given level.
Glucowatch Biographer also measure interstitial glucose through a patch of
membrane applied on the forearm. It provides real time interstitial fluid glucose
values
Measurement of Glycated hemoglobin (HbA1c):
HbA
1c
measurement reflects the average blood glucose concentration from the
preceding 2-3 mo.
It is recommended that HbA
1c
measurements be obtained 3-4 mes per yr to obtain
a profile of long-term glycemic control.
The HbA
1c
frac on is usually less than 6%; in diabe cs,
Values of 6-7.9% represent good metabolic control.
Values of 8.0-9.9%, fair control.
Values of 10% or higher, poor control.
٩
Urine or blood ketones also should be monitored when:
The blood glucose levels are elevated (eg, above250 mg/dL).
Children have a fever.
They feel nauseous or are vomiting.
When they are not feeling well.
This monitoring is important in achieving the goal of aborting DKA episodes by treating
early ketosis.
Complica ons of DM1
٠١
Hypoglycemia
Hypoglycemia is a major proplem of diabetic children on insulin therapy. It has
serious neurocognitive backdraws especially in the young children.
Most children with T1DM can expect:
mild hypoglycemia each week.
moderate hypoglycemia a few times each year.
severe hypoglycemia every few years.
Clinical Features:
Manifestation due to surge in catecholamines:
pallor, sweating, apprehension or fussiness, irritability, hunger, tremor, and tachycardia.
Manifestation due to cerebral glucopenia:
moderate hypoglycemia: drowsiness, personality changes, mental confusion,
and impaired judgment .
severe hypoglycemia: inability to seek help and seizures or coma. Prolonged
severe hypoglycemia can result in a depressed sensorium or stroke like focal
motor deficits that persist after the hypoglycemia has resolved.
Treatment:
The child & the family members should aware about the manifestations of
hypoglycemia & how to confirm it by measuring blood glucose level.
A source of emergency glucose should be available at all times and places, including
at school and during visits to friends. 5-10 g should be given as juice or a sugar-
containing carbonated beverage or candy, and the blood glucose checked 15-20
minutes later.
Patients, parents, and teachers should also be instructed in the administration of
glucagon when the child cannot take glucose orally. An injection kit should be kept at
home and school. The intramuscular dose is 0.5 mg if the child weighs ˂20 kg and 1
The patient is then taken to hospital if necessary to be given IV glucose.
M.R
