
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
1
ANATOMY
and
PHYSIOLOGY
The composition of blood is kept constant mainly through selective
elimination of water and solutes by kidneys. This control involves balancing
body's input of ions and water with amounts excreted. As Na+ and Cl- are most
abundant somatically active solutes in plasma, control of plasma volume and
tonicity can be largely achieved by controlling amounts of these ions and water
excreted.
FUNCTIONS
of
the
KIDNEY
1- Excretory:
Excretion of water products and drugs in urine.
2- Regulatory:
Kidney regulates volume, osmotic pressure of blood.
3-Endocrine:
Kidney produces the following hormones.
a-Renin:
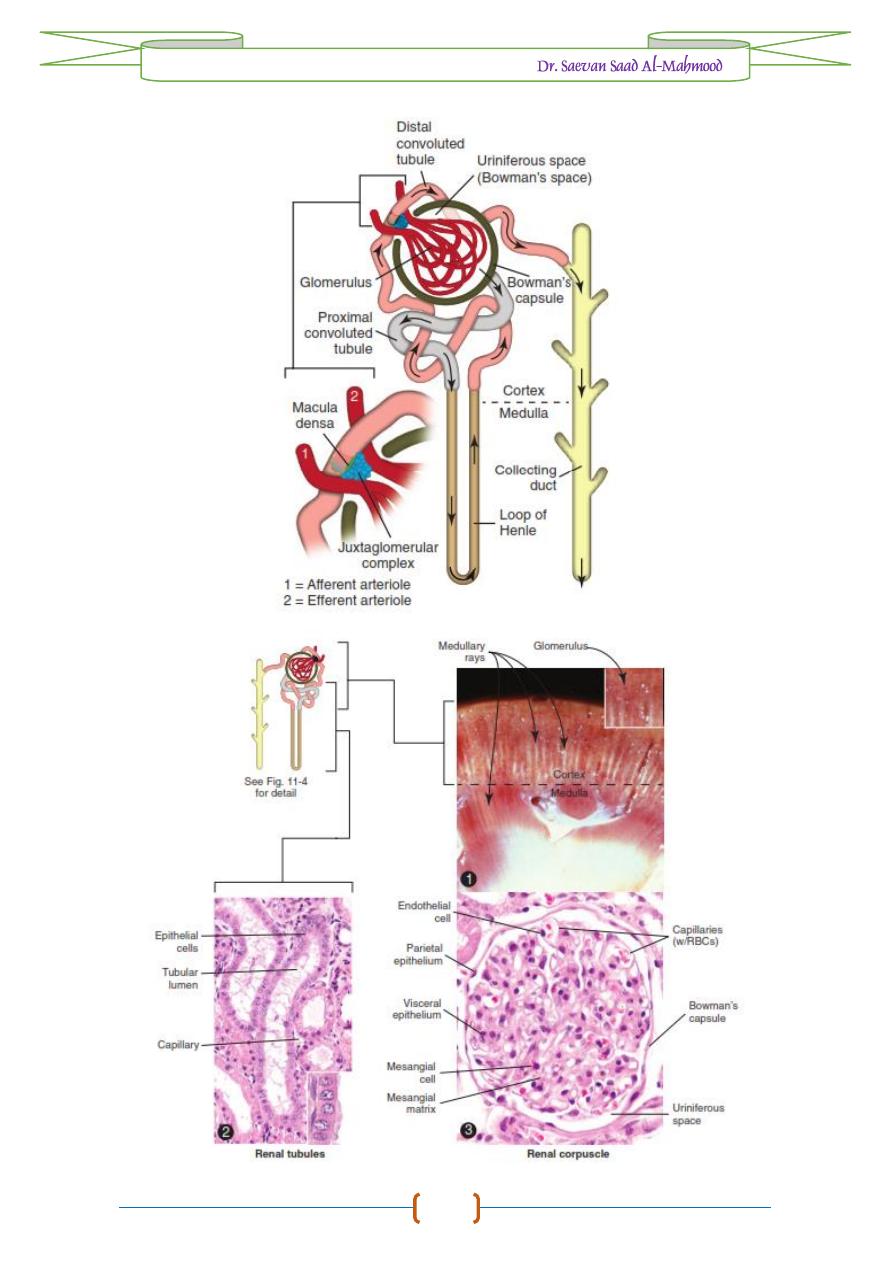
It is produced by juxtaglomerular apparatus which is made of
specialized cells on smooth muscle cells located on afferent glomerular
arteriole as it enters glomerulus.
b-Erythropoietin:
is a glycoprotein produced mainly by kidney and is one of the
major stimuli of erythropoiesis.
c-Prostaglandin:
The kidney produces prostaglandin E
2
, a powerful vasodilator
agent.
4-Metabolic:
a-Vitamin D metabolism:
Vitamin D requires hydroxylation in liver and again
by kidney to produce 1,25 dihydroxy calciferol.
b-Protein and polypeptide hormones:
The kidney is the major site for catabolism
of insulin, parathyroid hormone and calcitonin.
GROSS STRUCTURE
of
the
KIDNEY
The basic unit of kidney function is the nephron of which there are about
1,000,000 nephrons in each kidney. Urine formed in tubular part of nephron
collects in renal pelvis and then flows through ureter to bladder for subsequent
elimination via the urethra.
The glomerulus is formed by invagination of a tuft of 50 anatomizing
capillaries into dilated blind end of nephron (
Bowman's capsule
). Functionally
the glomerular membrane permits the passage of substances up to 4 nm in
diameter and does not allow the passage of those with diameter greater than 8 nm.
The proximal convoluted tubules (PCT) is made of a single layer of cells
which show on their luminal edges brush border due to the presence of numerous
microvilli. The structure of the loop of Henle differs according to its location in
the kidney. The distal convoluted tubule (DCT) has a similar structure to loop of
Henle. DCT from large number of different nephrons drain into a common
collecting duct and then via a papillary duct into the renal pelvis. The largest
collecting ducts empty through the renal pelvis through the tips of the renal
papillae, which protrude into the renal calyces.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
2
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
3
GENERAL TERMS
in
URINARY SYSTEM PATHOLOGY
1-Aplasia:
Absence of one or both kidneys, absence of one kidney is observed in
animals with compensatory hypertrophy of another kidney.
2-Hypoplasia:
The size of kidneys remains small which don't grow properly due
to
defect in autosomal gene
.
3-Hematuria:
Presence of blood in urine giving bright red color. Occur due to
damage in glomeruli, tubule or hemorrhage anywhere from glomeruli to
urethra. The most important cause of hematuria is
bracken fern toxicity
.
4-Hemoglobinuria:
When hemoglobin is present in urine without erythrocytes
due to intravascular hemolysis. The urine becomes brownish red in color.
Hemoglobinuria is caused by various infections such as
Leptospira
sp.,
Babesia
sp. or
phosphorus deficiency
in animals.
5-Anuria:
Absence of urine is known as anuria.
6-Polyuria:
Increased amount of urine leading to frequent urination due to
diabetes insipidus
,
hormonal imbalance
and
polydipsia
.
7-Oliguria:
Decreased in amount of urine that secreted, which occurs due to
glomerulonephritis
,
obstruction in urinary passage
,
dehydration
and
low blood
pressure
.
8-Uremia:
The presence of urine elements as uric acid, creatinine and urea in
blood, occur due to
damage in kidneys
so urine remains in blood and causes
uremia.
9-Glycosuria:
The presence of glucose in secreted urine. This is also known as
diabetes mellitus
occur due to insulin deficiency. Occur in dogs due to
hypoglycemia, in sheep due to enterotoxaemia caused by Clostridium welchii
type D.
10-Pyuria:
Presence of pus material in urine due to
suppurative inflammation
in
urinary tract.
11-Ketonuria:
Presence of ketone bodies in urine, which is common in
diabetes
mellitus
,
acetonemia
,
pregnancy toxemia
and in
starvation
.

Pathology of
URINARY SYSTEM
/
2016 – 2017 /
4
PIGMENTATION
in
RENAL TISSUES
Lipofuscinosis
: Fine golden granules of brown iron-free pigment with the
staining characteristics of lipofuscin (“wear and tear pigment”) can accumulate
in renal epithelial cells of old cattle, resulting in lipofuscinosis.
Grossly
, the
renal cortex can have streaks of brown discoloration, but renal function is not
affected.
Microscopically
, the accumulations are noted most prominently within
proximal convoluted epithelial cells.
Hemosiderin
and
Ferritin
: Pigment present in renal tubules. The origin of
hemosiderin pigment is most likely from degradation of hemoglobin resorbed
from glomerular filtrate by proximal tubular epithelium due to concurrent
hemolysis of blood. In dogs,
microscopic
present in cytoplasm of proximal
convoluted tubular epithelial cells.
Cloisonné
kidneys
: which occur in goats, due to proximal tubular basement
membrane thickening as a result of deposits of ferritin and hemosiderin.
Grossly
,
these kidneys have diffuse, intense, black or brown discoloration of cortex
separated from medulla and renal function is normal.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
5
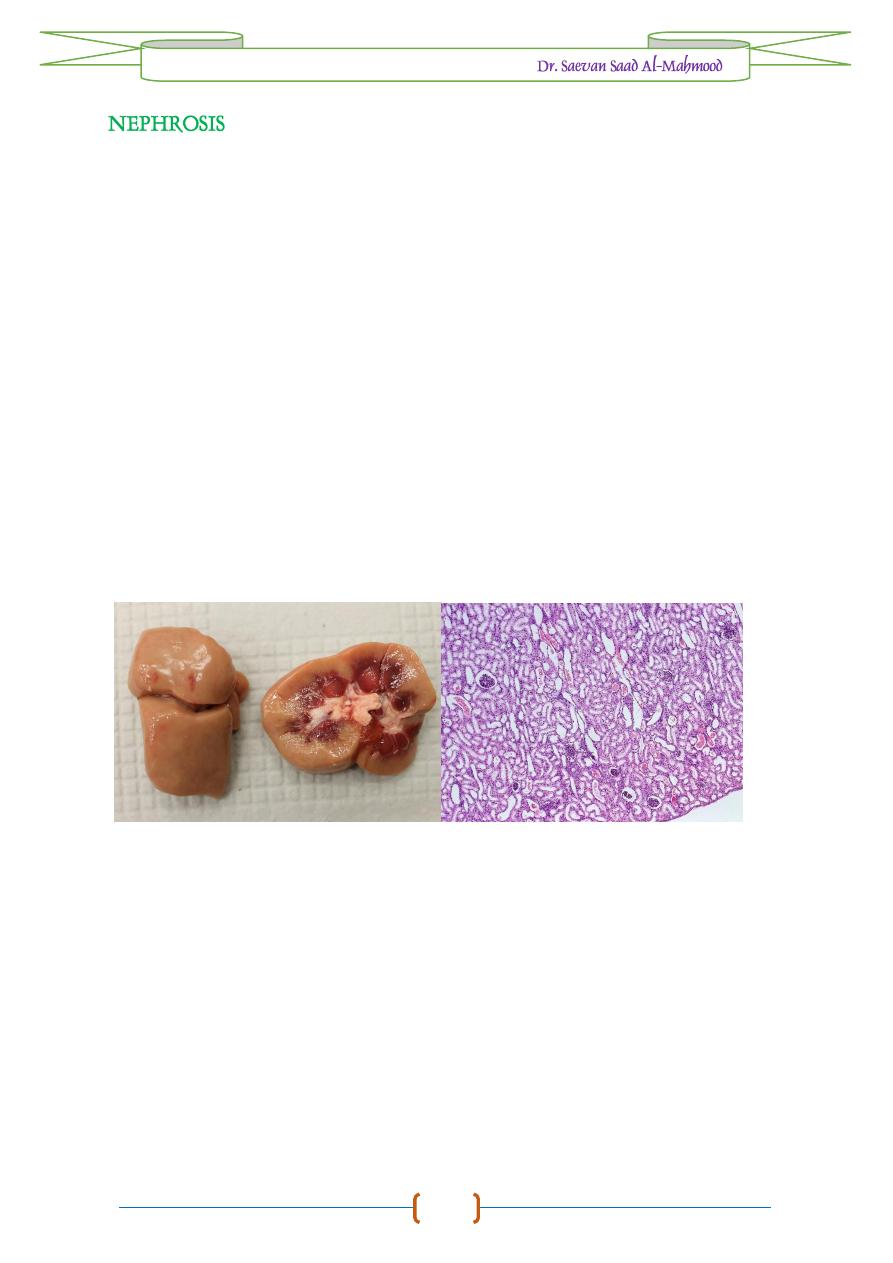
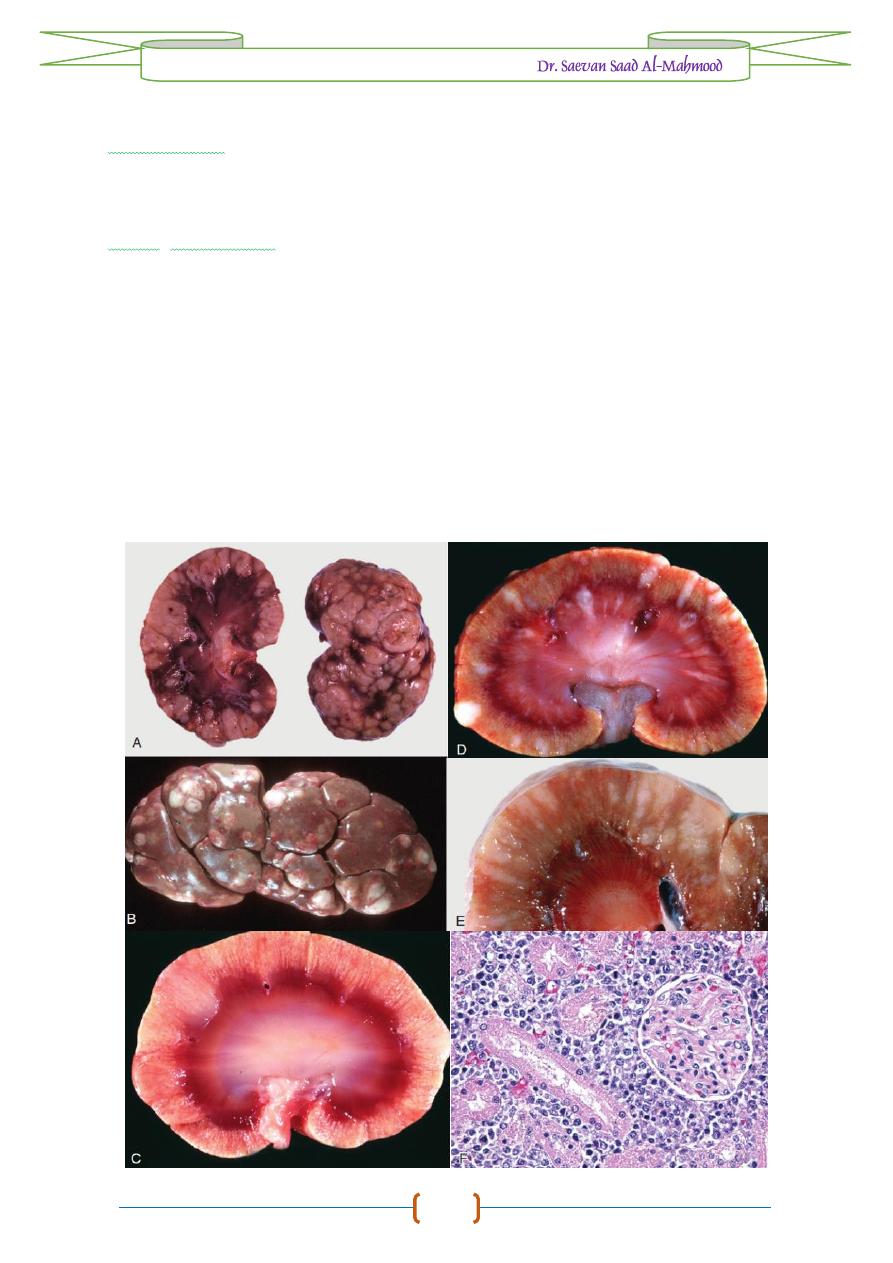
Nephrosis is degeneration and necrosis of tubular epithelium without
producing inflammatory reaction. It mostly includes acute tubular necrosis as a
result of ischemia or toxic injury to kidney. Nephrosis is characterized by necrosis
and sloughing of tubular epithelial cells exhibited by uremia, oligouria, anuria.
Etiology
1-
Hypotension.
2-
Heavy metals.
3-
Mycotoxins as Ochratoxin.
4-
Antibiotics as Gentamicin.
Macroscopic features
1-
Swelling of kidneys.
2-
Capsular surface smooth, pale and translucent.
Microscopic features
1-
Vacuolation in tubular epithelium.
2-
Coagulative necrosis.
3-
Sloughing of tubular epithelium.
Kidney of feedlot cattle showed nephrosis, the gross section showed pale color
in cortex with hemorrhage at medulla are of kidney, while histopathological
section showed degenerative and necrotic changes without infiltration of
inflammatory cells.

Pathology of
URINARY SYSTEM
/
2016 – 2017 /
6
Glomerulonephritis is the inflammation of glomeruli primarily characterized
by pale and enlarged kidneys with hemorrhage, edema of glomeruli, congestion
and infiltration of inflammatory cells.
Etiology
1-
Streptococci infection.
2-
Immune complexes.
3-
Organochlorine pesticides.
Macroscopic features
1-
Enlarged, pale kidneys.
2-
Petechial hemorrhage on kidneys.
3-
Proteinuria, uremia and hypercholesterolemia.
Microscopic features
1-
Edema of glomeruli leading to increase in size.
2-
Infiltration of neutrophils, macrophages.
3-
Thrombosis and necrosis of glomerular capillaries.
Mediators of Immune Glomerular Injury and Epithelial Cell Injury. A, Mediators of immune glomerular
injury, including effector cells, molecules, and cells affected or injured. B, Visceral epithelial cell
(podocyte) injury. The postulated sequence is a consequence of antibodies against epithelial cell
antigens, arriving in the circulating blood (1) with subsequent activation of effector cells, including
podocytes and mesangial cells (2). This leads to liberation of toxins, cytokines, or other effector
molecules (3) that cause injury of podocytes, podocyte foot processes, and endothelial cells (4) with
subsequent cell detachment, resulting in protein leakage through the defective glomerular basement
membrane and filtration slits.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
7
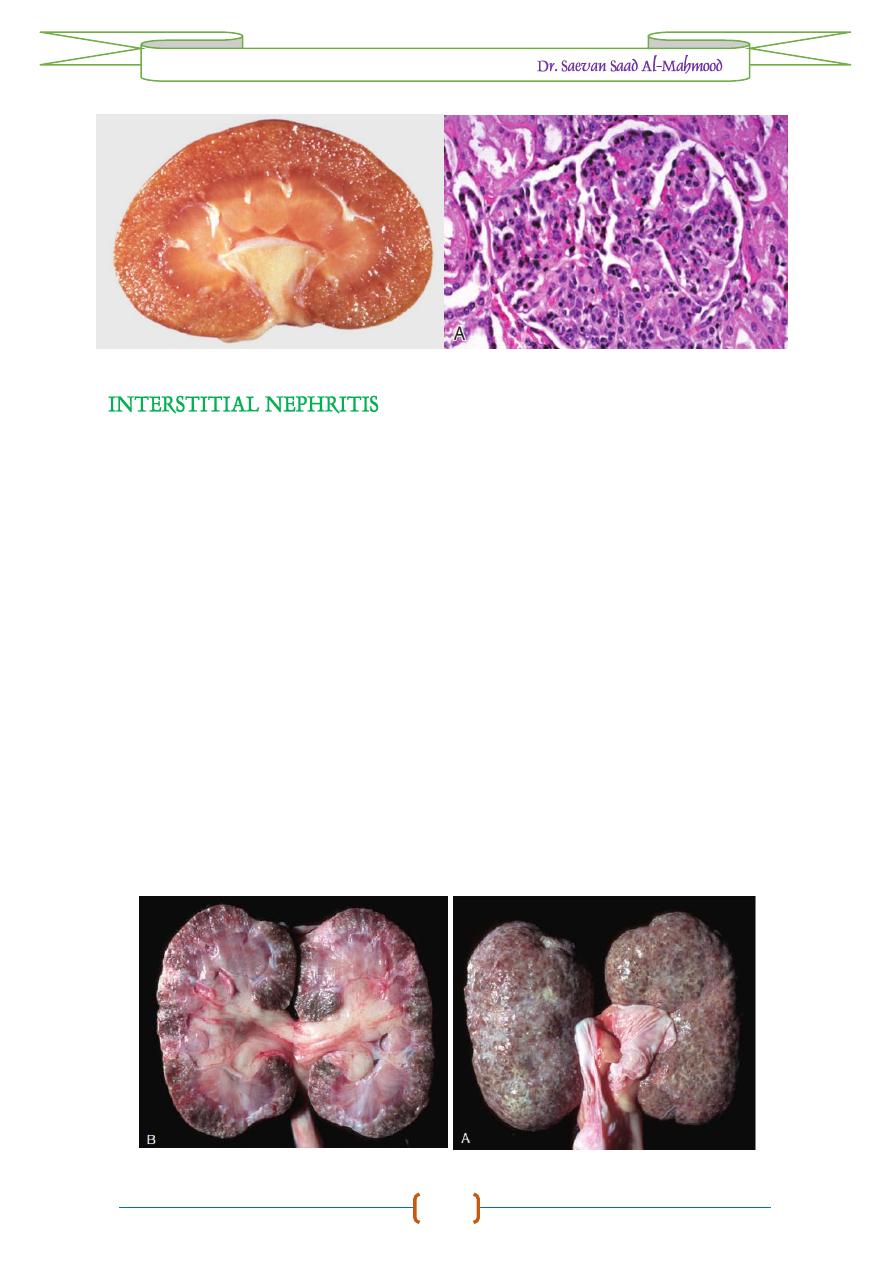
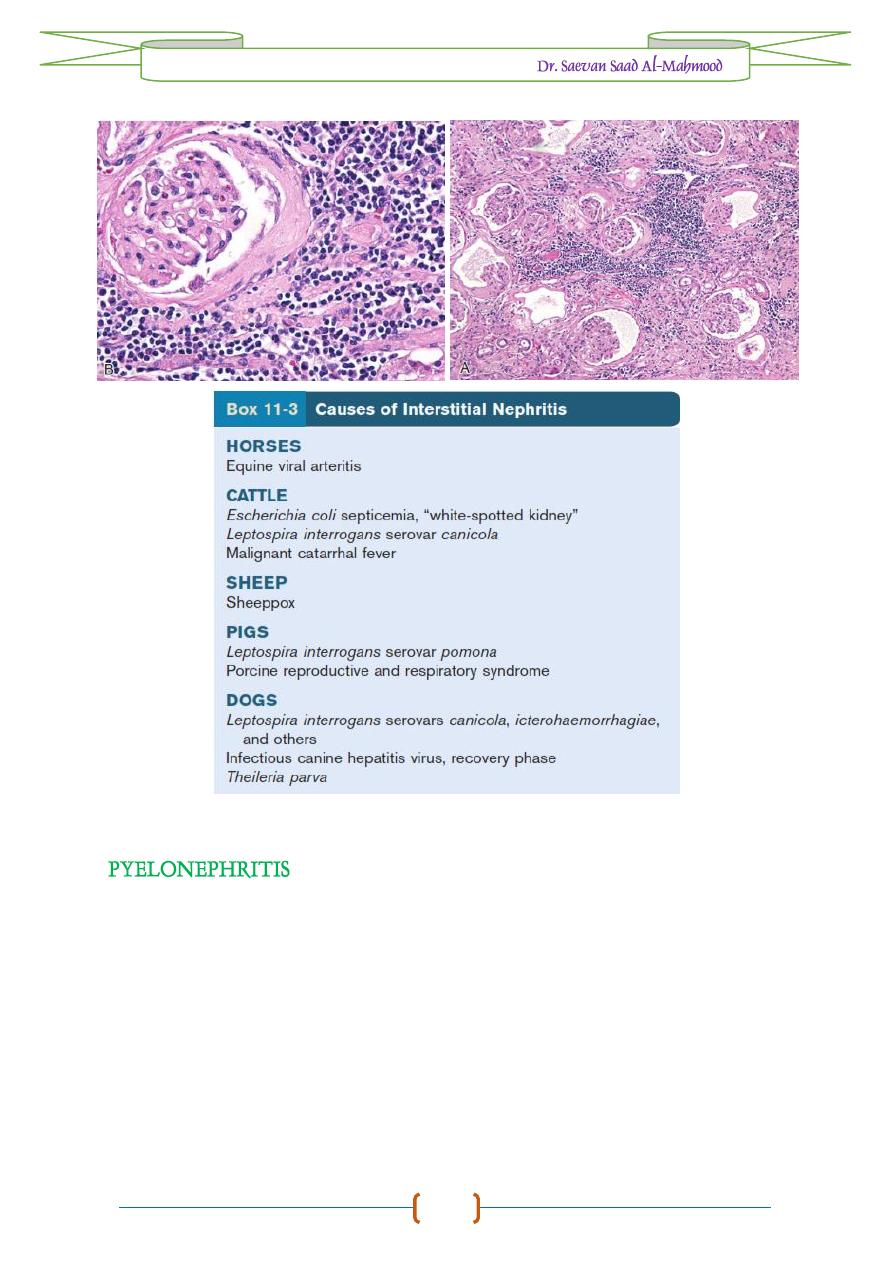
Inflammation of kidney characterized by degeneration and necrosis of
tubular epithelium, edema and infiltration of inflammatory cells in interstitial
tissue.
Etiology
1-
Fungal toxins as in ochratoxin.
2-
Leptospira spp.
3-
Toxins and pesticides.
4-
Herpes virus infection.
5-
Ketosis.
6-
Antibody - Antigen - Complement complex.
Macroscopic features
-
Enlargement of kidneys with petechial hemorrhage.
Microscopic features
1-
Edema, congestion, hemorrhage with necrosis of tubular epithelium.
2-
Infiltration of inflammatory cells neutrophils, macrophages and lymphocytes
in interstitial.
3-
Immune complexes are deposited in granular form causing degeneration of
epithelial cells of tubules and mononuclear cell infiltration with fibrosis in
chronic cases.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
8
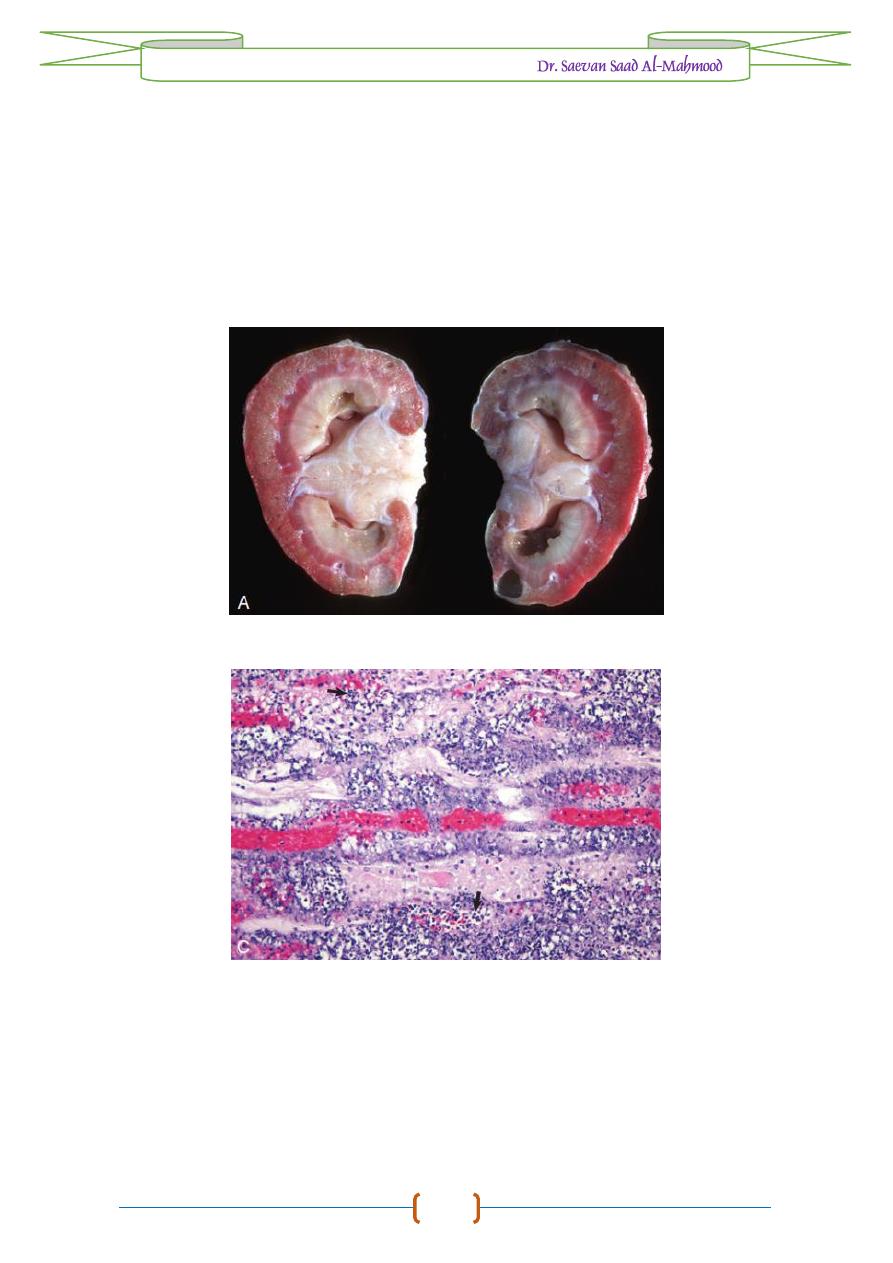
Inflammation of renal pelvis and parenchyma (tubules) characterized by
congestion with suppurative inflammation and fibrosis.
Etiology
1-
Corynebacterium renale.
2-
Staphylococcus aureus.
3-
E. coli.
4-
Actinomyces pyogenes.
5-
Pseudomonas aeruginosa.
Macroscopic features
1-
Congestion, hemorrhage with abscess formation in renal cortex, renal pelvis
and ureters.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
9
2-
Pyuria (pus mixed urine in bladder).
3-
Enlargement of kidneys.
Microscopic features
1-
Congestion, hemorrhage with Suppurative inflammation and purulent
exudate in both pelvis and kidney parenchyma with Infiltration of
neutrophils, lymphocytes and plasma cells in interstitial tissue of kidney.
2-
Necrosis of collecting ducts with sloughing of cellular debris in lumen.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
10
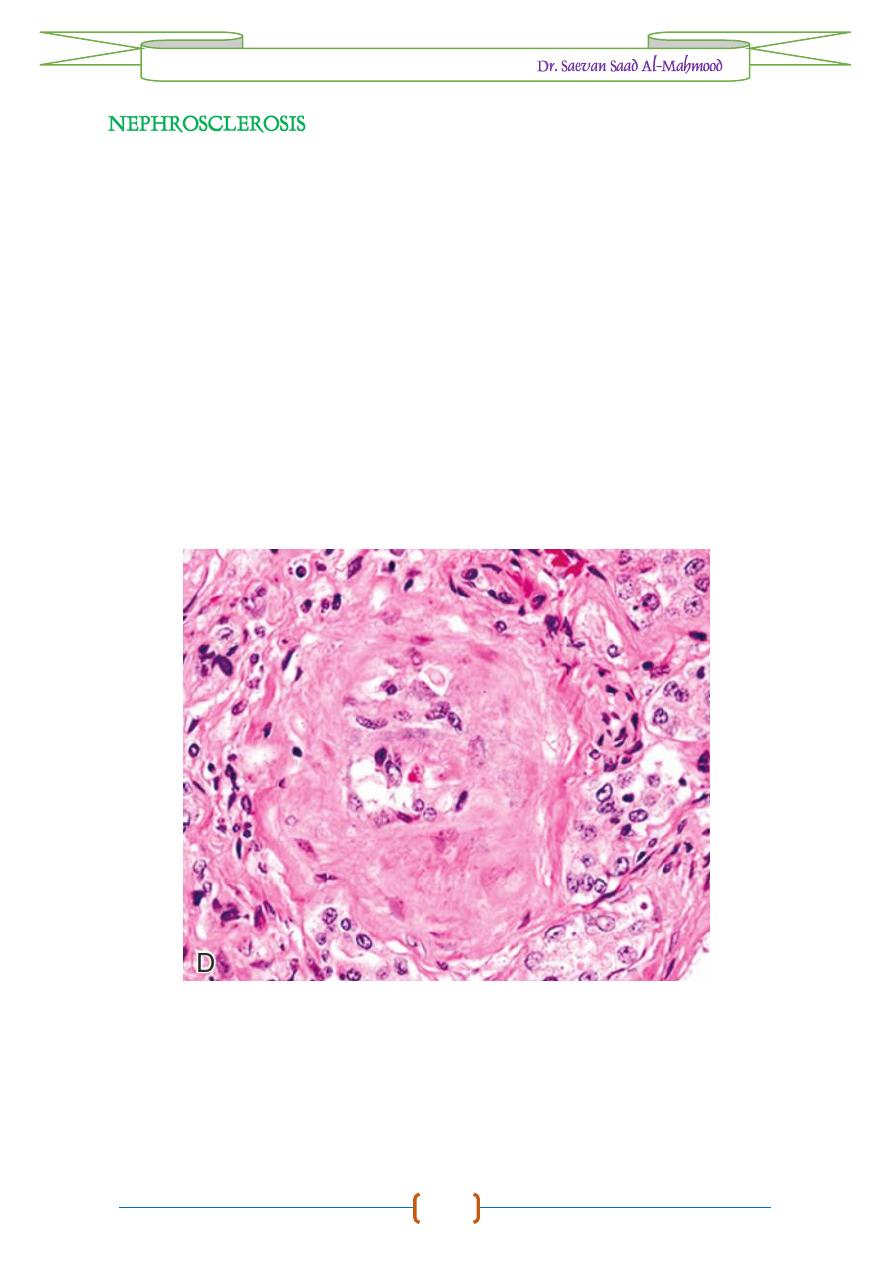
Chronic fibrosis of kidney characterized by loss of glomeruli and tubules
with extensive fibrosis.
Etiology
1-
Chronic Glomerulonephritis.
2-
Chronic Interstitial nephritis.
3-
Arterioloscleresis.
Macroscopic Features
1-
Hard, atrophied kidneys with fibrous nodules on surface.
2-
Thickening of capsule.
Microscopic features
1-
Ischemia, tubular atrophy.
2-
Loss of glomeruli and tubules.
3-
Extensive fibrosis.
4-
Deposition of hyaline casts.
5-
Infiltration of mononuclear cells.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
11
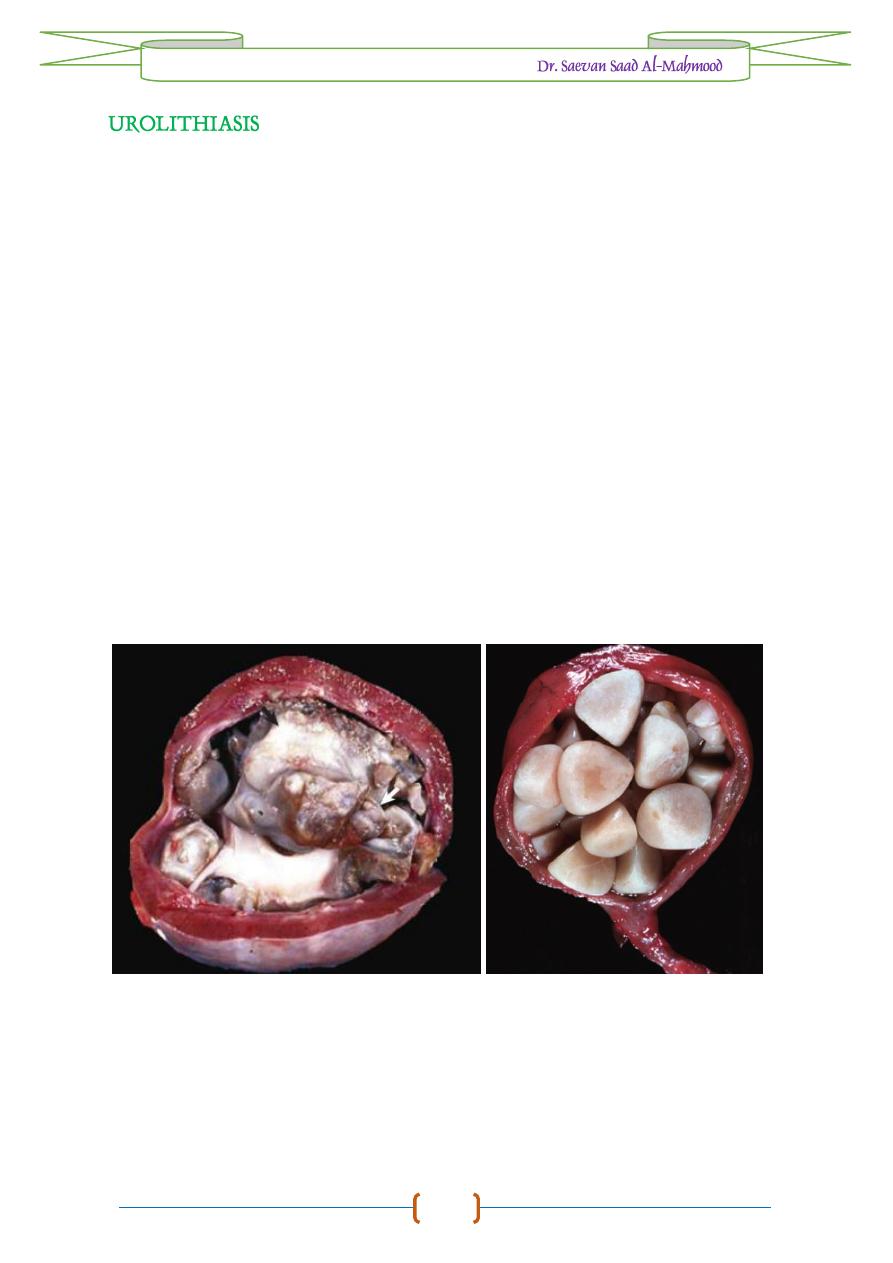
Formation of stony precipitates anywhere in urinary passage including
kidneys, ureter, urinary bladder or urethra.
Etiology
1-
Bacterial infections.
2-
Metabolic defects.
3-
Vitamin A deficiency.
4-
Hyperparathyroidism.
5-
Mineral imbalance.
Macroscopic features
1-
Nephrosis, Hydronephrosis.
2-
Distension of ureters, urethra and urinary bladder.
3-
Hard enlarged kidneys.
4-
Presence of calculi (stone) in kidney, ureter, bladder or urethra which differ
in size, shape and composition.
Microscopic features
1-
Presence of crystals (stone) in lumen of tubules.
2-
Degeneration and necrosis of tubular epithelium with hemorrhage.
3-
Proliferation of fibrous tissue.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
12
Inflammation of ureter characterized by enlargement, thickening of ureter
wall due to accumulation of urates, or calculi, pyonephrosis and pyelonephritis.
Etiology
1-
Tuberculosis.
2-
Calculi.
3-
Hydronephrosis.
4-
Pyelonephritis.
5-
Pyonephrosis.
Macroscopic features
1-
Deposits of whitish or yellowish urates in ureter.
2-
Obstructions of ureter due to calculi leads to its enlargement and formation
of diverticulum.
Microscopic features
1-
Thickening ureter wall by congestion and infiltration of inflammatory cells.
2-
Extensive fibrosis with infiltration of mononuclear cells in chronic cases.
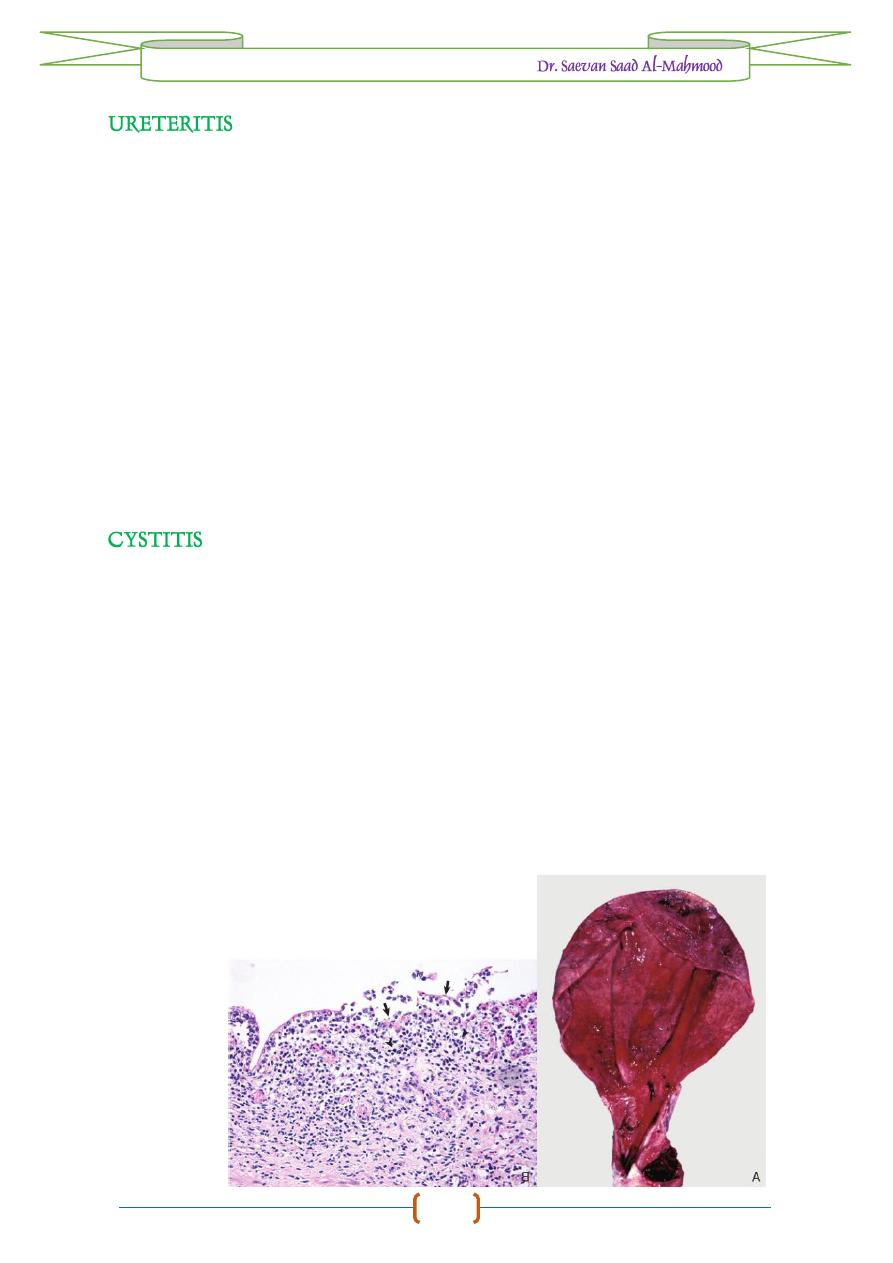
Inflammation of urinary bladder characterized by congestion and fibrinous,
purulent or hemorrhagic exudate.
Etiology
1-
Urinary calculi.
2-
Tuberculosis.
3-
Blockage in urethra.
4-
Bracken fern poisoning.
Macroscopic features
1-
Congestion, hemorrhage with enlargement of urinary bladder.
2-
Thickening of the wall and presence of small nodules on wall.
Microscopic features
1-
Congestion, hemorrhage with fibrosis in chronic cases.
2-
Thickening bladder wall due to infiltration of neutrophils and macrophages.
3-
granulomatous mases in case of tuberculosis.

Pathology of
URINARY SYSTEM
/
2016 – 2017 /
13
Inflammation of urethra which occurs as a result of catheter injury and
calculi. It is characterized by congestion, obstruction and hydronephrosis.
Etiology
1-
Calculi.
2-
Catheter injury.
3-
Trichomonas foetus infection.
4-
Picorna virus infection.
Macroscopic features
1-
Transient inflammation with congestion and hemorrhage.
2-
Obstruction due to calculi, presence of calculi.
Microscopic features
-
Thickening due to inflammatory exudate.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
14
TYPES
of
STONES
in
URINARY SYSTEM
Oxalate calculi
are hard, light yellow, covered with sharp spines found in urinary
bladder and formed due to calcium oxalate. It causes damage in urinary bladder
leading to hemorrhage.
Uric acid calculi
are composed of ammonium and sodium urates and uric acids,
yellow to brown in color, formed in acidic urine, spherical and irregular in shape
and they are not radiopaque.
Phosphate calculi
are white or grey in color, chalky in consistency, soft, friable
and can be crushed with mild pressure. They are mostly multiple in the form of
sand like granules. They are composed of magnesium ammonium phosphate and
occur as a result of bacterial infection.
Xanthine calculi
are brownish red, concentrically laminated, fragile and irregular
in shape. They rarely occur in animals.
Cysteine calculi
are small, soft with shiny and greasy in appearance, yellow in
color which becomes darker on air exposure. Insoluble amino acid cystine
precipitates in bladder to form calculi. Such calculi may cause obstruction of
urethra with cystinuria.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
15
TYPES
of
LESIONS
in
GLOMERULONEPHRITIS
1. Type-I MPGN
§-
Proliferation of mesangial cells.
§-
Deposition of immune complexes containing IgG, IgM, IgA and C3.
§-
Immune complexes penetrate vascular endothelium but not the basement
membrane and are deposited in subendothelial region.
§-
Proliferation and swelling of endothelial cells.
§-
Immune complexes induce production of transforming growth factor (TGFB1)
which increases production of fibrinolectin, collagen and proteoglycans
leading to thickness of basement membrane; this is also known as “
wire loop
”
lesions.
2. Type-II MPGN (Membranous)
§-
Deposition of immune complexes in basement membrane (lamina densa).
§-
Due to uncontrolled activation of complement.
§-
Proliferation of endothelium and mesangial cells.
§-
Demonstration of C3 component, no immunoglobulin.
3. Type III MPGN (Acute Proliferative)
§-
Subepithelial deposits of immune complexes and disruption of basement
membrane.
§-
Swelling of epithelium and its proliferation forming “
Epithelial cresent
”.
§-
Demonstration of IgG in subepithelial region.
§-
Congestion and edema of glomeruli.
§-
Infiltration of neutrophils, macrophages and lymphocytes.
4. Chronic glomerulonephritis
§-
Proliferation of epithelial and endothelial cells.
§-
Reduplication, thickening and disorganization of glomerular basement
membrane.
§-
Lumen of capillaries occluded.
§-
Entire glomerulus is replaced by Hyaline connective tissue.
5. Focal embolic glomerulonephritis
§-
Focal zone of necrosis in glomeruli.
§-
Infiltration of neutrophils.
§-
Proliferation of epithelial cells and formation of crescent.
Pathology of
URINARY SYSTEM
/
2016 – 2017 /
16
TUMORS
of
URINARY SYSTEM
Oncocytomas
. Oncocytomas are rare benign epithelial tumors that can occur in a
variety of tissues.
Grossly
, renal oncocytomas are tan, homogeneous, well-
encapsulated masses.
Histologically
, oncocytomas are composed of large
eosinophilic, granular, round cells with condensed round nuclei.
Renal
Carcinomas
. Renal carcinomas are the most common primary renal
neoplasms and occur most frequently in older dogs. The etiology including the
following:
1-
Viruses
:
Ranid herpesvirus 1 adenocarcinoma
(Lucke’s tumor) in kidney of
frogs,
avian erythroblastosis virus
(oncovirus) induce renal adenocarcinomas in
chickens.
2-
Chemical
carcinogens
: Several known carcinogens can be causative agents and
exert their neoplastic influence by direct DNA damage or inhibition of DNA
synthesis or repair.
3-
Autosomal
dominant
gene
mutations
in
Eker
rats
: These mutations predispose
these rats to bilateral renal cell carcinoma which resembling to human von
Hippel-Lindau disease.
