THE EAR
Dr. Mohamad S. Aziz
OtolaryngologistCABMS (ORL-HNS)
ENT Dept, College of Medicine, University of Mosul
Undergraduate, The EAR, 2016/2017
3
Facial Nerve and Its Disorders
ANATOMY AND FUNCTIONS OF FACIAL NERVE
Facial nerve is a mixed nerve having motor and a sensory root. The latter is also called the nerve of Wrisberg.
Nucleus of Facial Nerve
Motor nucleus of the nerve is situated in the pons. It receives fibres from the precentral gyrus. The function of forehead is preserved in supranuclear lesions because of bilateral innervation. The emotional movements such as smiling and crying are preserved in supranuclear palsies because of fibres from the thalamus
Course of Facial Nerve
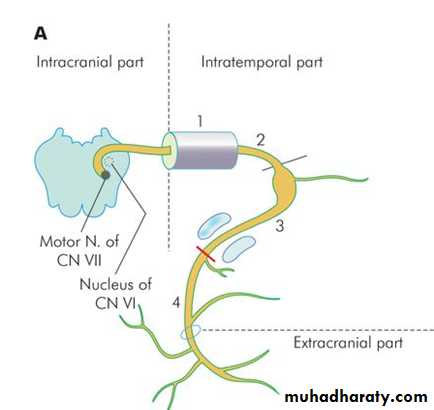
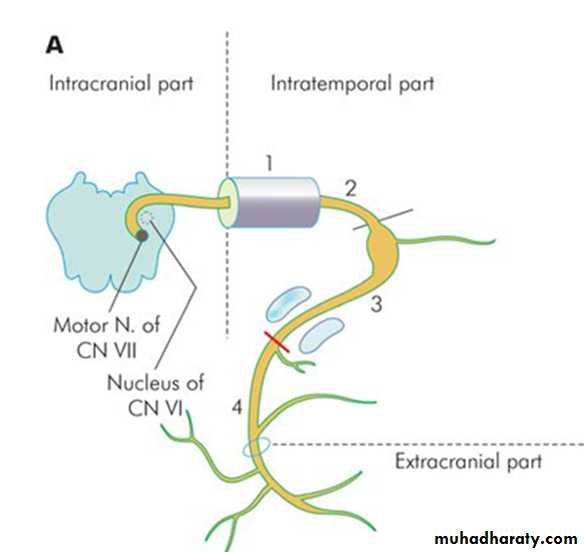
Motor fibres take origin from the nucleus of VIIth nerve, hook round the nucleus of VIth nerve and are joined by the sensory root (nerve of Wrisberg). Facial nerve leaves the brainstem , travels through posterior cranial fossa and enters the internal acoustic meatus. At the fundus of the meatus, the nerve enters the bony facial canal, traverses the temporal bone and comes out of the stylomastoid foramen
4
Course of Facial Nerve
1. Intracranial part: From pons to internal acoustic meatus (15-17 mm).
2. Intratemporal part: From IAM to stylomastoid foramen. It is further divided into: (a) Meatal segment. Within IAM (8-10 mm). (b) Labyrinthine segment. From fundus of meatus to the geniculate ganglion where nerve takes a turn posteriorly forming a "genu“, has the narrowest diameter, the shortest segment-only 4 mm. (c) Tympanic or horizontal segment. From geniculate ganglion to just above the pyramidal eminence, lies above the oval window and below the lateral semicircular canal (11 mm). (d) Mastoid or vertical segment. From the pyramid to stylomastoid foramen. Between the tympanic and mastoid segments is the 2nd genu of the nerve (13 mm).
3. Extracranial part
From stylomastoid foramen to the termination of its peripheral branches
5
Branches of Facial Nerve
1. Greater superficial petrosal nerve from geniculate ganglion, carries secretomotor fibres to lacrimal gland.
2. Nerve to stapedius arises at second genu and supplies the stapedius muscle.
3. Chorda tympani arises from vertical segment, and leaves the tympanic cavity through petrotympanic fissure, carries secretomotor fibres to submandibular and sublingual glands and brings taste from anterior two-thirds of tongue.4. Communicating branch joins auricular branch of vagus and supplies the concha, retroauricular groove, posterior meatus and the outer surface of tympanic membrane.
5. Posterior auricular nerve to muscles of pinna, occipital belly of occipitofrontalis.
6. Muscular branches to stylohyoid and posterior belly of digastric.
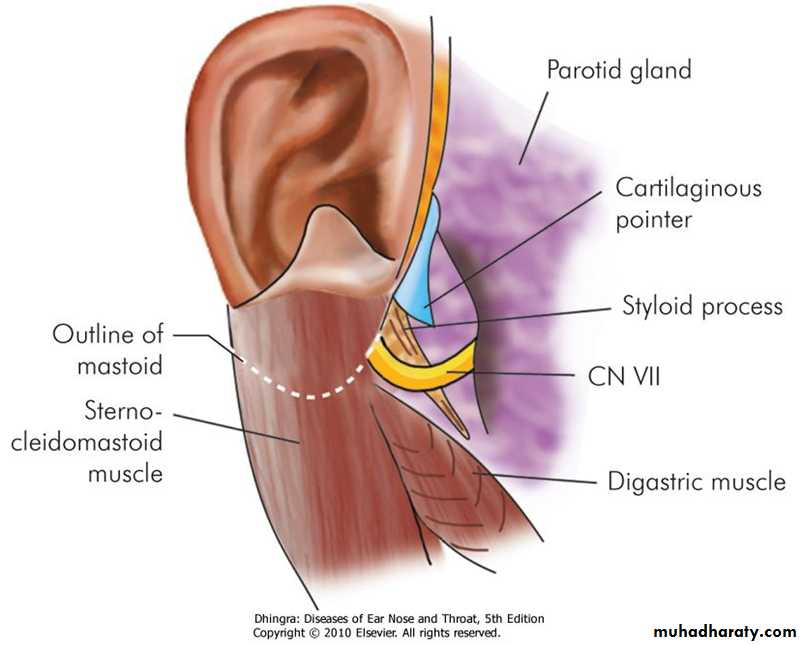
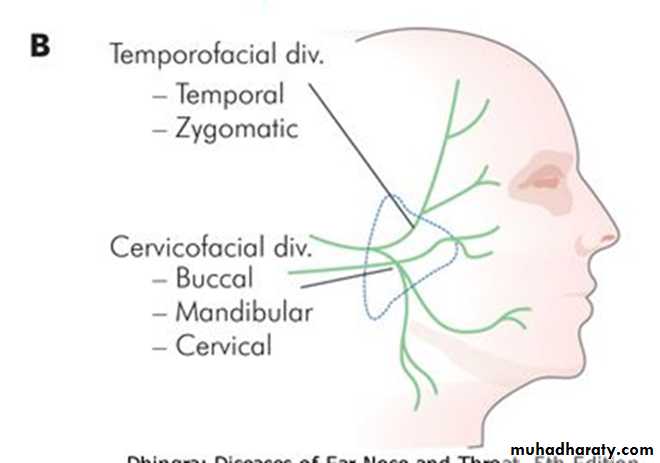
7. Peripheral branches: The nerve trunk, after crossing the styloid process, forms two divisions, an upper temporofacial and a lower cervicofacial, which further divide into smaller branches in the substance of the parotid gland. These are the temporal, zygomatic, buccal, marginal mandibular and cervical and together form pes anserinus (goose-foot). They supply all the muscles of facial expression.6
7
Electrodiagnostic Tests
These tests are useful to differentiate between neurapraxia and degeneration of the nerve. They also help to predict prognosis and indicate time for surgical decompression of the nerve.
1. Minimal nerve excitability test
2. Maximal stimulation test (MST)
3. Electroneuronography (ENoG)
4. Electromyography (EMG)
CAUSES OF FACIAL PARALYSIS
1.Central: Brain abscess,Pontine gliomas, Poliomyelitis, Multiple sclerosis2.Intracranial part (cerebellopontine angle):Acoustic neuroma, Meningioma, Congenital cholesteatoma, Metastatic carcinoma ,Meningitis
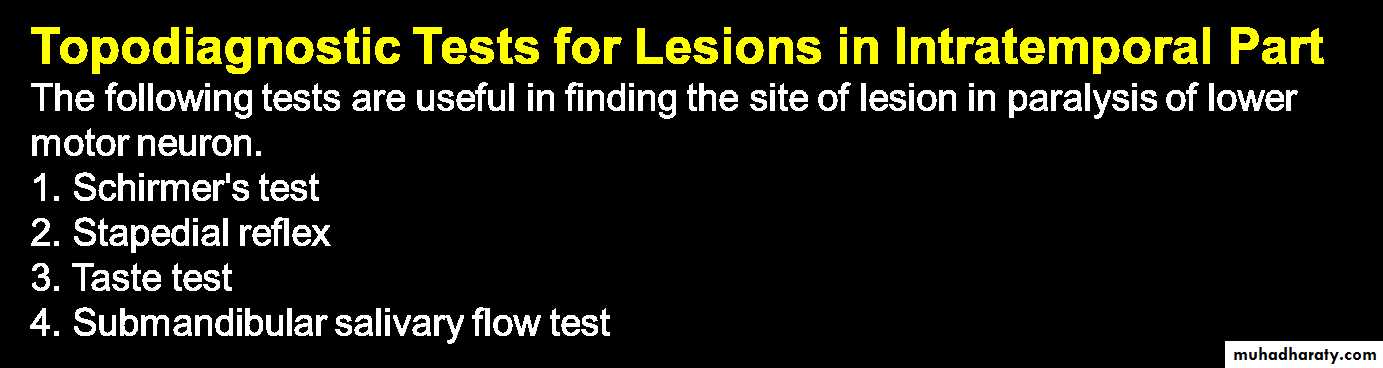
3.Intratemporal part
(a) Idiopathic: Bell's palsy, Melkersson's syndrome(b) Infections
ASOM , CSOM, Herpes zoster oticus, Malignant otitis externa
(c) Trauma
Surgical: Mastoidectomy, Stapedectomy
Accidental: Fractures of temporal bone
(d) Neoplasms
Malignancies of external and middle ear ,Glomus jugulare tumour ,Facial nerve neuroma, Metastasis to temporal bone (from cancer of breast, bronchus, prostate)4.Extracranial part
Malignancy of parotid, Surgery of parotid, Accidental injury in parotid region ,Neonatal facial injury (obstetrical forceps)5.Systemic diseases
DM, Hypothyroidism ,Uraemia
Polyarteritis nodosa ,Wegener's granulomatosis ,Sarcoidosis ,Leprosy
Leukaemia, Demyelinating disease
9
10
Bell's Palsy
Sixty to seventy-five percent of facial paralysis is due to Bell's palsy. It is defined as idiopathic, peripheral(LMN) facial paralysis or paresis of acute onset. Both sexes are affected with equal frequency. Any age group may be affected . A positive family history in 6-8% . Risk is more in diabetics (angiopathy) and pregnant women (retention of fluid).
Aetiology
(a) Viral infection : Herpes simplex?(b) Vascular ischaemia
(c) Hereditary
(d) Autoimmune disorder
Clinical Features
Onset is sudden. Patient is unable to close his eye. On attempting to close the eye, eyeball turns up and out (Bell's phenomenon). Saliva dribbles from the angle of mouth. Face becomes asymmetrical. Tears flow down from the eye (epiphora). Pain in the ear may precede or accompany the nerve paralysis. Some complain of noise intolerance (stapedial paralysis) or loss of taste (involvement of chorda tympani). may be complete or incomplete. Bell's palsy is recurrent in 3-10% of patients.11
Treatment
General
1. Reassurance.2. Relief of ear pain by analgesics.
3. Care of the eye.
4. Physiotherapy or massage of the facial muscles gives psychological support to the patient.
Medical management
Prednisolone is the drug of choice, the adult dose of prednisolone is 1 mg/kg/day divided into morning and evening doses for 5 days. Patient is seen on the 5th day. If paralysis is incomplete or is recovering, dose is tapered during the next 5 days. If paralysis remains complete, the same dose is continued for another 10 days and thereafter tapered in next 5 days. (total of 20 days).Contraindications to use of steroids include pregnancy, diabetes, hypertension, peptic ulcer, pulmonary tuberculosis and glaucoma.
Steroids can be combined with acyclovir for Herpes zoster oticus or Bell's palsy.
12
Surgical treatment
Nerve decompression relieves pressure on the nerve fibres and thus improves the microcirculation of the nerve. Vertical and tympanic segments of nerve are decompressed. Some workers have suggested total decompression including labyrinthine segment by postaural and middle fossa approach.
Prognosis
Eighty-five to ninety percent of the patients recover fully.10-15% recover incompletely and may be left with some stigmata of regeneration.
Recurrent facial palsy may not recover fully
13
Herpes Zoster Oticus (Ramsay-Hunt Syndrome)
There is facial paralysis along with vesicular rash in the external auditory canal and pinna . There may also be anaesthesia of face, giddiness and hearing impairment due to involvement of Vth and VIIIth nerves. Treatment is the same as for Bell's palsy.
14
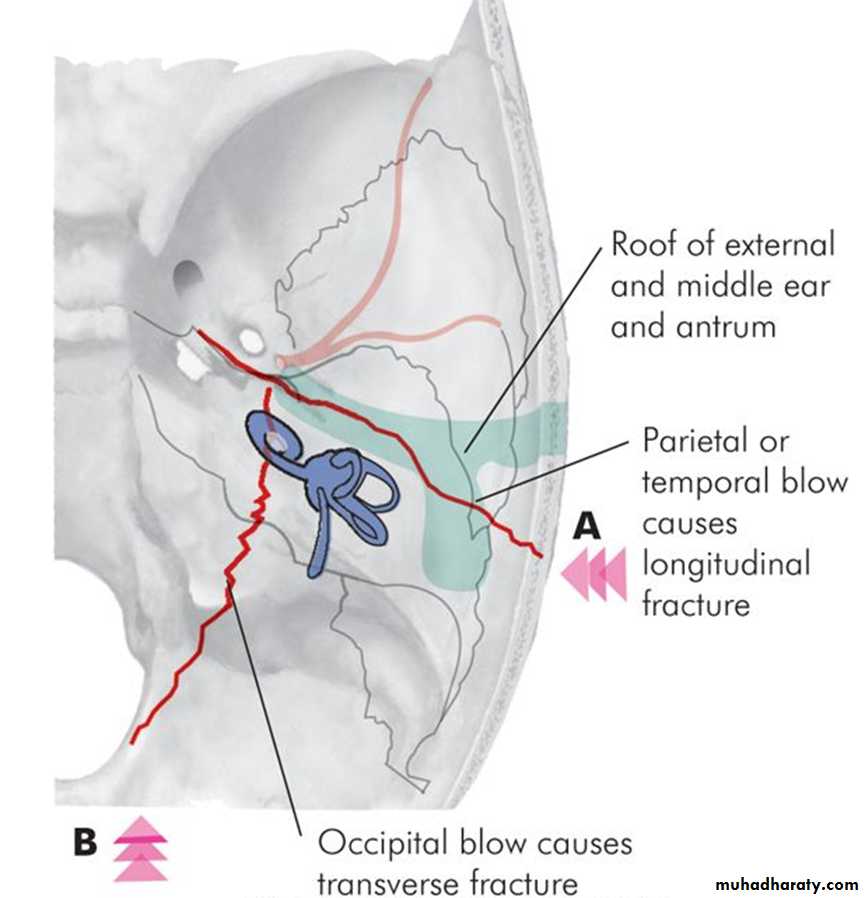
Fractures of Temporal Bone
may be longitudinal, transverse or mixed . Facial palsy is seen more often in transverse fractures (50%). Paralysis is due to intraneural haematoma, compression by a bony spicule or transection of nerve.
Delayed onset paralysis is treated conservatively like Bell's palsy while immediate onset paralysis may require surgery in the form of decompression, re-anastomosis of cut ends or cable nerve graft.
15
Ear or Mastoid Surgery
Facial nerve is injured during stapedectomy, tympanoplasty or mastoid surgery.Paralysis may be immediate or delayed and treatment is the same as in temporal bone trauma.
Sometimes, nerve is paralysed due to pressure of packing on the exposed nerve and this should be relieved first.
Parotid Surgery and Trauma to Face
Facial nerve may be injured in surgery of parotid tumours or deliberately excised in malignant tumours.
Accidental injuries in the parotid region can also cause facial paralysis. Application of obstetrical forceps may also result in facial paralysis in the neonate due to pressure on the extratemporal part of nerve
16
Intratemporal Neoplasms
Carcinoma of external or middle ear, glomus tumour, rhabdomyosarcoma and metastatic tumours of temporal bone, all result in facial paralysis. Facial nerve neuroma is treated by excision and nerve grafting. High resolution CT scan and gadolinium-enhanced MRI is very useful for facial nerve tumour
Tumours of Parotid
Facial paralysis with tumour of the parotid almost always implies malignancySYSTEMIC DISEASES AND FACIAL PARALYSIS
e.g diabetes, hypothyroidism, leukaemia, sarcoidosis, polyarteritis nodosa, Wegener's granulomatosis, leprosy, syphilis and demyelinating disease.17
HYPERKINETIC DISORDERS OF FACIAL NERVE
1. Hemifacial spasm
repeated, uncontrollable twitchings of facial muscles on one side .Microvascular decompression.
selective section of the branches of facial nerve in the parotid
Botulinum toxin in the affected muscle by preventing release of acetylcholine.
2. Blepharospasm
Twitchings and spasms are limited to orbiculars oculi muscles on both sides. The eyes are closed due to muscle spasms causing functional blindness.
The cause is uncertain.
It is treated by selective section of nerves supplying muscles around the eye on both sides.
Botulinum-A toxin injected into the periorbital muscles gives relief for 3-6 months.
18
19
Tumours of External Ear
Of all the cases of ear carcinoma, 85% occur on the pinna, 10% in the external canal and 5% in the middle ear.
Pinna
External ear canal
• Benign
• Preauricular cyst or sinus
• Sebaceous cyst
• Dermoid cyst
• Keloid
• Haemangioma
• Papilloma
• Cutaneous horn
• Keratoacanthoma
• Neurofibroma
• Malignant
• Squamous cell carcinoma
• Basal cell carcinoma
• Melanoma
• Benign
• Osteoma
• Exostosis
• Ceruminoma
• Sebaceous adenoma
• Papilloma
• Malignant
• Squamous cell carcinoma
• Basal cell carcinoma
• Adenocarcinoma
• Malignant ceruminoma
• Melanoma
TUMOURS OF EXTERNAL AUDITORY CANAL
Osteoma
presents as a single, smooth, bony, hard, pedunculated tumour, often arising from the posterior wall of the osseous meatus, near its outer end. Treatment is surgical removal by fracturing through its pedicle or removal with a drill.
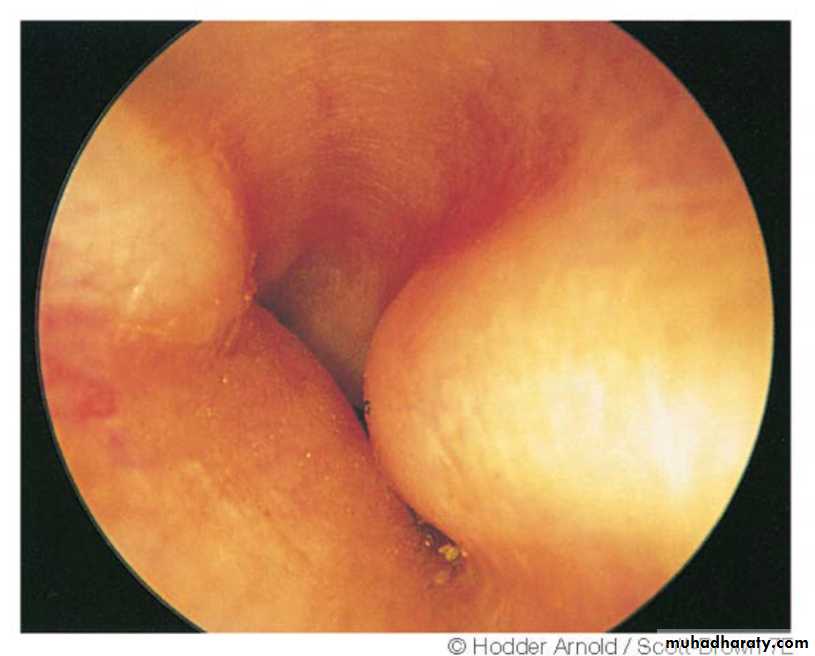
Exostoses
multiple and bilateral, presenting as smooth, sessile, bony swellings in the deeper part of the meatus near the TM. in persons exposed to entry of cold water in the meatus as in divers and swimmers. Males affected 3 times more than females. If small and asymptomatic, no treatment. If impair hearing or cause retention of wax and debris, may be removed with high speed drill.
20
21
Squamous cell carcinoma
it is seen in cases of long-standing ear discharge.
It may arise primarily from the meatus or be a secondary extension from the middle ear carcinoma.Presenting symptoms are: blood staining of mucopurulent or purulent discharge and severe earache.
Examination may show an ulcerated area in the meatus or a bleeding polypoid mass or granulations.
Facial nerve may be paralysed because of local extension of disease.
Regional lymph nodes may be involved.
Treatment is en bloc wide surgical excision with post-operative radiation.
22
Tumours of Middle Ear and Mastoid
Tumours of middle ear and mastoid can be divided into:
1. Primary Tumours• Benign: Glomus tumour
• Malignant: Carcinoma, sarcoma
2. Secondary Tumours
(a) From adjacent areas, e.g. nasopharynx, external meatus and the parotid. (b) Metastatic, e.g. from carcinoma of bronchus, breast, kidney, thyroid, prostate and gastrointestinal tract23
GLOMUS TUMOUR
It is the most common benign neoplasm of middle ear and is so-named because of its origin from the glomus bodies found in the dome of jugular bulb or on the promontory along the course of tympanic branch of IXth cranial nerve (Jacobson's nerve).
24
Clinical Features
often seen in the middle age (40-50 years).
Females are affected five times more.
Earliest symptoms are hearing loss and tinnitus. Hearing loss is conductive and slowly progressive. Tinnitus is pulsatile
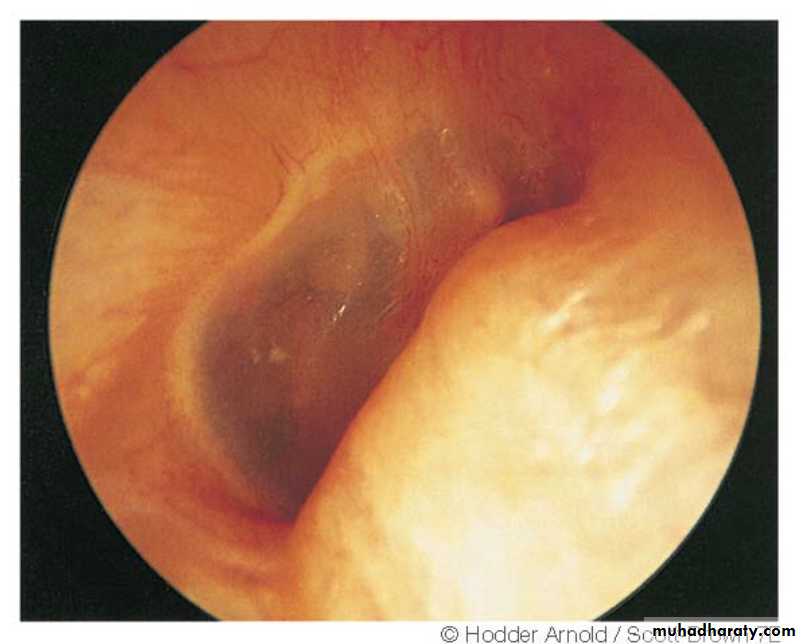
Otoscopy
"Rising sun" appearance is seen when tumour arises from the floor of middle ear.
Brown sign
Dizziness or vertigo and facial paralysis may appear. Earache is less common than in carcinoma of the external and middle ear,
Otorrhoea may occur
Audible bruit
Cranial nerve palsies(9-12 CN)
Some glomus tumours secrete catecholamines and produce symptoms like headache, sweating, palpitation, hypertension and anxiety.
25
Diagnosis
History and physical examination
Serum levels of catecholamines or their break-down products in urine (vanillylmandelic acid, metanephrine, etc.).
CT scan &/ or MRI
Four-vessel angiography +EmbolizationIn large tumours, embolization of feeding vessels 1-2 days before operation.
Biopsy
Preoperative biopsy of the tumour for diagnosis is never done.Treatment
It consists of:
1. Surgical removal.2. Radiation.
3. Embolisation.
4. Combination of the above techniques.
26
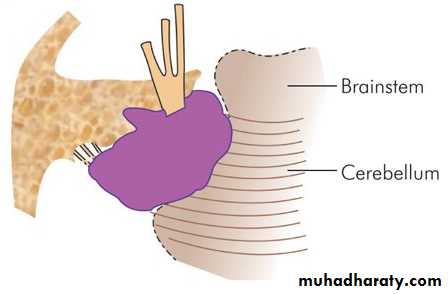
Acoustic Neuroma
Acoustic neuroma is also known as vestibular schwannoma, neurilemmoma or eighth nerve tumour.
Incidence
Acoustic neuroma constitutes 80% of all cerebellopontine angle tumours and 10% of all the brain tumoursPathology
It is a benign, encapsulated, extremely slow-growing tumour of the 8th nerve. Bilateral tumours are seen in patients with neurofibromatosis type 227
Clinical Features
1. Age and sex: 40-60 years. Both sexes are equally affected.
2. Cochleovestibular symptoms
Progressive unilateral SNHL, often accompanied by tinnitus, is the presenting symptom in majority of cases. There is marked difficulty in understanding speech. Some patients may get sudden hearing loss.Vestibular symptoms are imbalance or unsteadiness.
3. Cranial nerve involvement
Vth nerve: corneal reflexVIIth nerve
IXth and Xth nerves. There is dysphagia and hoarseness
Other cranial nerves are affected when tumour is very large.
4. Brainstem involvement.
5. Cerebellar involvement seen in large tumours.
6. Raised intracranial pressure
late feature. headache, nausea, vomiting, diplopia due to VIth nerve involvement and papilloedema with blurring of vision.
28
Investigations and Diagnosis
1. Audiological tests
2. Stapedial reflex decay test3. Vestibular tests
Caloric test will show diminished or absent response in 96% of patients.
4. Neurological tests
Fundus is examined for blurring of disc margins or papilloedema.
5. Radiological tests
(a) Plain X-rays.
(b) CT scan.
(c) MRI with gadolinium contrast is the gold standard for diagnosis of acoustic neuroma.
(d) Vertebral angiography. This is helpful to differentiate acoustic neuroma from other tumours of cerebellopontine angle when doubt exists.
6. Evoked response audiometry (BERA)
It is very useful in the diagnosis of retrocochlear lesions.
29
Differential Diagnosis
Acoustic neuroma should be differentiated from the cochlear pathology (i.e. Meniere's disease) and other cerebellopontine angle tumours, e.g. meningioma, primary cholesteatoma and arachnoidal cyst.Treatment
Surgery : Surgical removal of the tumour is the treatment of choice. Surgical approach will depend upon the size of tumour.Gamma knife surgery.
Cyber knife.
30
31
Otalgia (Earache)
Pain in the ear can be due to causes occurring locally in the ear or referred to it from remote areas.A. Local Causes
1. External ear
Furuncle, impacted wax, otitis externa, otomycosis, myringitis bullosa, herpes zoster, and malignant neoplasms.
2. Middle ear
Acute otitis media, eustachian tube obstruction, mastoiditis, extradural abscess, aero-otitis media, and carcinoma middle ear
32
B. Referred Causes
1. Via Vth cranial nerve
(a) Dental. Caries, apical abscess, impacted molar, malocclusion.
(b) Oral cavity. Benign or malignant ulcerative lesions of oral cavity or tongue.
(c) Temporomandibular joint disorders.(most common cause) Bruxism, osteoarthritis, recurrent dislocation, ill-fitting denture.
(d) Sphenopalatine neuralgia.
2. Via IXth cranial nerve
(a) Oropharynx. Acute tonsillitis, peritonsillar abscess, tonsillectomy. Benign or malignant ulcers of soft palate, tonsil and its pillars.(b) Base of tongue. Tuberculosis or malignancy.
(c) Elongated styloid process.
3. Via Xth cranial nerve
Malignancy or ulcerative lesion of: vallecula, epiglottis, larynx or laryngopharynx, oesophagus.4. Via C2 and C3 spinal nerves
Cervical spondylosis, injuries of cervical spine, caries spineC. Psychogenic Causes
When no cause has been discovered, pain may be functional.33
Tinnitus
Tinnitus is ringing sound or noise in the ear. The characteristic feature is that the origin of this sound is within the patient.
Usually, it is unilateral but may also affect both ears.
It may vary in pitch and loudness and has been variously described by the patient as roaring, hissing, swishing, rustling or clicking type of noise. Tinnitus is more annoying in quiet surroundings, particularly at night, when the masking effect of ambient noise from the environment is lost
Types of Tinnitus
Two types of tinnitus are described:(a) Subjective, which can only be heard by the patient.
(b) Objective, which can even be heard by the examiner with the use of a stethoscope
34
35
Treatment
Where possible, its cause should be discovered and treated.When no cause is found, management of tinnitus includes:
1. Reassurance and psychotherapy.
2. Techniques of relaxation and biofeedback.
3. Sedation and tranquillizers.(TCA).
4. Masking of tinnitus. Tinnitus is more annoying at bed time when the surroundings are quiet. Use of a fan, loudly clicking clock or a similar device may mask the tinnitus and help the patient to go to sleep. Use of a hearing aid, in persons with hearing loss, not only improves hearing but also provides a masking effect.
Tinnitus maskers can be used in patients who have no hearing loss. They are worn like a hearing aid.
36