١
Fifth stage
Ophthalmology
Chapter-14
د
.
ﻧزار
3/4/2017
The
visual
pathway
INTRODUCTION
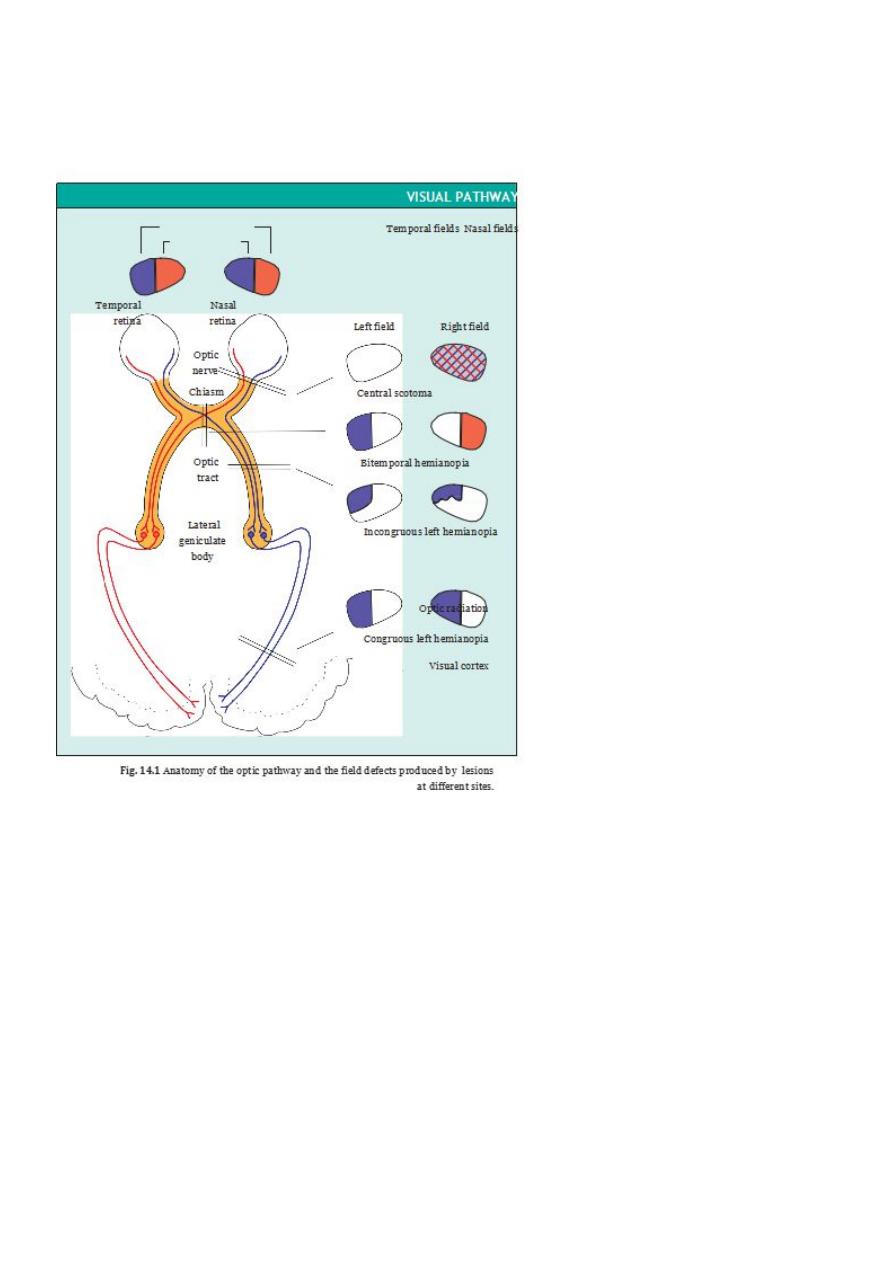
The innermost layer of the retina consists of the nerve fibres originating from its ganglion
cells .These fibres collect together at the optic nerve head, and form the optic nerve
Diagnosis and location of disease of the optic pathways is greatly aided by the differing
field defects produced, as Fig. 14.1 shows.
THE OPTIC NERVE
The normal optic nerve head has distinct margins ،a pinkish rim and usually a white
central cup .The central retinal artery and vein enter the globe slightly nasally in the optic
nerve head .
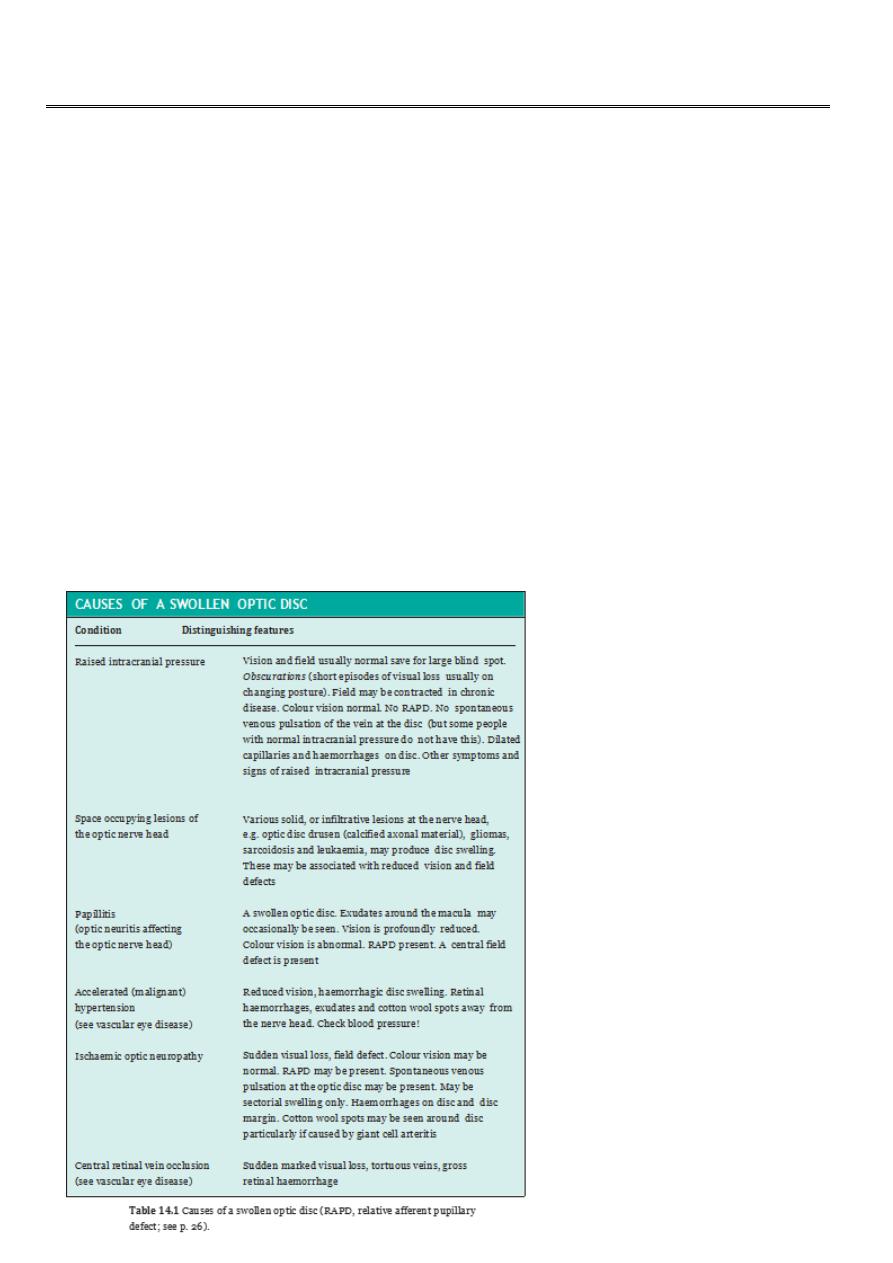
The swollen optic disc
The swollen disc is an important and often worrying sign.1- Papilloedema
is the term
given to disc swelling associated with raised intracranial pressure ،2-accelerated
hypertension and 3- optic disc ischaemia .4- Optic neuritis affecting the nerve head
)papillitis (has a similar appearance .

٢
Note also that myelinated nerve fibres (a normal variant where the nor- mally
unmyelinated retinal nerve fibre layer is partly myelinated giving it a white appearance)
may be mistaken for optic disc swelling. A high myope may also have an optic disc
surrounded by an atrophic area (peripapillary atrophy) that may be confused with disc
swelling.
Papilloedema due to raised intracranial pressure :
HISTORY
The crucial feature of disc swelling due to raised intracranial pressure is that there is no
acute prolonged visual loss. Some patients may develop fleeting visual loss lasting
seconds when they alter posture (obscurations of vision). Other features of raised
intracranial pressure may be present including:
headache, worse on waking and made worse by coughing;
nausea, retching;
diplopia (double vision) usually due to a sixth nerve palsy;
neurological symptoms, if the raised pressure is due to a cranial space-occupying
lesion;
a history of head trauma suggesting a subdural haemorrhage.
SIGNS
The optic disc is swollen, the edges blurred and the superficial capillaries are dilated
and thus abnormally prominent. There is no spontaneous venous pulsation of the
central re nal vein (5–20% of those with normal nerve heads have no spontaneous
pulsation, however).
A large blind spot will be found on visual field testing corresponding to the swollen
nerve head. In chronic papilloedema the field may become constricted. A field
defect may, how-ever, be caused by the space-occupying lesion causing the
papilloedema.
Abnormal neurological signs may indicate the site of a space-occupying lesion.
INVESTIGATION
CT and MRI scanning will identify any space-occupying lesion or enlargement of the
ventricles. Following neurological consultation (and normally after a scan) a lumbar
puncture will enable intracranial pressure to be measured.
TREATMENT
Intracranial pressure may be elevated and disc swelling present with no evidence of
intracranial abnormality and no dilation of the ventricles on the scan.This is termed benign
intracranial hypertension and usually presents in overweight women in the second and
third decade. Patients complain of headache and may have obscurations of vision and sixth

٣
nerve palsies. No other neurological problems are present. Although acute permanent
visual loss is not a feature of papilloedema, if the nerve remains swollen for several weeks
there will be a progressive contraction of the visual field. It is thus important to reduce
intracranial pressure. This may be achieved:
with medications such as oral acetazolamide;
through ventriculoperitoneal shunting;
through optic nerve decompression.
Space-occupying lesions (i.e. tumours and haemorrhage) and hydro- cephalus
require neurosurgical management.
Optic neuritis:
Inflammation or demyelination
(termed papillitis if the optic nerve head is affected and retrobulbar neuritis if the optic
nerve is affected more posteriorly).
HISTORY
There is:
An acute loss of vision
Pain on eye movement in retrobulbar neuritis
A preceding history of viral illness in some cases.
Between 40 and 70% of pa ents with op c neuri s will have or develop other
neurological symptoms to suggest a diagnosis of demyelination (multiple sclerosis).
EXAMINATION
This reveals:
reduced visual acuity;
reduced colour vision;
relative afferent pupillary defect (RAPD)
central scotoma on field testing;
a normal disc in retrobulbar neuritis. A swollen disc in papillitis.
TREATMENT
An MRI scan will help to identify additional ‘silent’ plaques of demyelination but the
patient must be suitably counselled before a scan is performed. There may be a role
for steroid treatment to speed up visual recovery.
Ischaemic optic neuropathy :
PATHOGENESIS
The anterior optic nerve may become ischaemic if the posterior ciliary vessels are
compromised as a result of degenerative or vasculitic disease of the (see p. 14).This
results in an anterior
ischaemic
optic
neuropathy .

٤
SYMPTOMS
sudden loss of vision or visual field ،often on waking since vascular perfusion is
decreased during sleep .
If accompanied by pain or scalp tenderness (jaw claudication,shoulder pain,malaise) ,the
diagnosis of giant
cell arteritis
must never be forgotten
SIGNS
There is usually :
• A reduction in visual acuity .
• A field defect ،typically an absence of the lower half of the visual field .
• A swollen and haemorrhagic disc with normal retina and retinal vessels
In arteritic ischaemic optic neuropathy the disc may be pale .
• A small fellow disc with a small cup in non-arteritic disease .
• A tender temporal artery ،a sign suggestive of giant cell arteritis .
INVESTIGATIONS
If giant cell arteritis is present the ESR and C-reactive protein are usually grossly
elevated(although 1 in 10 pa ents with giant cell arteri s have a normal ESR).Temporal
artery biopsy is often helpful but again may not lead to a diagnosis ،particularly if only a
small specimen is examined ،because the disease may skip a length of the artery .Giant
cell arteritis can also present as a central retinal artery occlusion when the vessel is
affected secondary to arteritis of the ophthalmic artery .
Investigation of the patient with non-arteritic ischaemic optic neuropathy includes :
• a full blood count to exclude anaemia ؛
• blood pressure check ؛
• blood sugar check ؛
• ESR and C-reactive protein to check for giant cell arteritis .
Both hypertension and diabetes may be associated with the condition .It may also be
seen in patients suffering acute blood loss ،e.g .haemateme -
sis ،where it may occur
some days after the acute bleed .Hypotensive episodes may also give rise to ischaemic
optic neuropathy .Occasionally clotting disorders or autoimmune disease may cause the
condition.
TREATMENT
If giant cell arteritis is suspected treatment must not be delayed while the diagnosis is
confirmed .High-dose steroids must be given ،intravenously and orally ،and the dose
tapered over the ensuing weeks according to both symptoms and the response of the
ESR or C-reactive protein .The usual precautions must be taken ،as with any patient on
steroids ،to exclude other medical conditions that might be unmasked or made worse by
the (e.g. tuberculosis, diabetes, hypertension and an increased sus-ceptiblity to infection).
٥
Steroids will not reverse the visual loss but should help prevent the fellow eye being
affected .
There is unfortunately no treatment for non-arteritic ischaemic optic neuropathy other
than the diagnosis of underlying conditions .
PROGNOSIS
It is unusual for the vision to get progressively worse in non-arteritic ischaemic optic
neuropathy and the visual outcome both in terms of visual field and acuity is very
variable .Vision does not recover once it has been lost .The second eye may rapidly
become involved in patients with untreated giant cell arteritis .There is also a significant
rate of involvement of the second eye in the non-arteritic form (40–50%).
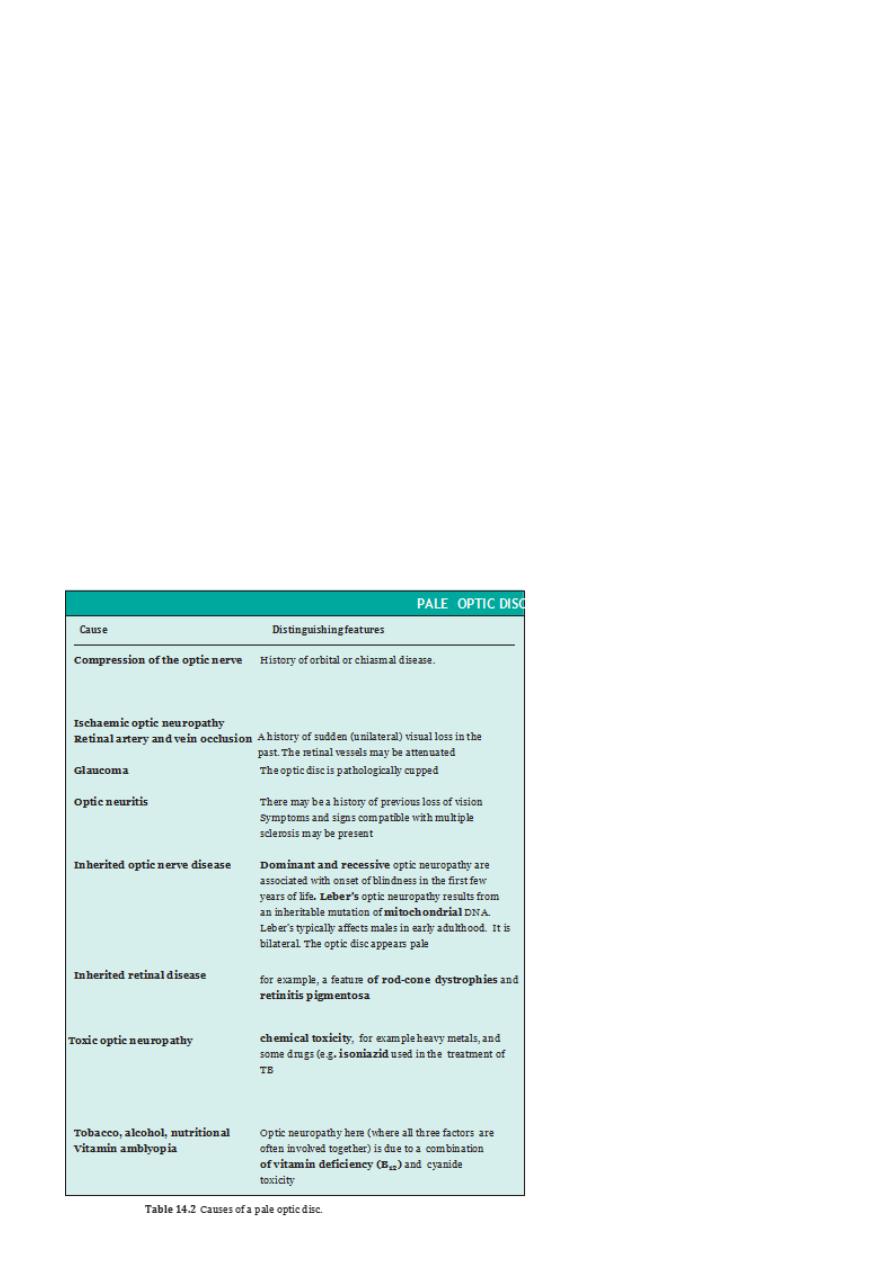
Optic atrophy :
A pale optic disc
The vision is usually reduced and colour vision affected .
The usual vascularity of the disc is lost.
Comparison of the two eyes is of great help.
A relative afferent pupillary defect will also be present .
٦
