HematopatHology
Hematopathology: branch of pathology which studies the diseases of hematopoietic cells
originate from the bone marrow and contribute the cellular components of blood including
red blood cells (erythrocytes), white blood cells (leukocytes), and platelets.
Blood
Blood is a life-sustaining fluid which circulates through the heart and blood vessels. It
carries oxygen and nutrients to the tissues and waste products to the lungs, liver and
kidneys, where they can be removed from the body.
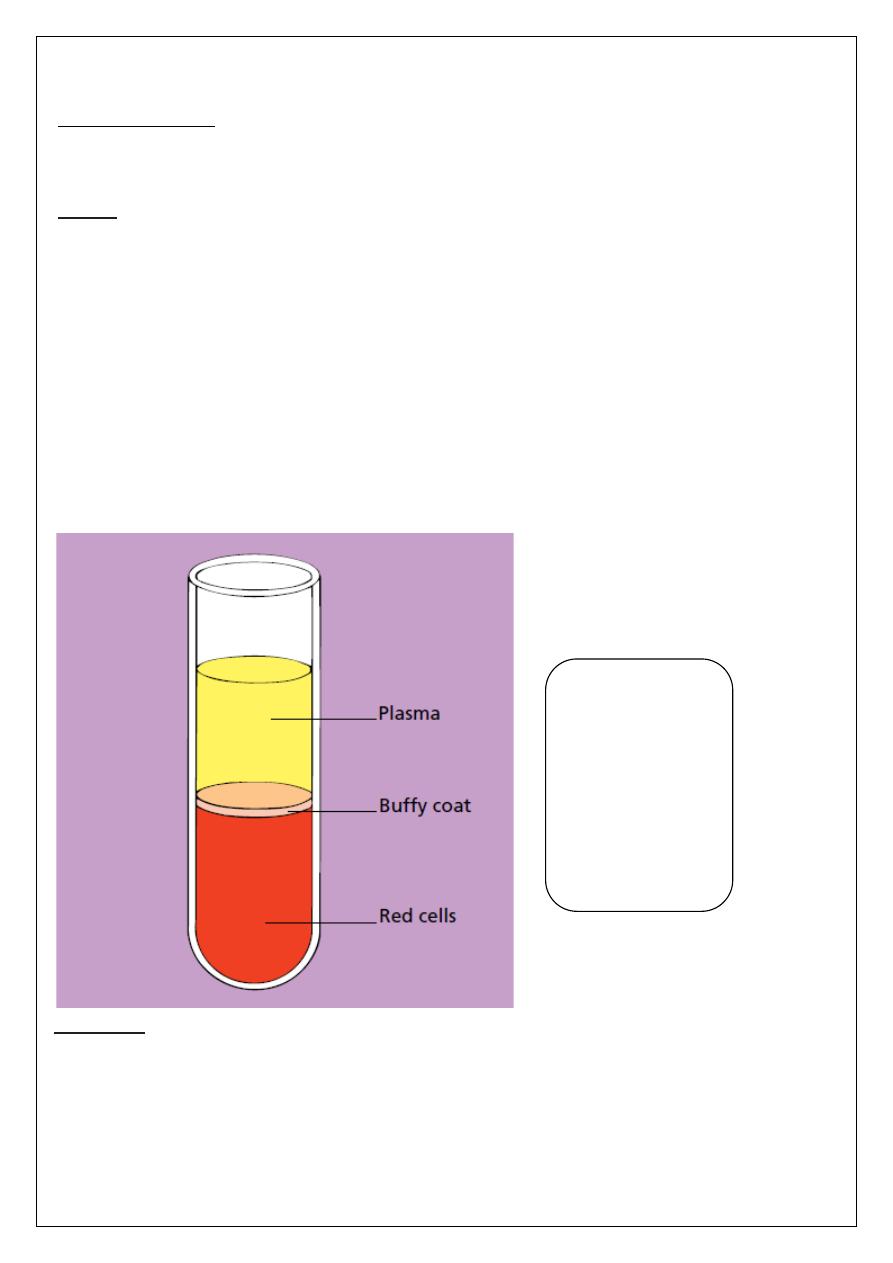
Usually when blood is removed from the body it forms a solid blood clot. However, if
clotting is prevented by mixing with an anticoagulant, the blood separates, under the
influence of gravity, into three layers.
The bottom layer is deep red in colour and is composed of red cells.
The top layer is clear and pale yellow. It is called
plasma and is composed of various salts
and proteins dissolved in water.
In between is a narrow layer called the buffy coat because
of its buff or yellowish white colour. The buffy coat is composed mainly of cells of a variety
of types, collectively known as white cells. In addition there are small cellular fragments,
called platelets, which have a role in blood clotting.
Red cells
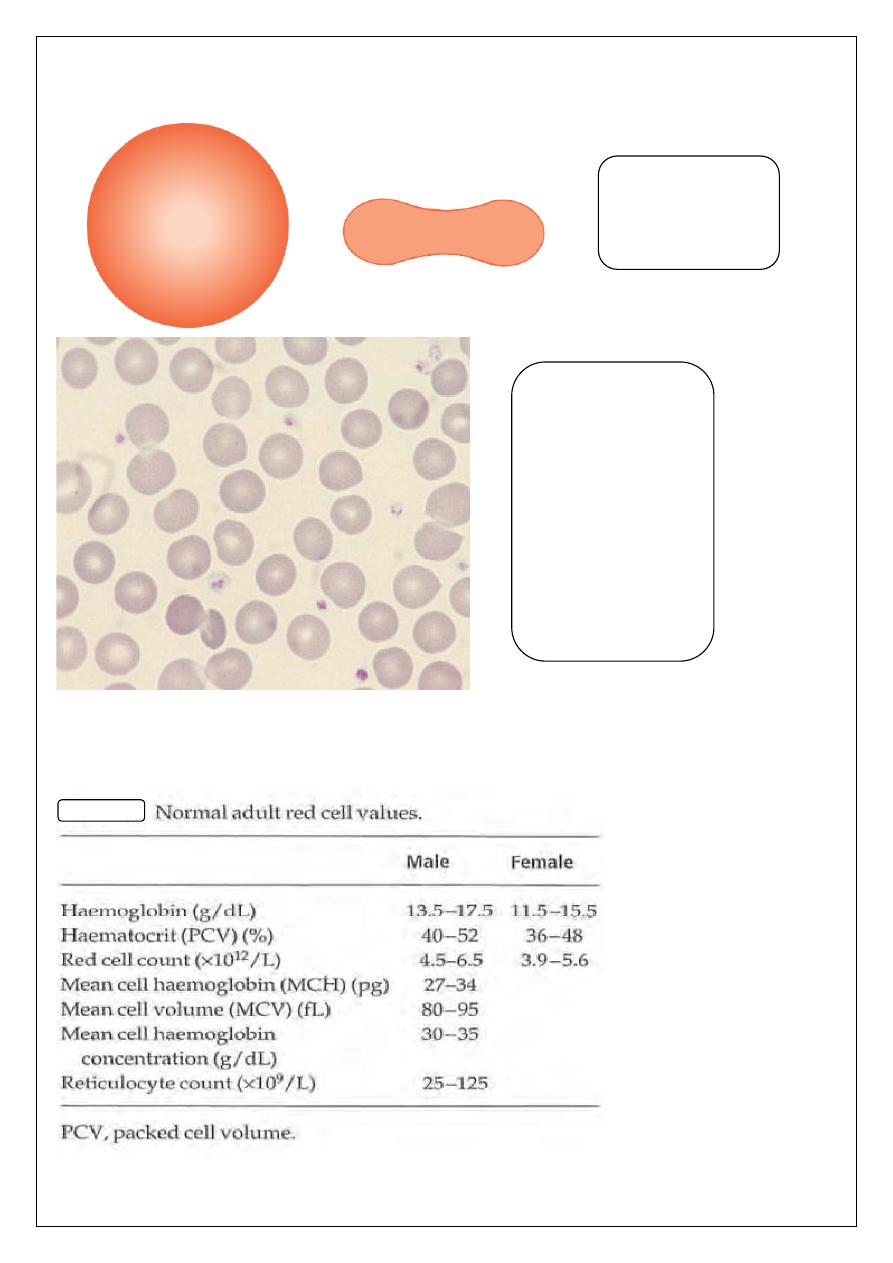
The most numerous cells in a blood are the red cells (erythrocytes). Normal red cells are
disc-shaped but are thinner in the center. As a consequence, on a stained blood film, they
have a circular outline and a paler central area. Red cells owe their pinkish-brown colour to
the presence of a complex protein,
haemoglobin
, which is their major constituent.
The haemoglobin combines with oxygen from inspired air, in the lungs, and transports it to
tissues where it is needed for the metabolic processes supplying the energy needs of the
body. Mature red cells in humans differ from most body cells in that they do not have a
Diagram of a tube
of anticoagulated
blood which has
been allowed to
sediment, showing
the separation of
blood into red cells,
a buffy coat (white
cells and platelets)
and plasma.
nucleus. Red cells are produced in the bone marrow and usually lose their nuclei when they
are released into the blood stream.
A diagram of a red
cell viewed from
above and in cross-
section
.
Normal red cells
(erythrocytes)
showing little
variation in size and
shape, an
approximately round
outline and a small
area of central pallor
in some of the cells.
The small lilac-
staining structures
between the red cells
are platelets.
Red Blood Cell Disorders
Anemia
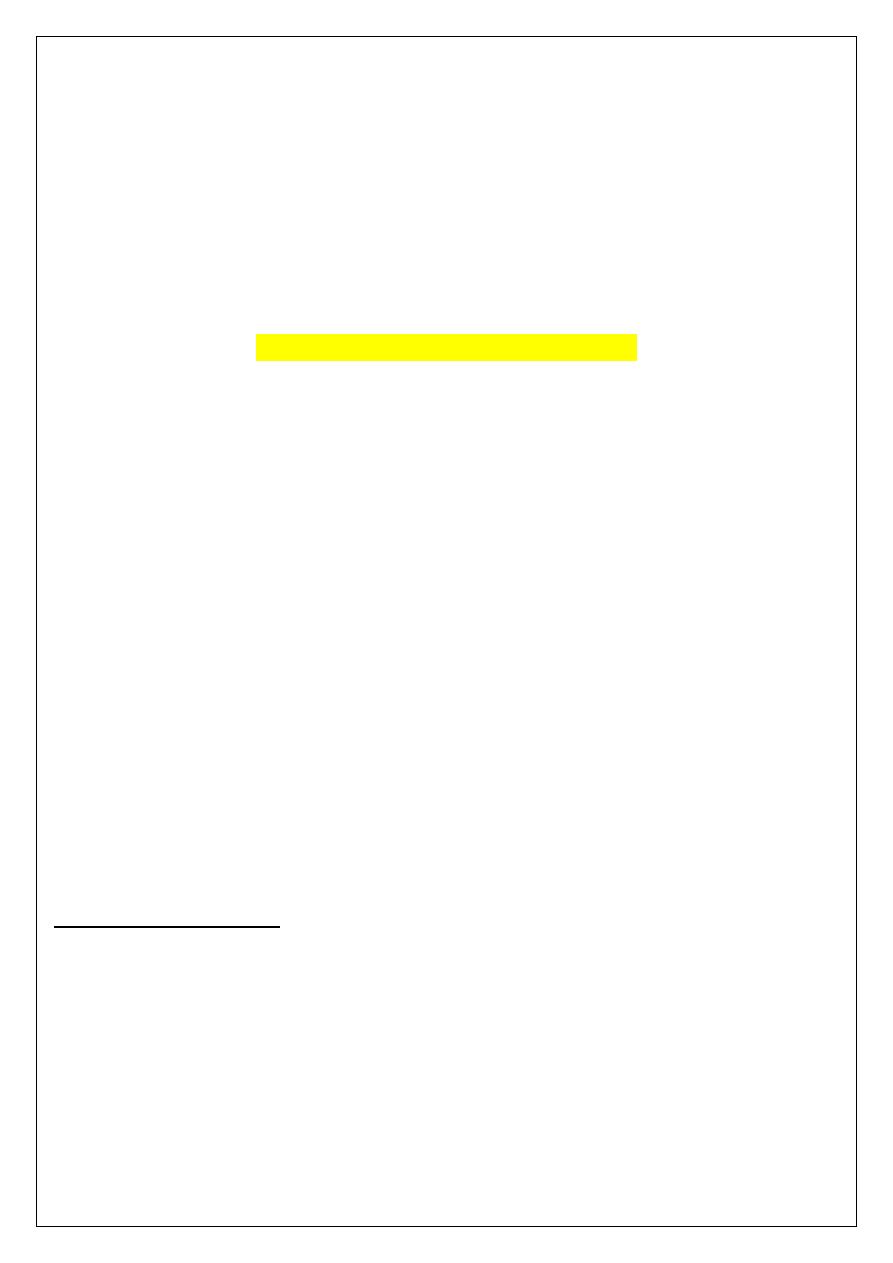
A reduction in the haemoglobin concentration in the blood, in comparison with what would
be found in a normal individual of the same age and gender.
Reduction of haemoglobin is usually accompanied by a fall in red cell count and packed cell
volume (PCV) but these maybe normal in some patients with subnormal haemoglobin levels
(and therefore by definition anemic).
Anemia not a diagnosis and an underlying cause should always be sought. It is the most
common disorder of the blood.
Definition of red blood cell indices:
• The mean cell volume (MCV) is a measure of the average red blood cell size.
• The mean cell hemoglobin (MCH) is the average mass of hemoglobin per red
blood cell in a sample of blood.
• The mean corpuscular hemoglobin concentration (MCHC) is a measure of the
concentration of hemoglobin in a given volume of packed red blood cells.
Morphologic Classification of Anemia
• Hypochromic microcytic anemia (low MCV <80 fl , low MCH <27 pg)
1. Iron deficiency
2. Anemia of chronic disease (some cases)
3. Thalassaemia
• Normochromic normocytic anemia (normal MCV 80-95 fl , normal
MCH ≥ 27 pg)
1. Hemolytic Anemia
2. Anemia of chronic disease ( some cases )
3. anemia of renal disease
4. Acute blood loss
5. Mixed deficiency ( iron + B12 or folate )
• Macrocytic anemia (high MCV
≥ 95 fl )
1. Megaloblastic Anemia (Vitamin B12, Folate deficiency)
2. Non-Megaloblastic Anemia (alcohol, liver disease, etc.)
Initial laboratory approach to the diagnosis of anemia:
• Hemoglobin, hematocrit or red cell counts to determine degree of anemia.
• Red cell indices (MCV, MCH, MCHC) to determine whether normocytic, macrocytic
or microcytic and hypochromic red cells.
• Reticulocyte count in PB is a fairly accurate reflection of erythropoietic activity
((Marrow response)).
((Reticulocyte a young erythrocyte, newly released from the bone marrow, identified
by its uptake of certain vital stains)).
• Examination of blood film to determine red cell shape, presence of red cell inclusions,
& accompanying abnormalities of white blood cells & platelets.
• Bone marrow examination is valuable in certain cases of anemia.
The Hypochromic Microcytic Anemia
IRON DEFICIENCY ANEMIA (IDA)
Iron deficiency is the most common cause of anemia in every country of the world. It is the
most important cause of a microcytic hypochromic anemia, in which the two red cell indices
MCV and MCH are reduced and the blood film shows small (microcytic) and pale
(hypochromic) red cells. This appearance is caused by a defect in hemoglobin synthesis.
Iron is one of the most common elements in the Earth's crust, yet iron deficiency is the most
common cause of anemia, affecting about 500 million people worldwide. This is because the
body has a limited ability to absorb iron and excess loss of iron as a result of hemorrhage is
frequent.
The transport and storage of iron is largely mediated by three proteins: transferrin, the
transferring receptor 1 (TfR1) and ferritin. Transferrin can contain up to two atoms of iron.
It delivers iron to tissues that have transferring receptors, especially erythroblasts in the bone
marrow which incorporates the iron into hemoglobin. At the end of their life, red cells are
broken down in the macrophages of the reticuloendothelial system (RES) and the iron is
released from haemoglobin, enters the plasma and provides most of the iron on transferrin.
Only a small proportion of plasma transferrin iron comes from dietary iron, absorbed
through the duodenum and jejunum. Some iron is stored in the macrophages as ferritin and
hemosiderin, the amount varying widely according to overall body iron status.
When iron deficiency is developing the reticuloendothelial stores (hemosiderin and ferritin)
become completely depleted before anaemia occurs.
Causes of iron deficiency:
• Chronic blood loss (uterine, gastrointestinal, others).
• Increased demands (Prematurity, Growth, and Pregnancy).
• Malabsorption (Gluten-induced enteropathy).
• Poor diet & vegetarian diet.
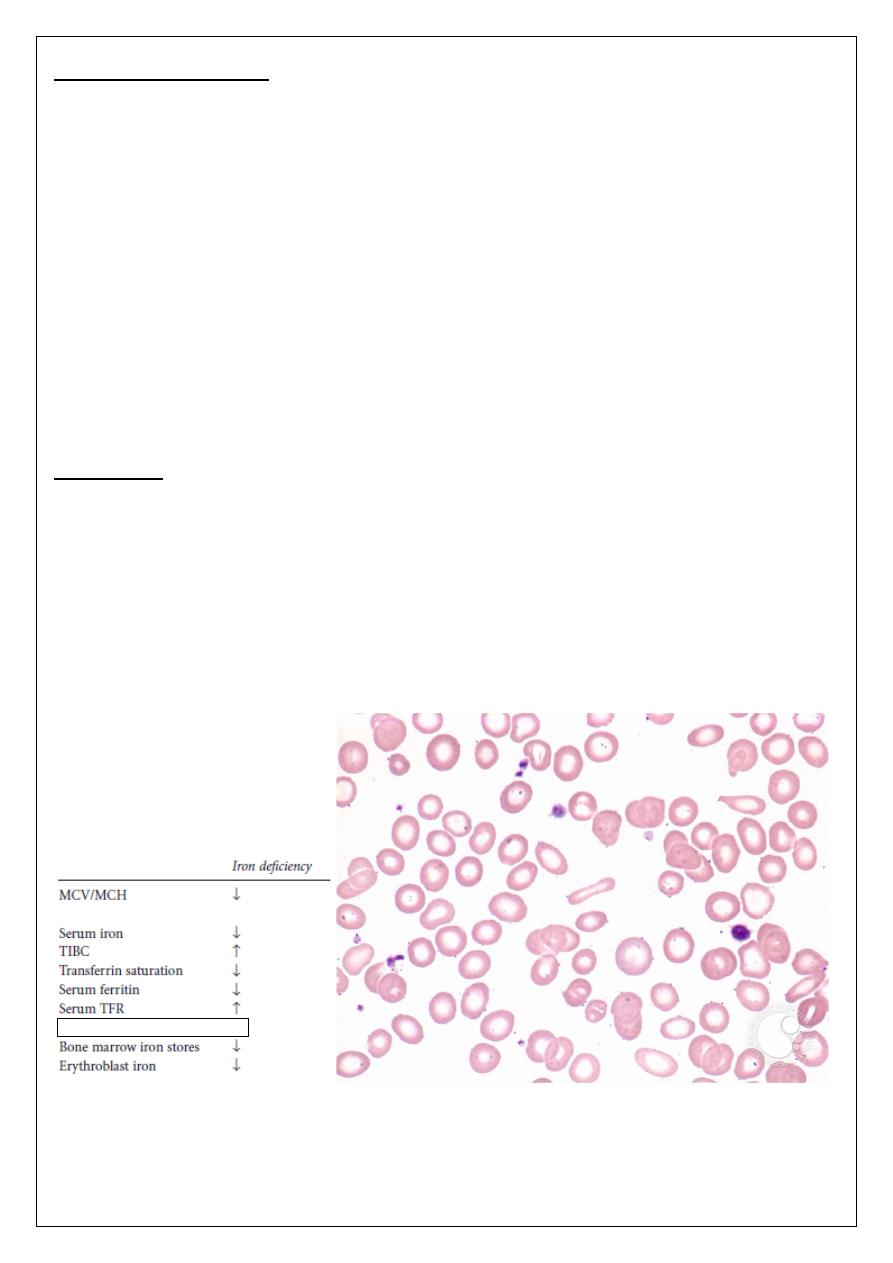
Laboratory findings:
1. Hematological findings:
Reduce in Hb
Reduce PCV, MCV, MCH, and MCHC.
Retic count is low to degree of anemia.
WBC usually normal, and Platelets counts often increase.
Blood film: Hypochromic Microcytic, with rod (pencil) and occasional target cells.
2. Biochemical findings:
Serum Iron reduced.
Total Iron binding capacity TIBC increased.
S. Iron/TIBC: Transferrin saturation reduced <15%.
S. transferring receptor (sTfR) increase.
S. Ferritin: reflects storage iron and is classically reduced in IDA.
3. Investigations for suspected underlying causes.
U
Treatment
The underlying cause is treated as far as possible. In addition, iron is given to correct
the anaemia and replenish iron stores.
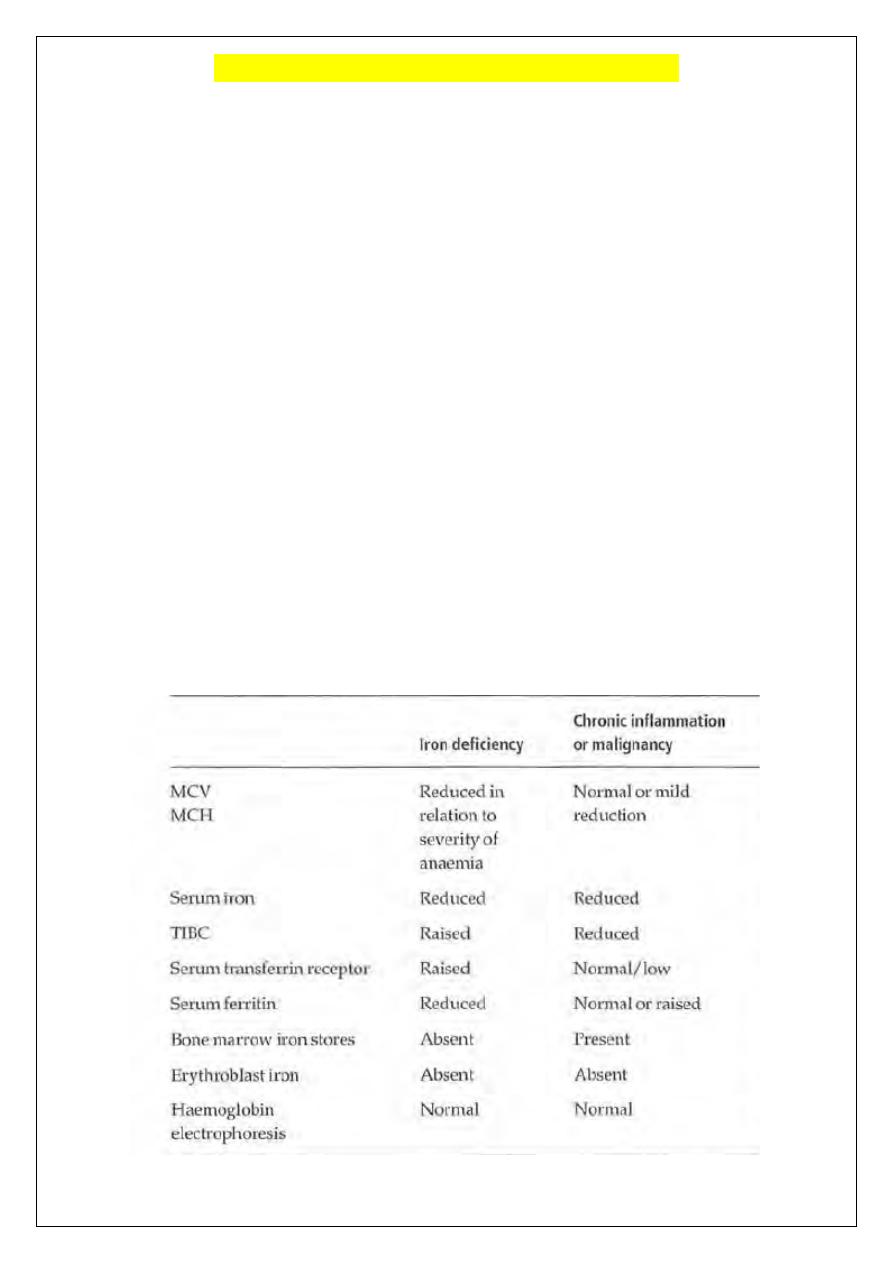
ANEMIA OF CHRONIC DISORDERS (ACD)
One of the most common anemias occurs in patients with a variety of causes:
Chronic inflammatory diseases (infections & non-infections).
Malignant diseases.
The characteristic features are:
a. Normochromic, normocytic or mildly hypochromic indices and red cell
morphology.
b. Mild and non-progressive anaemia (hemoglobin rarely <9.0 g/dL) start 1-3
months after the disease & the severity being related to the severity of the
disease.
c. Both the serum iron and TIBC are reduced ((low serum iron despite adequate
iron stores due to defect in iron mobilization from the storage sites));
d. The serum ferritin is normal or raised.
The pathogenesis of this anemia appears to be related to decreased release of iron from
macrophages to plasma, reduced red cell lifespan and an inadequate erythropoietin response
to anaemia caused by the effects of cytokines such as IL-1 and tumour necrosis factor (TNF)
on erythropoiesis.
The physiologic advantage of ACD to the patients is that iron is less available as a
micronutrient to infectious agents.
The anaemia is corrected by successful treatment of the underlying disease and does not
respond to iron therapy.
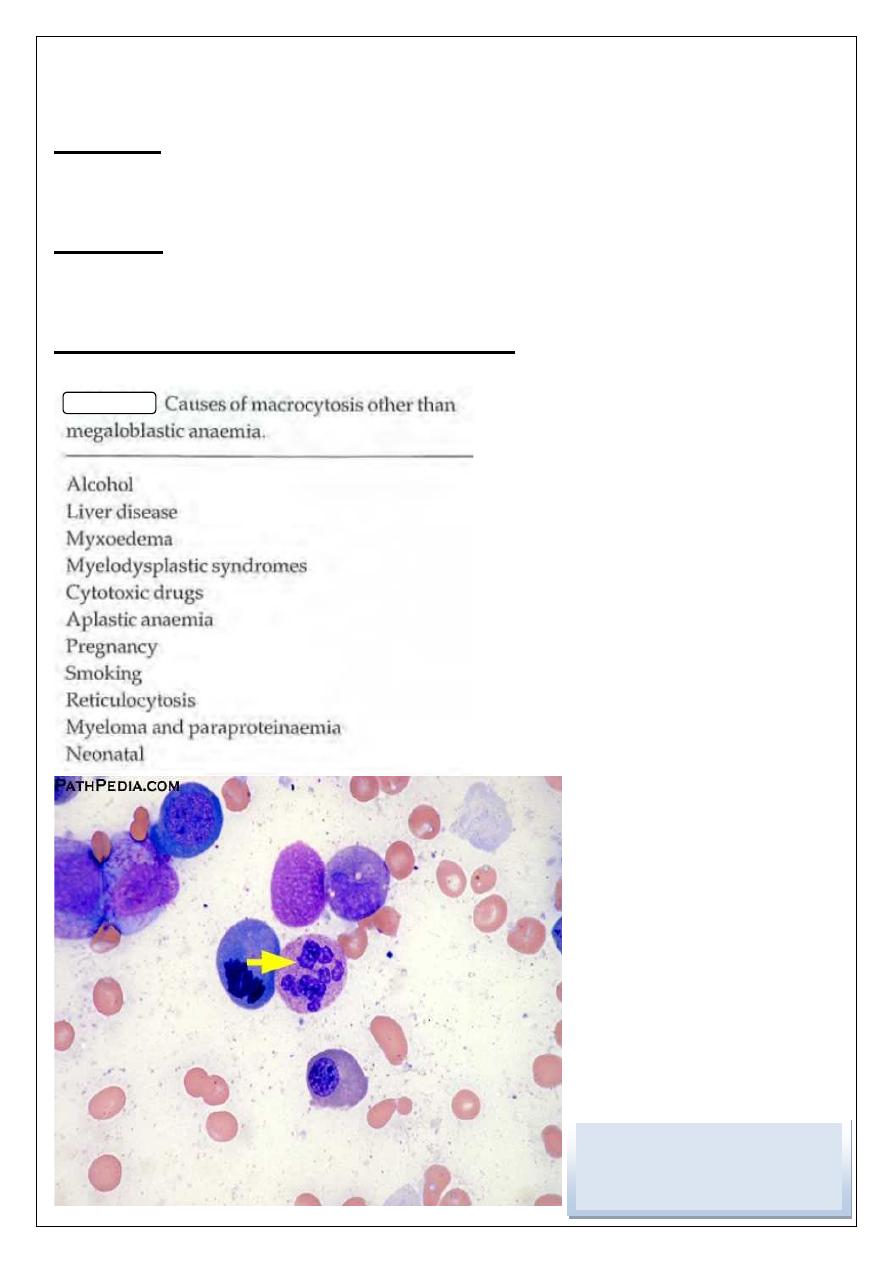
Macrocytic anemia
There are several causes but they can be broadly subdivided into megaloblastic and non-
megaloblastic, based on the appearance of developing erythroblasts in the bone marrow.
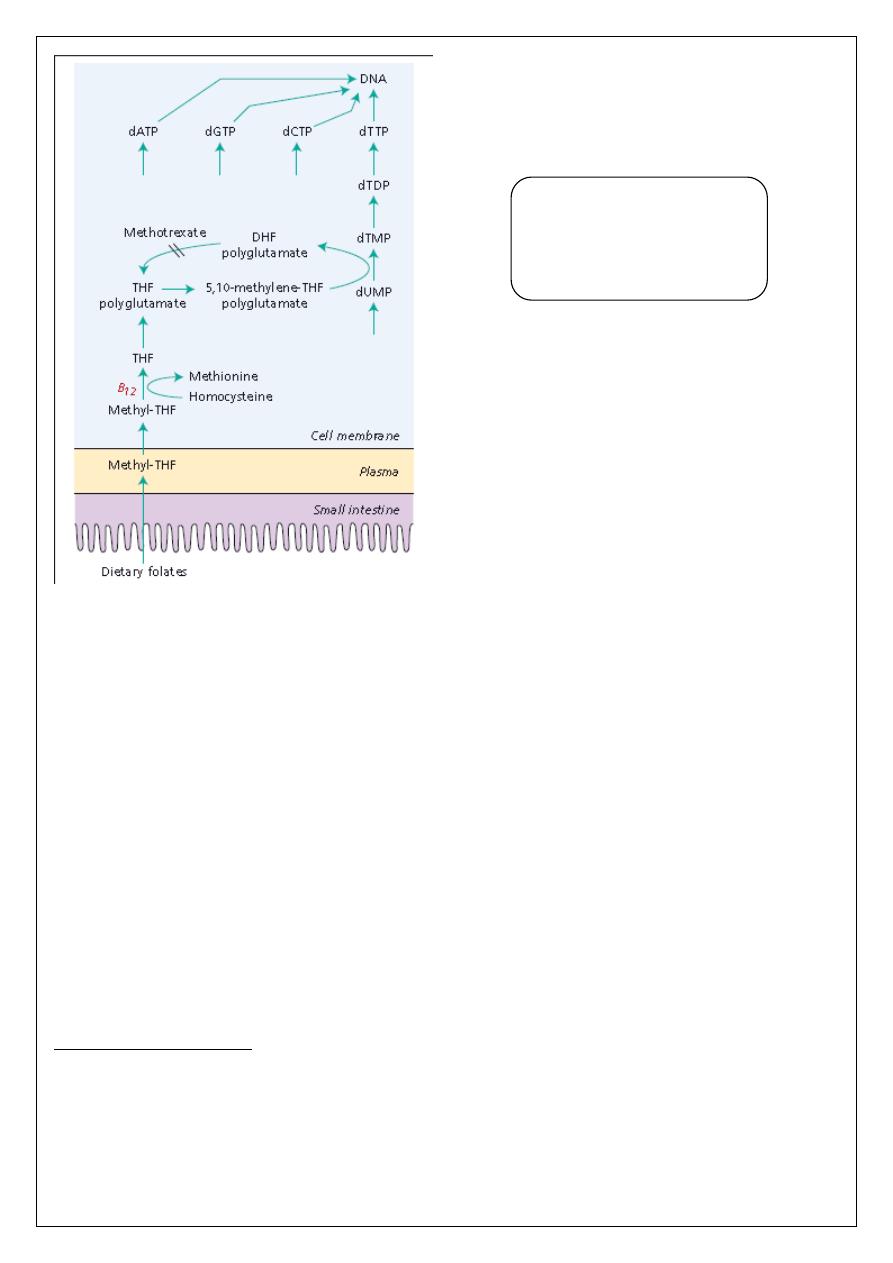
MEGALOBLASTIC ANEMIA:
This is a group of anemias in which the erythroblasts in the bone marrow show a
characteristic abnormality (maturation of the nucleus being
delayed relative to that of the
cytoplasm). The underlying defect accounting for the asynchronous maturation of the
nucleus is defective DNA synthesis and in clinical practice this is usually caused by
deficiency of vitamin Bl2 or folate.
VITAMIN B12 (cobalamin):
This vitamin is synthesized in nature by microorganisms. The vitamin is found in foods of
animal origin such as liver, meat, fish and dairy product but does not occur in fruit, cereals or
vegetables.
Absorption &
Transport:
A normal diet contains a large excess of B12 compared with daily needs. Bl2 is combined
with the intrinsic factor (IF) which is synthesized by the gastric parietal cells. The IF-B12
complex can then bind to a specific surface receptor for IF, which then binds to a second
protein, which directs the absorption of the complex in the distal ileum where Bl2 is
absorbed and IF destroyed.
Vitamin Bl2 is absorbed into portal blood where it becomes attached to the plasma-binding
protein
Transcobalamin (
TC) which delivers Bl2 to bone marrow and other tissues.
FOLATE:
Humans are unable to synthesize the folate structure and thus require preformed folate as a
vitamin.
Absorption & transport:
Dietary folates are converted to methylTHF during absorption through the upper small
intestine. Once inside the cell they are converted to folate polyglutamates.
Folate binding proteins are present on cell surfaces including the enterocyte and facilitate
entry of reduced folates into cells.
There is no specific plasma protein that enhances cellular folate uptake.
Vitamin B12 deficiency:
In Western countries, severe deficiency is usually caused by pernicious anaemia ((This is
caused by autoimmune attack on the gastric mucosa leading to atrophy of the stomach &
secretion of IF is absent)).
Less commonly, it may be caused by veganism in which the diet lacks B12, gastrectomy or
small intestinal lesions. There is no syndrome of B12 deficiency as a result of increased
utilization or loss of the vitamin ((the deficiency takes at least 2 years to develop)).
Folate deficiency:
This is most often a result of a poor dietary intake of folate alone or in combination with a
condition of increased folate utilization or malabsorption.
Excess cell turnover of any sort, including pregnancy, is the main cause of an increased need
for folate, because the folate molecule becomes degraded when DNA synthesis is increased.
Laboratory findings:
The anemia is macrocytic (MCV >95 fL and often as high as 120 fL in severe cases) and the
macrocytes are typically oval in shape. The reticulocyte count is low and the total white cell
and platelet counts may be moderately reduced, especially in severely anemic patients.
A proportion of the neutrophils show hypersegmented nuclei (with six or more lobes).
The bone marrow is usually hypercellular and the erythroblasts are large and show failure of
nuclear maturation but normal hemoglobinization (megaloblastic changes).
The biochemical basis of
megaloblastic anaemia caused
by vitamin BI2 or folate
deficiency.
The serum unconjugated bilirubin and lactate dehydrogenase (LDH) are raised as a result of
marrow cell breakdown.
Diagnosis:
a) Check serum B12 and serum and red cell folate.
b) Tests for the cause of vitamin B12 or folate deficiency accordingly.
Treatment
Most cases only need therapy with the appropriate vitamin. The patient feels better after
24-48 h of correct vitamin therapy with increased appetite and wellbeing.
Differential Diagnosis of Macrocytic Anemia :
ﺍﻟﺩﻛﺗﻭﺭﺍﻻﺧﺗﺻﺎﺹ
ﻋﻠﻲ ﻋﺒﻴﺪ ﺍﺒﺭﺍﻫﻴﻢ ﺍﻟﺨﻔﺎﺠﻲ
ﺑﻭﺭﺩ )ﺩﻛﺗﻭﺭﺍﻩ ( ﺍﻣﺭﺍﺽ ﺍﻟﺩﻡ
M.B.Ch.B. F.I.C.M.S
