د.سالم
Endocrinological Emergencies
seminar
1-Diabetic ketoacidosis (DKA)
INTRODUCTION :
Diabetic ketoacidosis (DKA) is an acute, major, life-threatening
complication of diabetes that mainly occurs in patients with type 1
diabetes, but it is not uncommon in some patients with type 2 diabetes.
This condition is a complex disordered metabolic state characterized by:
hyperglycemia: blood glucose level > 200 mg/ dl
-
Ketoacidosis: ketonuria > ++ on standard urine sample.
-
Metabolic acidosis: PH < 7.3, s. bicarbonate < 15
-
Pathophysiology
DKA typically occurs in the setting of hyperglycemia with relative or
absolute insulin deficiency and an increase in counterregulatory
hormones.
Sufficient amounts of insulin are not present to suppress lipolysis and
oxidation of free fatty acids, which results in ketone body production
and subsequent metabolic acidosis.
DKA occurs more frequently with type 1 diabetes, although 10% to
30% of cases occur in patients with type 2 diabetes.
Predisposing Factors
:
Several risk factors can precipitate the
development of extreme hyperglycemia:
infection.
-
intentional or inadvertent insulin therapy.
-
myocardial infarction.
-
Stress.
-
trauma.
-
- confounding medications, such as glucocorticoids or atypical
antipsychotic agents.
Clinical Presentation
The most common early symptoms of DKA are the insidious increase in
polydipsia and polyuria.
The following are other signs and symptoms of DKA:
-Malaise, generalized weakness, and fatigability
-Nausea and vomiting; may be associated with diffuse abdominal pain,
decreased appetite, and anorexia
Rapid weight loss in patients newly diagnosed with type 1 diabetes
-
-History of failure to comply with insulin therapy or missed insulin
injections due to vomiting or psychological reasons or history of
mechanical failure of insulin infusion pump
-Decreased perspiration
-Altered consciousness (eg, mild disorientation, confusion)
Signs and symptoms of DKA associated with possible intercurrent
infection are as follows:
-Fever
-Coughing
-Chills
-Chest pain
-Dyspnea
-Arthralgia
-Urinary symptoms
On examination
Ill appearance
-
Dry skin
-
Labored respiration
-
Dry mucous membranes
-
Decreased skin turgor
-
Decreased reflexes
-
Characteristic acetone (ketotic) breath odor
-
Tachycardia
-
Hypotension
-
Tachypnea
-
Investigations
-Serum glucose level
-Serum electrolyte levels
-Amylase and lipase levels
-Urine dipstick
-Ketone levels
-ABG measurements
-CBC count
-BUN and creatinine levels
-C-RP
-Urine and blood cultures if intercurrent infection is suspected
-ECG
-Chest radiography: to rule out pulmonary infection
-Head CT scanning: to detect early cerebral edema.
Management:
Managing diabetic ketoacidosis (DKA) in an intensive care unit during
the first 24-48 hours always is advisable.
Plan for therapy:
When treating patients with DKA, the following points must be
considered and closely monitored:
Correction of fluid loss with intravenous fluids
-
Correction of hyperglycemia with insulin
-
Correction of electrolyte disturbances, particularly potassium loss
-
Correction of acid-base balance
-
Treatment of concurrent infection, if present
-
Laboratory studies for diabetic ketoacidosis (DKA) should be scheduled
as follows:
-Blood tests for glucose every 1-2 h until patient is stable, then every 4-6
h
-Serum electrolyte determinations every 1-2 h until patient is stable,
then every 4-6 h
-Initial blood urea
-Initial arterial blood gas (ABG) measurements, followed with
bicarbonate as necessary
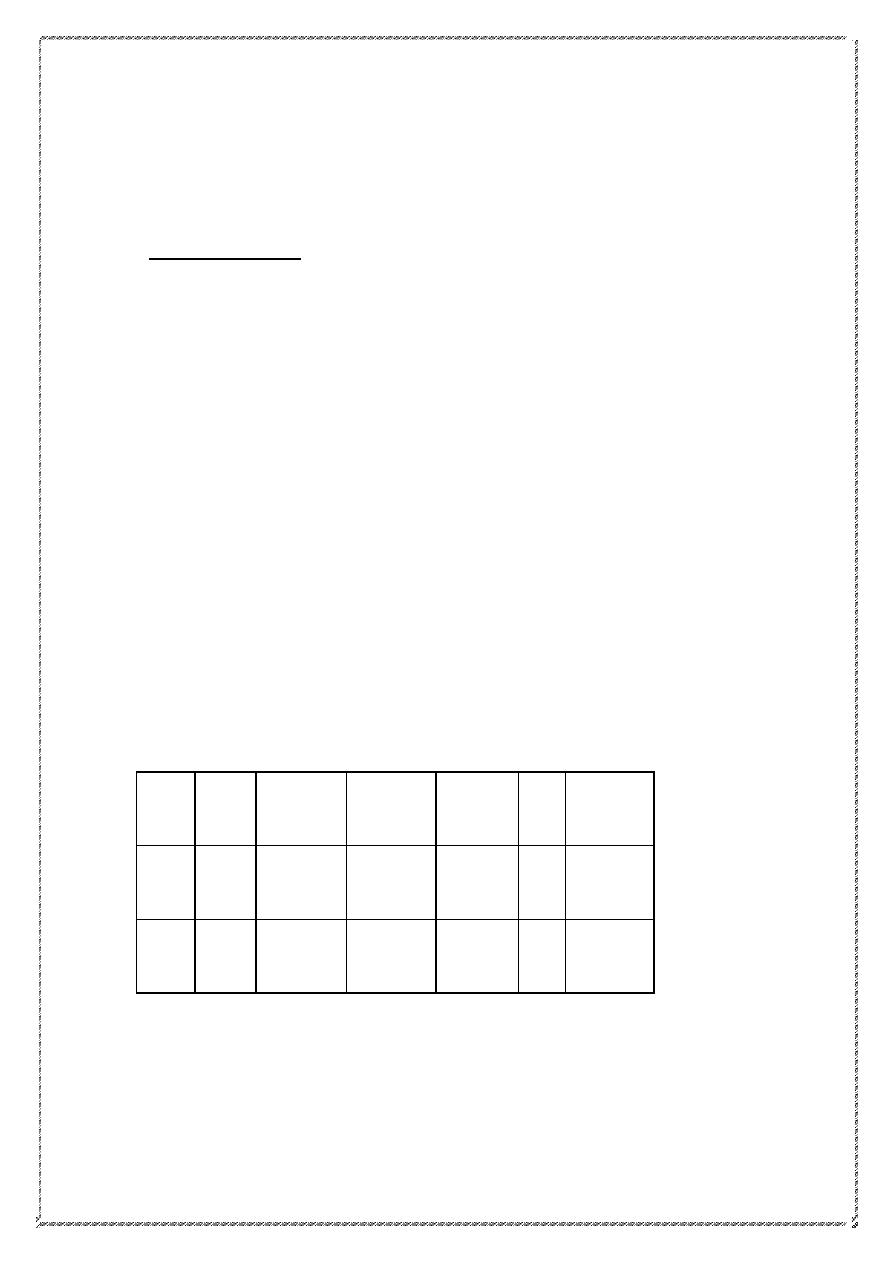
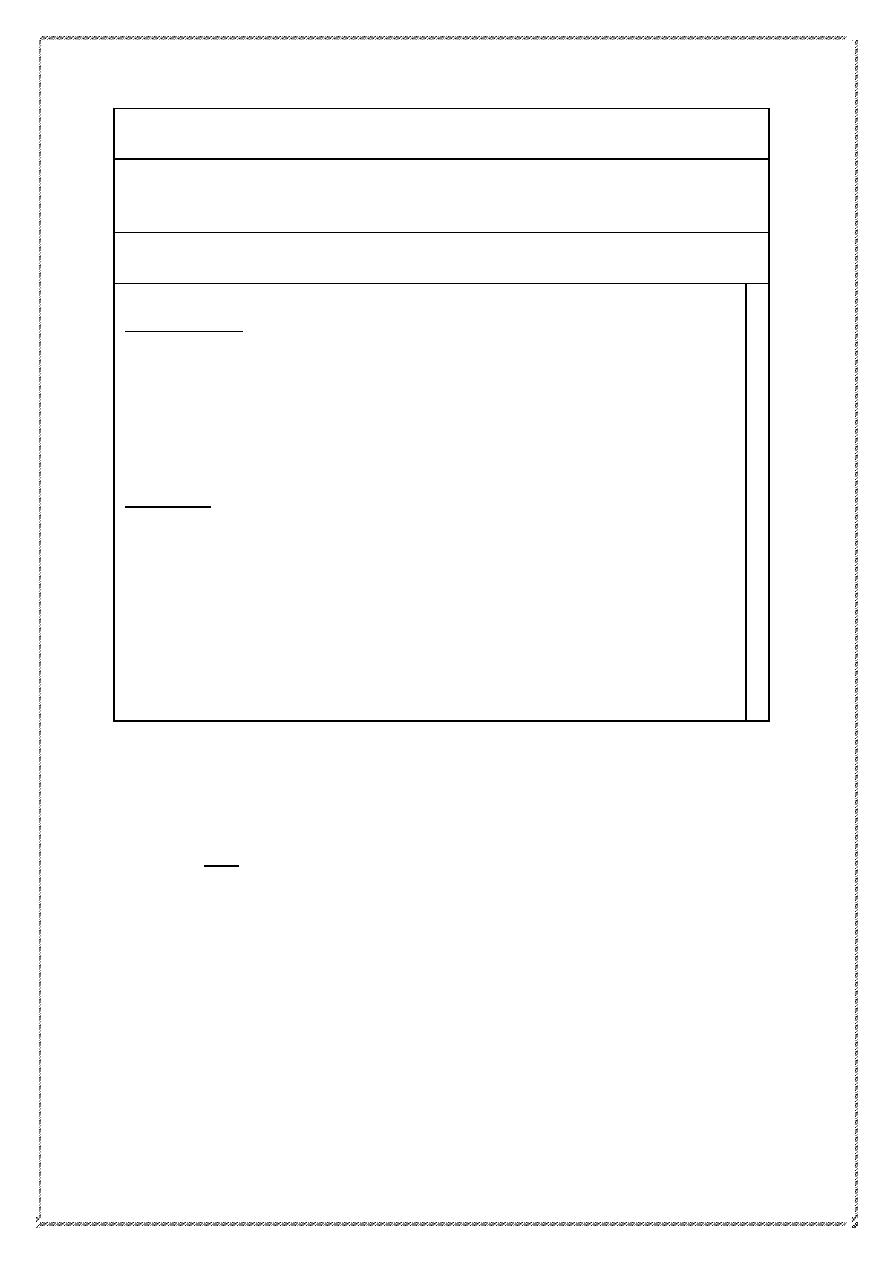
Example how to arrange a chart to follow a DKA patient
S. k
RBS
Output
Input
fluid
Insulin
BP
Time
6.2
410
Nil
2 L/NS
20 units
IM
80/50
3:00
PM
4:00
PM
Insulin Therapy
Using soluble (Short acting) insulin administered either:
I.V infusion(prefered method):
-
Bolus: 0.1 unit/ kg. I.V direct then maintain contiueous iv infusion of 0.1
unit/ kg./ hr. using syringe pump.
I.M:
-
Bolus: 10-20 units Followed by 5 units hourly.
Target blood sugar:
Falling 55-110 mg/ dl per hr. (3-6 mmol/l per hr)
-
Rapid decline → cerebral edema
-
Failure to reach the target → require reassessment of insulin therapy.
-
- Shift to subcutaneous insulin regimen when the patient vomiting
stopped and become biochemically stable.
Fluid Replacement:
Average of 6 litres fluid deficit exist
3 L are extracellular replaced by 0.9% isotonic saline.
3 L are intracellular replaced by dextrose
Set 2 wide bore IV line initially
Timing and amount as following:
1
st
hr: using normal (isotonic) saline
-
systolic BP > 90 mmHg → 1 L
systolic BP < 90 mmHg → 2 L
Then as :
-
1 L OVER 2 hrs
1 L OVER 2 hrs
1 L EVERY 6 hrs
Note : Shift to 10% dextrose fluid whenever blood sugar level become <
250 mg/dl (14mmol/l).
: be cautious with elderly, pregnant, those with heart or renal
Note
failure.
Potassium Replacememt
According to serum potassium level as:
-
> 5.5 mmol/l → non to be given
3.5 – 5.5 (mmol/l) → 40 meq/l
- be cautious in replacing K usually hyperkalemia occurs initially due to
prerenal failure secondary to dehydration for that reason K is not
recommended to be given in the first hour of therapy.
Others:
Acidosis: is usually corrected with the time by adequate fluid and insulin
replacement. Bicarbonate therapy is not recommended as it can induce
cerebral edema
Infection: should be treated by antibiotcs accordingly
Brain edema: is the leading cause of death in DKA, it can exist in spite of
metabolic stablisation. It should be treated by mannitol solution 20%
(7 ml/ kg.)
Case Scenario
A 20-year-old woman is evaluated in the emergency department for
polyuria, polydipsia, polyphagia, and an unintentional 5.4-kg (11.9-lb)
weight loss over the past month. She has had increasing lethargy over
the last 24 hours. Her medical history and family history are
unremarkable. She takes no medications.
On physical examination,
temperature is 37.5 °C , blood pressure is 98/52 mm Hg, pulse rate is
120/min, and respiration rate is 30/min. BMI is 17.
She is lethargic with dry mucous membranes, tachypnea, and
tachycardia. Chest auscultation is clear. Abdominal examination shows
diffuse mild tenderness and normal bowel sounds. There is no
rebound tenderness or guarding with palpation.
Laboratory studies:
Hemoglobin= 17 g/dL (170 g/L)
Leukocyte count= 14,200/µL (14.2 × 10
9
/L)
Blood gases, arterial::
pH= 7.25
PCO
2
= 21 mm Hg
Creatinine= 1.3 mg/dL
Electrolytes
Sodium= 130 mEq/L
Potassium= 3.0 mEq/L
Chloride= 99 mEq/L
Bicarbonate= 9 mEq/L
Glucose= 620 mg/dL (34.4 mmol/L)
An electrocardiogram shows sinus tachycardia 120/min.
Chest radiograph is normal.
What is the most appropriate management?
2-Hypoglycemia
Means blood glucose level < 63 mg/ dl (3.5 mmol/l) which is a common
complication in diabetes [ those on insulin therapy or on oral insulin
secretagoues especially sulphonylurea as Glibenclimide].
Risk factors:
1- strict glycemic control
2- extreme of age( elderly & young)
3- renal impairment
4- impaired awareness of hypoglycemia
5- long duration of DM
6- pevious history of hypoglycemia
Causes:
1- missed or inadequate meal
2- error in therapy or poorly designed regimen
3- exercise
4- alcohol
5- lipohypertrophy at site of insulin injection.
6- factitious
7- breastfeeding
Clinical presentation:
Autonomic symptoms: sweating, hunger, anxiety, trembling.
-
- Neuroglycopenic symptoms: confusion, inability to concentrate,
drowsiness, incoordination, slurring of speech, coma.
Non specific: nausea, headache
-
is common and usually not awake the person,
Nocturnal hypoglycemia
-
described as poor sleep, morning headache, vivid dreams. The partner
may notice sweating, twitching and seizure. It can be fatal in rare cases
( dead-in-bed syndrome)
means hypoglycemia that exist in non
:
hypoglycaemia
Spontaneous
-
diabetic person (uncommon condition).
Confirmed by whipple s criteria:
1- symptoms of hypoglycemia
2-low blood glucose
3- symptoms resolved by correction of blood sugar.
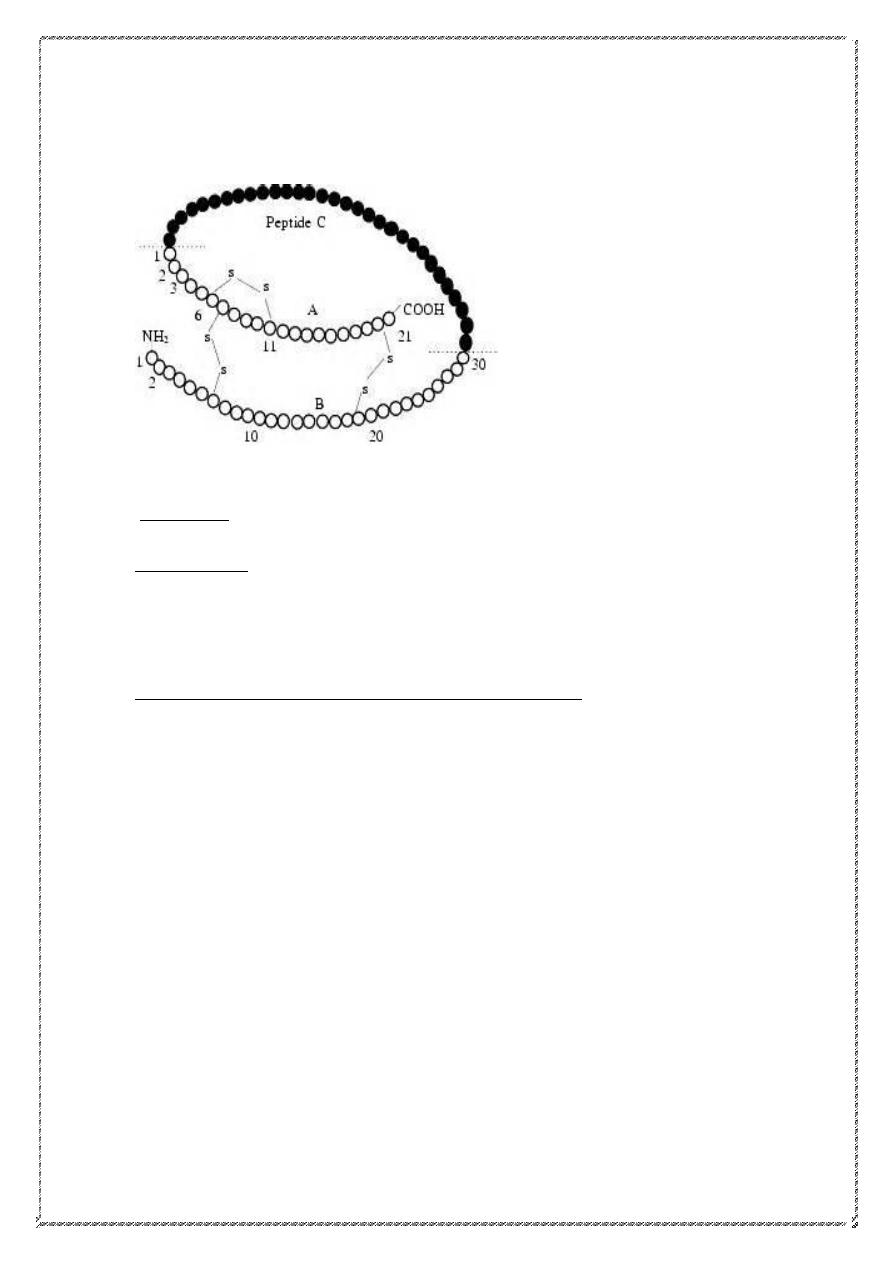
Assessed by doing serum insulin & Cpeptide level.
Management of Hypoglycemia:
ollowed by snack of complex
Glucose f
15 gm
-
: oral 10
Mild cases
carbohydrate content.
:
Severe cases
1- I.V hypertonic glucose 50% (30 ml) or 70 ml 20 %
2- I.M glucagon 1 mg
3- if the patient is conscious; 25 gm of oral refined sugar.
exclude
we should
then
if the patient fail to respond
1- cerebral edema
2- alcohol intoxicaion
3- post ictal state
4- cerebral hemorrhage
3-Adrenal insufficiency
Secondary (↓ACTH)
• Withdrawal of suppressive glucocorticoid therapy
• Hypothalamic or pituitary disease
Primary (↑ACTH)
Addison’s disease
Common causes
-Autoimmune
Sporadic
Polyglandular syndromes
-Tuberculosis
-HIV/AIDS
-Metastatic carcinoma
- Bilateral adrenalectomy
Rare causes
-Lymphoma
-Intra-adrenal haemorrhage
(Waterhouse–Friedrichsen syndrome following meningococcal septicaemia)
-Amyloidosis
-Haemochromatosis
-Corticosteroid biosynthetic enzyme defects
-Congenital adrenal hyperplasias
-Drugs :
(Metyrapone, ketoconazole, etomidate)
Clinical presentation of adrenal crisis :
presence of intercurrent infection, or surgery.
-
severe hypotension
-
, Ca ↑
K ↑
Na ↓,
-
Hypoglycaemia
-
muscle cramp
-
nausea, vomiting , diarrhea
-
unexplained fever
-
Investigations:
random plasma cortisol
-
short synacthin test
-
Management:
- volume replacement by isotonic saline to correct hyponatremia, and
hyperkalemia
- hydrocortisone 100 mg I.V, then 50-100 mg every 6 hrs. till the patient
tolerate oral steroid
-correct hypoglycemia
-Correct any underlying cause.
Thyrotoxic crisis: is a rare life threatening condition, usually result
from infection of a previously unrecognised or inadeqately treated
hyperthyroid state.
Presentation:
Fever
-
Tachycardia or atrial fibrillation
-
Agitation or confusion
-
Acute heart failure
-
Management
1- rehydration
2- propranolol 80 mg * 4 orally OR 1-5 mg * 4 I.V
3- sodium ipodate
4- Lugol s solution ( k iodide)
5- dexamethasone 2 mg * 4
6- carbimazole 40-60 mg/ day
Myxoedema coma: is a rare and fatal condition of old age. Usually
patient present with disturb level of consciousness with severe
hypothermia ( as low as 25 C), and convulsions.
Treatment:
1- I.V triiodothyronin ( T 3)… later by levothyroxine 50 Mg
2- rewarming
3- hydrocortisone
Sheehan syndrome(Hypopituitarism) :
- one of the commonest causes of panhypopituitarism, which occur as a
result of postpartum hemorrhage.
- During pregnancy the pituitary gland enlarges, so when bleeding exist
the hypophyseal vessele constrict (vasospasm) causing necrosis of the
pituitary gland.
Clinical presentation:
1- first symptom is inability of breast feeding
2- adrenal insufficiency
3- hypothyroidism
4- amenorrhea
5- diabetes insipidus
6- pallor ?
Management:
1- Cortisol replacement: H.C 15- 20 mg / day
2- Thyroxine 50-150 Mg / day
3- Sex hormone replacement for those below 50 years
اليسهر الليل م
كم
ل الدرس وحافظه
بل يسهر الليل تارك السج والسشن
ال يسهر الليل فاقد النت او قاطعه
بل يسهر الليل مدمن الفيس والفلم
