heart Failure
Clinical syndrome that develops when the heart cannot maintain adequate output, or
can do so only at the expense of elevated ventricular filling pressure.
Results from any structural or functional abnormality that impairs the ability of the ventricle to
eject blood (Systolic Heart Failure) or to fill with blood (Diastolic Heart Failure).
The prevalence of heart failure rises with age
Almost all forms of heart disease can lead to heart failure.
Mechanisms of heart failure
Reduced ventricular contractility
CAD (segmental dysfunction) ‘cardiomyopathy(global dysfunction)
o Ventricular outflow obstruction
Hypertension, aortic stenosis (left heart failure)
Pulmonary hypertension, pulmonary stenosis (right heart failure).
Ventricular inflow obstruction Mitral stenosis, tricuspid stenosis
Ventricular volume overload Ventricular septal defect.
Arrhythmia Atrial fibrillation ,Tachycardia cardiomyopathy Complete heart block
Bradycardia.
Diastolic dysfunction
Constrictive pericarditis, Restrictive cardiomyopathy
Cardiac tamponade.
Pathophysiology
Cardiac output is determined by preload (the volume and pressure of blood in the ventricles at
the end of diastole) afterload (the volume and pressure of blood in the ventricles during
systole) and myocardial contractility.
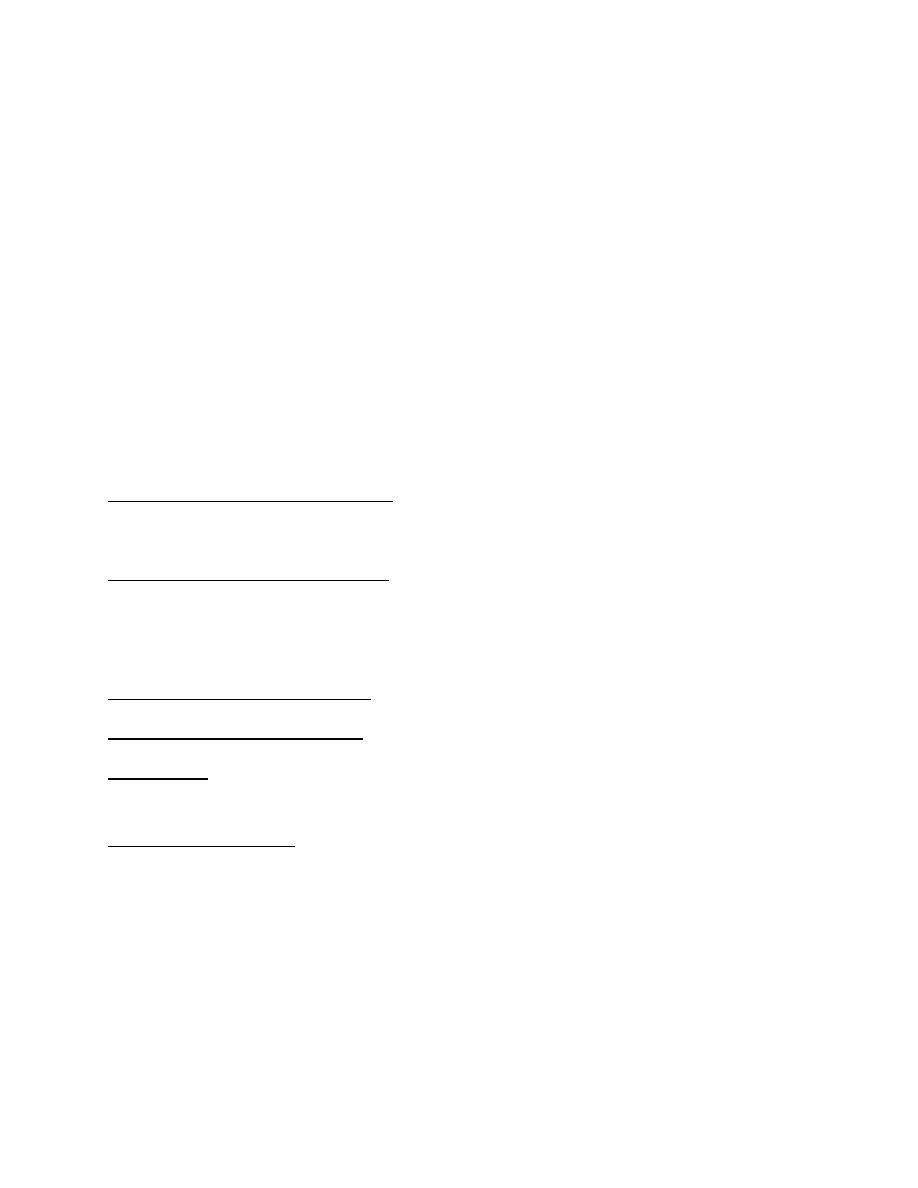
Fall in cardiac output. activates counter regulatory neurohumoral mechanisms , renin–
angiotensin–aldosterone system leads to vasoconstriction, sodium and water retention, and
sympathetic nervous system activation. Activation of the sympathetic nervous system may
initially sustain cardiac output through increased myocardial contractility (inotropy)and heart
rate (chronotropy). Prolonged sympathetic stimulation also causes negative effects, including
cardiac myocyte apoptosis, hypertrophy and focal myocardial necrosis. Sympathetic
stimulation also causes peripheral vasoconstriction and arrhythmias.
The Vicious Cycle of Congestive Heart Failure
Types of Heart Failure
-Left, right and biventricular heart failure.
-Diastolic and systolic dysfunction.
-High-output failure.
-Acute and chronic heart failure.
Causes of Low-Output Heart Failure
chronic
Systolic Dysfunction

Coronary Artery Disease
Idiopathic dilated cardiomyopathy (DCM)
Hypertension
Valvular Heart Disease
Diastolic Dysfunction
Hypertension
Coronary artery disease
Hypertrophic obstructive cardiomyopathy (HCM)
Restrictive cardiomyopathy
Factors that may precipitate or aggravate heart failure in pre-existing heart disease
Myocardial ischaemia or infarction
Intercurrent illness, e.g. infection
Arrhythmia, e.g. atrial fibrillation
Inappropriate reduction of therapy
Administration of a drug with negative inotropic (β-blocker)or fluid-retaining properties
(NSAIDs, corticosteroids)
Pulmonary embolism
Conditions associated with increased metabolic demand, e.g. pregnancy,
thyrotoxicosis, anaemia
IV fluid overload, e.g. post-operative IV infusion
Clinical Presentation of HeartFailure(Acute)
Sudden onset of dyspnoea that rapidly progresses to acute respiratory distress,
orthopnoea and cough.
The patient appears agitated, pale and clammy. The peripheries are cool to the touch
and the pulse is rapid. The BP is usually high, The jugular venous pressure (JVP) is usually
elevated.

Auscultation A ‘gallop’ rhythm, with a third heart sound, is heard. A new systolic
murmur may signify acute mitral regurgitation or ventricular septal rupture. crepitations
at the lung bases, or throughout the lungs if pulmonary oedema is severe.
Clinical Presentation of Heart Failure(Chronic)
Due to excess fluid accumulation:
Dyspnea (most sensitive symptom
Orthopnea, Paroxysmal Nocturnal Dyspnea (PND)
Edema
Hepatic congestion
Ascites
Due to reduction in cardiac output:
Fatigue (especially with exertion)
Weakness
Poor renal perfusion leads to oliguria and uraemia
Chronic heart failure is sometimes associated with marked weight loss (cardiac cachexia).
Physical Examination in Heart Failure
Dyspniac
Cool, pale, cyanotic extremities
Have sinus tachycardia, diaphoresis and peripheral vasoconstriction
Displaced Apex
S3 gallop Low sensitivity, but highly specific
Crackles or decreased breath sounds at bases (effusions) on lung exam
Elevated jugular venous pressure
Lower extremity edema
Ascites
Hepatomegaly

Splenomegaly
Complications
Renal failure
Hypokalaemia
Hyperkalaemia
Hyponatraemia
Impaired liver function
Thromboembolism
Atrial and ventricular arrhythmias
Lab Analysis in Heart Failure
CBC
Since anemia can exacerbate heart failure
Serum electrolytes and creatinine
before starting high dose diuretics
Fasting Blood glucose
To evaluate for possible diabetes mellitus
Thyroid function tests
Since thyrotoxicosis can result in A. Fib, and hypothyroidism can results in HF.
Iron studies
To screen for hereditary hemochromatosis as cause of heart failure.
ANA
To evaluate for possible lupus
Viral studies If viral mycocarditis suspected
BNP brain natriuretic pepetide

Chest X-ray in Heart Failure
Cardiomegaly
Cephalization of the pulmonary vessels
Kerley B-lines
Pleural effusions
Cardiac Testing in Heart Failure
Electrocardiogram:
May show specific cause of heart failure:
Ischemic heart disease
Dilated cardiomyopathy: first degree AV block, LBBB, Left anterior fascicular
block
Echocardiogram:
Left ventricular ejection fraction
Structural/valvular abnormalities
Further Cardiac Testing in Heart Failure
Exercise Testing
Should be part of initial evaluation of all patients with CHF.
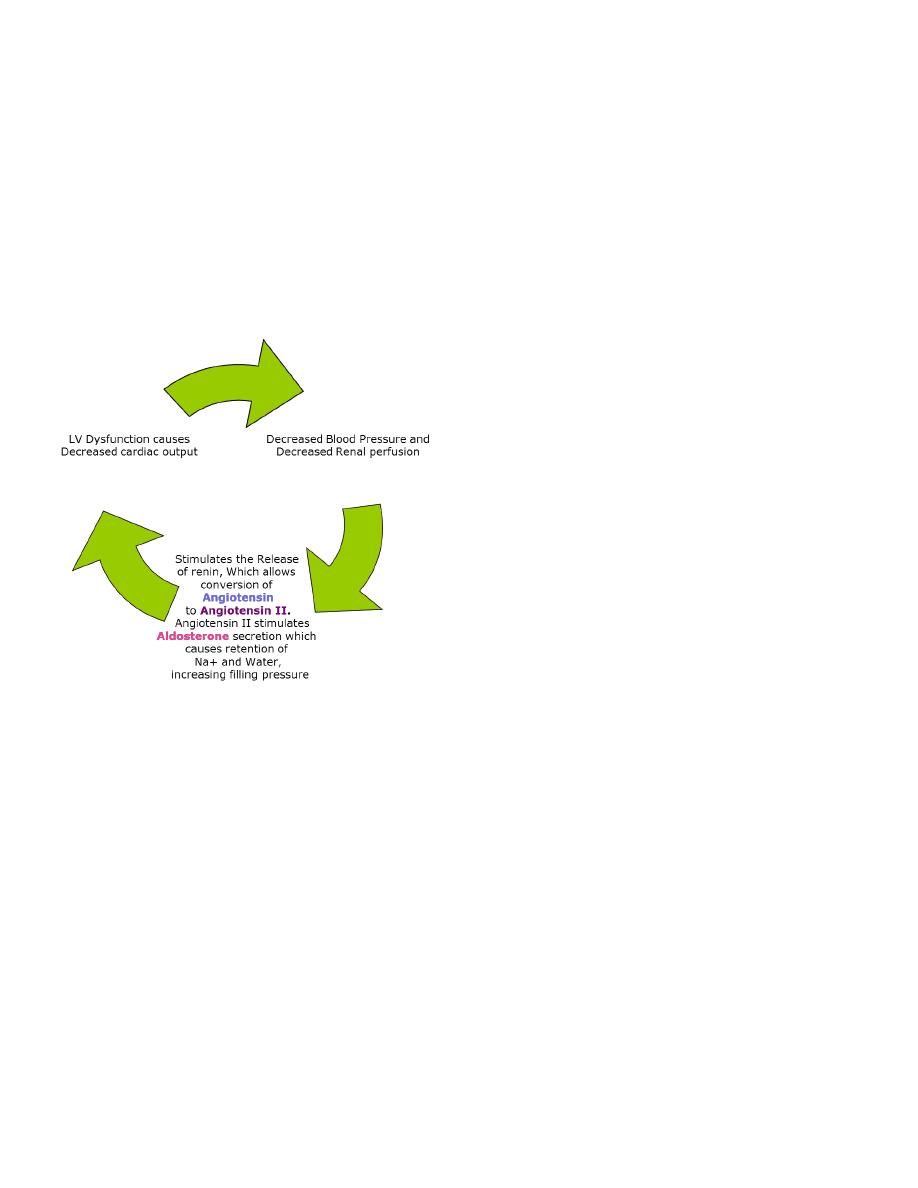
Coronary arteriography
Should be performed in patients presenting with heart failure who have angina or
significant ischemia.
Endomyocardial biopsy
Not frequently used Really only useful in cases such as viral-induced cardiomyopathy
Management of acute HF
acute medical emergency:
Sit the patient up to reduce pulmonary Congestion.
Give oxygen (high-flow, high-concentration).
IV diuretics (lasix)
Continuous monitoring of cardiac rhythm, BP .
Administer nitrates, such as IV glyceryl trinitrate until clinical improvement occurs or
systolic BP falls.
Intravenous opiates must be used sparingly in distressed patients.
If these measures prove ineffective, inotropic agents may be required to augment
cardiac output, particularly in hypotensive patients ( Dopamine).
Management of chronic heart failure
General measures
Drug therapy
Device therapy
Cardiac transplant

General measures
Education
Diet
•Good general nutrition and weight reduction for the obese
•Avoidance of high-salt foods and added salt.
Alcohol
Smoking cessation
Exercise
•Regular moderate aerobic exercise within limits of symptoms
Vaccination
•Consider influenza and pneumococcal vaccination
Treatment of the underlying cause of heart failure (CAD)
Drug therapy
1. ACE inhibitor (or ARB if not tolerated)
2. Beta blockers
3. Potassium sparing diuretics
4. Hydralazine, Nitrate
5. Loop diuretics
6. Digoxin
Diuretics
Loop diuretics
Furosemide, buteminide
diuretics produce an increase in urinary sodium and water excretion, leading to
reduction in blood and plasma volume
Potassium-sparing diuretics

Spironolactone, eplerenone
Help enhance diuresis
Maintain potassium
Shown to improve survival in CHF
ACE Inhibitor
Improve survival in patients with all severities of heart failure.
Begin therapy low and titrate up as possible:
Enalapril – 2.5 mg po BID
Captopril – 6.25 mg po TID
Lisinopril – 5 mg po Q Daily
If cannot tolerate, may try ARB
Beta Blocker therapy
Certain Beta blockers (carvedilol, metoprolol, bisoprolol) can increase ejection fraction,
improve symptoms, reduce the frequency of hospitalisation and reduce mortality.
Contraindicated:
Heart rate <60 bpm
Symptomatic bradycardia
Signs of peripheral hypoperfusion
COPD, asthma
PR interval > 0.24 sec, 2
nd
or 3
rd
degree block
Hydralazine plus Nitrates
Dosing:
Hydralazine
Started at 25 mg po TID, titrated up to 100 mg po TID

Isosorbide dinitrate
Started at 40 mg po TID/QID
Decreased mortality, lower rates of hospitalization, and improvement in quality of life.
Other medication in Heart Failure
Digoxin can be used to provide rate control in patients with heart failure and atrial
fibrillation. In patients with severe heart failure, digoxin reduces the likelihood of
hospitalisation for heart failure,
Statin therapy is recommended in CHF for the secondary prevention of cardiovascular
disease.
Some studies have shown a possible benefit specifically in HF with statin therapy
Meds to AVOID in heart failure
NSAIDS
Can cause worsening of preexisting HF
Thiazolidinediones
Include rosiglitazone (Avandia), and pioglitazone (Actos)
Cause fluid retention that can exacerbate HF
Metformin
People with HF who take it are at increased risk of potentially lethal lactic acidosis
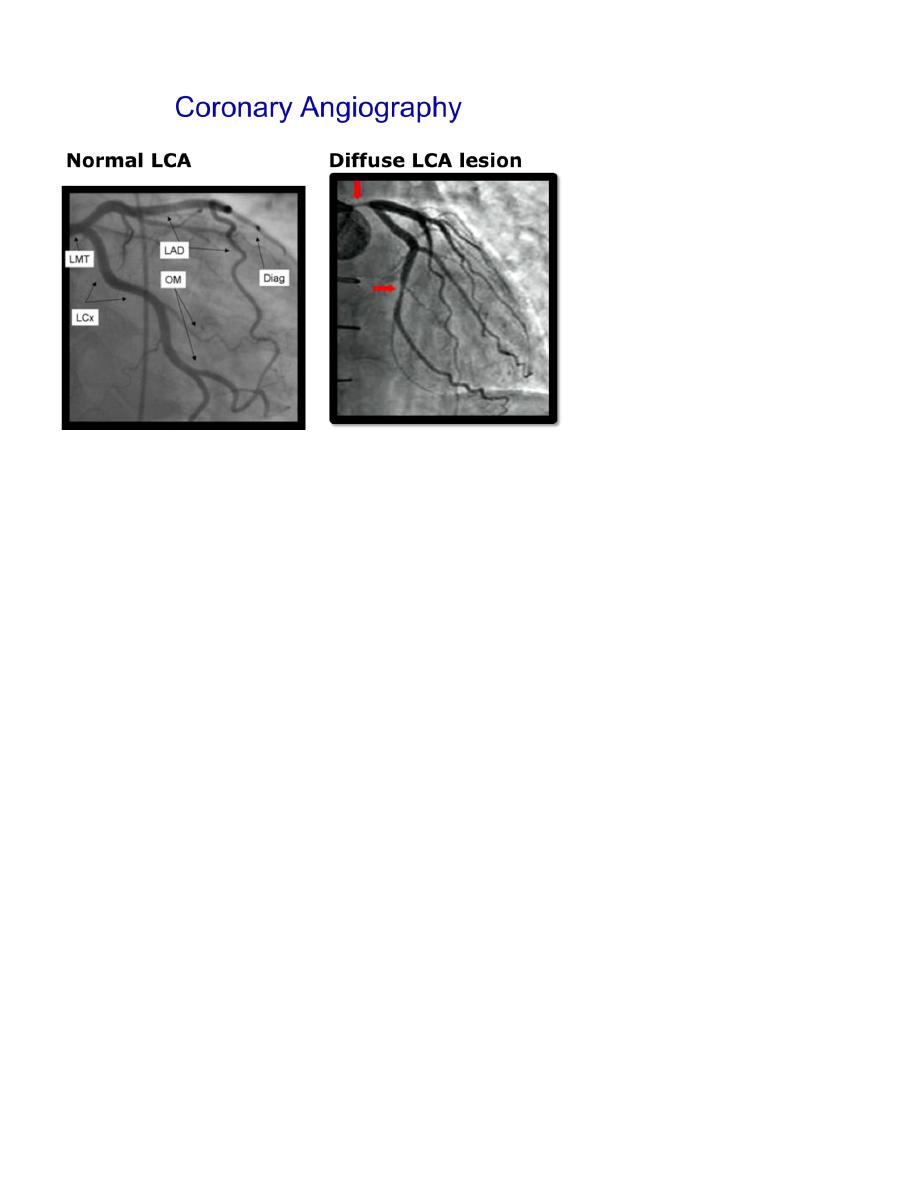
Implantable Cardioverter-Defibrillators for HF( ICD) -CRT
Sustained ventricular tachycardia is associated with sudden cardiac death in HF.
About one-third of mortality in HF is due to sudden cardiac death.
Patients with ischemic or nonischemic cardiomyopathy, NYHA class II to III HF, and LVEF
≤ 35% have a significant survival benefit from an implantable cardioverter-defibrillator
(ICD) for the primary prevention of SCD.
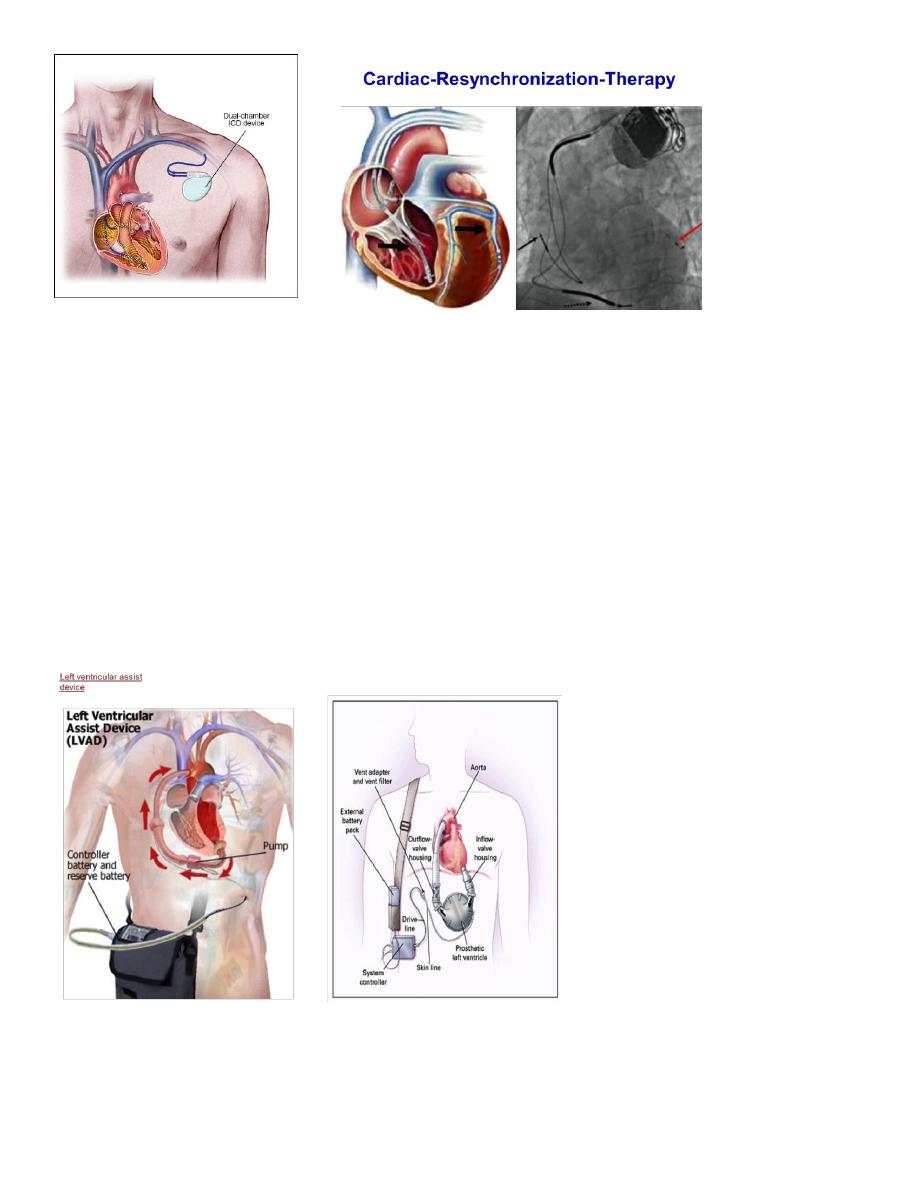
Management of Refractory Heart Failure
Inotropic drugs:
Dobutamine, dopamine, milrinone, nitroprusside, nitroglycerin
Mechanical circulatory support:
Intraaortic balloon pump
Left ventricular assist device (LVAD)
Cardiac Transplantation
