ISHIK UNIVERSITYFACULTY OF DENTISTRY
Oral Pharmacology2016-2017
Dr. Esra Tariq
Local AnAestheticsLocal anesthetics are employed routinely in dentistry by nerve block or by infiltration and/or regional block techniques to carry out various operative procedures.
Local anesthetics can also be classified into two categories based on their chemical structure
Local anesthetics are weak bases.
The pKa for most local anesthetics is in the range of 8.0-9.0. A balance of charged and uncharged forms is present in the body.The ratio between the cationic and uncharged forms of these drugs is determined by the Henderson-Hasselbalch equation (Log (cationic form/uncharged form) = pKa-pH).
The uncharged form is more lipophilic and thus more rapidly diffuses through the membrane. However, the charged form has higher affinity for the receptor site of the sodium channel.
a. Ester linked local anaesthetics e.g. cocaine, procaine, tetracaine, benzocaine, chloroprocaine.
b. Amide linked local anaesthetics e.g. lidocaine, bupivacaine, dibucaine, prilocaine, ropivacaine.
All the local anaesthetics possess varying degree of water and lipid solubility.
Both the properties are essential for a local anaesthetic, lipid solubility helps in migration of active drug into the neuronal fibrewater solubility is essential to get the drug to site of action from the site of administration.
Local anaesthetics block both the generation and conduction of the nerve impulse.
INJECTABLE
Low potency & short durationProcaine
Chloroprocaine
Intermediate potency & duration
Lignocaine
Prilocaine
High potency & long duration
Tetracine
Bupivacaine
Ropivacaine
SURFACE
SolubleCocaine
Lignocaine
Tetracaine
Insoluble : Benzocaine
CLASSIFICATION
Lignocaine
Mepivicaine
Prilocaine
Bupivacaine
• More intense and longer lasting anaesthesia
Cocaine
ProcaineTetracaine
Chlorprocaine
Benzocaine
Short DOA, less intense analgesia
Types of Local Anaesthetics
Esters
Amides
These get metabolized in the liver to inactive agents
Binding to amides is provided by alpha 1 glycoprotein in plamaNo allergies associated with amides
Hydrolysed in the plasma by a pseudo cholinesterase
One by-product of this reaction Para-Amino Benzoic Acid (PABA)
Allergic reaction are associated with PABA
Types of Local Anaesthetics
Esters
Amides
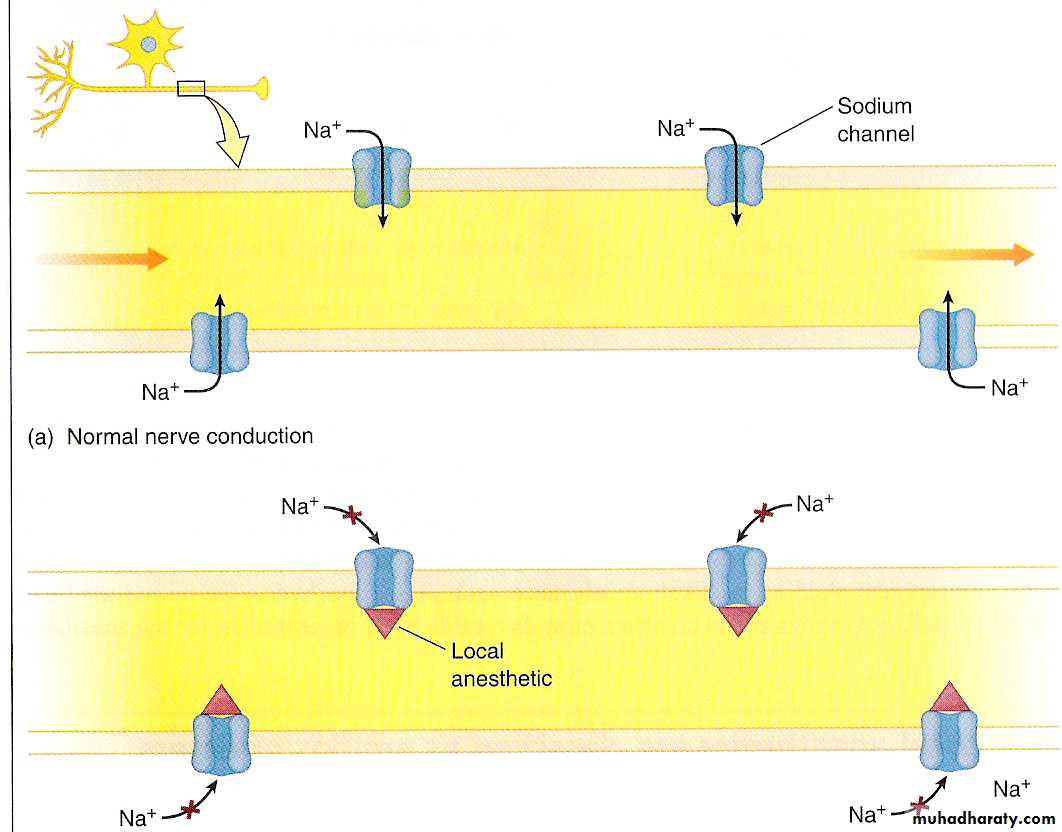
Mechanism of action
Local anesthetics reversibly bind to voltage-gated sodium channels, blocking Na+ movement through the channels, and thus block the action potential and neural conduction.At adequate dosage, these drugs should reversibly inhibit conduction of all neurons. Both pharmacological effects and most toxic effects of local anesthetics arise from this mechanism.
In simplest terms, local anesthetics bind to receptors near the sodium channel on the nerve membrane. As the amount of the local anesthetic accumulates, the sodium channels become obstructed. Impulses along the nerve are slowed, the strength and propagation of the action potential are diminished, and communication along the fiber is blocked.
Larger nerves require larger doses of the local anesthetic to achieve this effect
The uncharged form of local anesthetics is more likely to penetrate the membrane but the charged form is more active in blocking the Na+ channel.
At high pH, most local anesthetics are uncharged but also have a lower affinity for the sodium channel.
At very low pH, there is a higher percentage of charged molecules which reduces the effects of the drugs as they are less likely to enter cells.
Peripheral nerve functions are not affected equally by local anesthetics.
Loss of sympathetic function usually is followed by loss of temperature sensation; sensation to pinprick, touch, and deep pressure; and motor function. This phenomenon is called differential blockade.Differential blockade is the result of a number of factors, including the size of the nerve, the presence and amount of myelin, and the location of particular fibers within a nerve bundle.
Differential blockade
PHARMACOLOGICAL ACTIONS
CNS :
All can produce CNS stimulation followed by depression.
Cocaine:
Euphoria-excitement-mental Confusion-tremors-muscle Twitching-convulsions- Unconciousness -resp. Depression.
Procaine, Lignocaine: safe at clinical doses
CVS :
Cardiac depressant at iv doses
Antiarrhythmic action (procainamide)
Techniques of administration
Topical AnesthesiaInfiltration
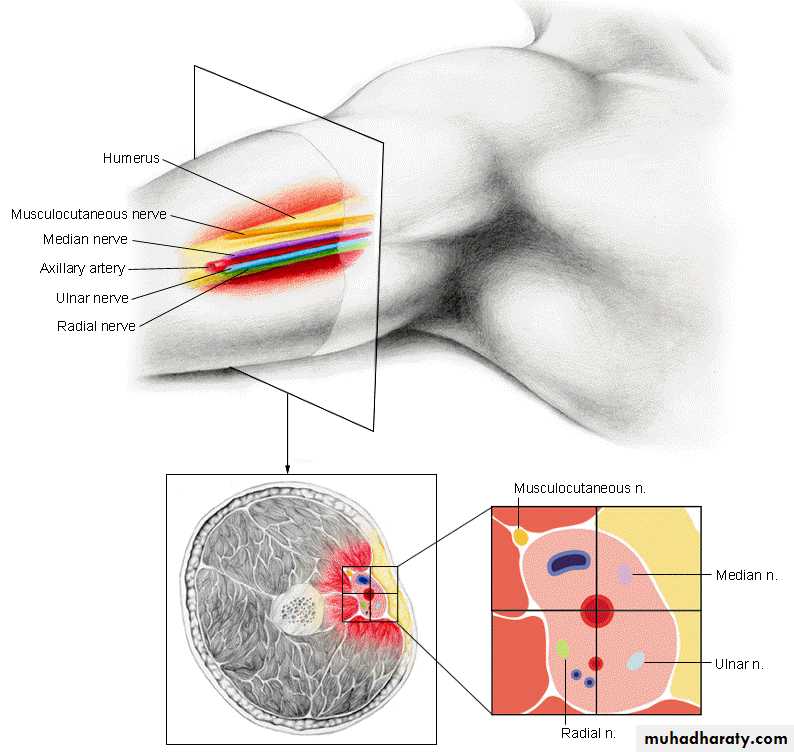
Conduction block
Field block
Nerve block
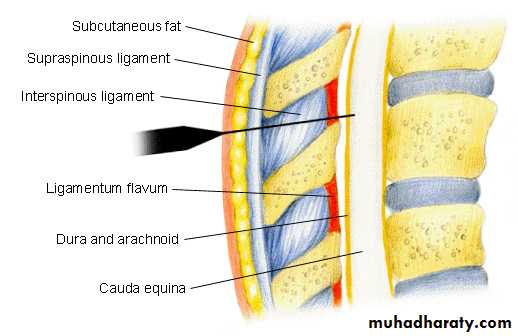
Peridural
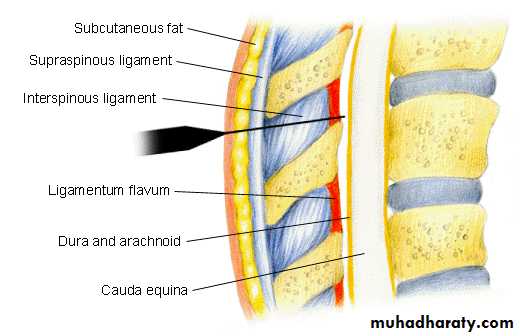
Spinal anesthesia
Topical Anesthesia
Done by the administering the anesthetic to mucous membranes or skin. Relieves itching, burning and surface pain, i.e. sunburns.Infiltration
Occurs by directly injecting a local anesthetic to block the nerve endings under the skin or in the subcutaneous tissue. Used mainly for surgeries, i.e. cavities being filled.
Conduction block
Epidural AnesthesiaThis is accomplished by injecting a local anesthetic into the peridural space, a covering of the spinal cord
Spinal anesthesia
Here, the local anesthetic is injected into the subarachnoid space of the spinal cordToxicity
CNS Toxicity:Systematic absorption can lead to excitement (tremors, shivering, convulsions),
If absorbed in even higher amounts can lead to depression (coma, respiratory arrest and death)
Cardiovascular toxicity:
If absorbed in excess systematically can lead to depression of the cardiovascular system
Hypersensitivity: Rashes to anaphylaxis
Local reactions: Combination with vasoconstrictor
(combination should be avoided-feet, fingers, toes, pinna, penis)
Adverse Effects
CNS side effects include: dizziness, mental confusion, tremors, twitching, visual disturbances, convulsion and respiratory depression.
CVS toxicity includes : hypotension, cardiac arrhythmias and bradycardia. Other side effects include allergic dermatitis, asthma, anaphylactic shock etc.
Pharmacokinetics
They are readily absorbed through mucous membranes and damaged skin. These are weak bases and at tissue pH diffuse through the connective tissue and cellular membranes to reach the nerve fibres where ionization can occur.Amide type local anaesthetics (lignocaine, bupivacaine) are metabolised in the liver and in some cases the kidneys. These are considerably protein bound.
For certain procedures the duration of action is prolonged by adding adrenaline 1 in 2,00,000. In dentistry, where the total dose is small higher concentration such as 1 in 80,000 may be used.
Therapeutic Uses
Surface anaesthesia.Spinal anaesthesia.
Infiltration anaesthesia.
Nerve block or conduction block
Systemic use in the treatment of cardiac arrhythmias
Dental anaesthesia: The total amount of local anaesthetics injected is much smaller (20-80 mg of lignocaine) than that used for other purpose.
LIGNOCAINE
Mechanism of ActionLignocaine stabilizes the neuronal membrane by inhibiting ionic fluxes required for initiation and conduction of impulses thereby affecting local anaesthetic action.
Pharmacokinetics
Lignocaine is completely absorbed following parenteral administration, its rate of absorption depending upon various factors such as site of administration and the presence or absence of vasoconstrictor agent. Lignocaine is metabolised rapidly by the liver and metabolites and unchanged drug are excreted by the kidneys. Approximately 90% of lignocaine administered is excreted in the form of various metabolites and less than 10% is excreted unchanged.
The elimination half-life of lignocaine following an intravenous bolus injection is 1.5 to 2.0 hours.
Adverse Effects
CNS manifestations are excitatory and/ or depressant and may be characterised by light-headedness, nervousness, apprehension, euphoria, confusion, dizziness, drowsiness, tinnitus, blurred or double vision, vomiting, sensation of heat, cold or numbness, twitching, tremors, convulsions, unconsciousness, respiratory depression.
Drowsiness following the administration of lignocaine is usually an early sign of a high blood level of the drug and may occur as a consequence of rapid absorption.
Cardiovascular manifestations are usually depressant and are characterised by bradycardia, hypotension and cardiovascular collapse, which may lead to cardiac arrest.
Allergic reactions are characterised by cutaneous lesions, urticaria, edema or anaphylactoid reactions may occur as a result of sensitivity to local anaesthetic agent.
Indication
Lignocaine injections are indicated for production of local or regional anaesthesia by infiltration techniques such as percutaneous injection, peripheral nerve block, spinal or subarachnoid block.Lignocaine (2%) with adrenaline (1:80,000) is mostly used local anaesthetic in dentistry which produces good soft tissue and pulpal anaesthesia and also reduces post extraction bleeding. The pulpal anaesthesia is obtained within 2-3 minutes after injection and lasts for about on hour.
BENZOCAINE
Inhibits conduction of nerve impulses from sensory nerves. This action is a result of alteration of cell membrane permeability to ions. It is poorly absorbed from the intact epidermis.Benzocaine has been termed by the FDA as ‘one of the most widely used and safest external analgesic and that the incidence of sensitivity of benzocaine is quite low’.
DIBUCAINE
It is another local anaesthetic with longer action but most toxic. It is used for surface anaesthesia.BUPIVACAINE
It is a potent and long acting local anaesthetic used for spinal, infiltration, epidural anaesthesia and nerve block.
Side effects include cardiac arrest, cardiac arrhythmias and respiratory failure.
Bupivacaine (0.5%) with adrenaline (1:2,00,000) is less frequently used in dentistry because of its poor penetration into bone.
BENOXINATE
It is a surface anaesthetic used in eye for producing corneal anaesthesia for tonometry and does not cause mydriasis or any corneal damage.
OXETHAZAINE
A potent local anaesthetic used for anaesthetizing gastric mucosa. Along with antacid in suspension form it is used in gastritis, gastric irritation and gastroesophageal reflux.
Side effects include drowsiness and dizziness.
ROPIVACAINE
Newer compound, long acting local anaesthetic which produces less cardiotoxicity. It is used mainly for nerve block and in postoperative pain. It is occasionally used in dentistry.
The Use of Vasoconstrictors in LocalAnesthesia
With the exception of cocaine, local anesthetics cause a transient vasodilation (dilatation of blood vessels) following application or injection. Vasodilation causes an increased perfusion of blood to the injected area, with two possible results:(1) the drug being carried away, and therefore becoming less effective
(2) the anesthetic agent reaching the cardiac muscle with the potential for undesired myocardial effects
The effect on the heart muscle is a valid consideration since one of the prototype drugs in these discussions, lidocaine, has a use in medical emergencies in the treatment for life-threatening ventricular arrhythmia.
In order to maintain effective concentrations of local anesthetics at the injection site, vasoconstrictive drugs are often added to the solution.
The primary additive is epinephrine.
The addition of epinephrine not only minimizes the vasodilation caused by the local anesthetic agent, but causes vasoconstriction of the blood vessels in the area surrounding the injection. The vasoconstriction decreases perfusion of blood to the region, and the local anesthetic is not carried away.Patients with diabetes are predisposed to problems with capillary circulation.
The addition of epinephrine can cause further vasoconstriction to capillaries already compromised by the disease process.Patients with diabetes may experience an increase in tissue damage as a result.
Another vasoconstrictor: phenylphrine, felypressin, levonordefrin.
The most common dilution for levonordefrin 1:20,000.