1
L1
Esophagus
Lesions of the esophagus run from bland esophagitis to highly lethal cancers, yet they evoke
a similar and remarkably limited range of symptoms.
All produce dysphagia, Heartburn (retrosternal burning pain). Hematemesis (vomiting of
blood) and melena (blood in the stools) are evidence of severe inflammation, ulceration, or
laceration of the esophageal mucosa.
Massive hematemesis may reflect life- threatening rupture of esophageal varices.
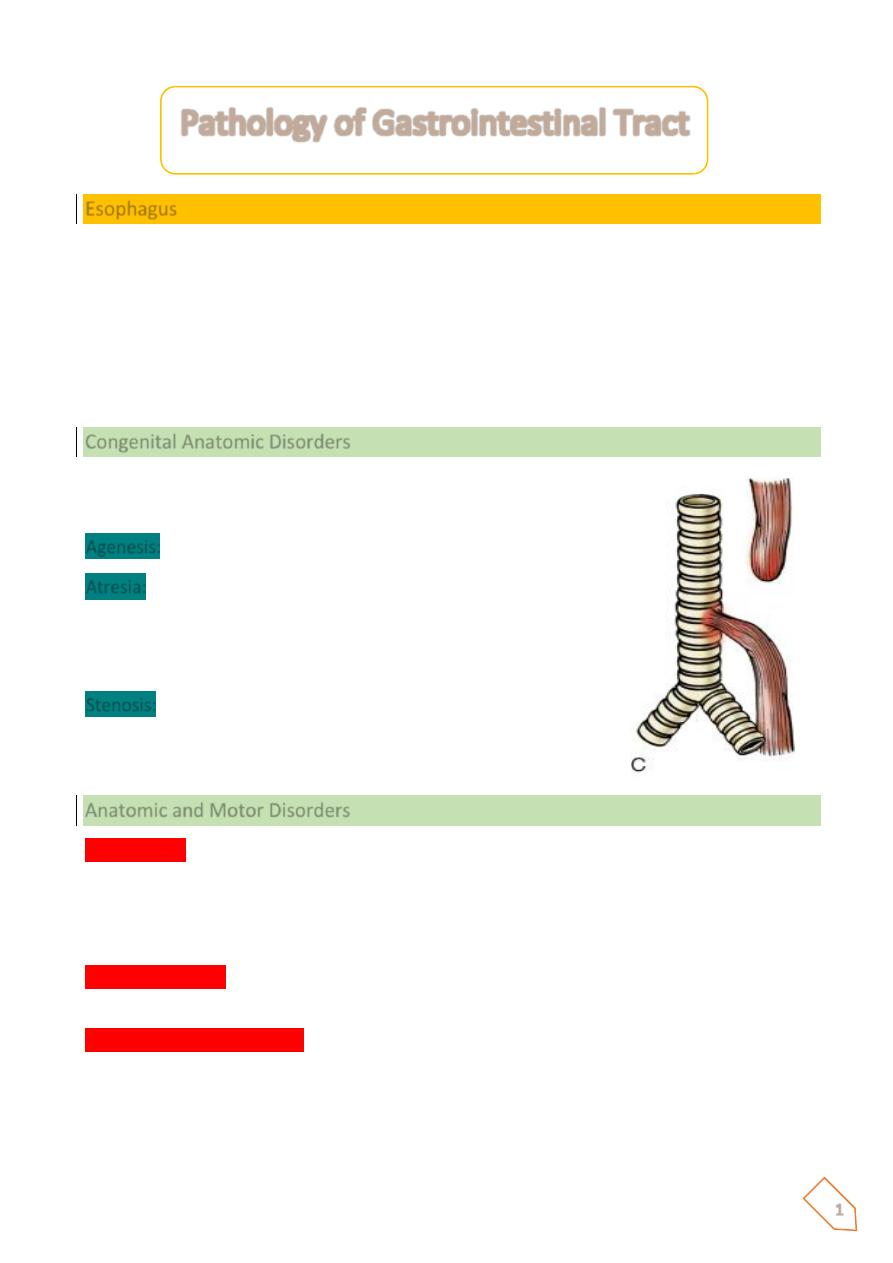
Congenital Anatomic Disorders
Present at birth with vomiting, aspiration (pneumonia, asphyxia),
and gastric distention
Agenesis:
absence of esophagus. Very rare
Atresia:
failure of development of a segment of esophagus,
which is replaced by a thin non-canalized cord (absence of
lumen) with formation of upper & lower pouches; associated
with tracheo-esophageal fistula
Stenosis:
developmental defect resulting in partial obstruction or
narrowing of the esophageal lumen
Rx: Urgent medical & surgical intervention
Anatomic and Motor Disorders
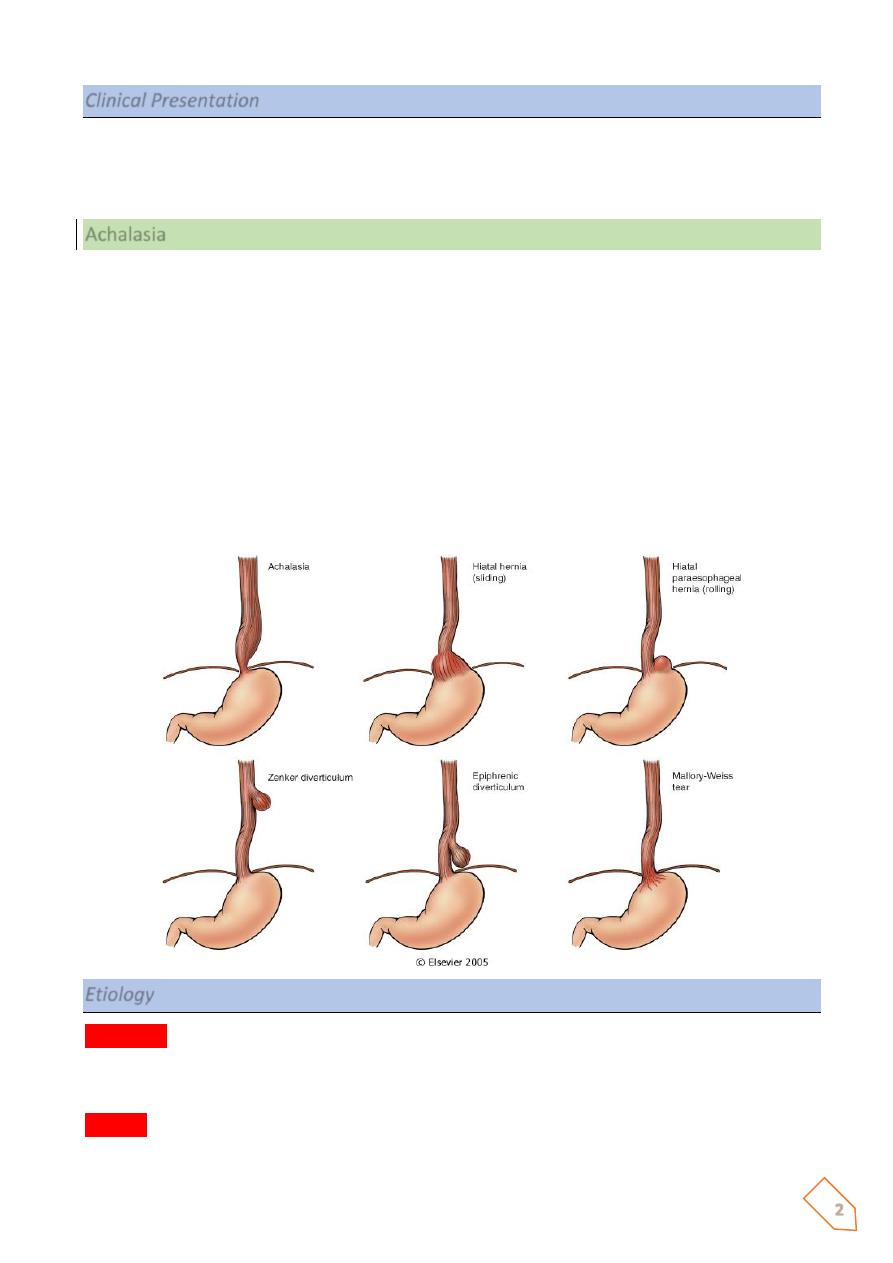
Hiatal hernia
In hiatal hernia, separation of the diaphragmatic crura and widening of the space
between the muscular crura and the esophageal wall permits a dilated segment of the
stomach to protrude above the diaphragm. Two anatomic patterns are recognized :
1- the axial, or sliding, hernia 2- and the nonaxial, or paraesophageal, hernia.
The sliding hernia
constitutes 95% of cases; protrusion of the stomach above the diaphragm
creates a bell-shaped dilation, bounded below by the diaphragmatic narrowing
In paraesophageal hernias
, a separate portion of the stomach, usually along the greater
curvature, enters the thorax through the widened foramen.
The cause of this deranged anatomy is obscure. On the basis of radiographic studies, hiatal
hernias are reported in 1% to 20% of adult subjects, increasing in incidence with age.
Pathology of Gastrointestinal Tract
2
Clinical Presentation
Adult with progressive dysphagia to solids and eventually to all foods; heartburn or
regurgitation of gastric juices into the mouth. These symptoms result from incompetence of
the lower esophageal sphincter than from the hiatal hernia per se
Achalasia
The term achalasia means “failure to relax” and in the present context denotes incomplete
relaxation of the lower esophageal sphincter in response to swallowing. This produces
functional obstruction of the esophagus, with consequent dilation of the more proximal
esophagus. Manometric studies show three major abnormalities in achalasia:
1. aperistalsis,
2. partial or incomplete relaxation of the lower esophageal sphincter with swallowing, and
3. Increased resting tone of the lower esophageal sphincter.
It is now generally accepted that in primary achalasia there is loss of intrinsic inhibitory
innervation of the lower esophageal sphincter and smooth muscle segment of the esophageal
body.
Etiology
Secondary
achalasia may arise from pathologic processes that impair esophageal function.
The classic example is Chagas disease, caused by Trypanosoma cruzi, which causes
destruction of the myenteric plexus of the esophagus, duodenum, colon, and ureter.
Primary
disorder of uncertain etiology. Autoimmunity and previous viral infection have been
hypothesized but remain unproven
3
Morphology
ⱴ In primary achalasia, there is progressive dilation of esophagus above the level of the
lower esophageal sphincter.
ⱴ The wall of the esophagus may be of normal thickness, thicker than normal because of
hypertrophy of the muscularis, or markedly thinned by dilation.
ⱴ The myenteric ganglia are usually absent from the body of the esophagus -
Inflammation in the location of the esophageal myenteric plexus is pathognomonic of
the disease.
C/P: progressive dysphagia and inability to completely convey food to the stomach. Nocturnal
regurgitation and aspiration of undigested food may occur. It usually becomes manifest in
young adulthood, but it may appear in infancy or childhood.
Complication
Is the hazard of developing esophageal squamous cell carcinoma, reported to occur in about
5% of patients and typically at an earlier age than in those without achalasia.
Lacerations (Mallory-Weiss Syndrome)
Definition:
Longitudinal tears in the esophagus at the esophagogastric junction are termed Mallory-
Weiss tears.
Etiology:
They are encountered in chronic alcoholics after a bout of severe retching or vomiting, but
they may also occur during acute illnesses with severe vomiting.
Pathogenesis:
May be due to inadequate relaxation of the musculature of the lower esophageal sphincter
during vomiting, with stretching and tearing of the esophagogastric junction at the moment
of propulsive expulsion of gastric contents.
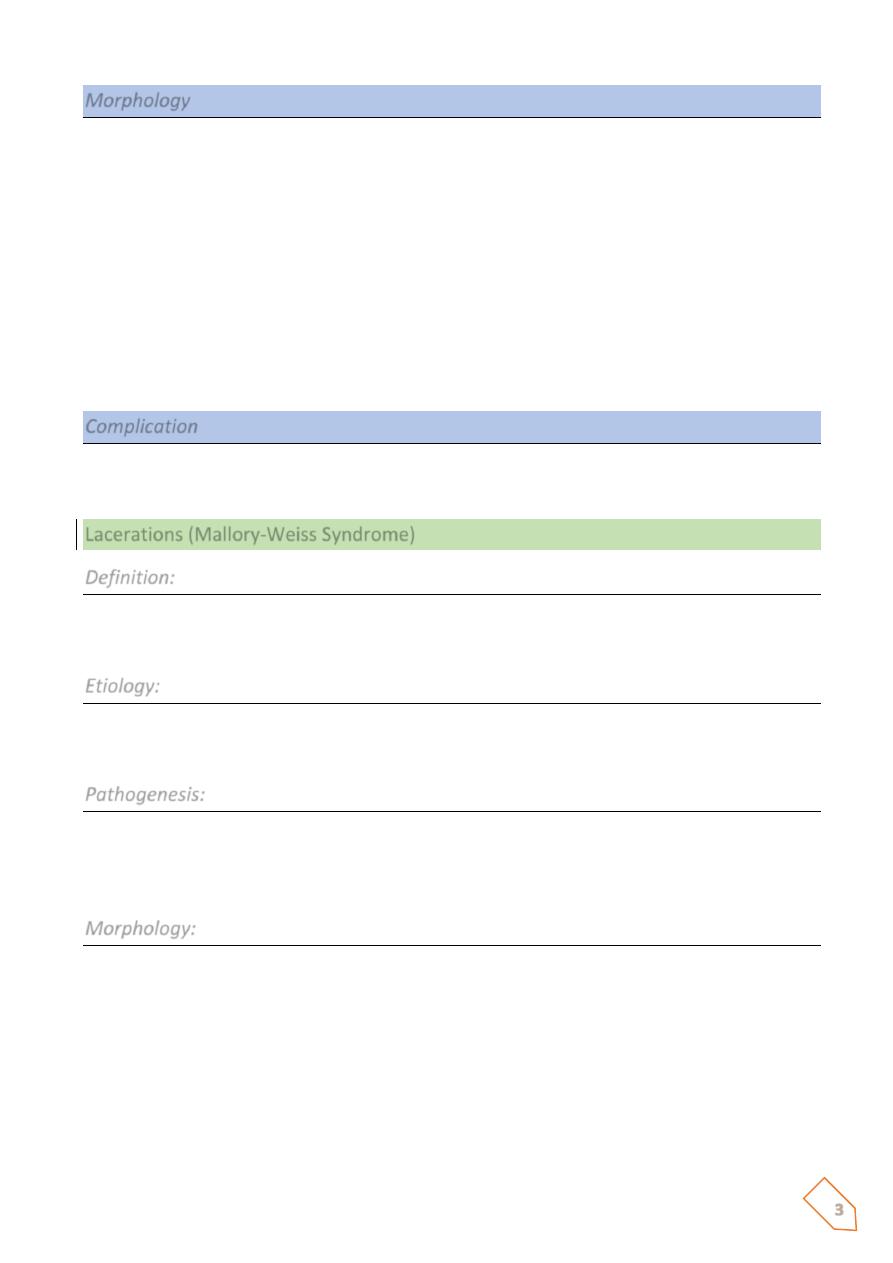
Morphology:
Tears may involve only the mucosa or may penetrate the wall. Infection of the defect may
lead to an inflammatory ulcer or to mediastinitis. Most often bleeding is not profuse and
ceases without surgical intervention, but life-threatening hematemesis may occur. Even with
severe blood loss, supportive therapy with vasoconstrictive medications, transfusions, and
sometimes balloon tamponade, is usually all that is required. Healing is usually prompt, with
minimal to no residua
4
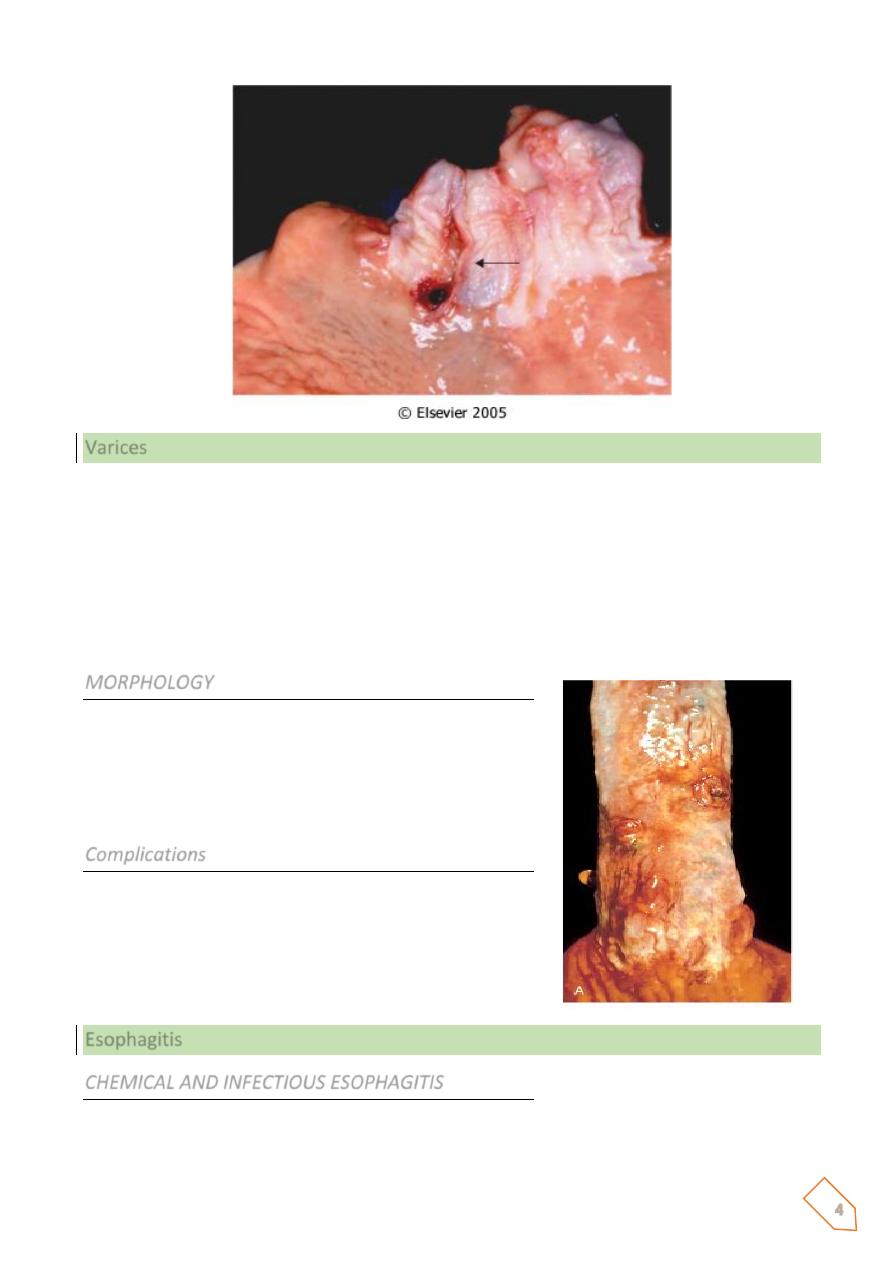
Varices
One of the few potential sites for communication between the intra-abdominal splanchnic
circulation and the systemic venous circulation is through the esophagus. When portal
Venous blood flow into the liver is impeded by cirrhosis or other causes the resultant portal
hypertension induces the formation of collateral bypass channels wherever the portal and
systemic systems communicate. The increased pressure in the esophageal plexus produces
dilated tortuous vessels called varices. They are most often associated with alcoholic
cirrhosis.
MORPHOLOGY
Varices appear primarily as tortuous dilated veins lying
primarily within the submucosa of the distal esophagus
and proximal stomach.
Varices produce no symptoms until they rupture.
Complications
Rupture of varices. The factors leading to initial rupture
of a varix are unclear: silent erosion of overlying thinned
mucosa, increased tension in progressively dilated
veins, and vomiting with increased intra-abdominal
pressure are likely to be involved.
Esophagitis
CHEMICAL AND INFECTIOUS ESOPHAGITIS
The stratified squamous mucosa of the esophagus may be damaged by a variety of irritants
including alcohol, corrosive acids or alkalis, excessively hot fluids, and heavy smoking.
5
The esophageal mucosa may also be injured when medicinal pills lodge and dissolve in the
esophagus rather than passing into the stomach intact, a condition termed pill-induced
esophagitis.
C/P:Esophagitis due to chemical injury generally only dysphagia (pain with swallowing).
Hemorrhage, stricture, or perforation may occur in severe cases.
Infectious esophagitis may occur in otherwise healthy individuals but are most frequent in
those who are debilitated or immunosuppressed as a result of disease or therapy.
REFLUX ESOPHAGITIS
GE reflux disease affects about 0.5% is of the US adult population. Dominant symptom
recurrent heartburn.
Etiology:
• Decrease efficacy of esophageal antireflux mechanisms.
• Inadequate or slowed esophageal clearance of refluxed material.
• Sliding hiatal hernia. Fat, chocolate, alcohol, smoking
• Increased gastric volume.
• Impaired reparative capacity of the esophagus mucosa by prolonged exposure to
gastric juices.
MORPHOLOGY
The anatomic Changes depend on the causative agent and on the duration and severity of
the exposure. Mild esophagitis may appear macroscopically as simple hyperemia, with
virtually no histologic abnormality. In Contrast the mucosa in severe esophagitis exhibits
confluent epithelial erosions or total ulceration into the submucosa
The histologic feature
Are characteristic of uncomplicated reflux esophagitis is:
1. eosinophils, with or without neutrophils, in the epithelial layer;
2. basal zone hyperplasia; and
3. elongation of lamina propria papillae
COMPLICATIONS
• BLEEDING
• STRICTURE
• BARRETT ESOPHAGUS
• PREDISPOSITION TO MALIGNANCY
6
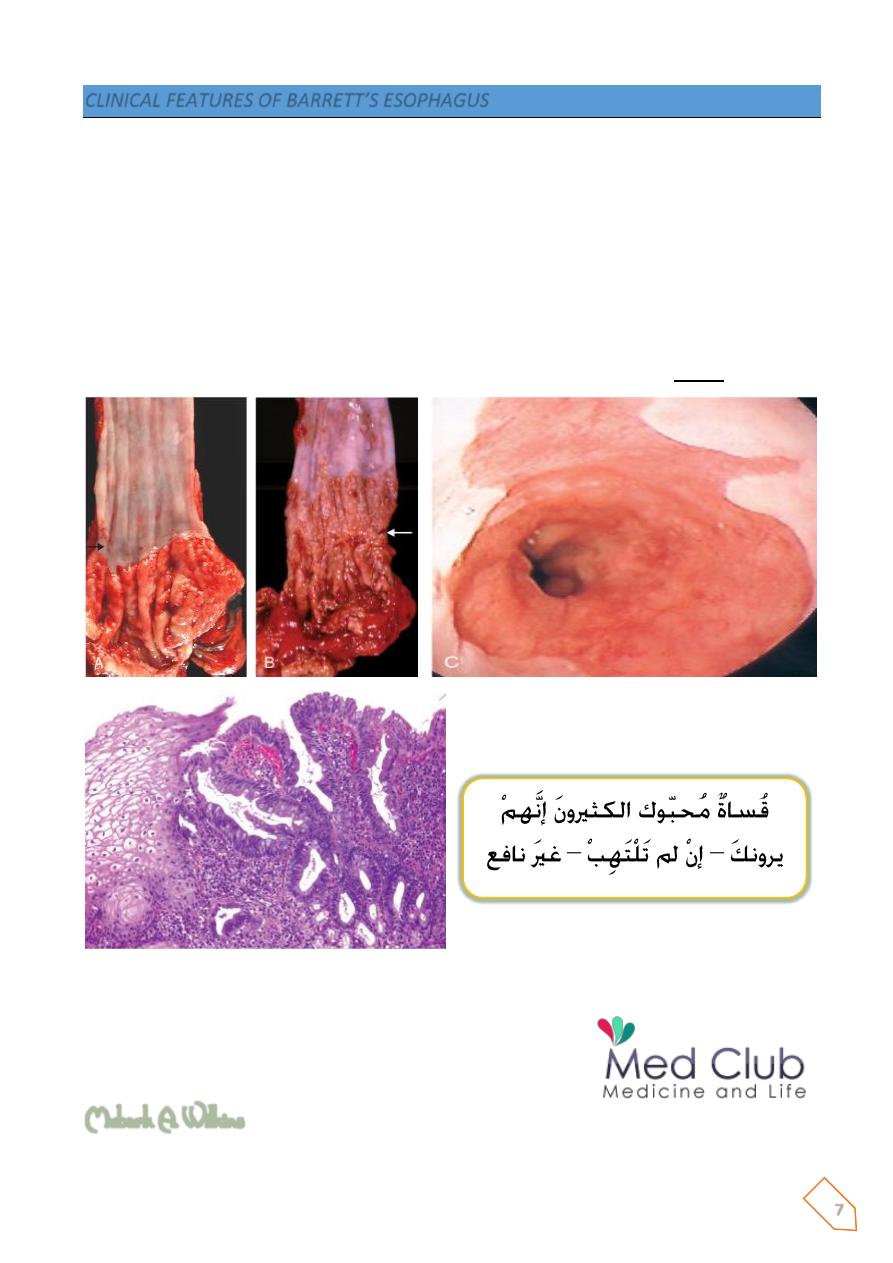
BARRETT ESOPHAGUS
Barrett esophagus is a complication of long-standing gastroesophageal reflux, occurring in up
to 10% of patients with persistent symptomatic reflux disease, as well as in some patients
with asymptomatic reflux.
Barrret esophagus is defined as
the replacement of the normal distal stratified squamous
mucosa by metaplastic columnar epithelium containing goblet cells.
Prolonged and recurrent gastroesophageal reflux is thought to produce inflammation and
eventually ulceration of the squamous epithelial lining.
Healing occurs by in growth of stem cells and re-epithelialization. In the microenvironment of
an abnormally low pH in the distal esophagus caused by acid reflux, the cells differentiate into
columnar epithehum.
Metaplastic columnar epithelium is thought to be more resistant to injury from refluxing
gastric contents.
Barrett esophagus affects males more often than females (ratio of 4:1) and is much more
common in whites than in other races. Genetic factors are suggested by clustering in families.
Ulcer and stricture may develop as a complication of Barrett esophagus.
However, the chief clinical significance of Barrett esophagus relates to the development of
adenocarcinoma. Patients with Barrett esophagus have a 30- to 40-fold greater risk of
developing esophageal adenocarcinoma compared with normal populations
MORPHOLOGY
Barrett esophagus is apparent as a salmon-pink, velvety mucosa between the smooth, pale
pink esophageal squamous mucosa and the more light brown gastric mucosa.
Microscopically, the esophageal squamous epithelium is replaced by metaplastic columnar
epithelium.
7
CLINICAL FEATURES OF BARRETT’S ESOPHAGUS
ⱴ Clinical symptoms:
• Dysphagia, retrosternal pain, hemetemesis, melena
ⱴ Secondary complications:
• Barrett’s ulcers
• Strictures
• Dysplasia
• Adenocarcinoma: 8-10% of patients develop Ca (patients with Barrett’s
esophagus have 30-40 fold higher risk than general population)
Barrett’s esophagus is the only recognized precursor of esophageal adenocarcinoma
Mubark A. Wilkins
