Cardiac Examination
•Inspection
• Palpation
• Percussion
• Auscultation

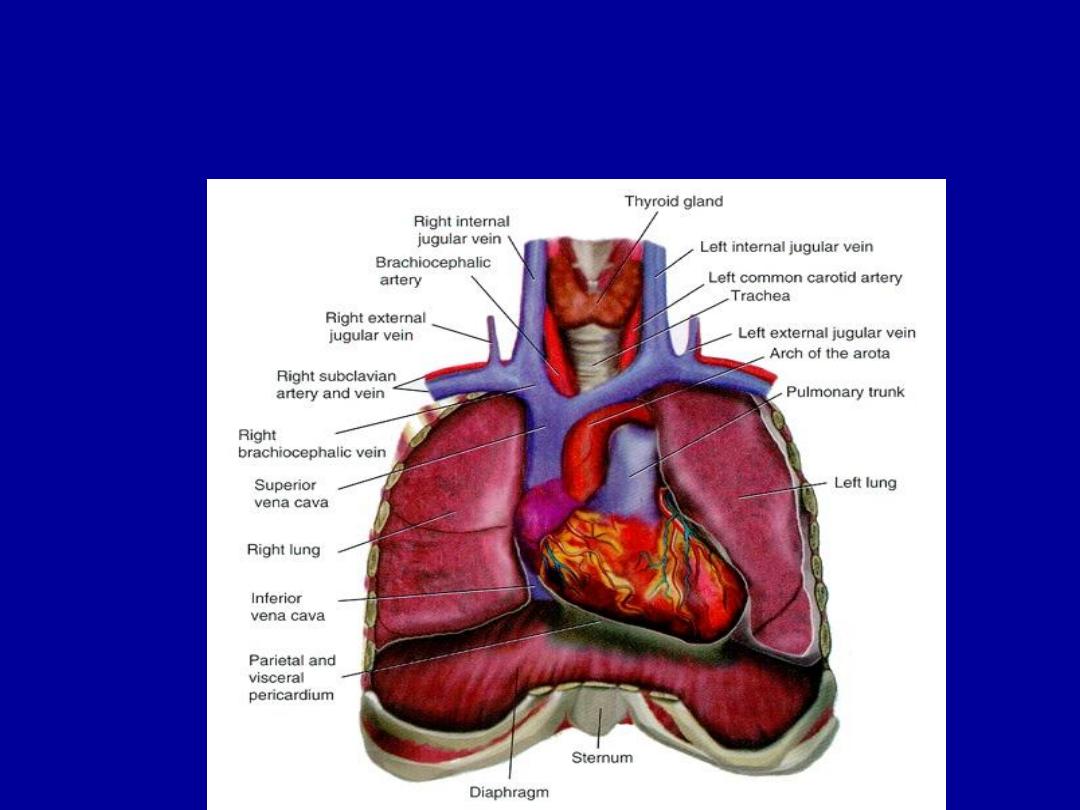
Cardiovascular Anatomy
• Heart :
is shaped like
“Cone”
• “top” of the heart is the base
• “bottom” is the apex
• Heart size = clenched fist
• Precordium: area on anterior chest that
covers heart and great vessels
• Atria :
are tilted slightly toward the back
and
ventricles
:extend to left and toward
anterior chest wall
Assessment of the Heart, Great vessels of
the neck, and Peripheral Vascular system


• Inspection :
1.
Apex beat .
2.
left parasternal movement due to right
ventricular hypertrophy.
3.
pulsation in 2d left ICS 2ry to enlarged
PA.
4.
epigastric pulsation 2ry to expanded
abdominal aorta .

• 5-chest wall deformity (pectus excavatum,
carinatum)
• 6-scars (thoracotomy, pacemaker)
• 7-dilated veins

Palpation
By PALPATION
• Explain the procedure to the patient
• - Ensure the patient is in a supine position
at an angle of 45 degs.
• - Ask the patient to breathe normally.
:
➡
Apex
beat:It
is primarily due to recoil of the
heart
’s apex as blood is expelled during systole
.
➡
Site
(the most lateral and most inferior; normally in
the 5th left intercostals space in the mid clavicular
line)
Displaced or not
Character
( tapping ,thrusting ,heaving)
➡
Parasternal impulse:
•
By the heel of the hand rested just to the left of
the sternum.

• Palpation :
• Left parasternal heave : at the left sternal
border due to right ventricle hypertrophy
• Palpable second heart sound at the
base of the heart (2
nd
intercostal space )
due to loud s2 ex: pulmonary
hypertension .

➡
Palpable murmurs (thrills):
•
Start at the apex then the left sternal
edge and the base of the heart.
• Either systolic or diastolic thrills according
• to timing with carotid or apex beat .
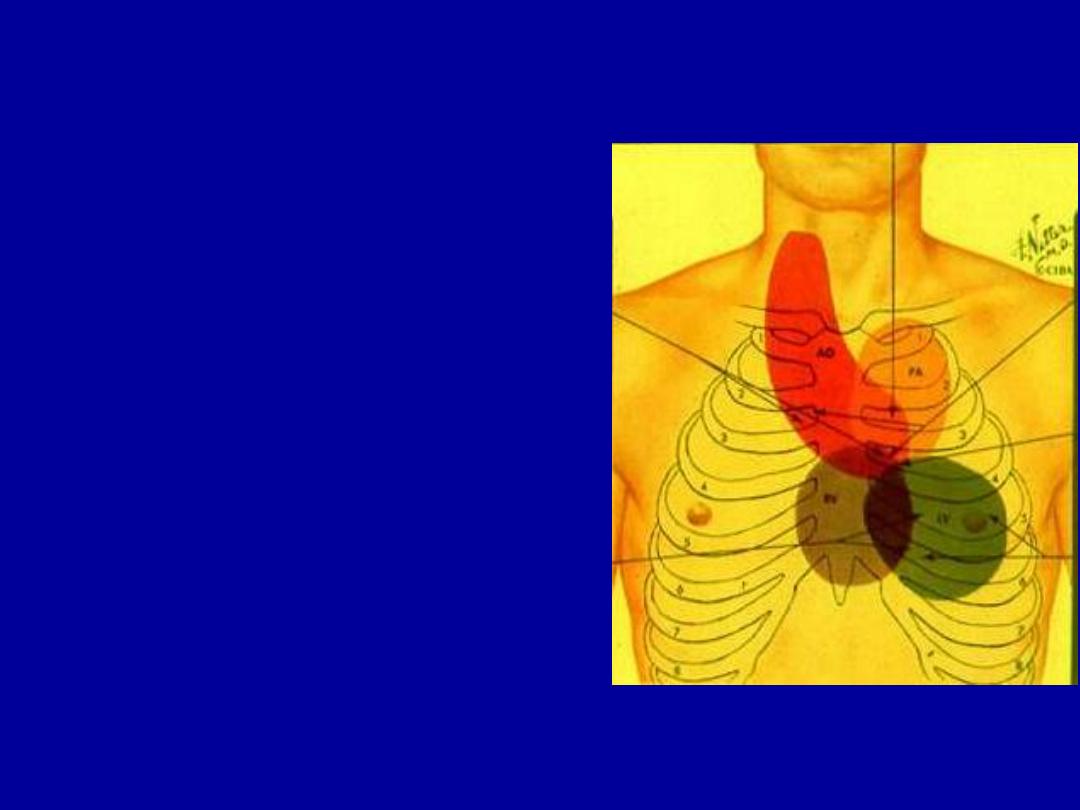
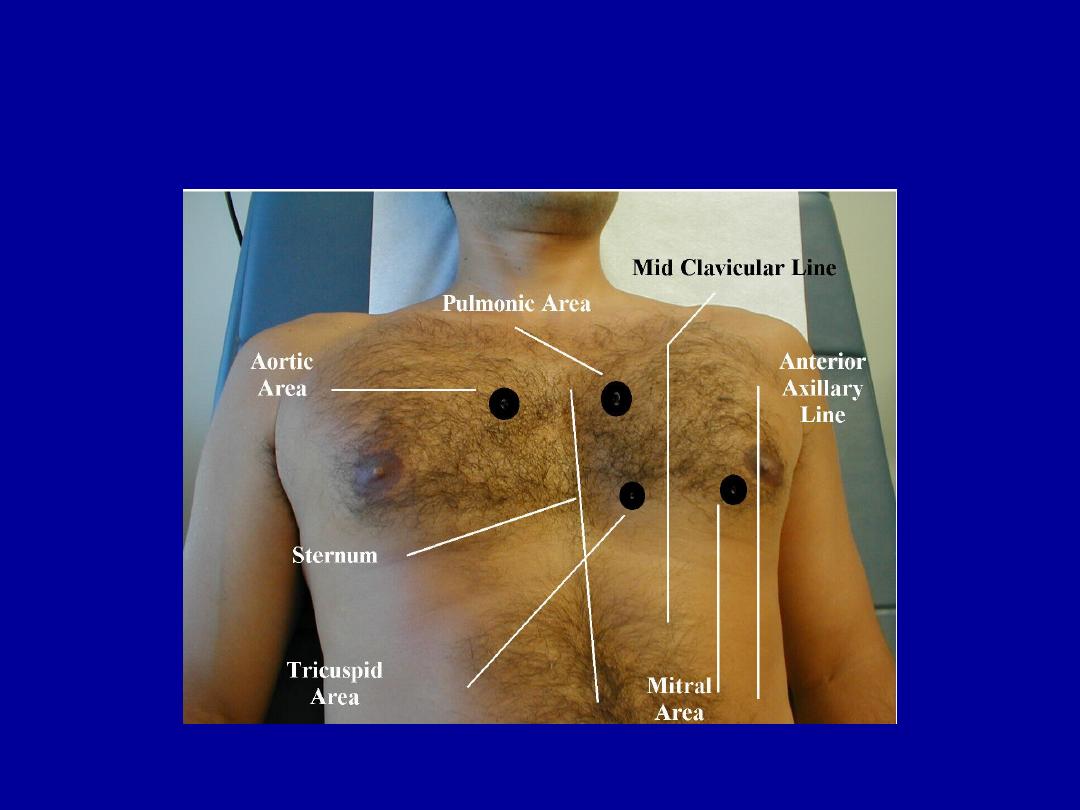
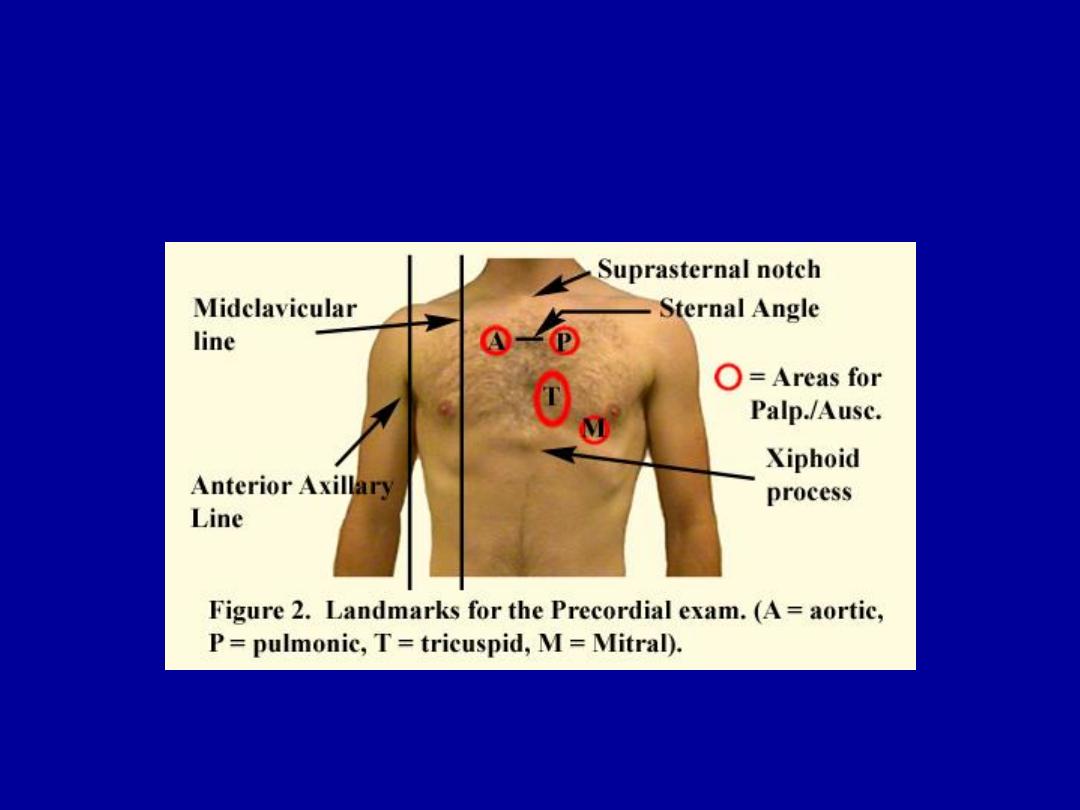
I. Auscultatory Valve Area
1. MV: apex, fifth left intercostal
space, medial to the
midclavicular line
2. PV: second left intercostal space
3. AV: second right intercostal space
4. AV
2
: left third intercostal space
5. TV: lower part of sternal

–
Auscultation:
–
bell
to detect low-pitched sounds ,
press lightly against the skin
–
diaphragm
detect high-pitched
sounds
–
press firmly against the skin

Cardiovascular: Heart Sounds
• Heart sounds: lub dub
• SYSTOLE: lub= S1 (closing of AV valves)
• DIASTOLE: dub = S2 (closing of semilunar
valves)
• During the cardiac cycle, valves are opening
and closing, causing different heart sounds
(S1 and S2).
• Sometimes abnormal heart sounds are
heard due to improper opening or closing of
the valves.(murmurs)

AUSCULTATION
• S
1
– closure of mitral and tricuspid valves
• S
2
– closure of aortic and pulmonic valves
• Low pitched sounds S
3
, S
4
, mitral stenosis,
• S
1
systole S
2
diastole S
1

Cont. auscultation
•
Normally audible heart sounds:
1
st
& 2
nd
HS
•
Added sounds: 3
rd
& 4
th
HS, pericardial
friction rub (pericarditis), opening snap
(m.s), mitral click(m.v.p)
•
murmers

Murmurs
• Turbulent blood flow caused by diseased
valve or if a large amount of blood flows
through a normal valve.
• characteristics of murmurs suggest the
cause of it (site, radiation, pitch, timing
gradig and the intensity) .

Cont.
• Site;
area over which a murmur is best
heared depends upon the valve of origin
and the direction of the blood flow.
(Mitral m.at apex, aortic m.at right 2
nd
ICS)
• Radiation;
occurs along line of blood flow.
(MR radiate to the axilla
… AS» neck,
Cont.
• Pitch
;
high pitch murmurs MR &AR
• Low pitch murmurs MS & AS
• Timing
;
in relation to the1
st
and the 2
nd
HS
Systolic;
time between 1
st
and the 2
nd
HS, could be mid-
systolic (AS), pansystolic (MR).
Diastolic;
time between 2
nd
and the 1
st
HS, can be divided
into tow phases. Early (AR), Mid-diastole (MS).

Grading of Murmurs:
Grade 1 - only a staff man can hear
Grade 2 - audible to a resident
Grade 3 - audible to a medical student
Grade 4 - associated with a thrill or palpable heart
sound
Grade 5 - audible with the stethoscope partially off the
chest
Grade 6 - audible at the bed-side
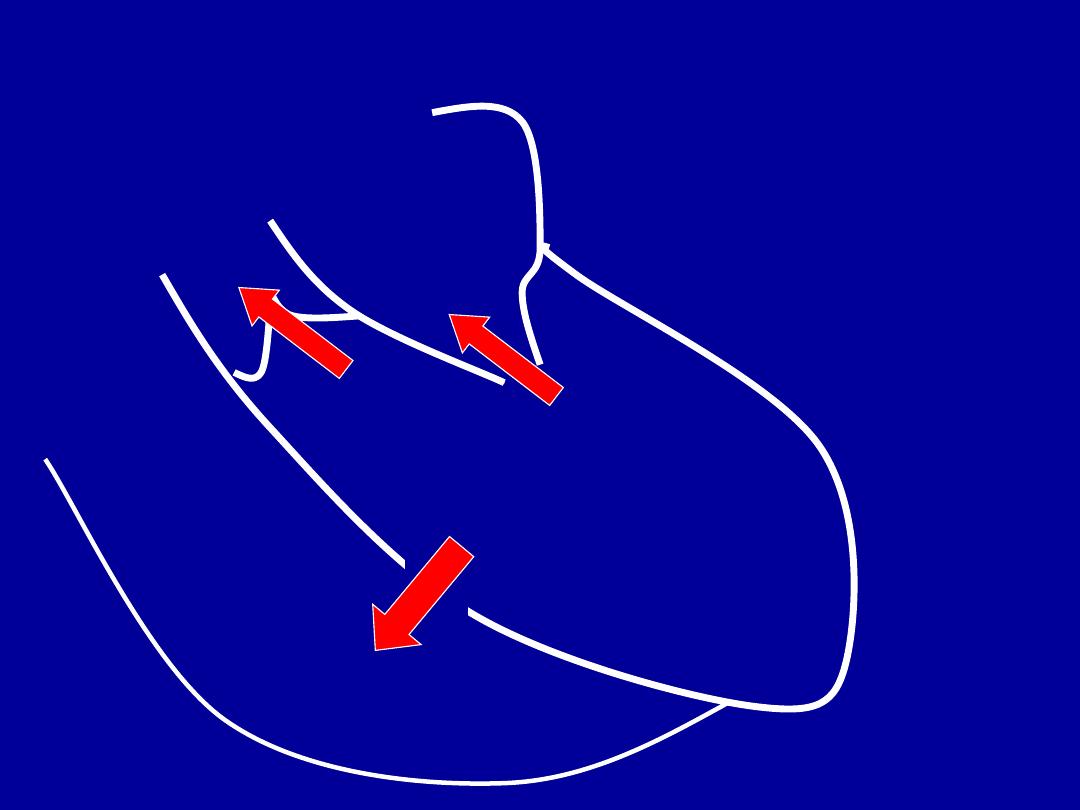
LA
LV
AO
Systole
RV
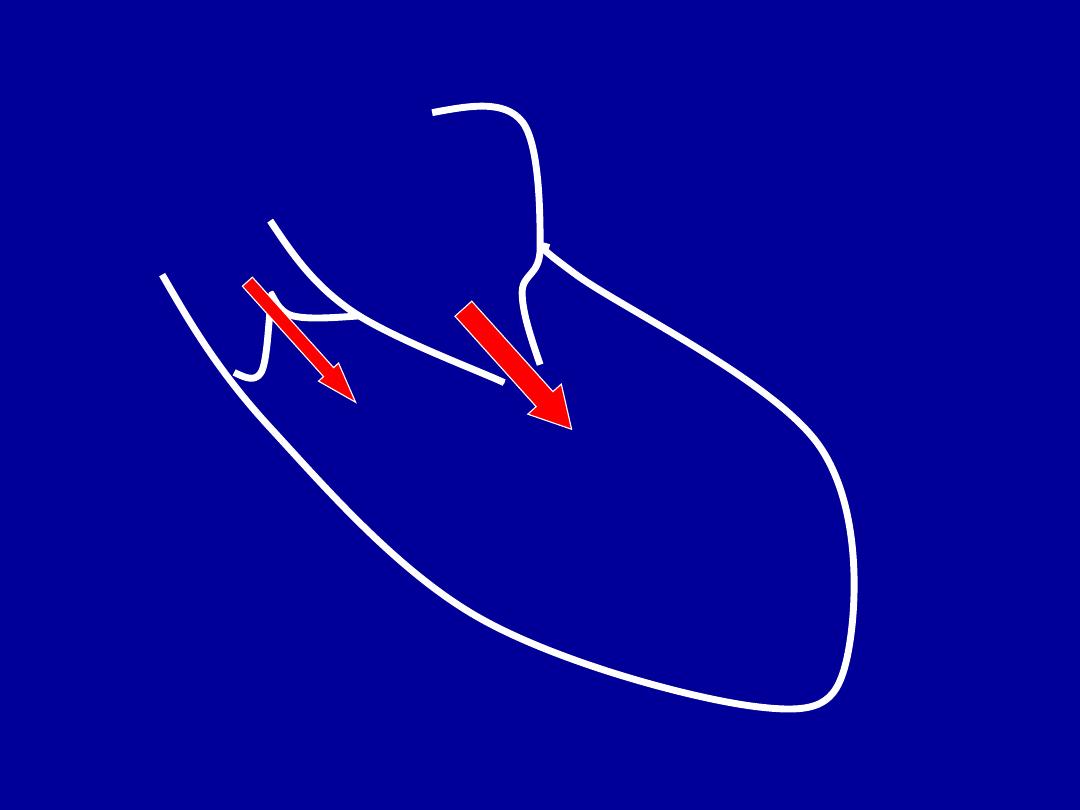
LA
LV
AO
Diastole
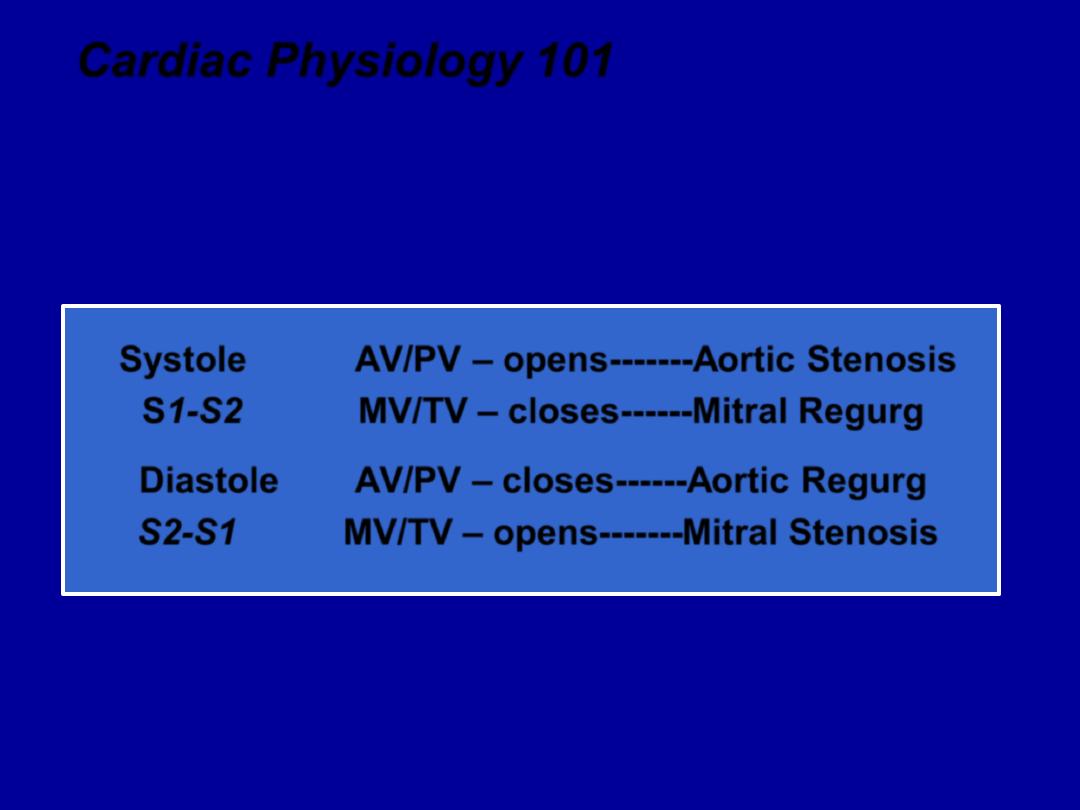
Cardiac Physiology 101
Regurg/ Insuff
– leaking
(backflow)
of blood across a
closed
valve
Stenosis
– Obstruction of
(forward)
flow across an
opened
valve
Systole
AV/PV
–
opens
-------
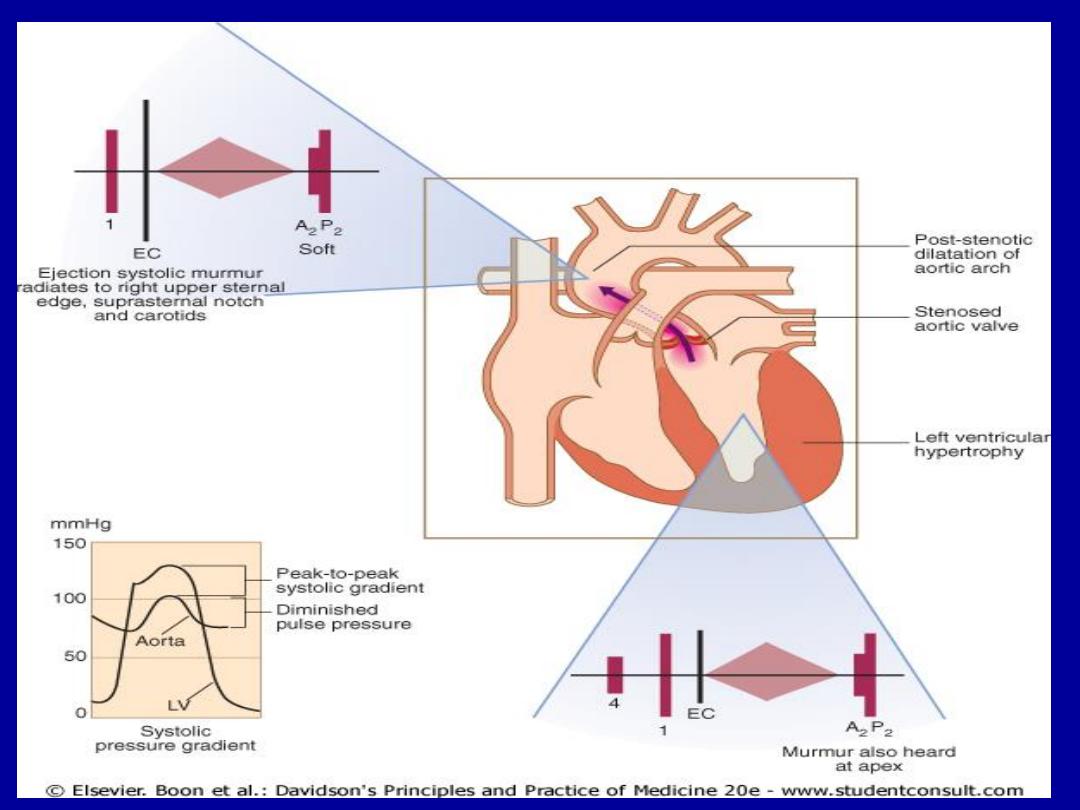
Aortic Stenosis
S1-S2
MV/TV
–
closes
------
Mitral Regurg
Diastole
AV/PV
–
closes
------
Aortic Regurg
S2-S1
MV/TV
–
opens
-------
Mitral Stenosis
These concepts are set in stone, it can
’t occur any other way,
It would be anatomically impossible
Common Murmurs and
Timing
(click on murmur to play)
Systolic Murmurs
• Aortic stenosis
• Mitral insufficiency
• Mitral valve prolapse
• Tricuspid insufficiency
Diastolic Murmurs
• Aortic insufficiency
• Mitral stenosis
S1 S2 S1

Holosystolic Murmurs
• Atrioventricular valve leakage
– Mitral Regurgitation
– Tricuspid Regurgitation
• Interventricular shunt
– Ventricular septal defect

Holosystolic Murmurs
• “Pansystolic Murmurs”
• Begin with S1 and end after S2
• Caused by flow from high pressure area to
much lower pressure area
– Ventricle to atrium
– Left ventricle to right ventricle

MR
• Radiates to axilla or back in most cases
• May radiate to the base if posterior leaflet
prolapse
• Well heard with diaphragm but listen with
bell also for S3 or diastolic
“flow” rumble
– Due to high volume flowing back from LA
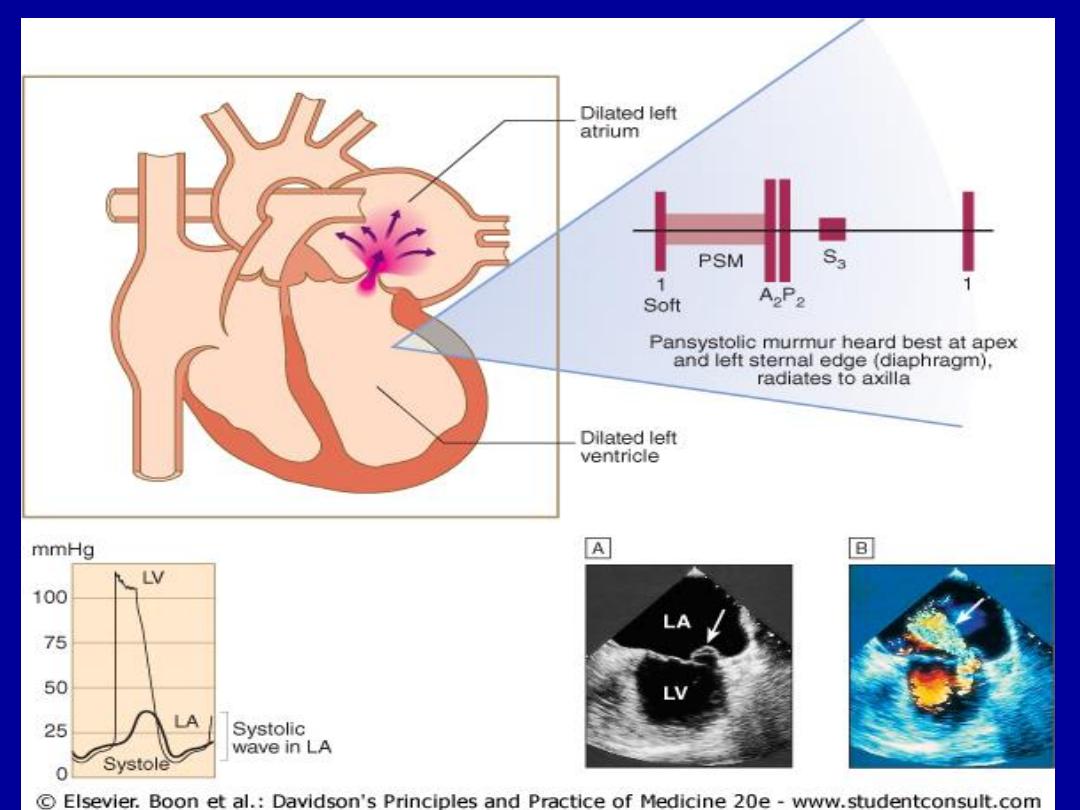
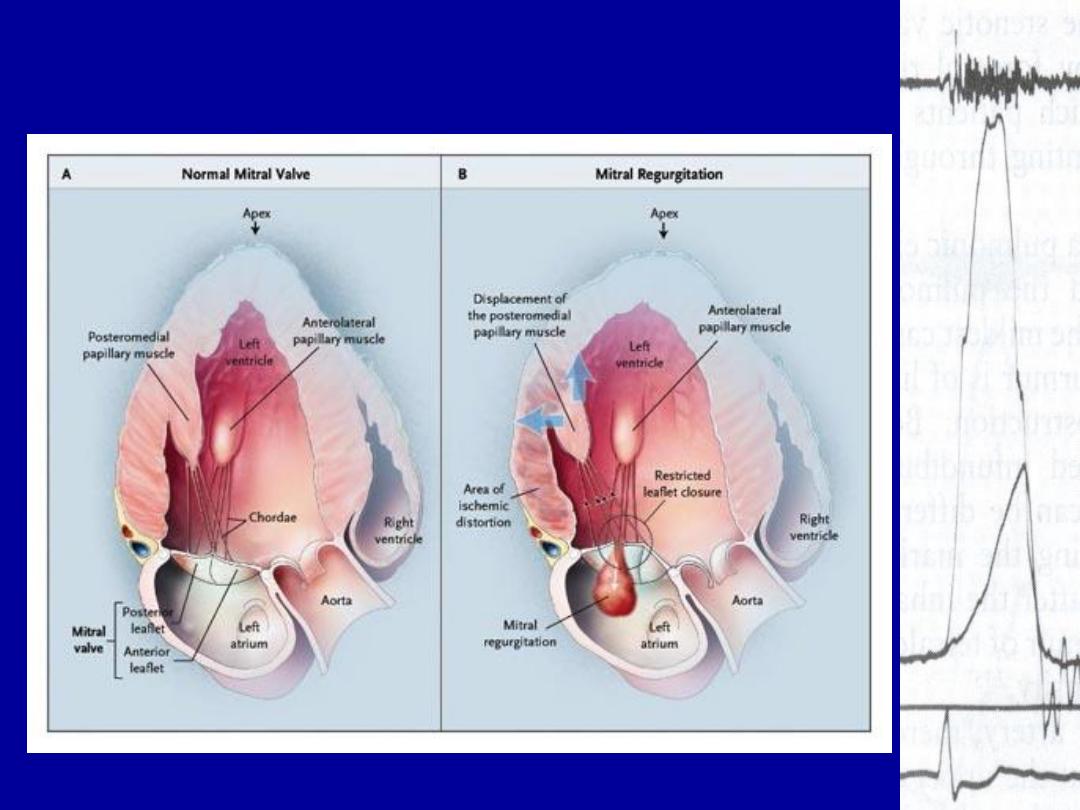
Mitral Regurgitation after MI
Aortic Stenosis
• The typical murmur of aortic stenosis is
harsh, similar to the sound of clearing
one
’s throat. Aortic events are usually well
heard at the apex.
• The murmur of aortic stenosis
characteristically radiates up into the
supraclavicular area of the neck, over the
carotids, and the suprasternal notch.
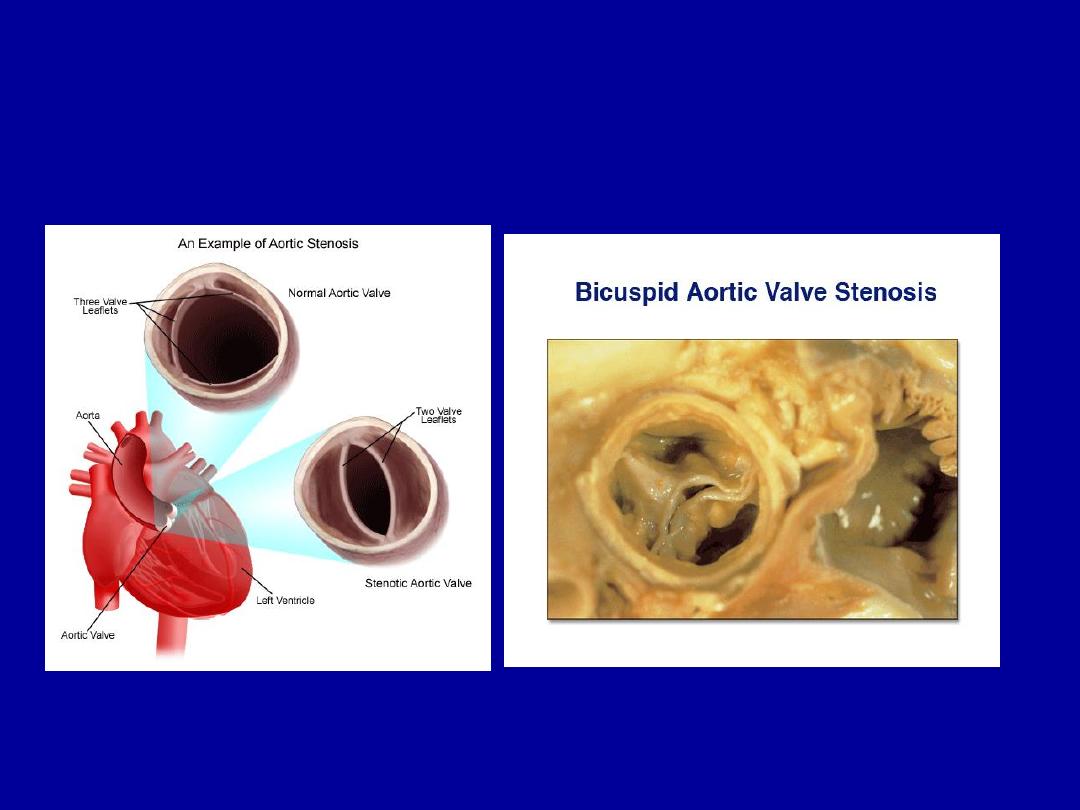
Aortic Stenosis

Pulmonic Stenosis
• Usually congenital, may be associated with other
abnormalities
• Causes a mid-systolic ejection murmur similar to
AS but does NOT radiate to carotids
– Radiates to left infraclavicular area
– Murmur intensity and ejection sound vary with
respiration
– Widened S2 split

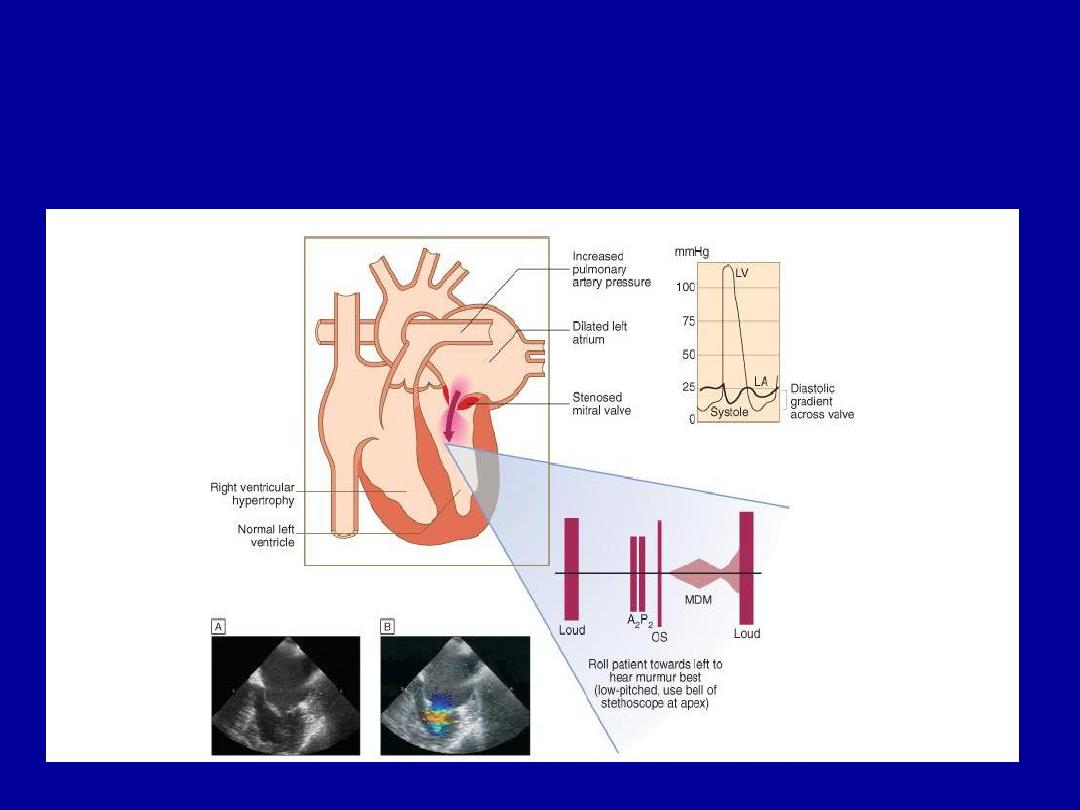
Mitral Stenosis
• “always” rheumatic in origin
• Turbulent, high velocity flow occurs during
diastole
• Always look for MS in patient with new
Atrial fibrillation

Mitral Stenosis
• Loud S1, present
• -
normal
S2
• Opening snap
• .
Rumbling mid-diastolic murmur
– heard at apex with stethoscope bell, patient in L
lateral decubitus
– Palpate carotid to identify diastole

Left lateral decubitus

Aortic Regurgitation
• congenital, endocarditis, age,
aortic disease, collagen vascular,
syphillis
• Early diastolic, decrescendo
murmur best heard at LLSB with
diaphragm

Aortic regurgitation findings
• Soft S1 and A2
• Blowing decrescendo diastolic
murmur
– Begins immediately with A2
– High frequency (diaphragm)
• Press firmly & concentrate
–
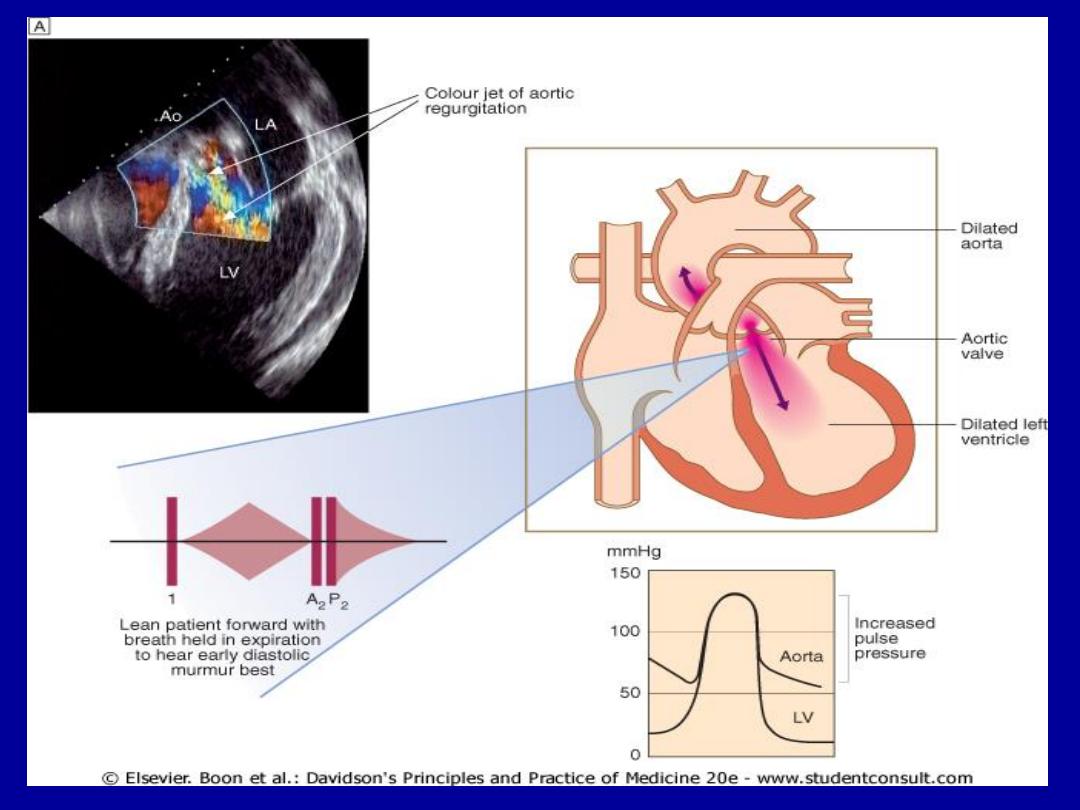

AR easily missed
Aortic Regurgitation
• Positions and techniques for auscultation:
• The murmurs of aortic regurgitation are
generally heard when the patient is sitting
upright, leaning forward, breath held in
deep expiration.

Additional findings
• Wide pulse pressure with low diastolic
– “Water hammer pulses”
• Durrosiez’s sign
– To and fro bruit at femoral artery
• Quinke’s sign
– Nailbeds flush with systole
• de Musset's sign (Head nodding in time
with the heart beat)
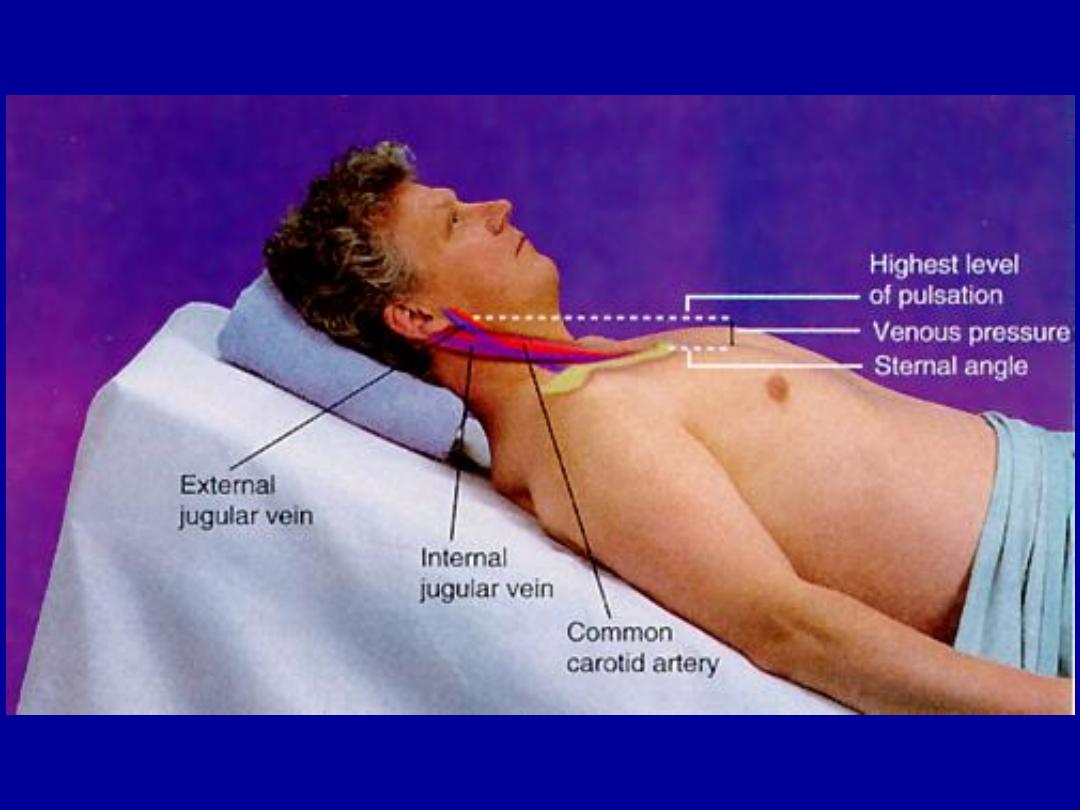
JUGULAR VENOUS DISTENTION
