1
INFLAMMATORY BOWEL DISEASES
chronic inflammatory bowel diseases (Ulcerative colitis and Crohn's disease)
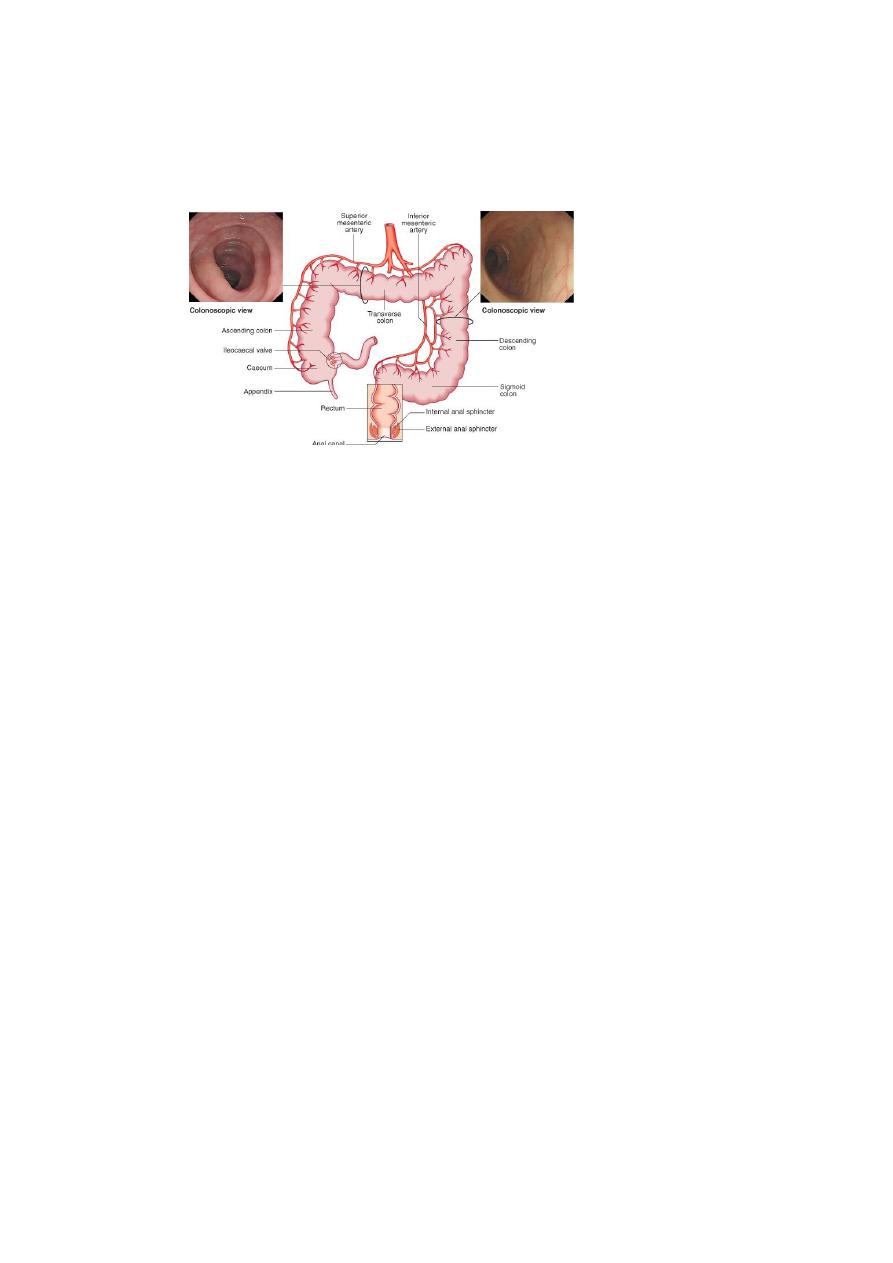
LARGE BOWEL
Characters:
(1) relapsing and remitting course.
(2) The diseases have many similarities and it is sometimes impossible to differentiate
between them.
(3) ulcerative colitis only involves the colon, while Crohn's disease can involve any part of
the gastrointestinal tract from mouth to anus .
Epidemiology
1. Crohn's disease appears to be very rare in the developing world but ulcerative colitis, is
becoming more common.
2. In the West, the prevalence of ulcerative colitis 100-200 per 100 000, while the prevalence
of Crohn's disease is 50-100 per 100 000.
3. Both diseases most commonly start in young adults (20-40) years, with a second incidence
peak in the seventh decade.
FACTORS ASSOCIATED WITH THE DEVELOPMENT OF IBD
1. Genetic factors
1. More common in Ashkenazi Jews
2. 10% have a first-degree relative or at least one close relative with IBD
3. High concordance between identical twins
4. Association with autoimmune thyroiditis and SLE
2
5. Gene mutations on chromosome 16 and some time on chromosomes 12, 6 and 14.
6. HLA-DR association in severe ulcerative colitis
and with HLA-B27 and ankylosing spondylitis in both (UC and CD) commonly develop
2. Environmental
3. Ulcerative colitis-more common in non-smokers and ex-smokers
4. Crohn's-most patients are smokers
5. Associated with low-residue, high refined sugar diet
6. Appendicectomy protects against ulcerative colitis
PATHOLOGY
1. In both diseases the intestinal wall is infiltrated with acute and chronic inflammatory cells.
2. There are important differences in the distribution of disease and in histological features
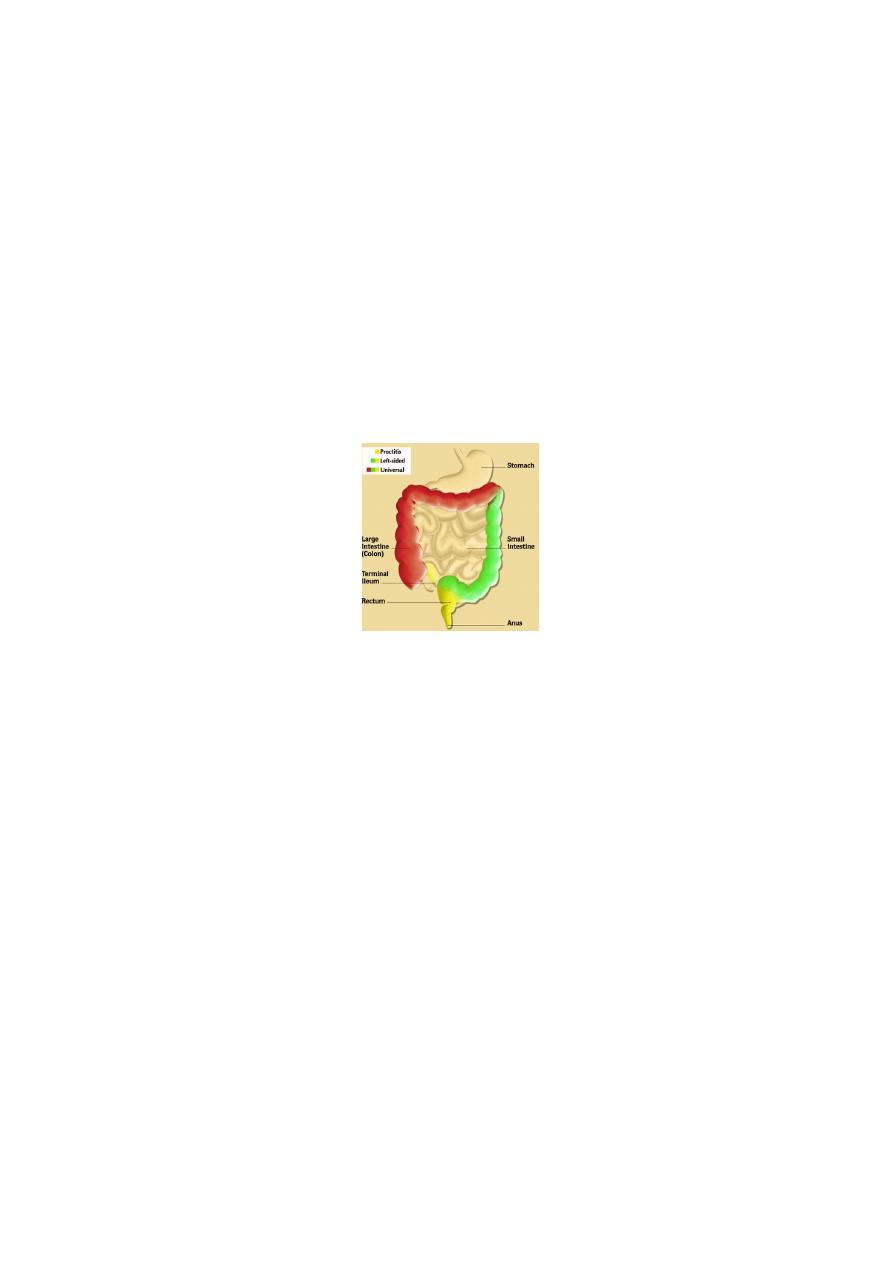
SITE OF INVOLVEMENT
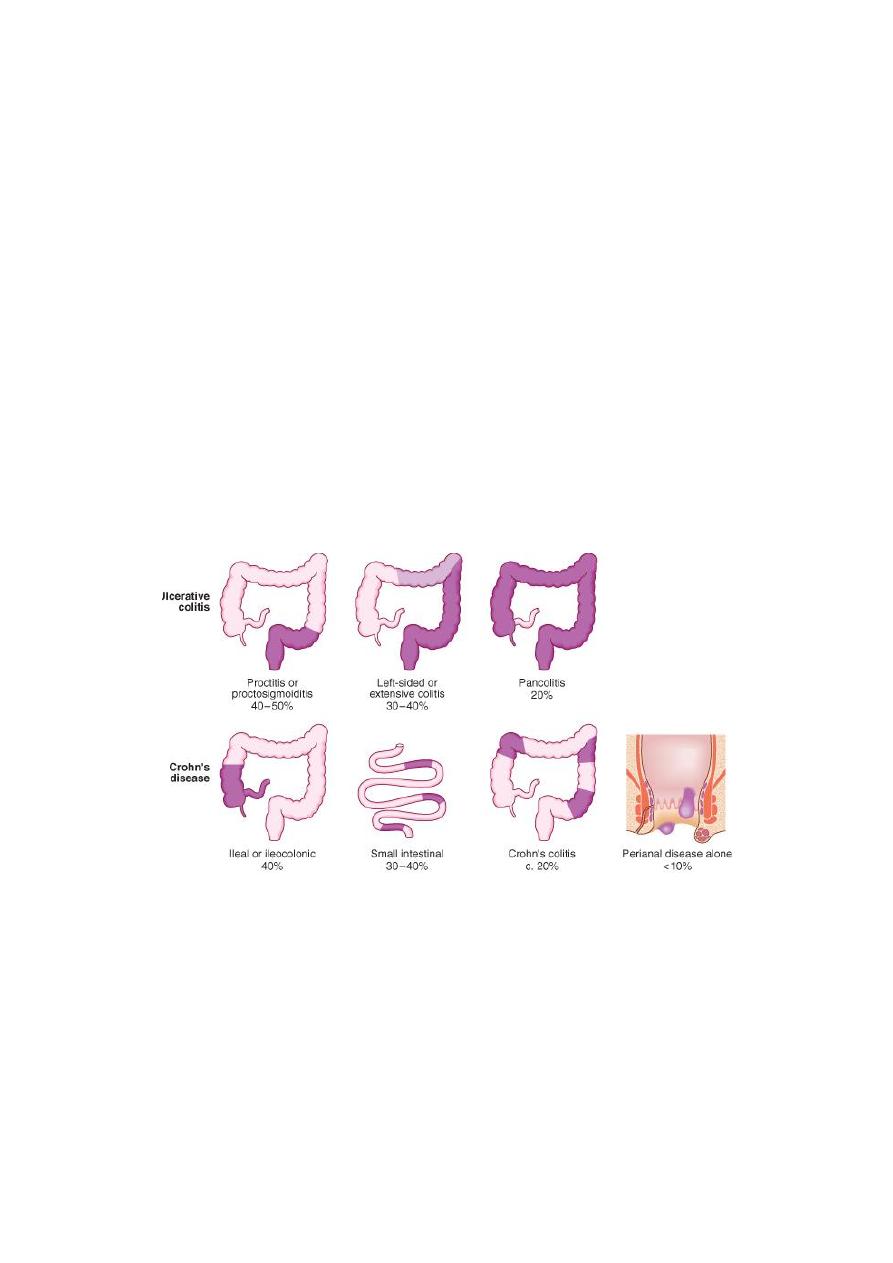
A. UC
1. Inflammation is almost always involves and start from the rectum (proctitis).
2. It may spread proximally to involve the sigmoid colon (proctosigmoiditis)
3, and in a minority the whole colon is involved (pancolitis).
4. Inflammation is confluent and is more severe distally.
5. In long-standing pancolitis the bowel becomes shortened and 'pseudopolyps' develop
which represent normal or hypertrophied residual mucosa within areas of atrophy
3
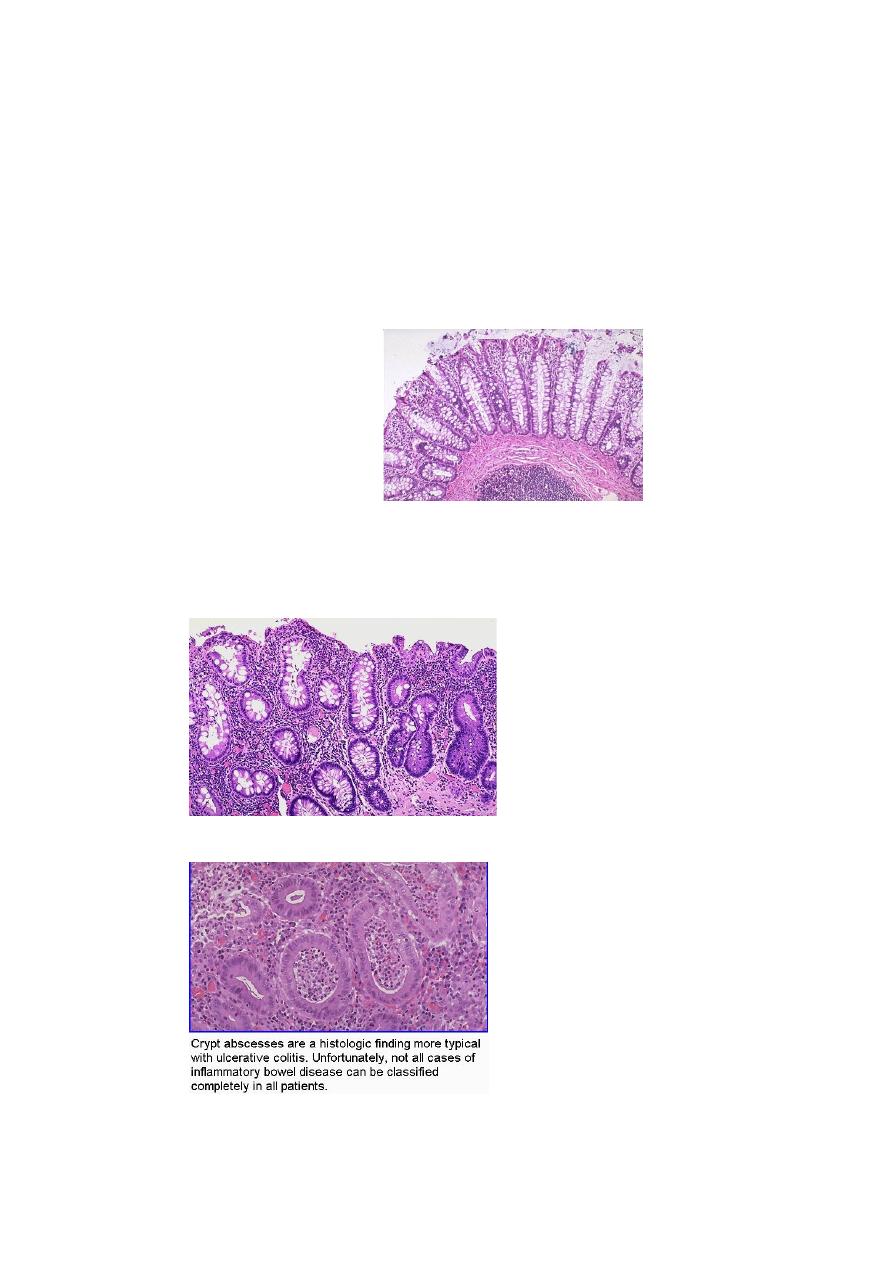
HISTOPATHOLOGY
(1) the inflammatory process is limited to the mucosa (not involve the deeper layers) of
the colon
(2) Both acute and chronic inflammatory cells infiltrate the lamina propria and the crypts
('cryptitis').
(3) Crypt abscesses are typical.
(4) Goblet cells lose their mucus and in long-standing cases glands become distorted.
(5) Dysplasia occurs and may lead to the development of colon cancer
NORMAL HISTOLOGY-COLON
UC PATHOLOGY
4
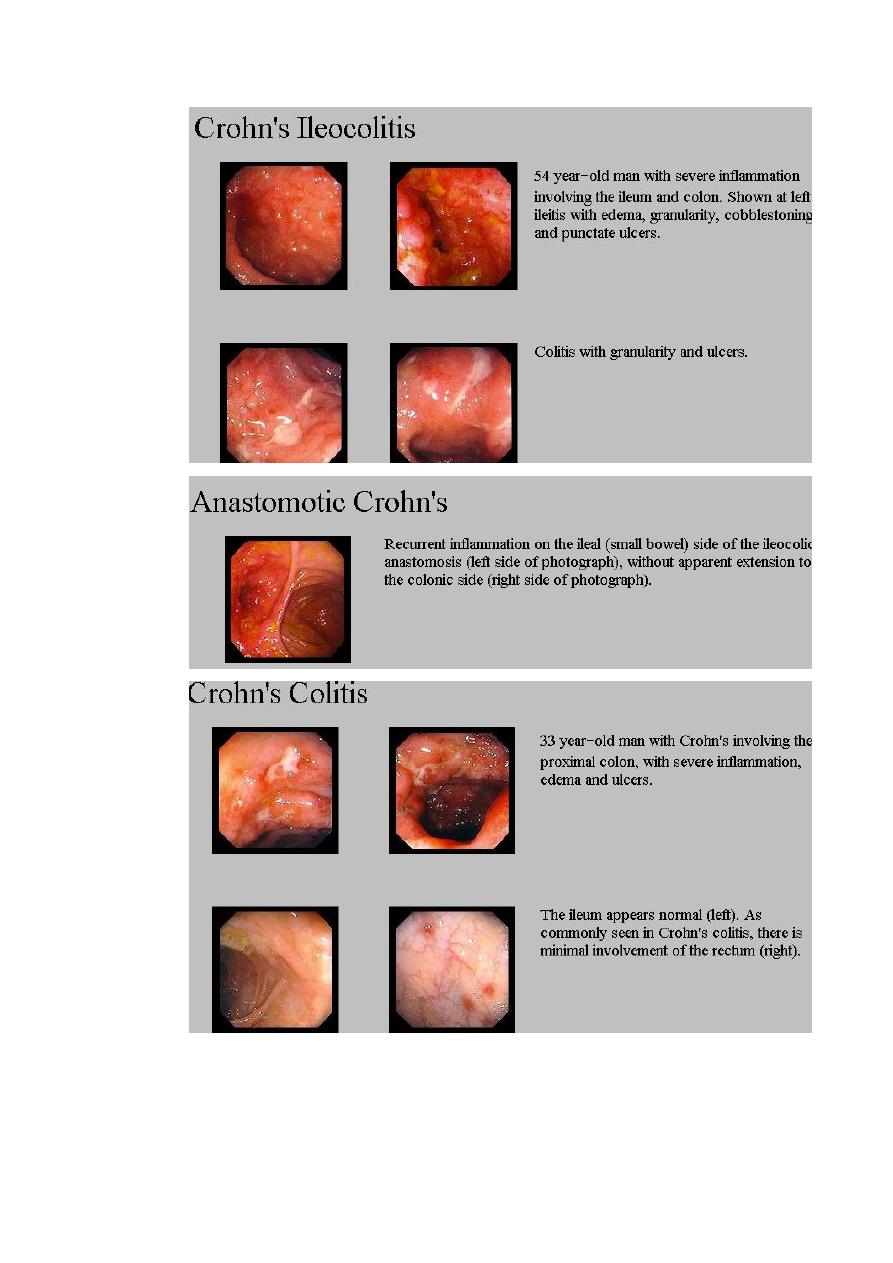
B. CD - PATHOLOGY
The sites most commonly involved, in order of frequency, are:
1. terminal ileum and right side of colon
2. colon alone
3. terminal ileum alone
4. ileum and jejunum
Fistulae may develop between adjacent loops of bowel or between affected segments of
bowel and the bladder, uterus or vagina, and may appear in the perineum.
a. The changes are patchy and interrupted by islands of normal mucosa ('skip' lesion).
b. The mesenteric lymph nodes are enlarged and the mesentery thickened .
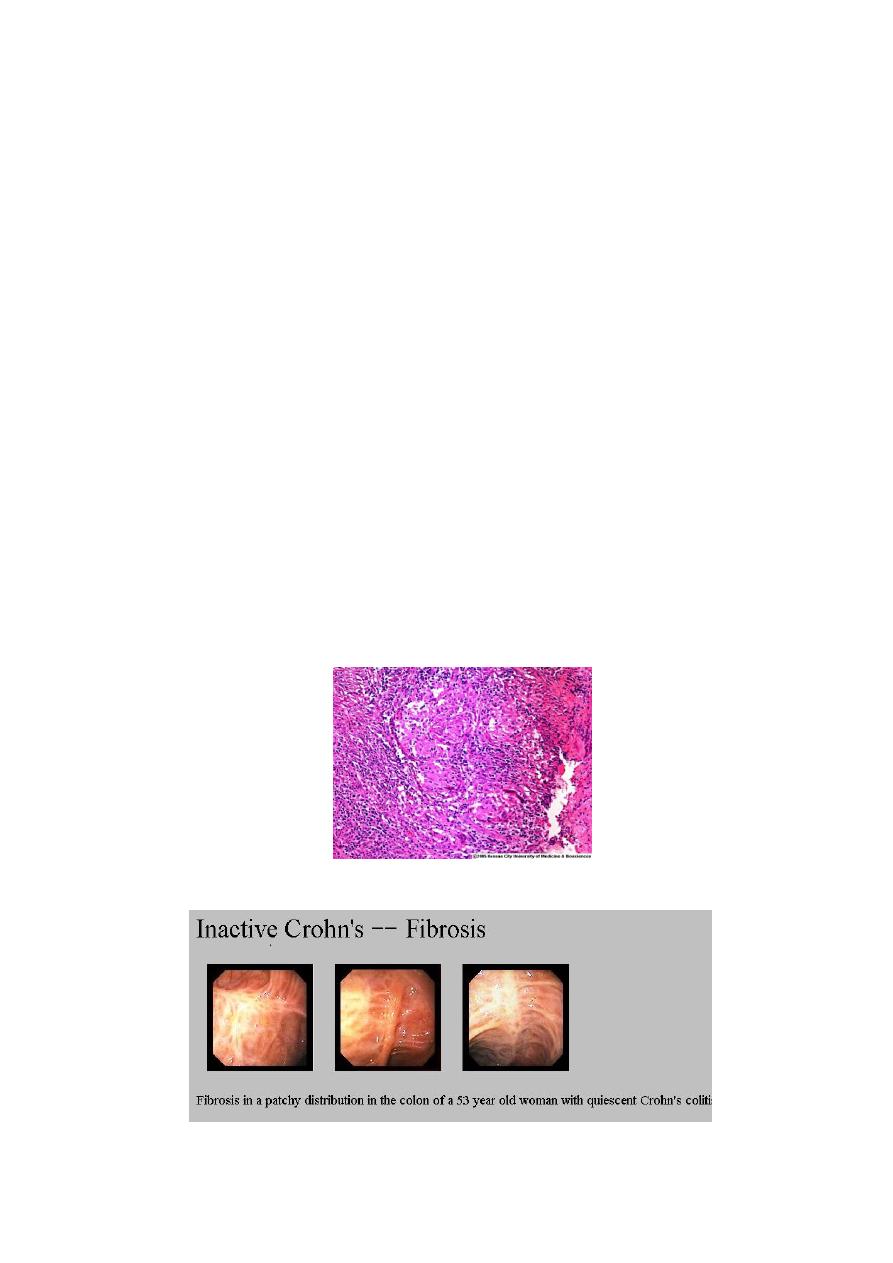
Histology:
1. chronic inflammation is seen through all the layers of the bowel wall, which is thickened as
a result.
2. focal aggregates of epithelioid histiocytes, which may be surrounded by lymphocytes and
contain giant cells.
3. Lymphoid aggregates or microgranulomas are also seen, and when these are near to the
surface of the mucosa they often ulcerate to form tiny aphthous-like ulcers.
CD GRANULOMA
5
CLINICAL FEATURES
A. UC
The major symptom is bloody diarrhoea
GENERAL FEATURES
1. The first attack is usually the most severe and thereafter the disease is followed by relapses
and remissions.
2. Only a minority of patients have chronic, unremitting symptoms.
3. Emotional stress, intercurrent infection, gastroenteritis, antibiotics or NSAID therapy may
provoke a relapse.
4. The clinical features depend upon the site and activity of the disease
INVOLVES LARGE BOWEL ONLY
CLINICAL FEATURES ACCORDING TO SITE INVOLVED
1. Rectal involvement (Proctitis) causes:
a) rectal bleeding
b) mucus discharge
c) tenesmus.
d) Some patients pass frequent, small-volume fluid stools.
e) others are constipated and pass pellety stools.
f) Constitutional symptoms do not occur
2. Rectum and sigmoid (Proctosigmoiditis) cause
a. Bloody diarrhoea with mucus.
b. Almost all patients are constitutionally well but a small minority who have very
active, limited disease develop fever, lethargy and abdominal discomfort
3. The whole colon Extensive colitis causes
a. bloody diarrhoea with passage of mucus. b. In severe cases anorexia, malaise, weight loss
and abdominal pain occur, and the patient is toxic with fever, tachycardia and signs of
peritoneal inflammation

6
B. CD
The major symptoms are abdominal pain, diarrhoea and weight loss
LARGE AND SMALL BOWEL
1. Ileal Crohn's disease (small bowel) causes
a. abdominal pain, principally because of subacute intestinal obstruction, but
inflammatory mass, intra-abdominal abscess or acute obstruction may be
responsible.
b. Pain is often associated with diarrhoea which is watery and does not contain
blood or mucus. 3. Weight lose almost always occur ( because eating provokes
pain and also may be due to malabsorption).
c. Some patients present with features of fat, protein or vitamin deficiencies e. g.
B
12
due to malabsorption. B
12
def. causes anaemia and neuropathy.
2. Crohn's colitis presents similar to ulcerative colitis.
a. Bloody diarrhoea.
b. Passage of mucus.
c. Constitutional symptoms including lethargy, malaise, anorexia and weight loss.
d. Rectal sparing and the presence of perianal disease are features which favour a
diagnosis of Crohn's disease rather than ulcerative colitis.
3. Many patients present with symptoms of both small bowel and colonic disease.
4. A few have isolated perianal disease, vomiting from jejunal strictures or severe oral
ulceration
5. Physical examination:
a. Evidence of weight loss.
b. Anaemia
c. Glossitis and angular stomatitis.
d. There is abdominal tenderness, most marked over the inflamed area.
e. An abdominal mass due to matted loops of thickened bowel or an intra-
abdominal abscess may occur.
f. Perianal skin tags, fissures or fistulae are found in at least 50% of patients

7
COMPLICATION OF IBD
INTESTINAL COMPLICATIONS
1. Toxic megacolon (mainly in ulcerative colitis).
2. Intestinal perforation (small and large-in both).
3. Haemorrhage (in both but rare).
4. Fistulae (in Crohn’s disease).
5. Colonic cancer (in ulcerative colitis and to lesser extend in Crohn’s colitis).
6. Small bowel adenocarcinoma (in Crohn’s disease).
1. TOXIC MEGACOLON:
• Is severe, life-threatening inflammation of the colon, occurs in both ulcerative colitis
and Crohn's disease.
• the colon dilates (toxic megacolon) and bacterial toxins pass freely across the diseased
mucosa into the portal then systemic circulation.
• This complication occurs most commonly during the first attack of colitis .
• An abdominal X-ray should be taken daily because when the transverse colon is
dilated to more than 6 cm there is a high risk of colonic perforation .
2. Perforation of the small intestine or colon: This can occur without the development of
toxic megacolon
3. Life-threatening acute haemorrhage due to erosion of a major artery is a rare
complication of both.
4. Fistulae : Fistulous connections between loops of affected bowel, or between bowel and
bladder or vagina are specific complications of Crohn's disease and do not occur in
ulcerative colitis.

8
5. increased risk of colon cancer in patients with extensive active colitis of more than 8 years'
duration especially in UC.
6. Small bowel adenocarcinoma is a rare complication of long-standing small bowel Crohn's
disease.
SYSTEMIC COMPLICATIONS OF IBD
1. Seronegative arthritis:
a. Acute medium size joint involvement.
b. Sacroiliatis.
c. Ankylosing spondylitis.
2. Dermatological:
a. erythema nodosum.
b. Pyoderma gangrenosum.
c. oral aphthous ulcers.
3. Ocular complications:
a. Conjunctivitis.
b. iritis.
c. episcleritis.
4. Hepatic and billiary:
a. Primary sclerosing choliangitis (UC).
b. Gall stone.
c. Autoimmune hepatitis.
d. fatty liver.
e. Portal pyaemia and liver abscess.
5. Renal complications:
a. Oxalate calculi (Crohn’s).
b. Amyloidosis.
c. Ureteric obstruction (Crohn’s).
6. Vascular:
a. DVT
b. Portal or mesenteric vein thrombosis.

9
FOLLOW UP
surveillance colonoscopy programmes
• Patients with long-standing (8-10 years)
extensive colitis (total) .
• Multiple random biopsies are taken every 10 cm throughout the colon and additional
biopsies are taken from raised or ulcerated areas.
• Mild dysplesia: Do colonoscopy every 1-2 years.
• If high dysplesia: Do proctocolonectomy.
MICROSCOPIC COLITIS
Some patients experience watery diarrhoea as a consequence of microscopic ('lymphocytic')
colitis. The colonoscopic appearances are normal but histological examination of biopsies
shows a range of abnormalities.
Collagenous colitis
Is a type of microscopic colitis, characterised by the presence of a thick submucosal band of
collagen; a chronic inflammatory infiltrate is usually seen. The disease is more common in
women and is associated with rheumatoid arthritis, diabetes and coeliac disease. Patients
have a history of intermittent watery diarrhoea and treatment is based on anti-diarrhoeal
drugs, bismuth, aminosalicylates and topical corticosteroid enemas.
COMPARISON BETWEEN UC AND CD
1. UC more in non-smoker or ex-smoker, while CD more common in smoker.
2. Sever UC is associated with HLA-DR103, while CD with chromosome 16 mutation
(CARD15/NOD2).
3. Involve colon , start from rectum and extend proximally, the lesions are confluent. CD
involve any part of GIT from mouth to anus, perianal lesions and lesion are patchy
with skip-lesion.
4. Extra-intestinal involvement is common in both.
5. In UC: Main presentation is bloody diarrhea, while in CD: Abdominal pain, diarrhea
and weight loss.
6. In UC the lesions are limited to mucosa with cryptitis and crypt abscess, but in CD
submucosa, transmural, deep fissuring ulcers, fistula, patchy changes and granuloma.
7. R of UC: 5ASA, steroid, azathioprine, colectomy is curable. In CD: steroid,
azathioprine, methotrexate, infliximab, nutritional R, surgery for complications is not
curable.

10
Differential diagnosis of IBD
CONDITIONS WHICH CAN MIMIC ULCERATIVE OR CROHN'S COLITIS
Infective (with first attack of IBD colitis)
1. Bacterial
• Salmonella
• Shigella
• Campylobacter jejuni
• E. coli O:157
• Gonococcal proctitis
• Pseudomembranous colitis (Antibiotics)
• Chlamydia proctitis
2. Viral
• Herpes simplex proctitis
• Cytomegalovirus
3. Protozoal
• Amoebiasis
Non-infective
Vascular
Ischaemic colitis
Radiation proctitis
Idiopathic
Collagenous colitis
Behçet's disease
Drugs
NSAIDs
Neoplastic
Colonic carcinoma
Other
Diverticulitis

11
The major diagnostic difficulty is to distinguish the first attack of acute colitis from infection.
In general, diarrhoea lasting longer than 10 days is unlikely to be the result of infection.
Stool microscopy, culture and examination for Clostridium difficile toxin or for ova and cysts,
sigmoidoscopy and rectal biopsy.
blood cultures and serological tests for infection are useful
DIFFERENTIAL DIAGNOSIS OF SMALL BOWEL CROHN'S DISEASE
• Other causes of right iliac fossa mass
– Caecal carcinoma
– Appendix abscess
– Infection (TB, Yersinia, actinomycosis)
• Mesenteric adenitis
• Pelvic inflammatory disease
• Lymphoma
Investigations of IBD
• Blood examination
1. Full blood count may show anaemia resulting from bleeding or malabsorption of iron,
folic acid or vitamin B12.
2. Serum albumin concentration falls as a consequence of protein-losing enteropathy,
or because of poor nutrition.
3. The ESR is raised in exacerbations or because of abscess. Elevation of CRP
concentration is helpful in monitoring Crohn's disease activity
• Bacteriology Stool cultures are performed to exclude superimposed enteric infection in
patients who present with exacerbations of IBD. Blood cultures are also advisable in
patients with known colitis or Crohn's disease who develop fever.
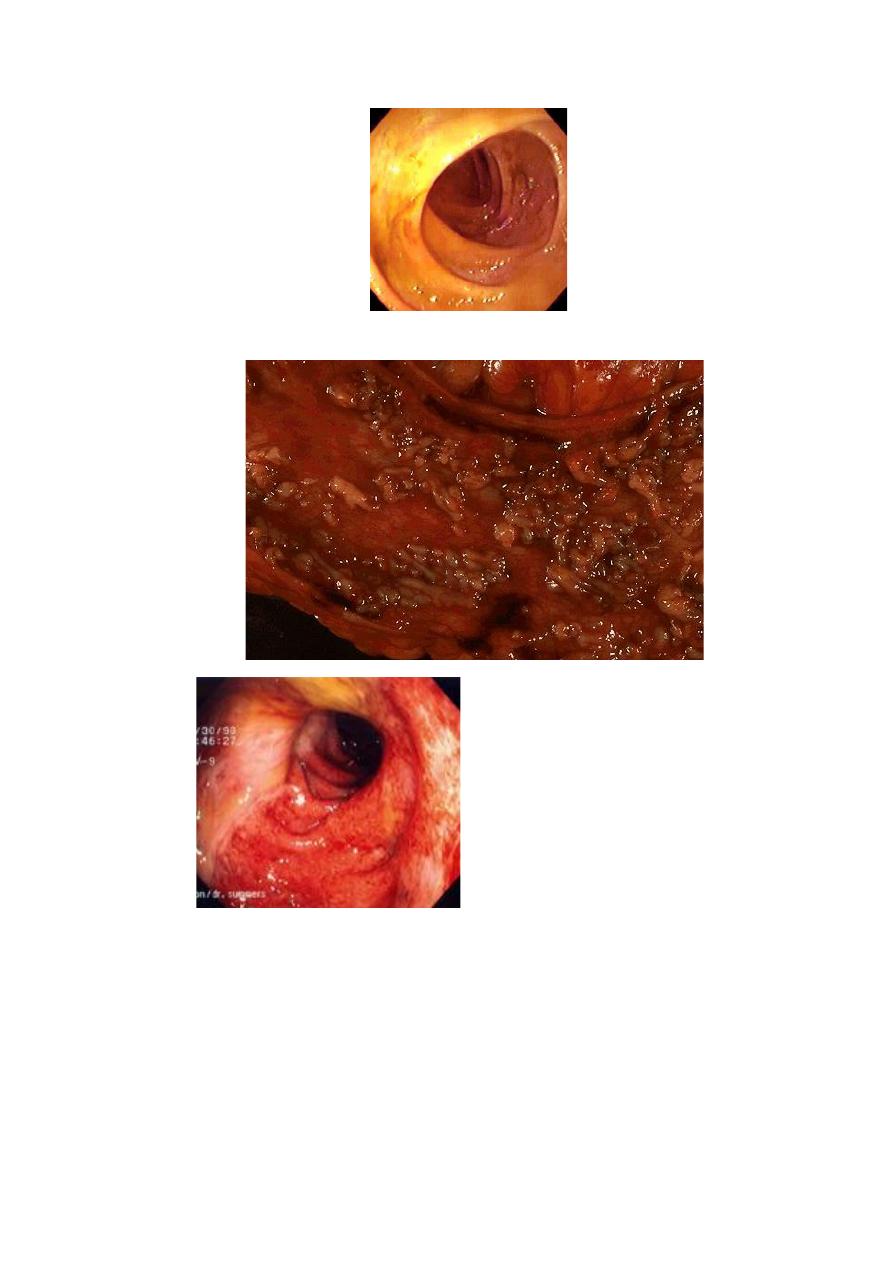
• Sigmoidoscopy and/or colonoscopy:
A. Ulcerative colitis
• loss of vascular pattern.
• granularity.
• friability
• and ulceration.
12
• Also pseudopolyps,
• And carcinoma.
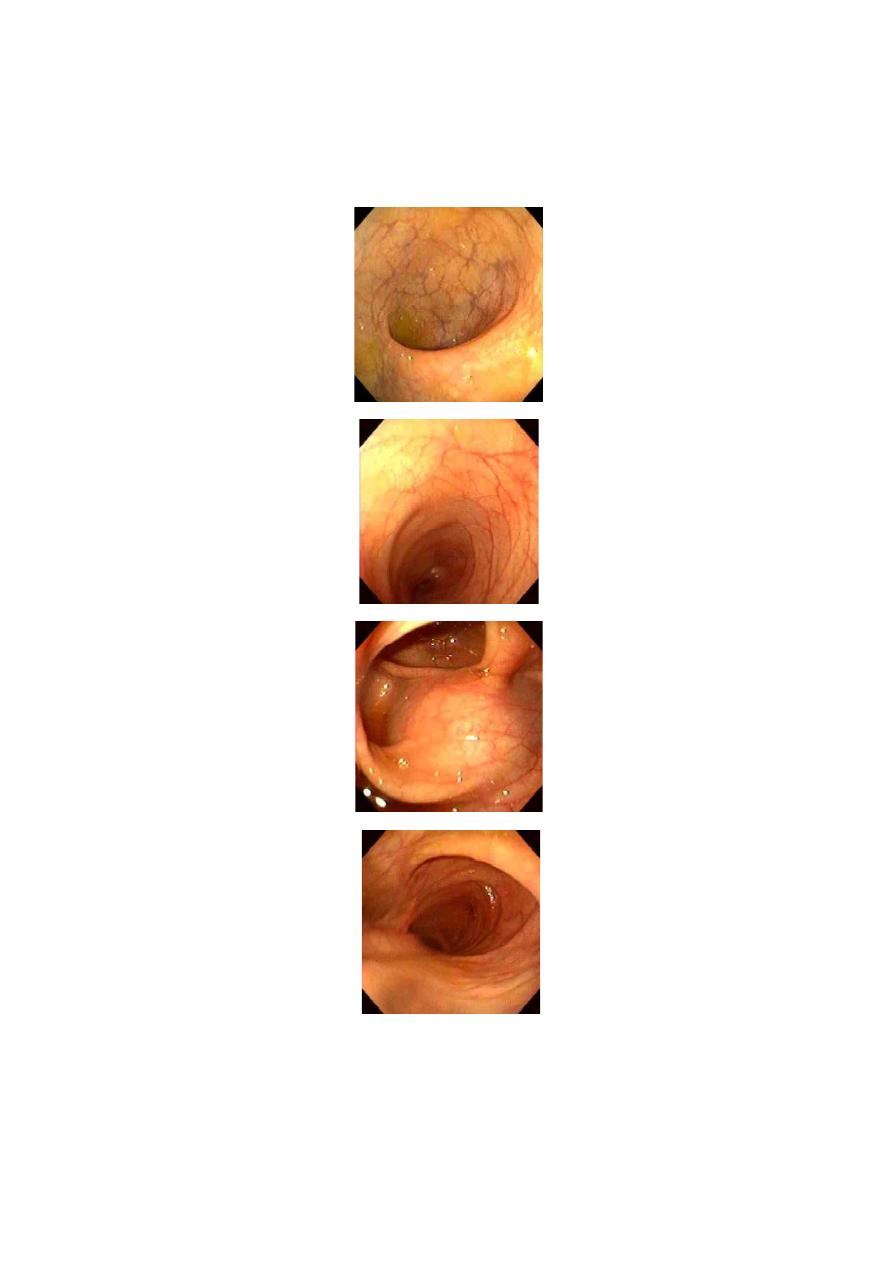
NORMAL RECTUM
NORMAL SIGMOID COLON
NORMAL SPLENIC FLEXURE
NORMAL TRANVERSE COLON
13
NORMAL ASCENDING COLON
UC GROSS
UC
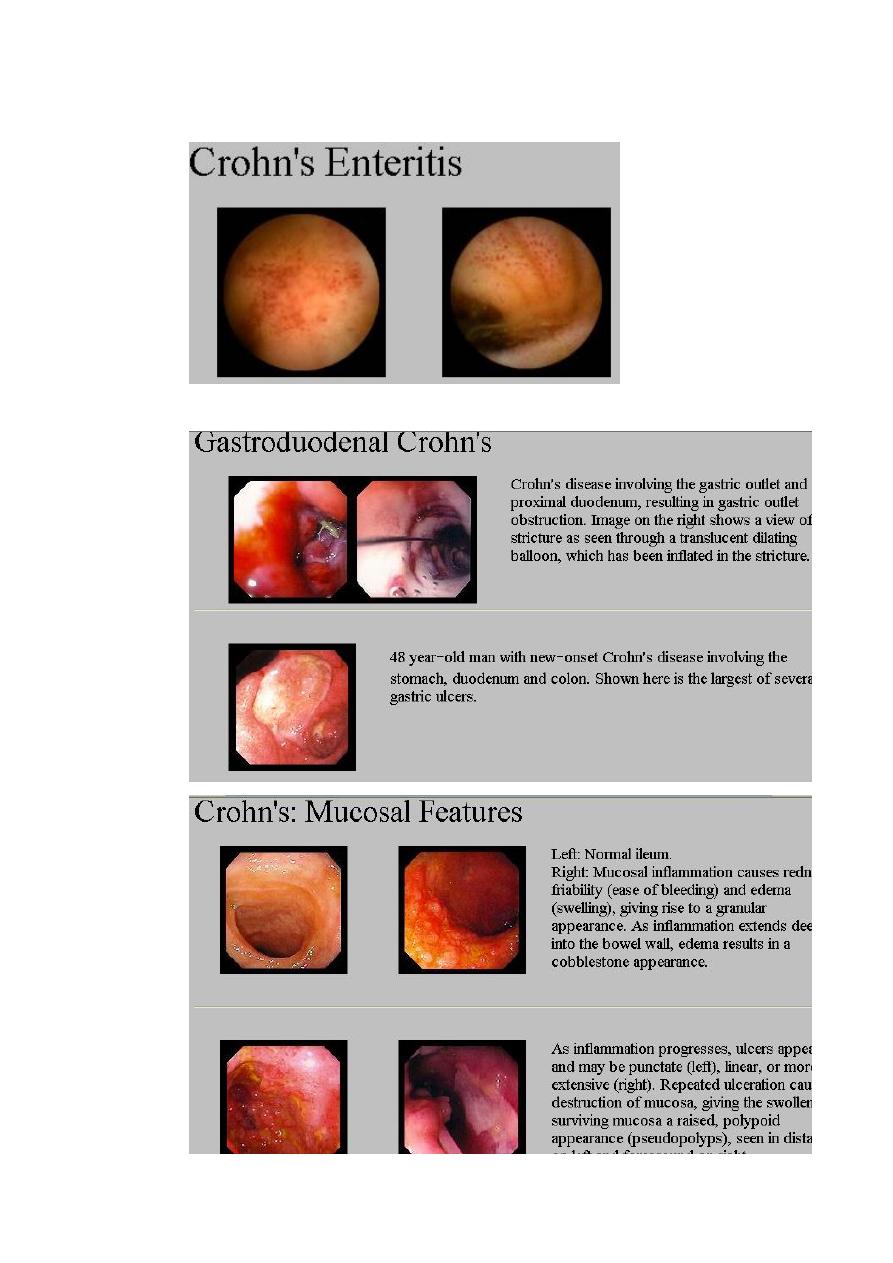
B. In Crohn's disease
• patchy inflammation with discrete, deep ulcers or aphthus like ulcers.
• perianal disease (fissures, fistulae and skin tags)
• or rectal sparing may occur.
14
15
• CAPSULE ENDOSCOPY
16
• Barium studies
Barium enema is a less sensitive investigation than colonoscopy. In long-standing ulcerative
colitis the colon is shortened and loses haustra to become tubular, and pseudopolyps are
seen. In Crohn's colitis a range of abnormalities occur. The appearances may be identical to
those of ulcerative colitis but skip lesions, strictures and deeper ulcers are characteristic .
Reflux into the terminal ileum may show stricture and ulcers. Contrast studies of the small
bowel are normal in ulcerative colitis, but in Crohn's disease affected areas are narrowed and
ulcerated; multiple strictures are common .
• Plain abdominal X-ray
is essential in the management of patients who present with severe active disease. Dilatation
of the colon , mucosal oedema ('thumb-printing') or evidence of perforation may be found. In
small bowel Crohn's disease there may be evidence of intestinal obstruction or displacement
of bowel loops by a mass.
• Ultrasound
may identify thickened small bowel loops and abscess development in Crohn's disease.
Diagnosis of Small bowel Crohn's disease
1. white cell scanning may help identify inflamed intestinal segments.
2. In atypical cases biopsy or surgical resection is necessary to exclude other diseases . This
can often be done endoscopically by ileal intubation at colonoscopy, but sometimes
laparotomy or laparoscopy with resection or full-thickness biopsy is necessary.
Aim of treatment
1. To treat acute attacks
2. To prevent relapses
3. To detect carcinoma at an early stage
4. To select patients for surgery.
17
18
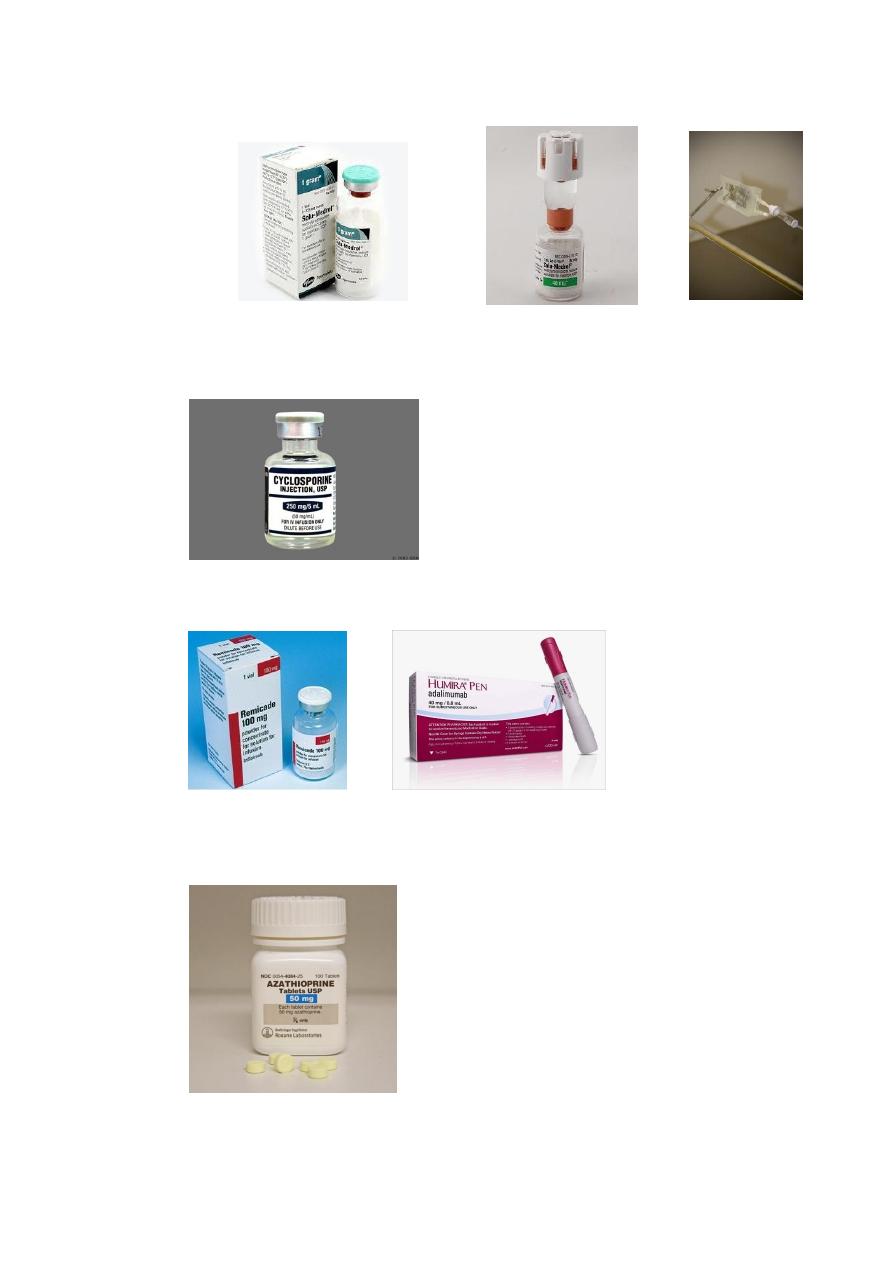
Methylprednisolone IV Drip (SEVERE IBD)
Cyclosporine IV drip
(SEVERE UC)
Biological Agents
Infliximab 5mg/kg, IV drip (0, 2W, 6Ws. Adalimumab (subcutaneous)
Thiopurines
Maintenance therapy / steroid sparing

19
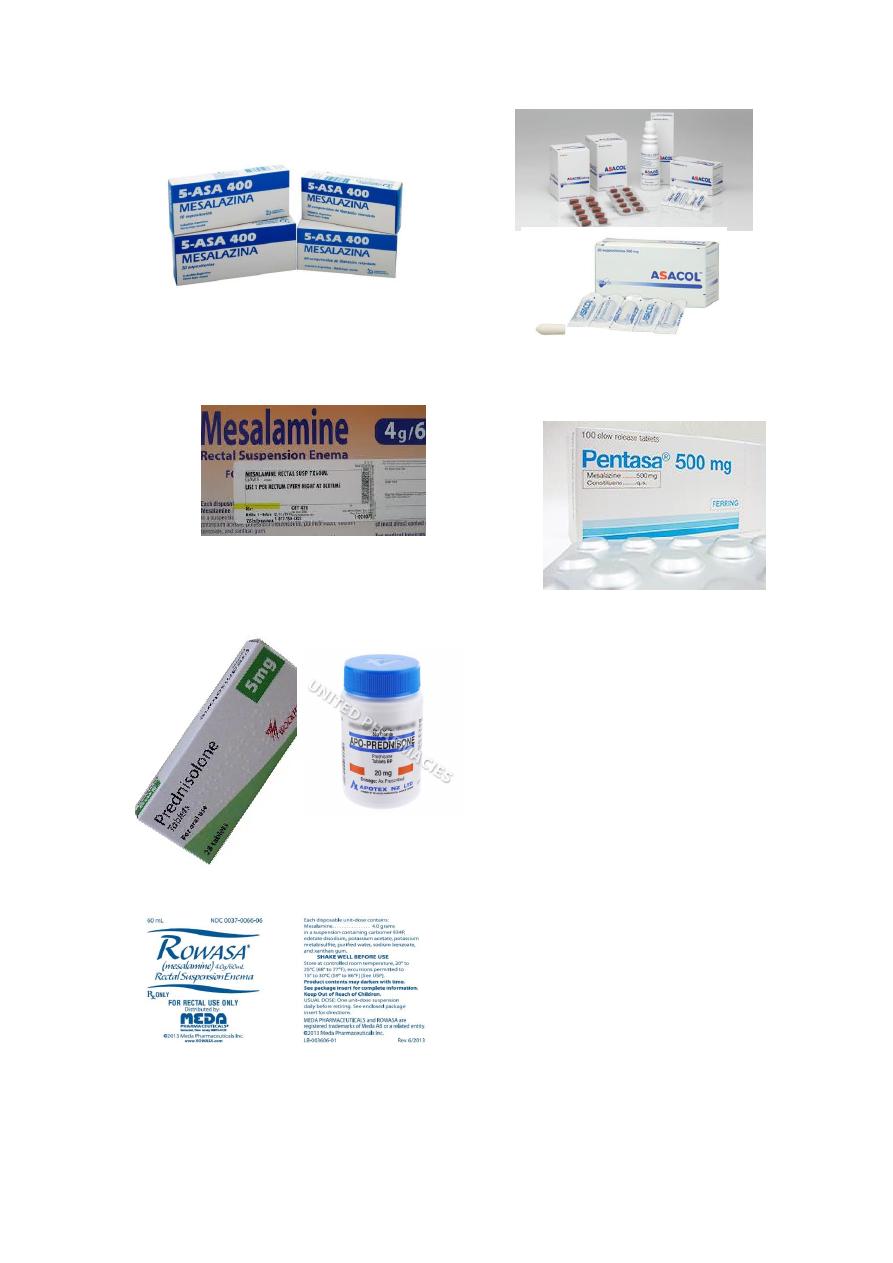
Medical management of ulcerative colitis
Treatment depends upon the extent and activity of colitis.
Active proctitis
1) In mild to moderate disease Mesalazine (5ASA) enemas or suppositories combined with
oral mesalazine are effective first-line therapy.
2) Topical corticosteroids are less effective and are reserved for patients who are intolerant
of topical mesalazine.
3) Patients who fail to respond are treated with oral prednisolone 40 mg daily.
Active left-sided or extensive ulcerative colitis
In mildly active cases, high-dose aminosalicylates( Mesalazine) combined with topical
aminosalicylate and corticosteroids are effective.
Oral Prednisolone 40 mg daily is indicated for more active disease or when initial
aminosalicylate therapy is ineffective.
Severe ulcerative colitis
1. Admit to hospital.
2. Systemic high doses of steroid (iv methyl prednisolone or hydrocortisone).
3. Supportive treatment like iv fluid, blood transfusion and nutritional support.
4. Antibiotic therapy if infection is evidence of infection.
5. Lab tests (Hb, ESR, Electrolytes, S. Urea….)
6. Plain X-ray of abdomen to exclude toxic megacolon.
7. DVT prophylaxis by Heparin.
8. Avoid opiates and anti-diarrheal agents.
9. Iv ciclosporin (cyclosporine) (2mg/kg) or infliximab (5mg/kg) in patients not
responding to 3-5 days of steroid therapy.
10. If Patient not responding to above treatment or develop toxic megacolon consider
surgery (total colectomy).
INDICATIONS FOR SURGERY IN ULCERATIVE COLITIS
1. Impaired quality of life
2. Failure of medical therapy
3. Fulminant colitis
4. Disease complications unresponsive to medical therapy
5. Colon cancer or severe dysplasia

20
R OF ACTIVE CROHN’S DISEASE
Patients with active colitis or ileocolitis are initially treated in a similar manner to those with
active ulcerative colitis. Aminosalicylates and corticosteroids are both effective and usually
effect remission in active ileocolitis and colitis. In severe disease intravenous prednisolone is
indicated, but abscess or fistulating disease should be excluded before instituting therapy with
corticosteroids.
R OF ILEAL DISEASE IN CD
1. Steroid: Budesonide is appropriate for treating moderately active disease, although it is
marginally less effective thanprednisolone. Aminosalicylates have little added value
2. there is some evidence to support the use of oral metronodazole.
3. Poorly responding patients should, at an early stage, be considered for surgical resection
since this is associated with prolonged remission in most cases.
4. Infliximab (anti-TNF monoclonal antibody ) given as an intravenous infusion 4-8-weekly
on three occasions induces remission in patients with active Crohn's disease at any site
within the gastrointestinal tract and is also effective for the management of some
extraintestinal complications including pyoderma gangrenosum and some forms of
arthritis. combined with disease-modifying agents, either thiopurines or methotrexate, to
maintain remission.
5. nutritional support which in the most severe cases involves prolonged parenteral nutrition
Maintenance of remission
The most effective step, and one greater than any pharmacological intervention, is smoking
cessation. Unlike UC Aaminosalicylates have minimal efficacy. Patients who relapse more than
once a year are treated with thiopurines . Those patients who are intolerant of, or resistant to
azathioprine or 6-mercaptopurine are treated with once-weekly methotrexate combined with
folic acid. Patients with aggressive disease are managed using a combination of
immunomodulating agents and infliximab . Chronic use of corticosteroids is avoided since this
leads to osteopenia and other side-effects, without preventing relapse.
