ENDODONTIC EMERGENCIES
1• DEFINITION :-
• EMERGENCY: Defined as a sudden, urgent, usually unexpected occurrence requiring immediate action. Endodontic emergencies are circumstances associated primarily with Pain and or Swelling that require immediate diagnosis and treatment.2
• Most of the emergencies are unscheduled.
• Although, all forms of medical emergencies may develop in dental practice. These are situations produced entirely by stress or those that are acutely aggravated when the patient is under stress.3
The reason for endodontic emergency treatment is PAIN and at times SWELLING arising from pulpo-periapical pathosis. Because dental pain has many causes, the clinician must diagnose the origin of pain as quickly as possible to render rapid and effective relief.
SUBJECTIVE SYMPTOMS : Which is the chief complaint of patient eliciting either:
1) Pain2) Swelling
3) Lack of function
4) Esthetics
DENTAL HISTORY
MEDICAL HISTORY
4OBJECTIVE SYMPTOMS
Which are determined by tests and observations performed by clinicians.The tests are as follows:
• Visual Inspection.
• Percussion apical and lateral.
• Palpation.
• Mobility and Depressibility.
• Radiographs.
• Electric pulp test
• Thermal tests
- Hot
- Cold
• Anesthetic test
• Cavity test
5
6
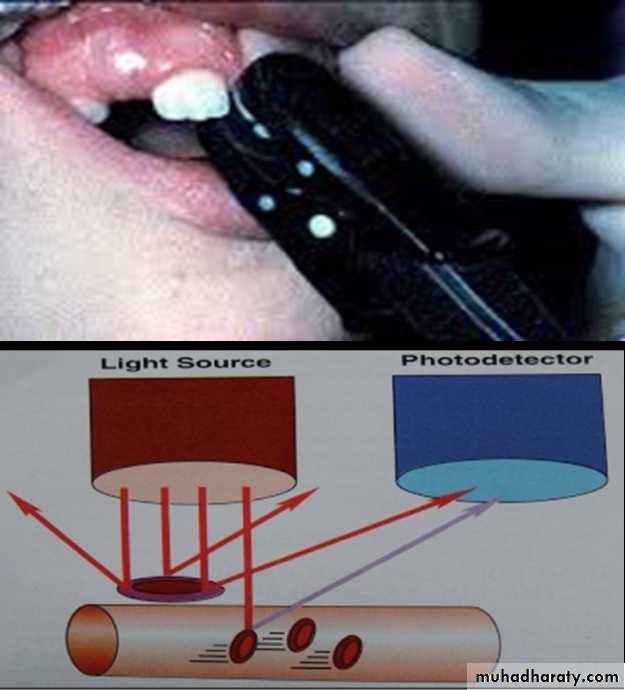
Modern method for diagnosis of pulpal vitality
1-Pulse Oximetry2-laser Doppler Flowmetry.
• Acute reversible pulpitis
• Acute irreversible pulpitis• Acute apical periodontitis.
• Acute apical abscess.
• Phoenix abscess.
7
If bacteria gain access to root canal of necrotic teeth they can create a significant colony before the body’s immune system knows about their presence.
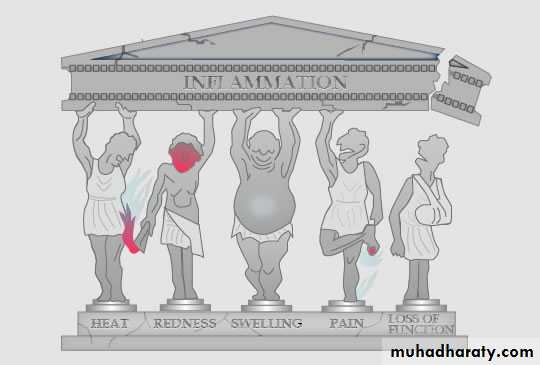
Large bacterial colonies are capable of producing a significant amount of tissue destroying enzymes and acids and toxins, when the immune system begins to fight the infection the bone and soft tissues around the tooth become tender on percussion and become hot to touch.
8
The pain management is the most critical factor which affects the prognosis of the treatment.
To obtain an adequate anaesthesia of inflamed tissues is the challenge.
Maxillary anaesthesia is easier to obtain by giving infiltration or block injections in the buccal or palatal region.
For adequate pulpal anaesthesia in the mandible, inferior alveolar, lingual and long buccal injections are preferred.
9
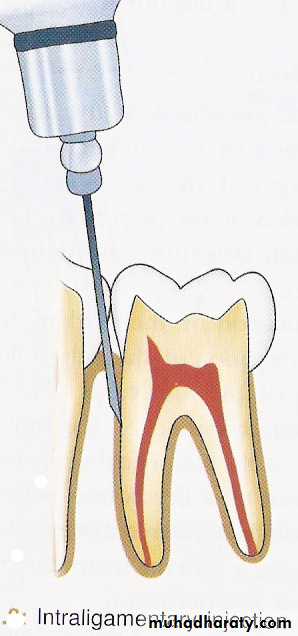
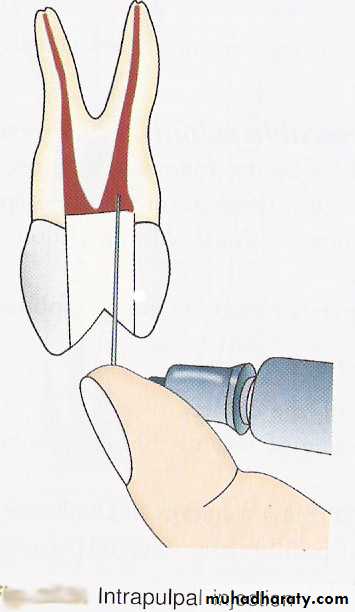
If anaesthesia is required in the lower premolars, canine and incisor, then other alternative techniques such as mental nerve block, periodontal ligament injection, intraosseous anaesthesia and intrapulpal injection are given.
10
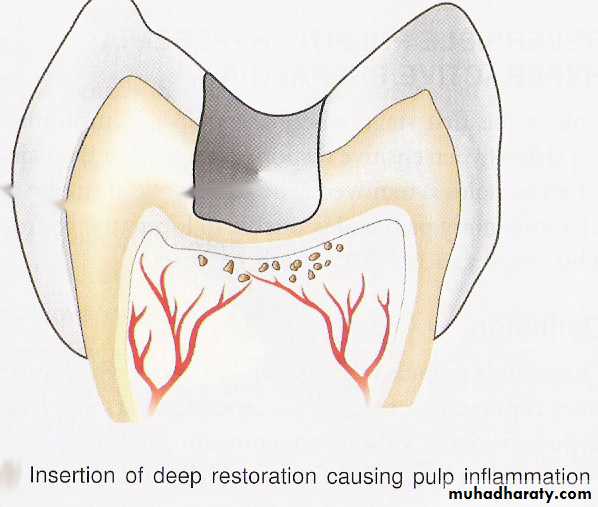
ACUTE REVERSIBLE PULPITIS:-[Hyperemia]
DEFINITION:It is a mild to moderate
inflammatory condition of the
pulp caused by noxious
stimuli in which the pulp is
capable of returning to the uninflamed state
following removal of the stimulus
11
Symptoms:
A.R.P. is characterized by:• Sharp pain lasting for a moment.
• Shooting pain lasting for short-duration.
• Pain brought on by cold beverages and sweets.
• Clinically – the patient can identify the tooth by pointing to it.
12
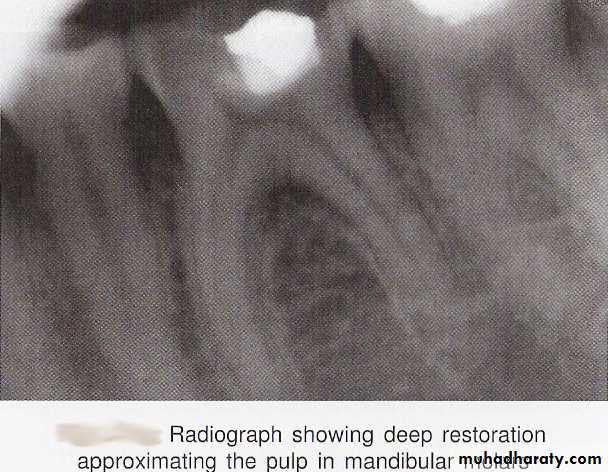
ETIOLOGY:-
1.Caries Lesions which are close to pulp can cause mild to moderate sensitivity to patients.Treatment Caries excavation and placing a sedative cement like dycal and zinc oxide eugenol (IPC).
2.Recent restoration which has a premature contact point.
Treatment Recontouring or removal of high spot.13
4.Recurrent caries under an old restorations.
Treatment Remove all caries and replace with a sedative cement.
5.Thermal shock from preparing a cavity with a dull bur or keeping the bur in contact with the tooth for a long time or low water spray can cause acute reversible pulpitis which exaggerates on placing a metallic restoration over the tooth.
3.Persistent pain and severe sensitivity after cavity preparation Suggesting chemical leakage.
Treatment Removal of restoration and placing sedative cement like ZOE.
14
TREATMENT:-
The best Rx is prevention.In a recently restored tooth, occlusion is adjusted.
In cases of marginal leakage or secondary caries ,the old
restorations are removed and replaced with sedative cement.Pain usually disappears with in several days ,if it persists
then pulp has to be extirpated15
.
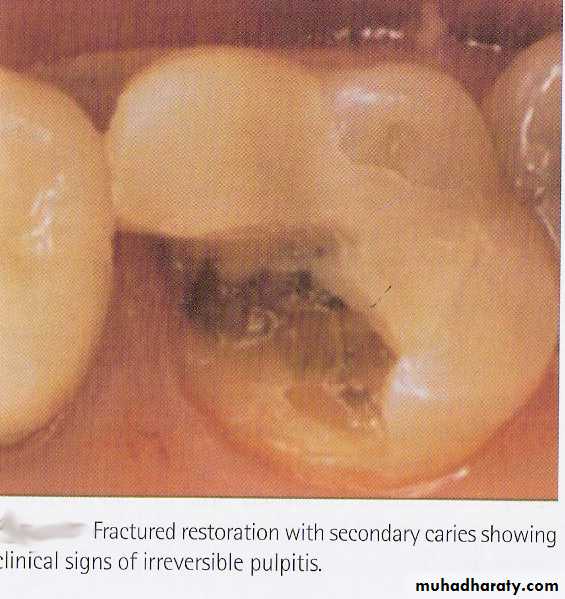
ACUTE IRREVERSIBLE PULPITIS
DEFINITION:It is a persistent inflammatory condition of the pulp, symptomatic caused by a noxious stimulus. Acute Irreversible Pulpitis exhibits sever pain usually caused spontaneously or by hot and cold stimulus
16
Symptoms:
Pain lasts for minutes to hoursIt is spontaneous.
It often continues even when the cause is removed.Pain is present even on bending over.
Patient complains of disturbed sleep.Pain is experienced on sudden temperature change.
On taking sweets or acidic foodstuff.From packing of food into cavity/food impaction.
17
Causes:
The most common cause of irreversible pulpitis is bacterial involvement of pulp through caries or from deep infra bony pocket.Reversible pulpitis may also deteriorate into irreversible pulpitis.
In irreversible pulpitis the pulp may be Vital or partially Non-vital
18Necrosis can occur partially or completely
Acute pulpitis is usually not tender but some times immunological reaction (antigen anti body) reaction occur due to bacterial toxins can reach the apex.
Vital pulp
The preferable emergency treatment is PULPECTOMY complete removal of the pulp and placement of an intracanal medicament to act as a disinfectant (RCT).In posterior teeth, where time is a factor, PULPOTOMY or removal of coronal pulp and placement of dressing (MTA, CaoH and ZOE) on the radicular pulp should be performed as an emergency treatment whereas in single rooted teeth, pulpectomy can be performed directly.
19
2. Non-Vital Pulp
Necrotic pulp rarely causes an emergency procedure.Most of the time these teeth do not respond to stimuli such as hot, cold or electric stimulation.
They may still contain vital inflamed tissue in the apical portion of root canal and also inflamed periapical tissue which causes pain.
20
ACUTE APICAL PERIODONTITIS:-
DEFINITION:-It is a painful inflammation of periodontium as a result of trauma, irritation or infection through root canal whether the pulp is vital or non vital.
CAUSES:-
Occlusal trauma
Pulpal origin infection
Blow to tooth
Over instrumentation or over filling
Symptoms: Sever pain & tenderness of the tooth, sometimes the tooth may be extruded.
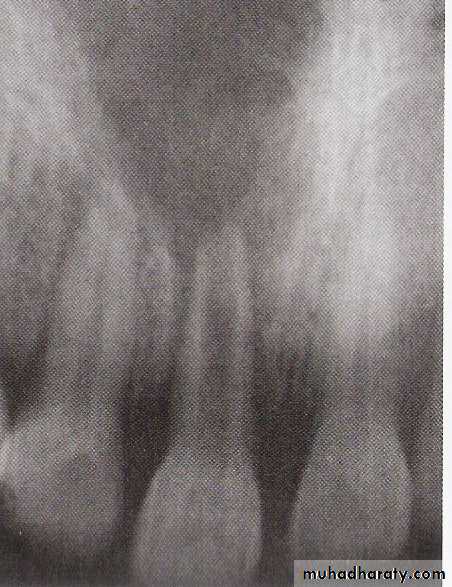
Radiographic picture: Mostly normal or mild widening of periodontal ligament.
21
Management:
• Profound anaesthesia of the involved tooth• Preparation of the access cavity
• Total extirpation of pulp in pulp chamber
• Determination of working length
• Bio-mechanical preparation
• Thorough irrigation
• Leave the tooth opened for at least 24h.
• Relieve occlusion
• Prescribe antibiotic in case of infection and analgesics to reduce pain.
• After 24h continue the RCT.
22
ACUTE ALVEOLAR ABSCESS:
Acute apical abscess.DEFINITION:
It is a localized collection of pus in the alveolar bone at the root apex following pulp death with extension of infection through apical foramen into periapical tissues.
23
The acute episode may result from:
PULPITIS that progressively developedinto pulp necrosis affecting the periapical tissues.
b) ACUTE EXACERBATION of a chronic periapical lesion Phoenix abscess
c) ENDO-PERIO lesion when the periodontal abscess secondarily affects the pulp through the lateral canals or deep infrabony pockets.24
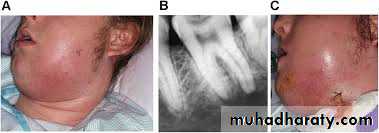
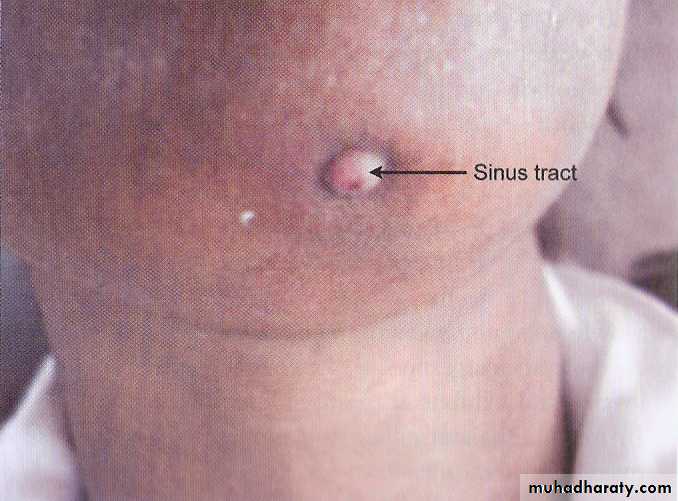
Signs and Symptoms
There are local reactions like:Tenderness of tooth.
Severe throbbing pain.
Extra oral swelling.
Sinus tract in case of chronic exacerbation.
Systemic signs and
symptoms
25
Systemic reactions are:
Elevated temperature.Gastro-intestinal disturbances.
Malaise.
Nausea.
Dizziness.
Lack of sleep.
Radiographically usually there is apical widening or radiolucency
It depend on amount of compact bone loss, not cancellous type.26
TREATMENT
The main treatment is biphasic in nature i.e.I – Debridement of canals.
II – Drainage of abscess.
The emergency treatment of acute alveolar abscess differs from acute irreversible pulpitis, as the pulp is necrotic, local anaesthesia is not required and frequently contraindicated.
Forcing anaesthetic solution into an acutely infected and swollen area may increase pain and may spread infection.
27
BLOCK MAY BE USED IN SUCH CASESMost of the pain that occurs during access cavity preparation is caused by tooth movement resulting from vibration of the bur, therefore, one should stabilize tooth with finger pressure so that the pain is reduced.
Treatment procedure follows as:
1- Access cavity preparation.
2- Profuse irrigation avoiding forcing of any solution or debris into the periapical tissue.
3- In most cases PURULENT EXUDATE escapes into the chamber and indicates that root canal is patent and draining.
4- If drainage does not occur, the apical constriction is enlarged to a minimum of 20/25 no. instrument to allow for exudate to drain because in most cases the apical constriction may prevent the drainage.
28
leaving the tooth OPEN for drainage reduces the possibility of continued pain and swelling. Open root canals permit drainage and frequently eliminate the need for surgical incision as well as routine administration of oral antibiotics and analgesics.
29
In cases where periapical drainage cannot be established, Surgical Trephination is done.
Definition:Trephination is the surgical perforation of alveolar cortical plate [over the root end] to release the accumulated tissue exudate that is causing pain.
[A small vertical incision is made adjacent to the tooth, the mucosa is retracted and No.6 round bur is used to penetrate cortical plate. This provides a drainage.]
30
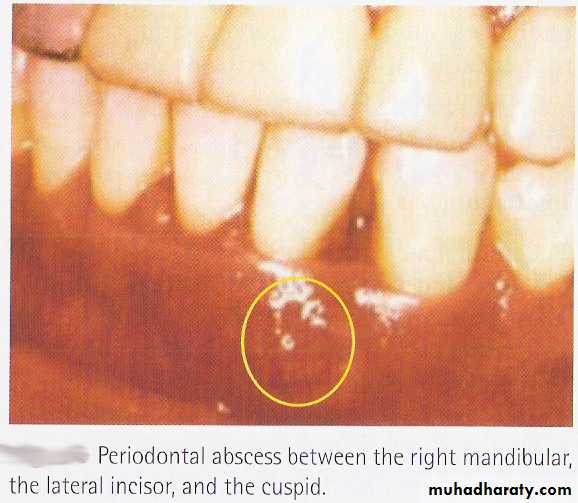
ACUTE PERIODONTAL ABSCESS
Pain and swelling
It is usually mistaken for acute
alveolar abscess
It may occur with vital or
necrosed pulp, but its origin
is usually an exacerbation
of infection with pus
formation in an existing
deep infra bony pocket.
31
DIFFERENCES
Acute apical abscess Acute periodontalabscess
• Origin—pulp
• Periodontal
• Non vital
• Vital
• No bone loss
• Bone loss
• Lesion is at the apex
• Laterally placed
• Tender on vertical percussion
• Tender on horizontal percussion
• No pocket
• Infra bony pocket
32
EMERGENCIES DURING TREATMENT
Endodontic emergencies can occur during the course of treatment.
Most emergencies are reactive phenomenon to pressure and chemical mediators created as a result of inflammatory response in periradicular tissues.
The emergencies can be due to:
1- Instrumentation beyond the root apex causing trauma to . periradicular tissue.1- When debris and microorganisms are pushed beyond the . . apical foramen which can cause an infectious reaction.
3- Chemical irritants like - Irrigating solution.
- Intracanal medicament
33
Therefore PREVENTION OF FLARE-UPS can be done by:
• The most important preventive measure is preparing the patient to accept some discomfort which should subside in a day or two i.e. psychological preparation of patients.• Using long acting anaesthetic solution.
• Complete cleaning and shaping of root canals with crown down technique.
• Administration of appropriate analgesics, prophylactic analgesics before next appointment reduces the incidence of discomfort and flare-ups.
• Leave the prepared canal opened.
34
HYPOCHLORITE ACCIDENT
Another very important but rare emergency is due to expelling of an irrigant such as NaOCl beyond the apex.This happens only by blocking the needle of the irrigating syringe in the canal and forcefully injecting the irrigant.
Within minutes the patient feels SUDDEN EXTREME PAIN.
SWELLING within minutes.
Profuse, prolonged BLEEDING through the root canal.This bleeding is the body’s reaction to the irrigant.
35
Treatment:
Allow the bleeding to continue. If the body rids itself of toxic fluid healing may be faster.Prescribing an antibiotic and an analgesic for 5-8 days respectively to avoid infected hematoma.
Since this may be hypersensitive reaction consider prescribing an antihistaminic.
36
37
THANK YOU