Occlusion:
Occlusion of the teeth means the relationship in which the teeth of one arch bear to the teeth of other arch when the jaws are closed into maximum cuspal occlusion.Normal occlusion:
Normal occlusion is commonly defined as,“An occlusion within the accepted deviation of the ideal.’’
Malocclusion may be defined as an irregularities of teeth beyond the accepted range of normal.
In modern times, Dr. Edward Angle,who is considered as father of “Orthodontics’’, gave us the first indices of malocclusion which is based on the mesio-distal relation of the teeth,dental arches and the jaws.
Malocclusion
Different classes of malocclusion according to
Angle are:1. Class I malocclusion
2. Class II division 1 malocclusion
3. Class II division 2 malocclusion
4. Class II subdivision malocclusion
5. Class III malocclusion
6. Pseudo-class III malocclusion
7. Class III subdivision malocclusion.
Classification of malocclusion
Malocclusion can be broadly divided into:
1. Intra-arch malocclusions
Mesial,Distal,Lingual,Buccal inclination
Mesial,Distal,Lingual,Buccal displacement
Types of malocclusion
-Infraversion
-Supraversion-Rotations
Mesio-lingual or Disto-lingual disto-buccal or mesio-buccal
-Transposition
2. Inter-arch malocclusions
-Sagittal plane
-Vertical plane
-Transverse plane
3. Skeletal malocclusions.
Types of malocclusion (continued…)
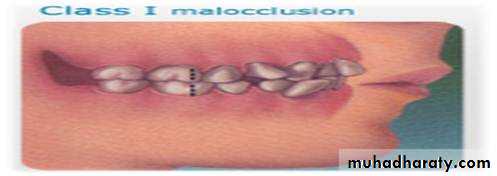
Angle’s class I malocclusion is characterized by the presence of a normal inter-arch molar relationship. The mesio-buccal cusp of the maxillary first permanent molar occludes in the anterior-buccal groove of mandibular first permanent molar.
The patient may exhibit dental irregularities such as crowding,spacing,rotations,missing tooth,etc.
Class I malocclusion
Approximately 60%-70% of all cases of malocclusion fall into this class.
Class I malocclusion (continued…)FEATURES OF CLASS I MALOCCLUSION
Extra-oral features:1. Straight profile
2. Competent/incompetent lips
3. Normal/deep/shallow mento-labial sulcus
Intra-oral features:
1. Class I molar canine incisor relationship
2. Spacing of teeth
3. Crowding of teeth
4. Anterior crossbite
5. Posterior crossbite
Features of class I malocclusion
6. Anterior openbite
7. Proclination
8. Retroclination
9. Rotation of teeth
10. Deep bite
11. Bi-maxillary protrusion
Features of class I malocclusion (continued…)
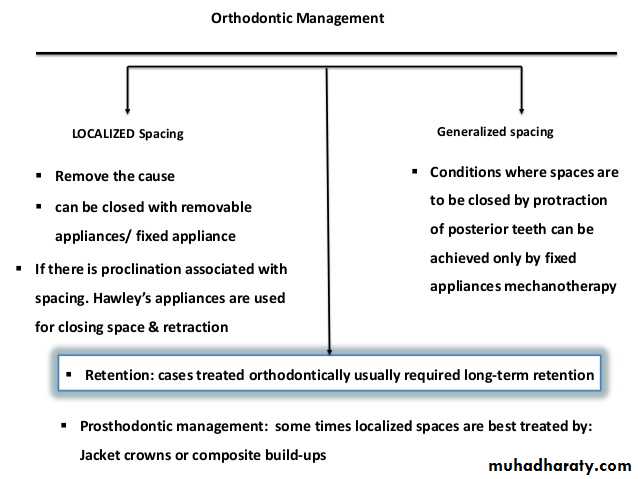
MANAGEMENT OF CLASS I MALOCCLUSION
Spacing
Midline diastemaCrowding
Crossbite
Openbite (anterior)
Rotations
Deepbite (anterior)
Bimaxillary protrusion.
Treatment aimed at correcting
• History
• Clinical examination• Study models
• Radiography
-OPG
-Intra-oral periapical
-Lateral cephalogram.
Diagnosis
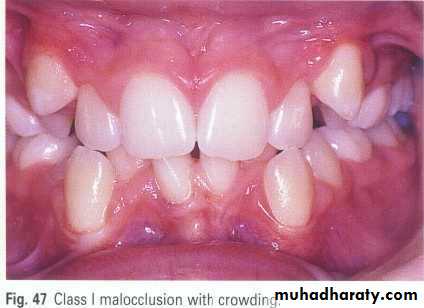
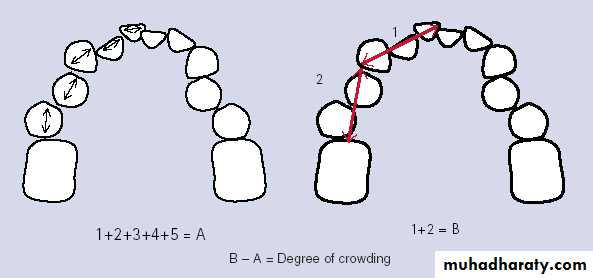
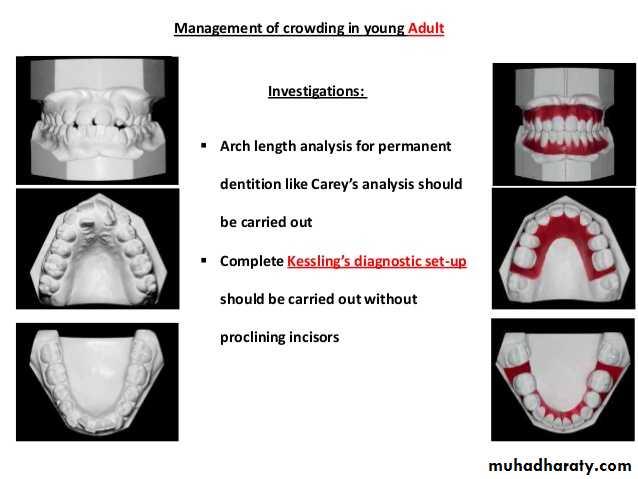
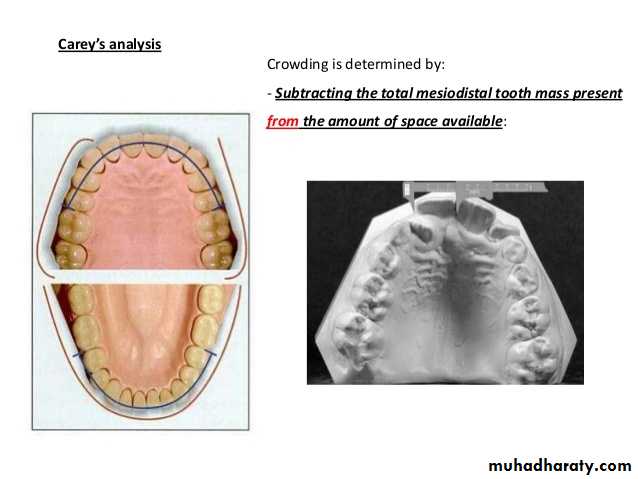
Dental Crowding
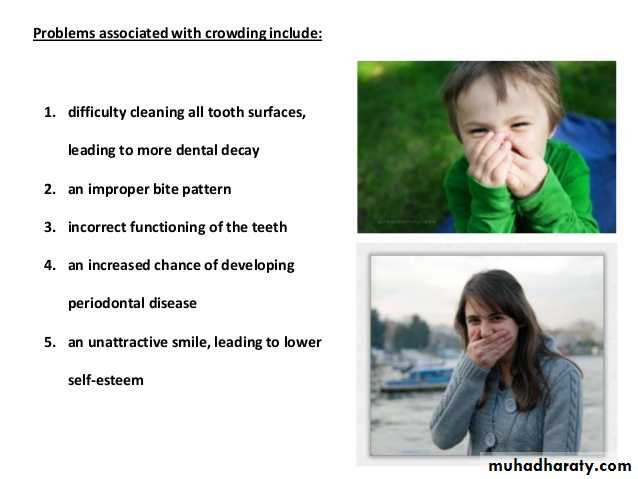
Definitioncrowding is a condition where there is malalignment of teeth caused by inadequate space
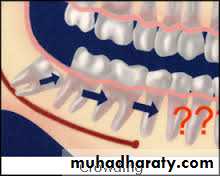
Crowding: lack of space for a permanent tooth to erupt. Those teeth that erupt last in segment, e.g. lateral incisors, upper canines, 2nd premolars, 3rdmolars are most commonly affected
Dental Crowding
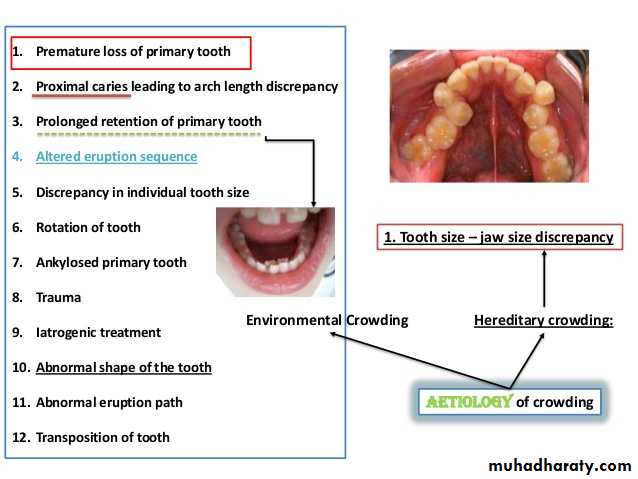
Dental CrowdingAetiology of crowding
Dental Crowding
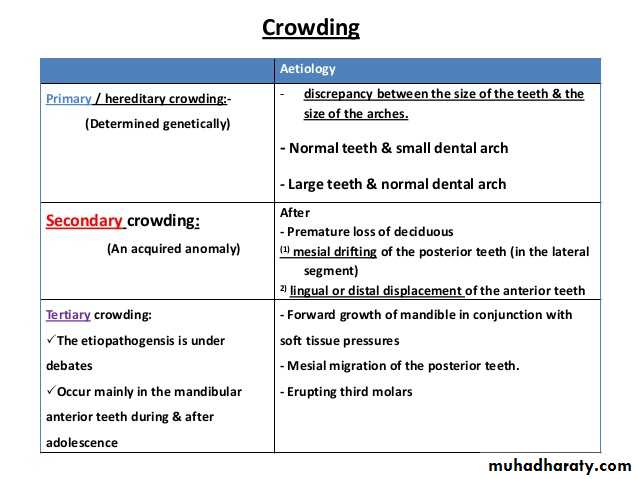
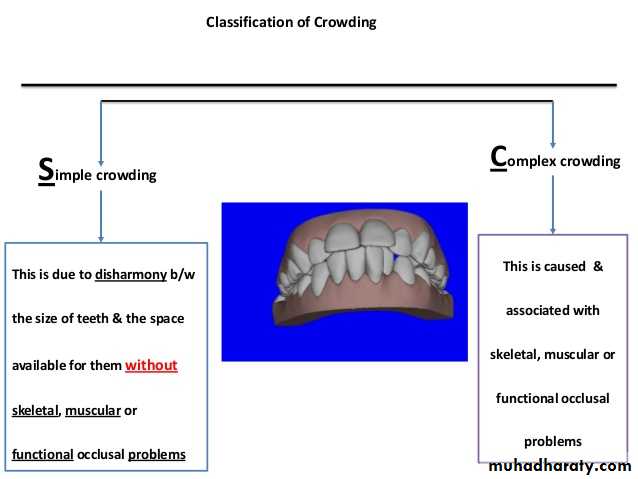
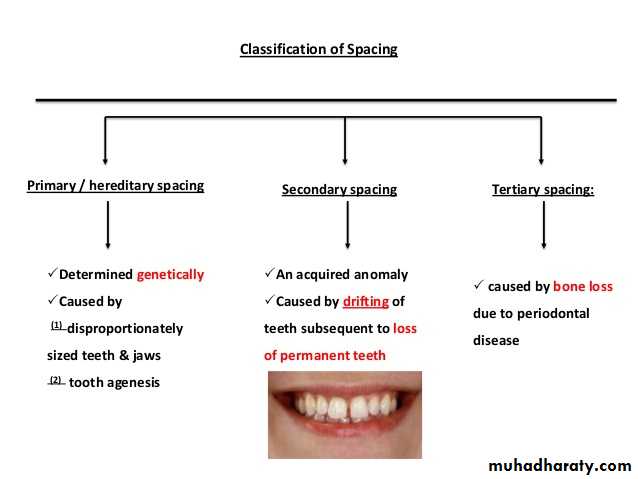
Classification of crowdingthere are different methods of classification of crowding1-according to the sourcehereditary crowding
enviromental crowding
Primary crowding
Secondary crowdingTertiary crowding
2-according to the time of appearance
Tertiary crowding
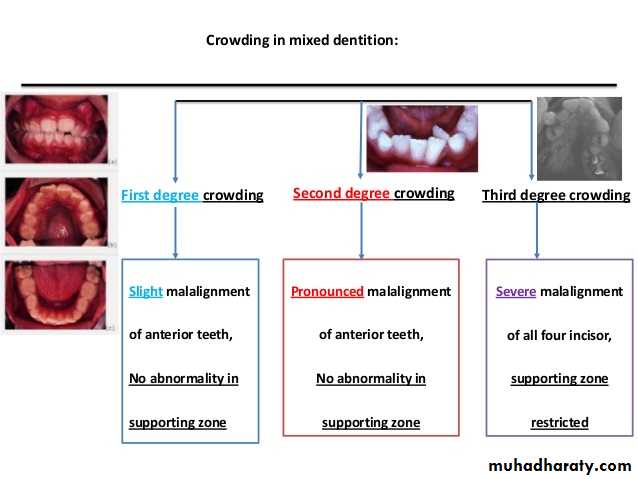
3-according to the severity
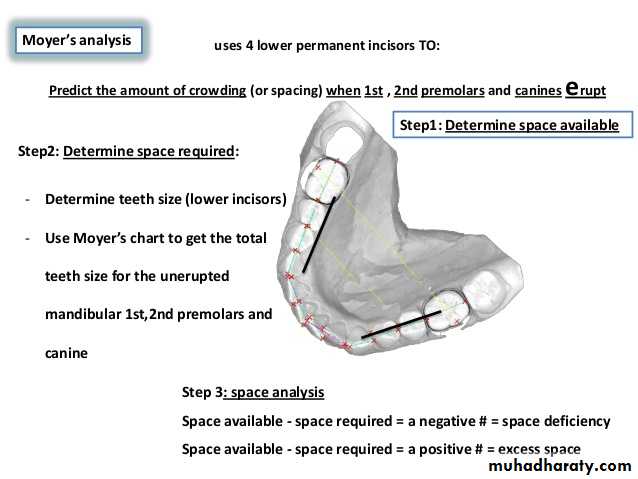
Moyer's prediction table
Use four mandibular incisor to predict the distance of lower , the maxillary canine, premolar from mesial to distal .Low incisor 19.5 20.0 20.5 21.0 21.5 22.0
maxillary 20.6 20.9 21.2 21.3 21.8 22.0
mandibular 20.1 20.4 20.7 21.0 21.3 21.6
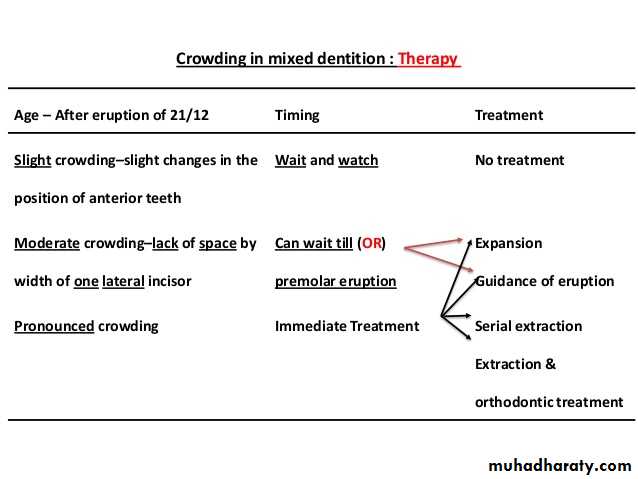
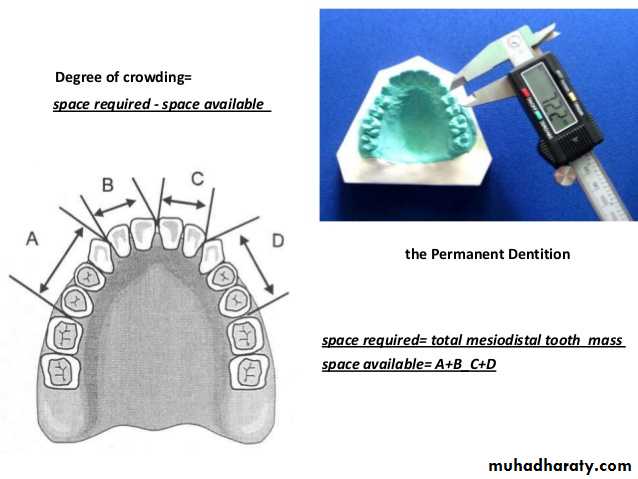
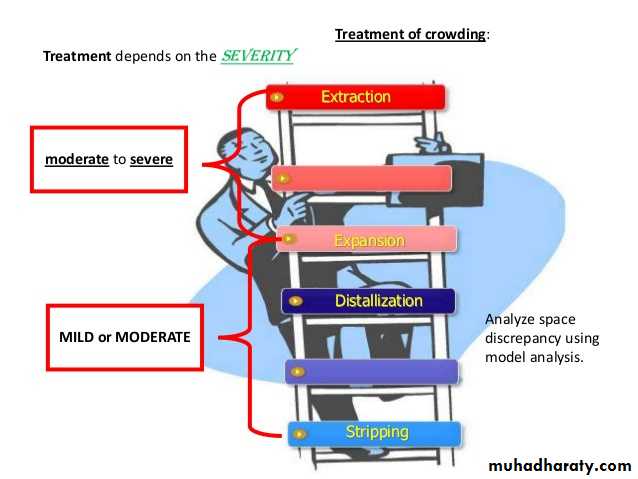
Treatments of crowding
++*
1.Mild crowding:
If the space discrepancy is upto 4mm, accepted or-Usually resolves without extraction
-Proximal stripping
2. Moderate crowding:
If the space discrepancy is in the range of
5-9mm,treated without extractions by:
-Arch expansion ,lip bumpers
-Molar distalization or anchorage
-Enamel reduction. Or by extractions
Crowding of teeth
3. Severe crowding:Patients with space discrepancy of 10mm or more,
-Extraction of all first premolars+space maintenance
Treatment of Crowding
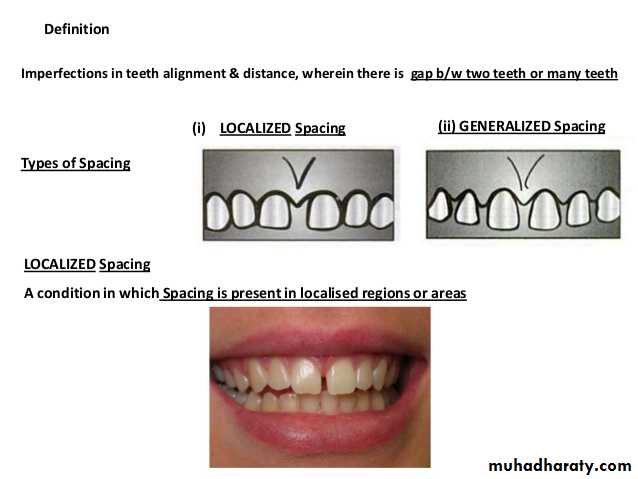
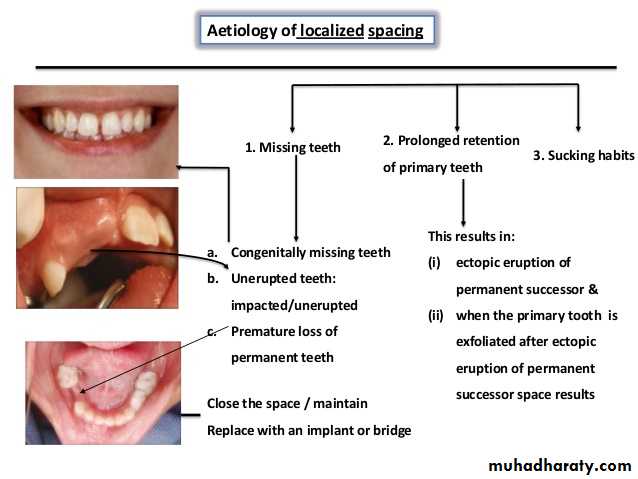
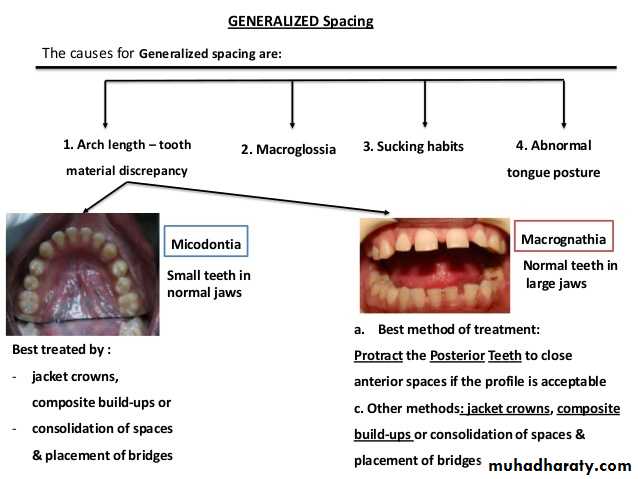
Dental spacing
Dental spacing
MIDLINE DIASTEMA
DEFINATION OF DIASTEMAA space between adjacent teeth is called a diastema.
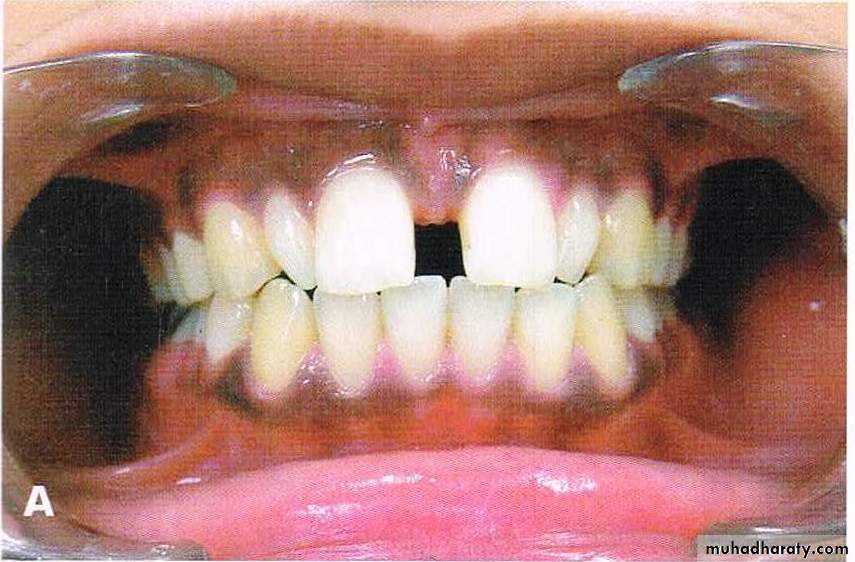
DEFINATION OF MIDLINE DIASTEMAMidline diastema refers to anterior midline spacing between the two central incisors.
47
ETIOLOGY OF MIDLINE DIASTEMA
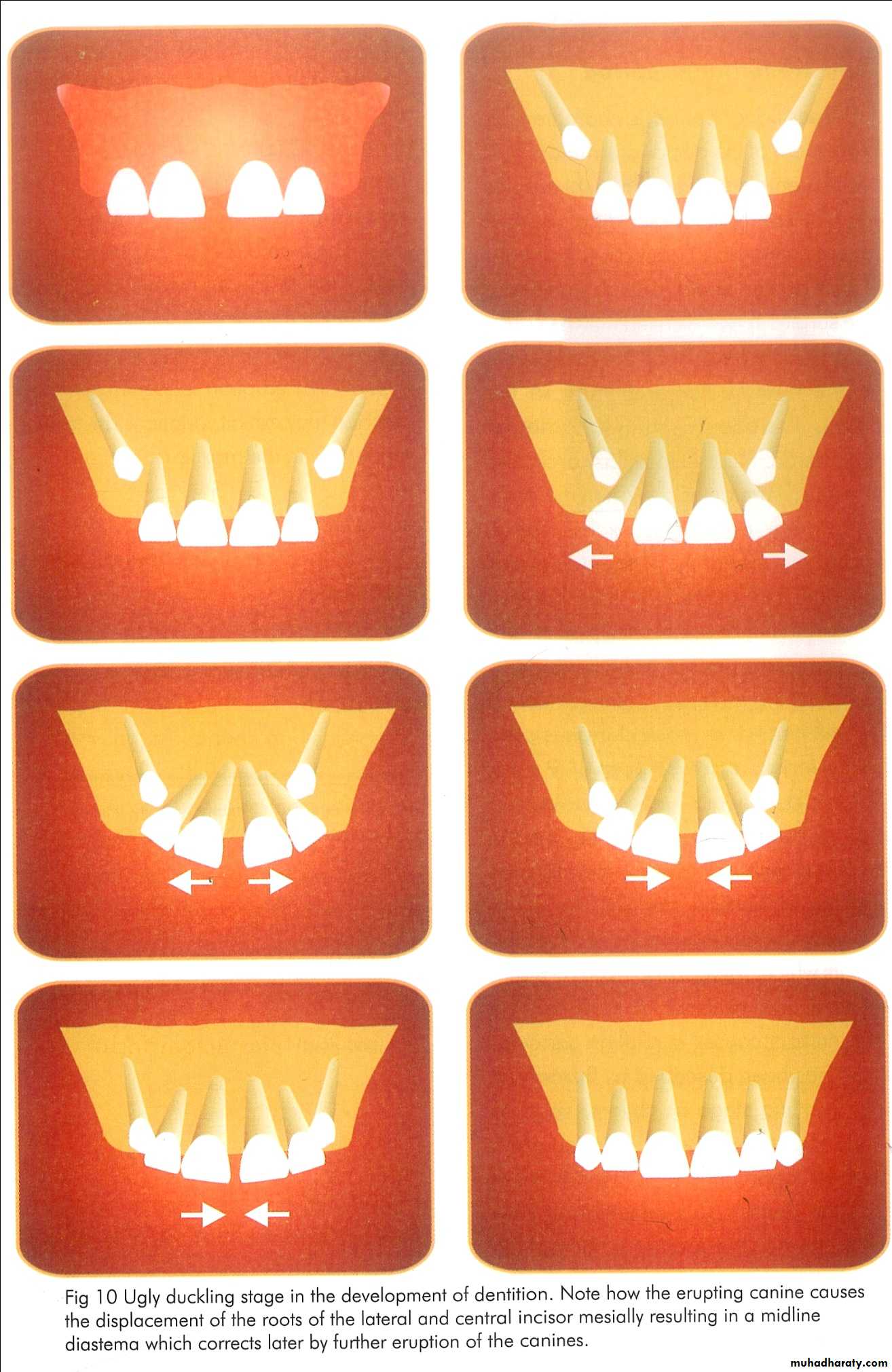
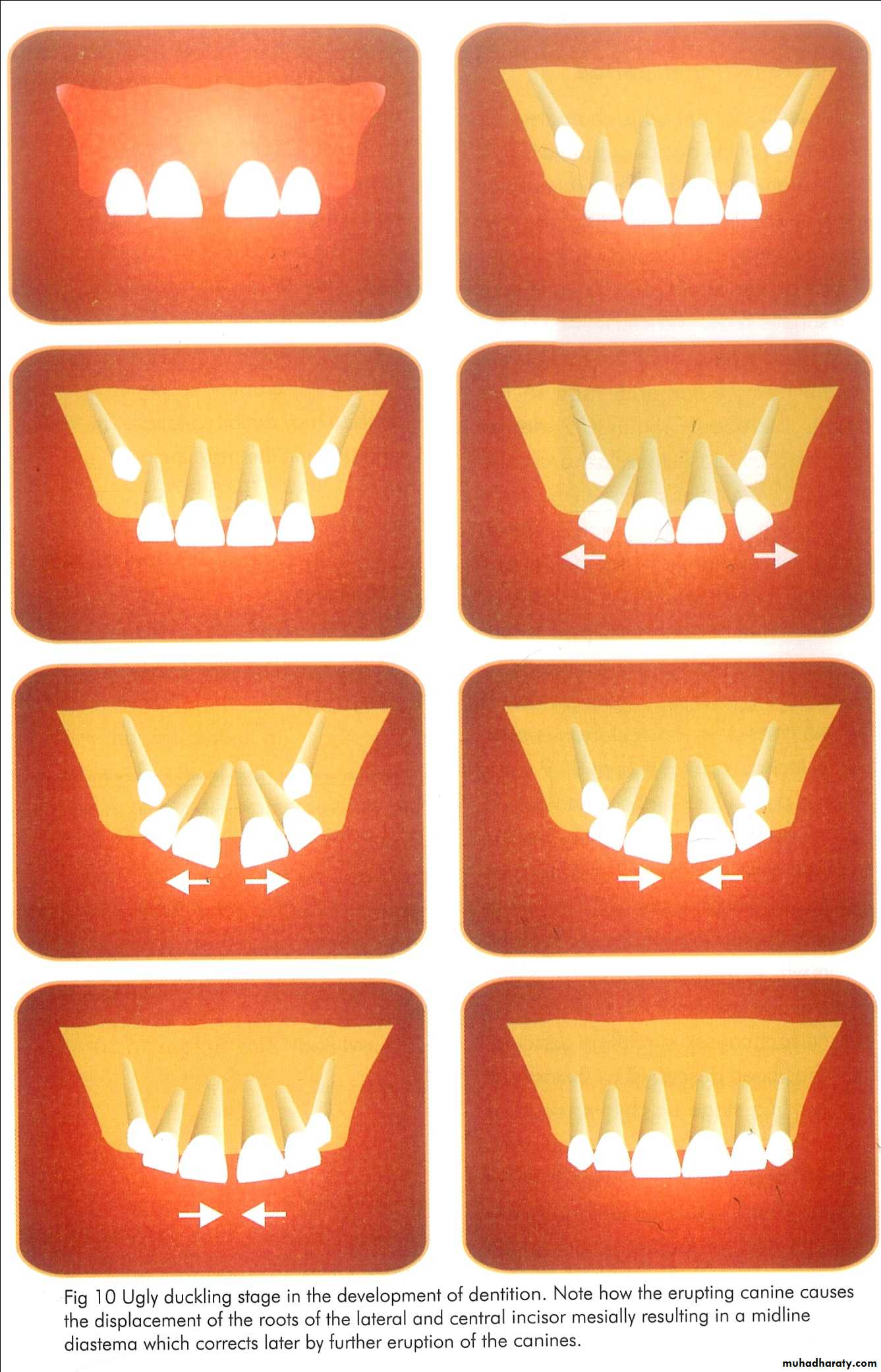
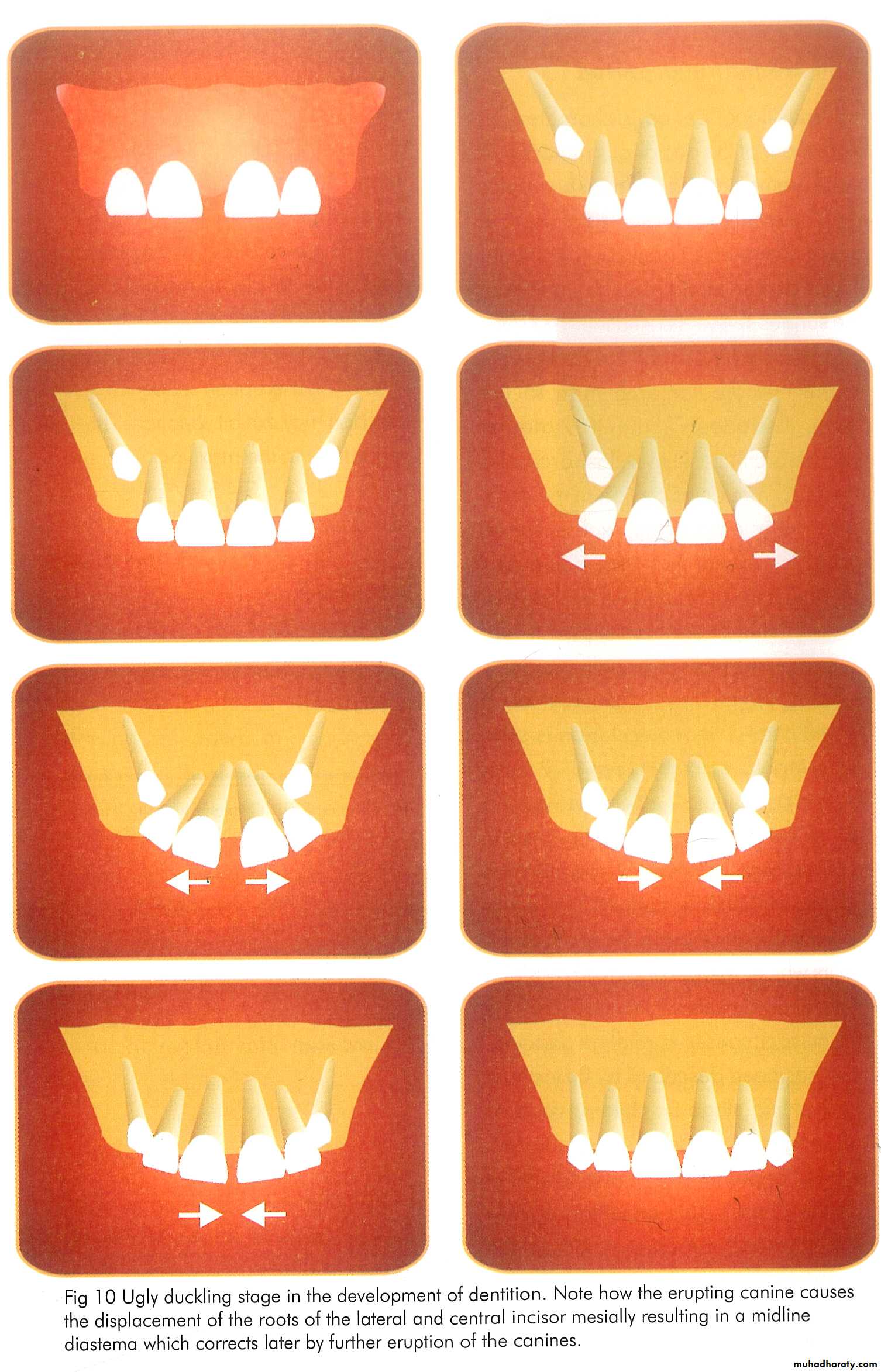
• NORMAL DEVELOPING DENTITION• Physiologic median diastema/ ugly duckling stage
• Ethnic and familial
• Imperfect fusion of midline of premaxilla
2. TOOTH MATERIAL DEFICIENCY
• Microdontia
• Macrognathia
• Missing lateral
• Peg laterals
• Extracted tooth
48
49
3. PHYSICAL IMPEDIMENT
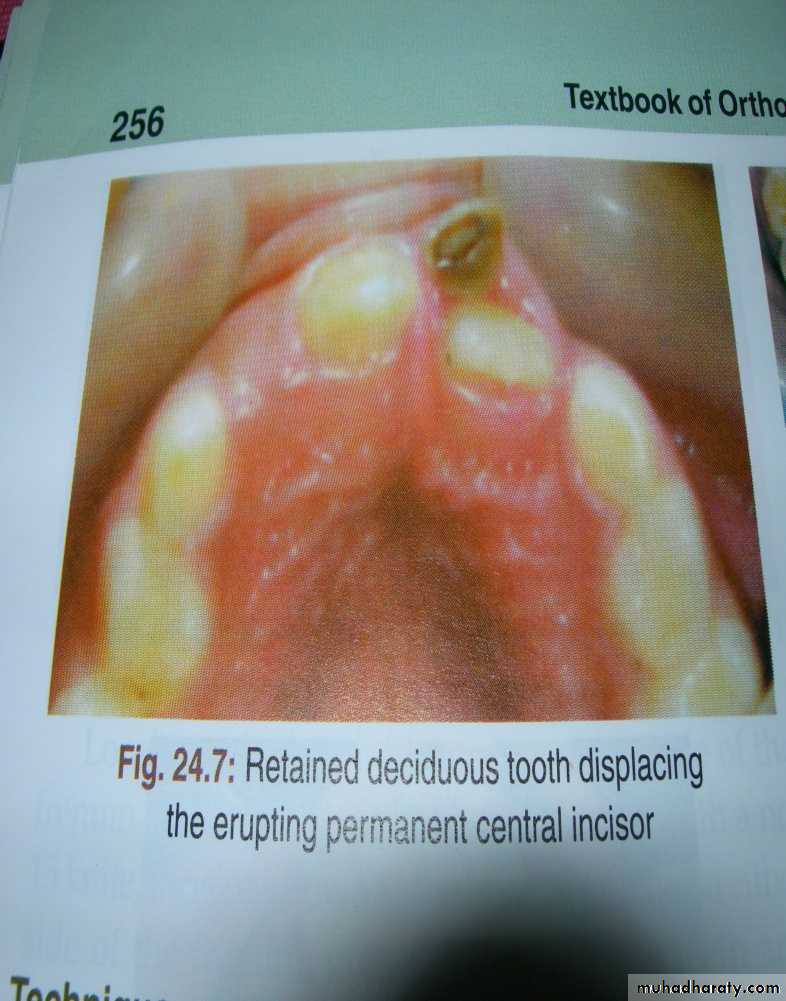
• Retained deciduous
• Mesiodens
• Abnormal labial frenum
• Midline pathology
• Deep bite
4. HABITS
• Thumb sucking• Tongue thrusting
• Frenum thrusting
• ARTIFICIAL CAUSES
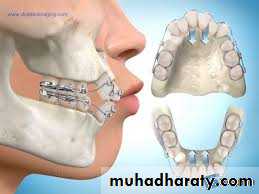
Rapid maxillary expansion1. NORMAL DEVELOPING DENTITION
50a) Physiologic median diastema/ ugly duckling stage
It is a transient or self correcting malocclusion which is seen in the maxillary incisor region between 8-9 years. It is particularly seen during the eruption of the permanent canines.
51
52
b) Ethnic and familial
Certain group of peoples, especially negroid groups exhibit median diastema as an ethnic norm.
c) Imperfect fusion at the midline
Median diastema occurs due to imperfect fusion at the midline of the premaxilla.
2. TOOTH MATERIAL DEFICIENCY
53a) Microdontia
54
b) macrognathia
c) Missing lateral.
d) Extracted tooth
.3. PHYSICAL IMPEDIMENT
55
a) Retained deciduous teeth.
This causes ectopic eruption of tooth and formation of median diastema.
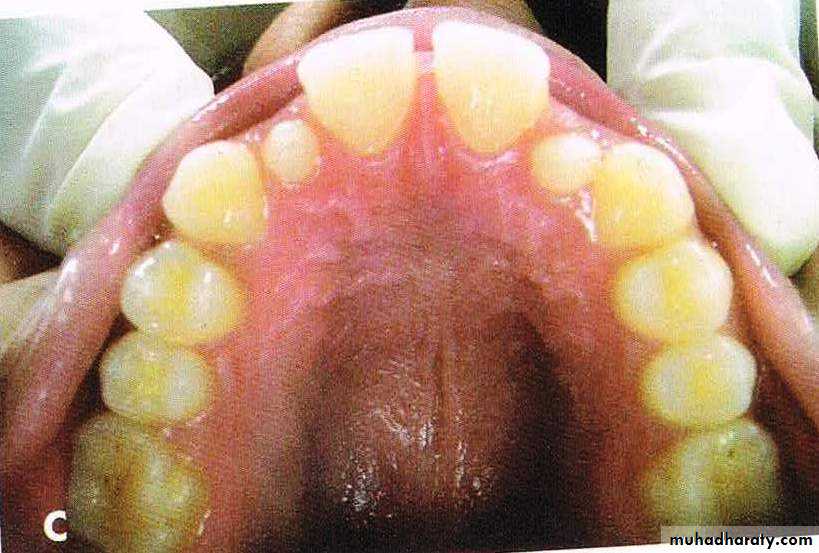
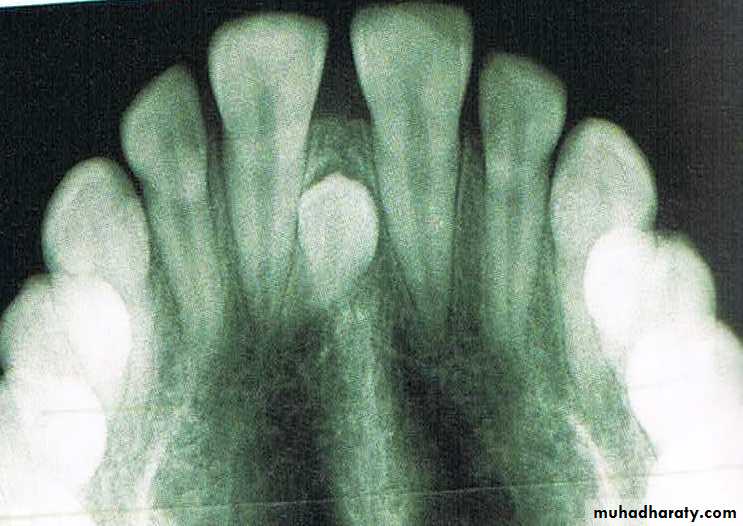
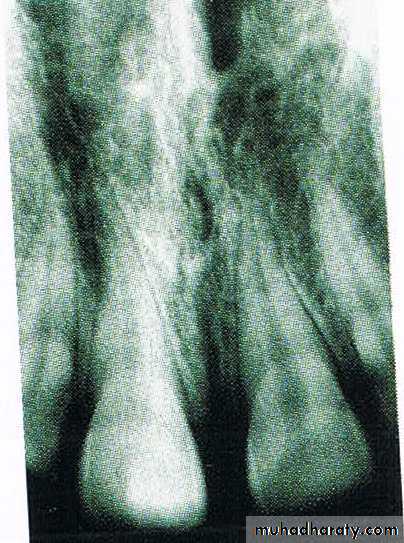
b) Mesiodens
Presence of an unerupted mesiodens between the two central incisors also predispose to midline diastema.56
c) Abnormal labial frenum
The presence of a thick and fleshy labial frenum can cause a midline diastema.This type of fibrous attachment can prevent the two maxillary central incisors from approximating each other.
d) Midline pathology
Soft tissues and hard tissue pathologies such as cysts, tumors and odontomes may cause midline diastema.
4. HABITS
57a) Thumb sucking
Thumb sucking is defined as placement of the thumb or one or more fingers in various depths into the mouth.
It can cause severe proclination of the maxillary anterior teeth along with formation of diastema
b) Tongue thrusting
This is a condition in which the tongue makes contact with any teeth anterior to the molars during swallowing.
It also causes proclination of anterior teeth along with diastema and open bite.
c) Frenum thrusting
This habit is a self injurious habit.
If the maxillary incisors are slightly spaced apart, the child may lock his labial frenum between these teeth and permit it to remain in this position for several hours.
58
5. ARTIFICIAL CAUSES/ IATROGENIC CAUSES
59Rapid maxillary expansion
With rapid expansion at a rate of 0.5 to 1 mm/day 1 cm or more of expansion is obtained in 2 to 3 weeks.
A space is created at the mid-palatal suture which is filled initially by tissue fluids and hemorrhage, and the expansion is highly unstable.
The opening of the mid-palatal suture is fan-shaped or triangular with maximum opening at the incisor region and gradually diminishing toward the posterior part of the palate.
As a result there is incisor separation and a midline diastema is formed.
This diastema closes as a result of the trans-septal fibre traction.
60
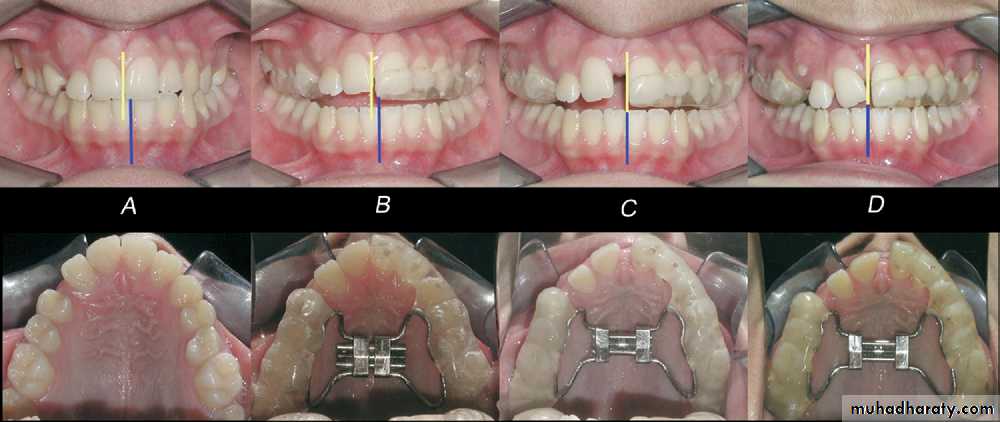
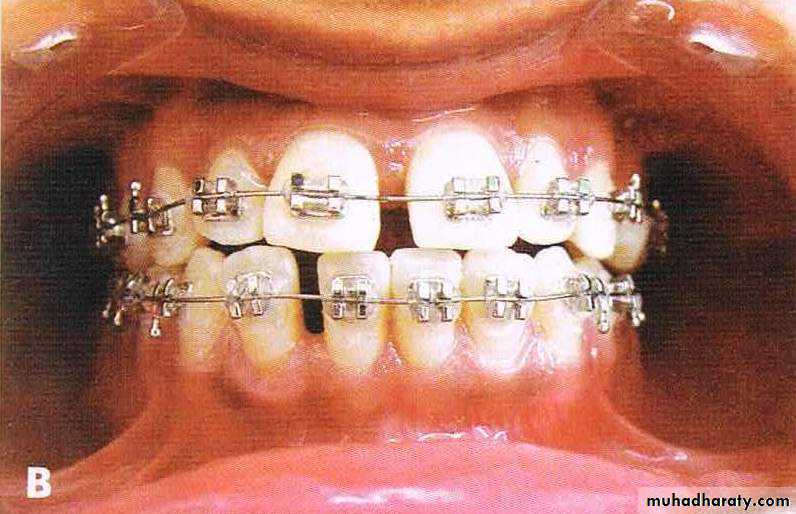
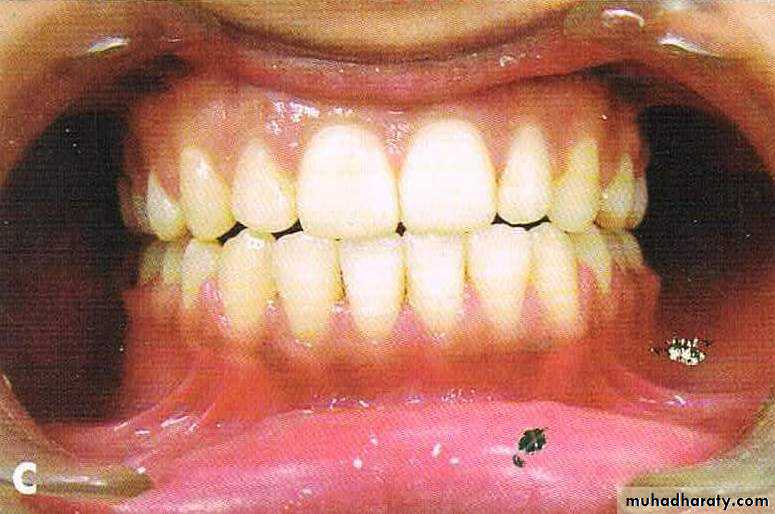
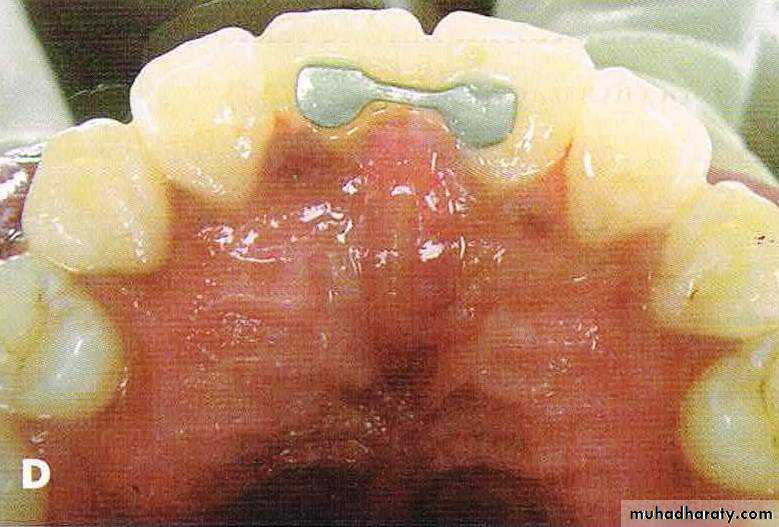
A, Bilateral constricted maxilla with upper midline shift; B, type 1 RME appliance in mouth;
C, end of expansion; D, correction of upper midline shift at end of retention period.
DIAGNOSIS
61• a. A proper history and clinical examination should be done.
• b. Measure the mesiodistal width of the teeth which will help in determining the tooth material-arch length discrepancies.
• c. BLANCH TEST:- Lift the upper lip and pull in outward and look for blanching of the soft tissues lingual to and between two central incisors.
• Presence of blanch indicates high frenal attachment as cause of midline diastema.
• d. check for any pernicious oral habits
• e. periapical radiograph:- presence of notching in the interdental bone is a diagnostic of a thick and fleshy frenum.
• f. midline radiographs will help in diagnosing midline pathology.
62
MANAGEMENT
• REMOVAL OF CAUSE
• ACTIVE TREATMENT• RETENTION
1. REMOVAL OF CAUSE
63• DIASTEMA DUE TO UGLY DUCKLING STAGE
• No treatment required
• DIASTEMA DUE TO IMPERFECT FUSION AT THE MIDLINE Excision of included interdental tissue between the incisors.
• A flap is raised interdentally and fissure bur inserted gently into the cleft. With the bur, the included tissues are removed and flap sutured. An orthodontic appliance for closure of median diastema is given during healing process.
64
DIASTEMA DUE TO MICRODONTIA AND MACROGNATHIA
Such conditions can be treated by orthodontic means or by mean of jacket crowns or composite build-up.
DIASTEMA DUE TO MISSING TEETH/EXTRACTED TOOTH
Space can be consolidated and replaced with implant or bridge65
• DIASTEMA DUE TO RETAINED DECIDUOS TEETH/MESIODENS
• The retained deciduous tooth or mesiodens should be extracted at the earliest.
• DIASTEMA DUE TO ABNORMAL FRENUM
• Frenectomy should be done to excise a thick fleshy frenum.
• DIASTEMA DUE TO MIDLINE PATHOLOGY
• Midline pathology like cysts has to be treated.
• DIASTEMA DUE TO ABNORMAL HABITS
• Habits should be eliminated using fixed or removable habit breakers.
2. ACTIVE TREATMENT
66• REMOVABLE APPLIANCES
• Simple removable appliances incorporating finger springs
• Finger springs can be given distal to the two central incisors.
• In a reciprocal tooth movement the forces are applied to teeth Fare equal and opposite as a result each unit moves to a normal occlusion.
67
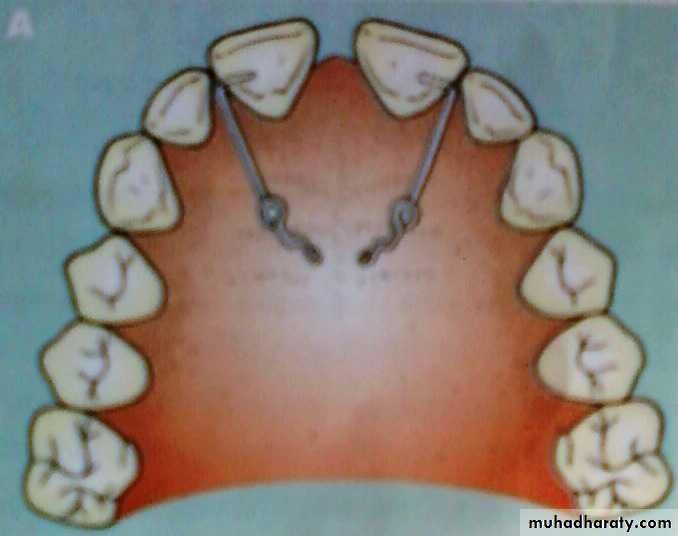
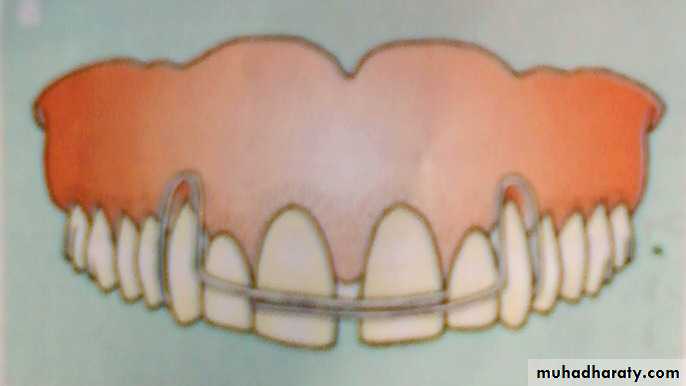
A, Closure of a midline diastema can be accomplished with a removable appliance and finger springs to tip the teeth mesially.
68
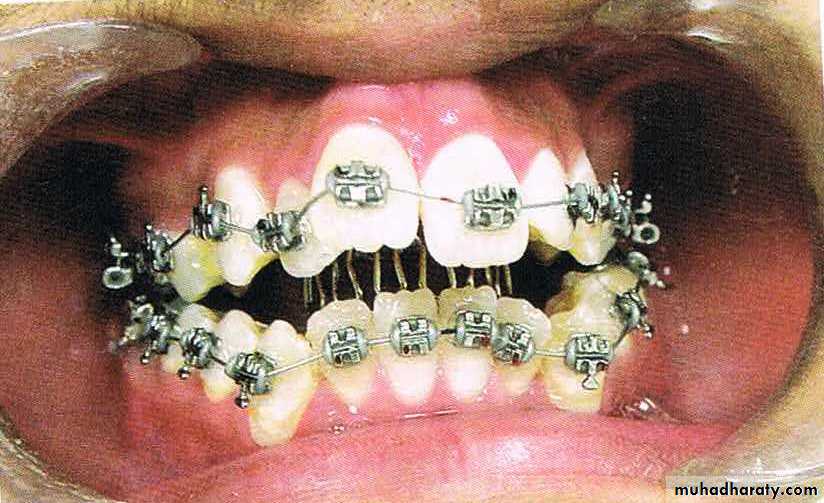
FIXED APPLIANCES
Fixed appliances incorporating elastics and springs bring about the most rapid correction of midline diastema.
69
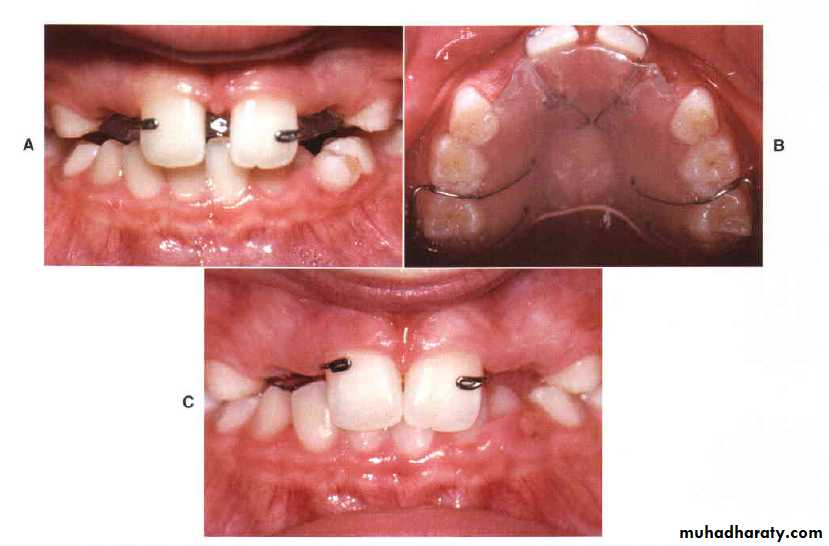
Closure of a diastema with a fixed appliance, immediately after space closure, the teeth are retained, preferably with, (D) a fixed lingual retainer at least until the permanent canines erupt.
70
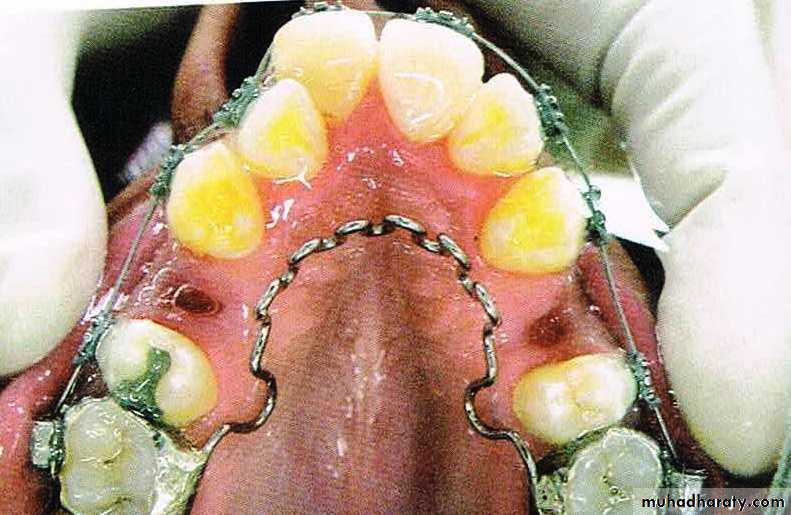
3. RETENTION
Midline diastema is often considered easy to treat but difficult to retain.
Retention can be achieved by:-Lingual bonded retainers
Hawley’s retainer
71
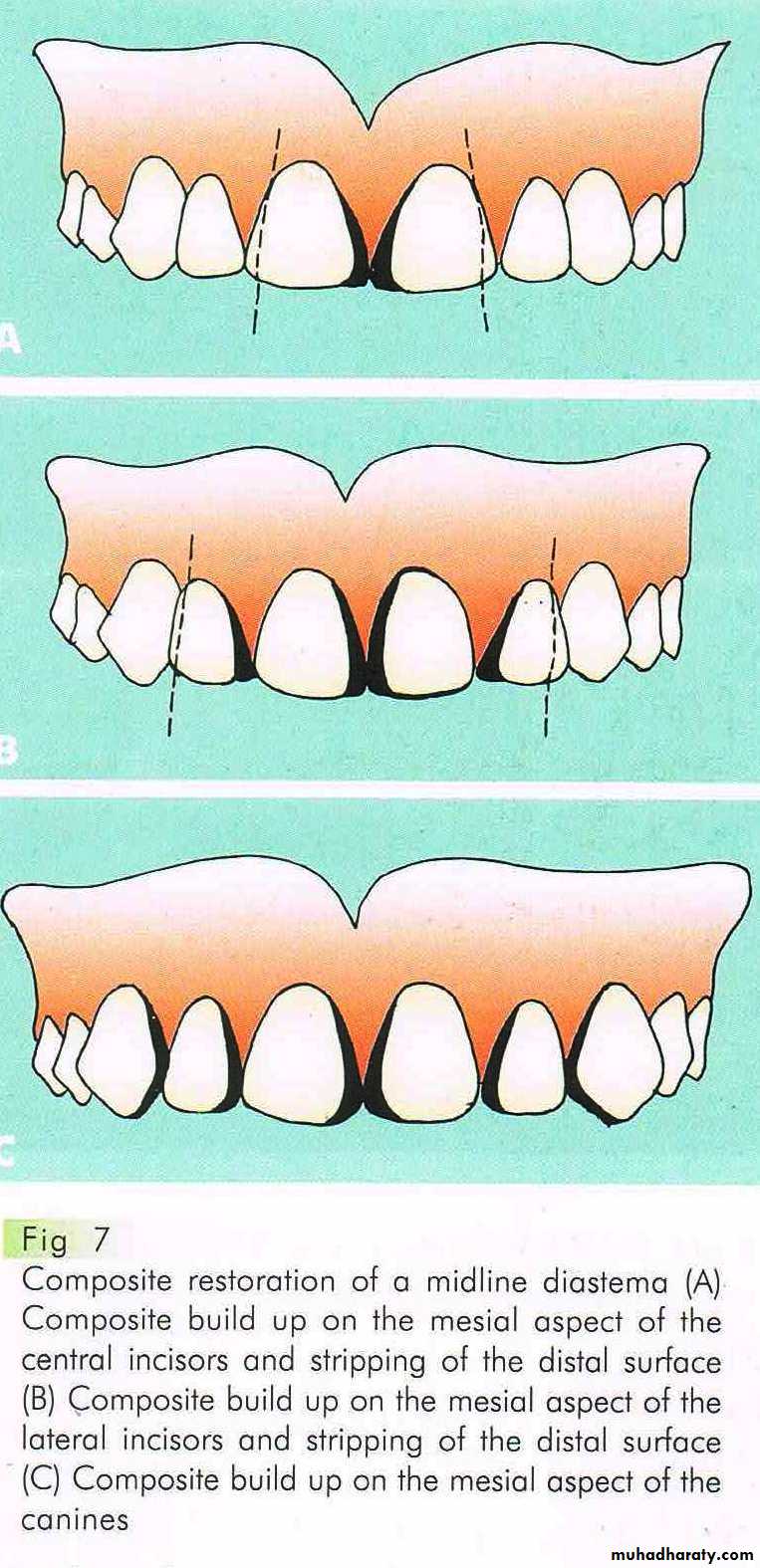
NEWER APPROACH
ROLE OF COSMETIC RESTORATION
Esthetic composite resins are used to close midline diastema especially in adult patients.
PROSTHESIS/CROWN
Presence of peg shaped laterals or teeth with other anomalies of shape and size require prosthetic rehabilitation.Missing teeth should be replaced with fixed or removable prosthesis.
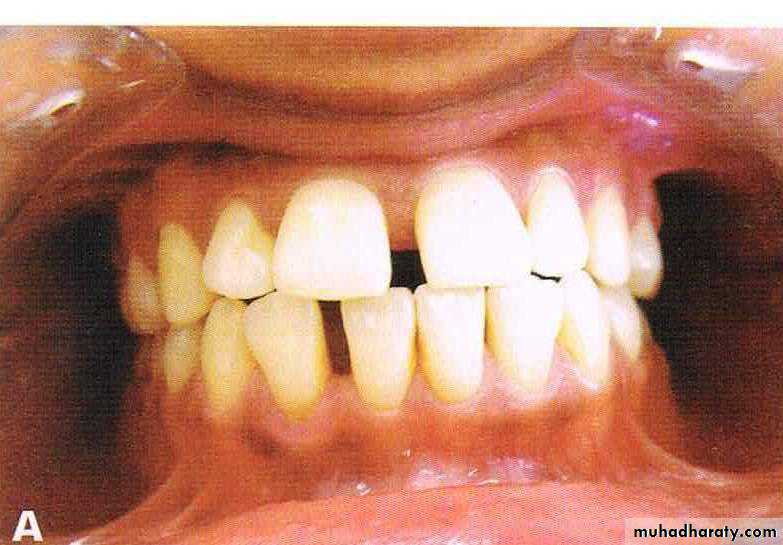
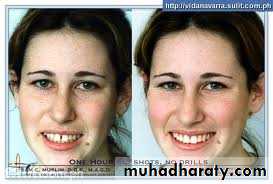
Before & after treatment
Fig: Midline diastema
Fig: Spacing73
Thank you…
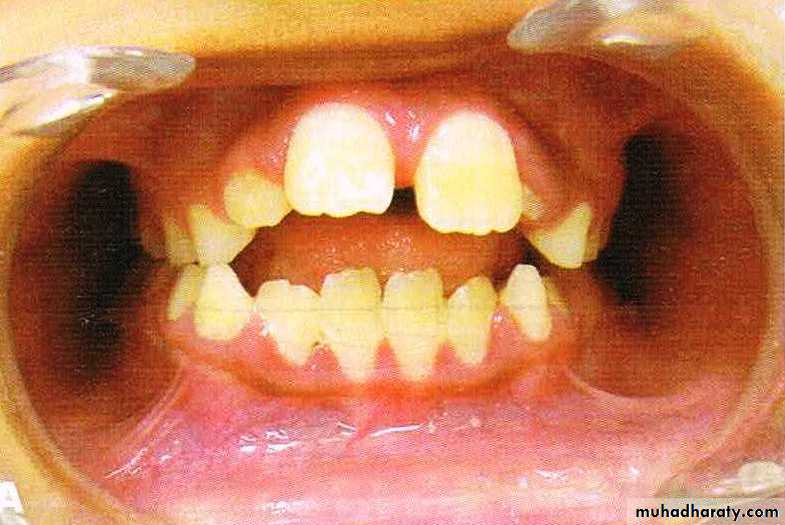
Bimaxillary protrusion
Bimaxillary proclination: the teeth are proclined on normal bases
Bimaxillary protrusion or bialveolar protrusion refers to a protrusive dentoalveolar position of maxillary and mandibular dental arches that produces aconvex facial profile .Bimaxillary prognathism: the jaws/basal bones are forward relative to the cranial base
Definition
PrevalenceMost common in Negros
It is also common among Arab groups and Asians
It is less prevalent in white Caucasian populations
• Aetiology
• 1-Soft tissue factors
Lip length
Adenoid & nasal blockage
Endogenous (primary) thrust
2-Dental factors
3-Habit factors
4-Pathological factors
Bimaxillary proclination or protrusion
Soft tissue factors
• nasal blockageSoft tissues stretching theory that where the patient can't breathe through nose, so adopt a head up posture with extension, so stretch the superhyoid muscles, skin + fascia. This in turn imparts a force on the mandible and in turn the mandible adopts a downward posture this will allow the tongue to drop and imparts less force on maxillary arch in the lateral dimension which with the unopposed action of the cheeks pushes the dentition into a narrower arch which leads to cross bite situation. At the same time the tongue will be pushed forward to increase the phyryngeal space overcoming the lip force and causing bimaxillary proclination.
Adenoids: It was proposed that the “Adenoids” were the most important “soft tissue” responsible for the difficulty in breathing through nose then the adenoids enlarged causing chronic constriction in the nasopharyx followed by the same pathway as “soft tissue stretch theory”.
tongue Occasionally the tongue is very large and is the primary cause of the bimaxillary proclination.
Lip length, activity, morphology and position : in bimaxillary proclination cases, usually the lips are full, loose and everted, and the tongue acts to mould the dental arches forward as they erupt. The effect of abnormality of soft tissues at rest is more influential than that during function
• Dental factors
Due to way of incisors eruption in a forward direction.Tooth size discrepancy has been associated
• Habit like tongue thrust
• Pathological conditions
Cerebral palsy
Haemangioma with swelling of the lips/tongue/cheeks produces a “new” zone of balance.
Untreated cleft lip or palate swings forwards
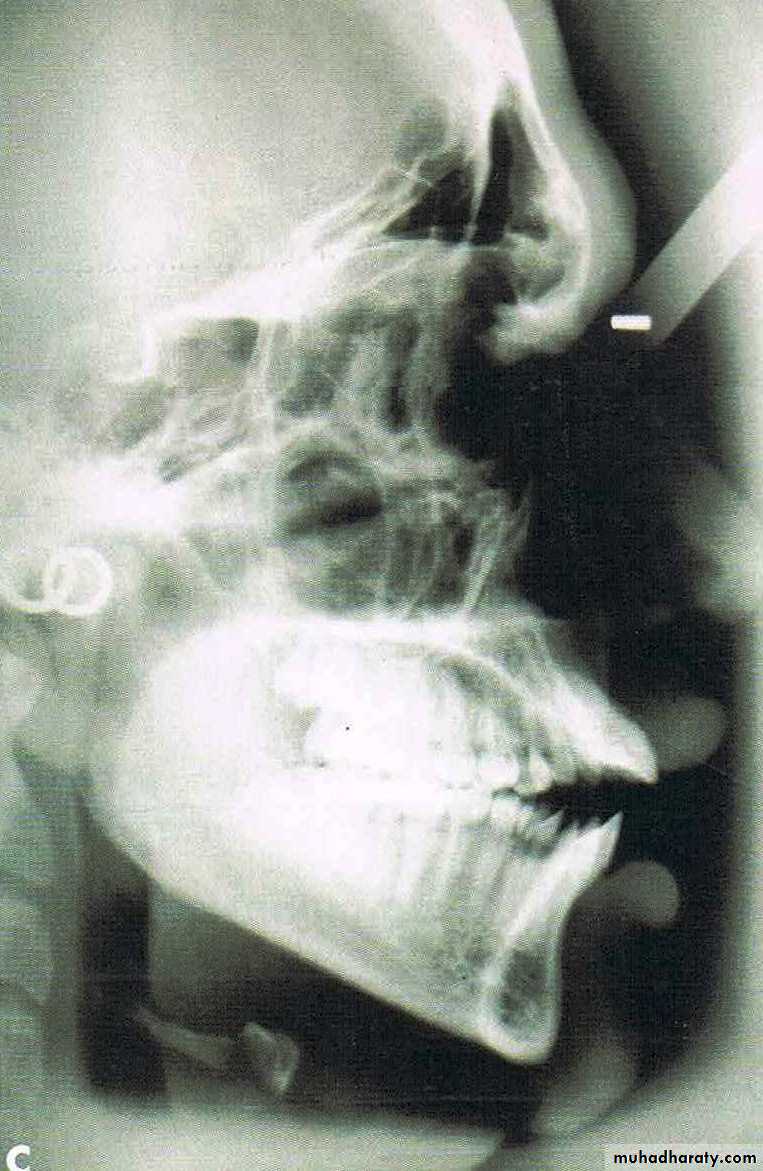
From the dental perspective, the severity of the dentoalveolar protrusion is best characterised by the interincisal angle.
• 125 degree- 115 degree = mild
• 115 degree- 105 degree = moderate
• <105 degree = severe.
Classification
Features
• Soft tissue• Convex facial form.
• Reduced lip length.
• Lips incompetency.
• Low lower lip line and high upper lip line
• prominent lips.
• Receded chin.
• Dental
• Dental bimaxillary proclination• Larger dental arch length with resultant spacing and diastema
• Normal or increased OJ
• Variable molar relationship but usually normal.
• Large teeth compared to normal population
• May have other superimposed malocclusion
Normal aims for any orthodontic treatment including:
• Relieve of crowding• Alignment and levelling
• Close diastema and spacing
• Normal OJ and OB
• Correct incisor relationship
• Normalization of buccal occlusion
• Maintain a stable result
Aims for treatment of bimaxillary proclination
Other facial aims including;Improving facial aesthetics i.e. flatten profile.
Enabling lip competence
Mild cases
Better to accept becauseAging can mask the protrusion by down and forward growth of the nose and chin
The high risk of relapse.
Treatment
• Moderate casesEnmass retraction with or without & extraction
Extraction in both arches usually first premolars.
If the condition is class II then it might be treated with extraction in the upper alone.
• In severe cases
Orthognathic surgery is required to correct significant skeletal problems using subapical osteotomies with extraction and with or without Genioplasty.Stability & Relapse
30% of cases showed almost relapse.Long-term stability is unpredictable, depends on lip adapting to incisor retraction, i.e. lower lip becoming competent
Permanent fixed retainer in both archs
• The aims for a good stability at the end of treatment should be:
Interincisal angle should be normalized
Lower lip should cover one third of upper incisor
If the tongue is very large, then surgical reduction can be justified
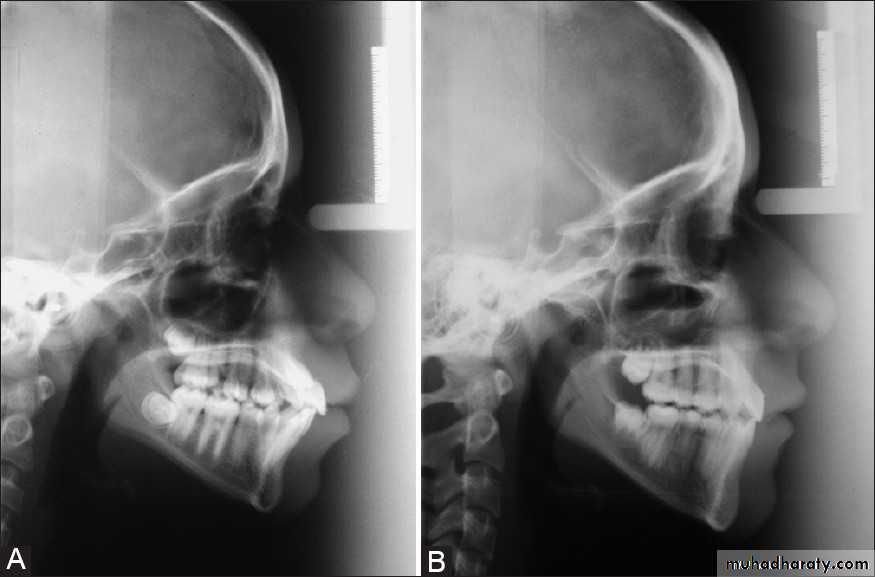
Before & After Treatment