
Multiple sclerosis
# Multiple sclerosis (MS) is a chronic disease characterized by inflammation,
demyelination, gliosis (scarring), and neuronal loss.
Lesions of MS typically occur at different times and in different CNS locations.
#
# 5 million individuals worldwide.
# Manifestations of MS vary from a benign illness to a rapidly evolving and
incapacitating disease requiring profound lifestyle adjustments.
Epidemiology and causes:
# MS is approximately threefold more common in women than men.
# The age of onset is typically between 20 and 40 years
# Geographicly the highest known prevalence for MS (250 per 100,000)
in north of Scotland. In other temperate zone areas (e.g., northern
North America, northern Europe, southern Australia, and south New
Zealand),
# the prevalence of MS is 0.1–0.2%.
# one proposed explanation for the latitude effect on MS is that there is
a protective effect of sun exposure.
# studies have confirmed that vitamin D deficiency is associated with
an increase in MS risk and preliminary data also suggest that ongoing
deficiency may increase the relapse rate in established MS.
# The cause of MS is unknown; however, it is believed to occur as a
result of some combination of genetic and environmental factors such
as infectious agents any
have been proposed as triggers of
MS, but none have been confirmed.
# Moving at an early age from one location in the world to another
alters a person's subsequent risk of MS.
Smoking has been shown to be an independent risk factor for MS.
# Stress may be a risk factor although the evidence to support this is
weak.
Multiple sclerosis types:
# Relapsing remitting MS
# Primary progressive MS
# 2nd progressive MS
Progressive relapsing MS
#
# Relapsing remitting MS:
It occurs more than 85% of the cases
-
- characterized by discrete attacks that generally evolve over days to
weeks (rarely over hours).
There is often complete recovery over the ensuing weeks to months
-
approximately half will fail to improve.
Between attacks, patients are neurologically stable.
-
# Primary progressive MS:
- accounts for ∼ 15% of cases. These patients do not experience attacks
but only a steady functional decline from disease onset.
-Compared to RRMS, the sex distribution is more even, the disease
begins later in life (mean age ∼ 40 years), and disability develops faster .
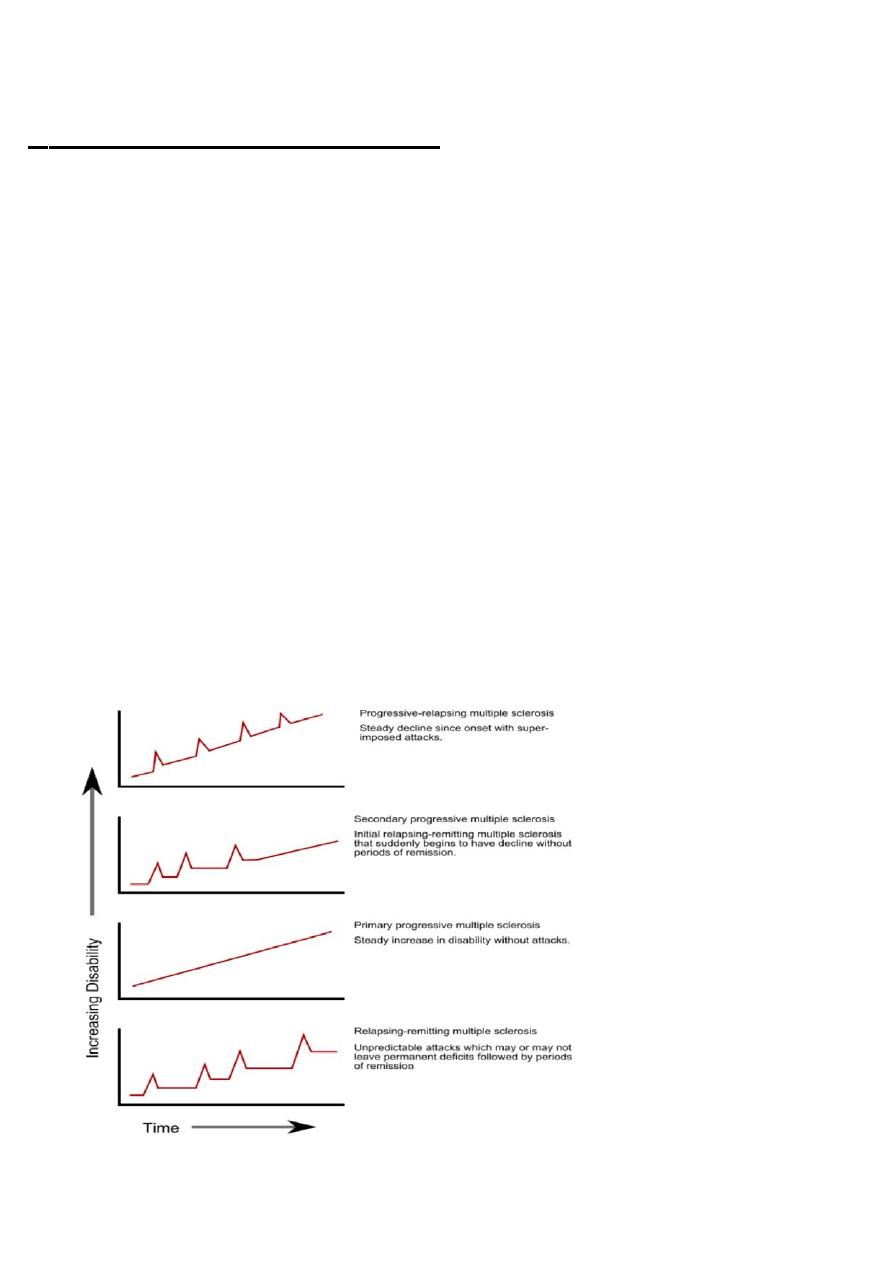
Secondary progressive Ms:
#
-(SPMS) always begins as RRMS At some point, however, the clinical
course changes so that the patient experiences a steady deterioration in
function unassociated with acute attacks (which may continue or cease
during the progressive phase).
-Progressive/relapsing MS (PRMS) overlaps PPMS and SPMS and
accounts for ∼ 5% of MS patients.
-Like patients with PPMS, these patients experience a steady
deterioration in their condition from disease onset. However, like SPMS
patients, they experience occasional attacks superimposed upon their
progressive course.
#CLINICAL MANIFESTATIONS:
Sensory symptoms
-
-Motor symptoms
Visual symptoms
-
-Sphincter disturbance
Cognitive impairment
-
Ataxia and vertigo
-
Double vision
-
Motor symptoms:
The onset of MS may be abrupt or insidious
-
Weakness of the limbs may manifest as loss of strength,heaviness
Exercise-induced weakness is a characteristic symptom of MS
The weakness is of the upper motor neuron type
-More than 30% of MS patients have moderate to severe spasticity,
especially in the legs
Sensory symptoms:
#
-Sensory symptoms are varied and include both paresthesias (e.g.,
tingling, prickling sensations, formications, “pins and needles,” or painful
burning) and hypesthesia (e.g., reduced sensation, numbness, or a “dead”
feeling). Unpleasant sensations (e.g., feelings that body parts are swollen,
wet, raw, or tightly wrapped) are also common
-Sensory impairment of the trunk and legs below a horizontal line on the
torso (a sensory level) indicates that the spinal cord is the origin of the
sensory disturbance
-Pain is a common symptom of MS, experienced by >50% of patients. Pain
can occur anywhere on the body and can change locations over time
#Visual symptoms
-System Optic neuritis (ON) presents as diminished visual acuity,
dimness, or decreased color perception
-Visual symptoms are generally monocular but may be bilateral.
Periorbital pain (aggravated by eye movement) often precedes or
accompanies the visual loss
- Pallor of the optic disc (optic atrophy) commonly follows ON
-Diplopia may result from internuclear ophthalmoplegia (INO) or from
palsy of the sixth cranial nerve (rarely the third or fourth).

-Ataxia usually manifests as cerebellar tremors (Chap. 31). Ataxia may
also involve the head and trunk or the voice, producing a characteristic
cerebellar dysarthria (scanning speech).
-Bladder dysfunction is present in >90% of MS patients, and in a third of
patients, dysfunction results in weekly or more frequent episodes of
incontinence
-Cognitive dysfunction can include memory loss, impaired attention,
difficulties in executive functioning, memory, problem solving, slowed
information processing, and problems shifting between cognitive tasks
-Depression , experienced by approximately half of patients
-Fatigue is experienced by 90% of patients; this symptom is the most
common reason for work-related disability in MS.
#Diagnosis
-There is no definitive diagnostic test for MS.
-Diagnostic criteria for clinically definite MS require documentation of
two or more episodes of symptoms and two or more signs that reflect
pathology in anatomically noncontiguous white matter tracts of the CNS
-Symptoms must last for >24 h and occur as distinct episodes that are
separated by a month or more.

DIAGNOSTIC TESTS
#
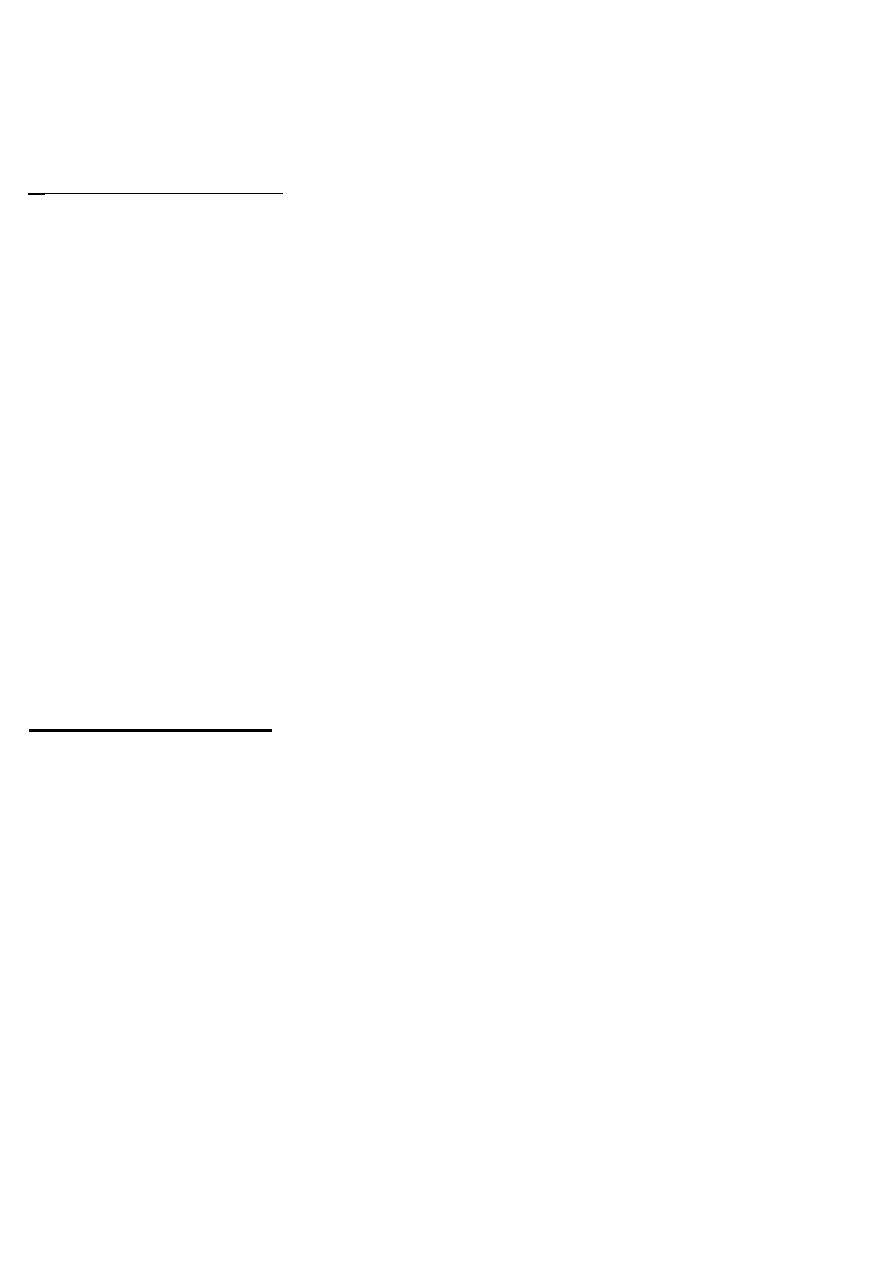
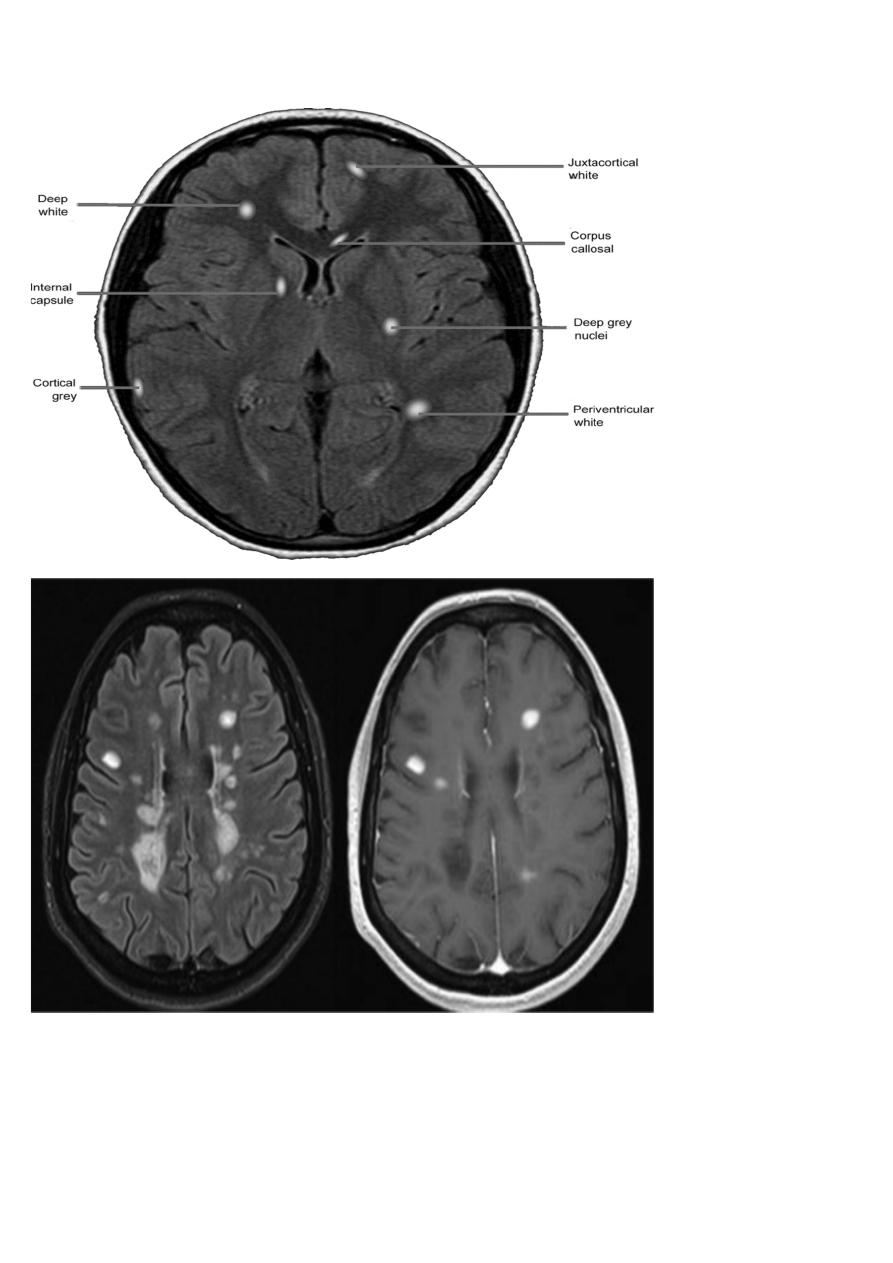
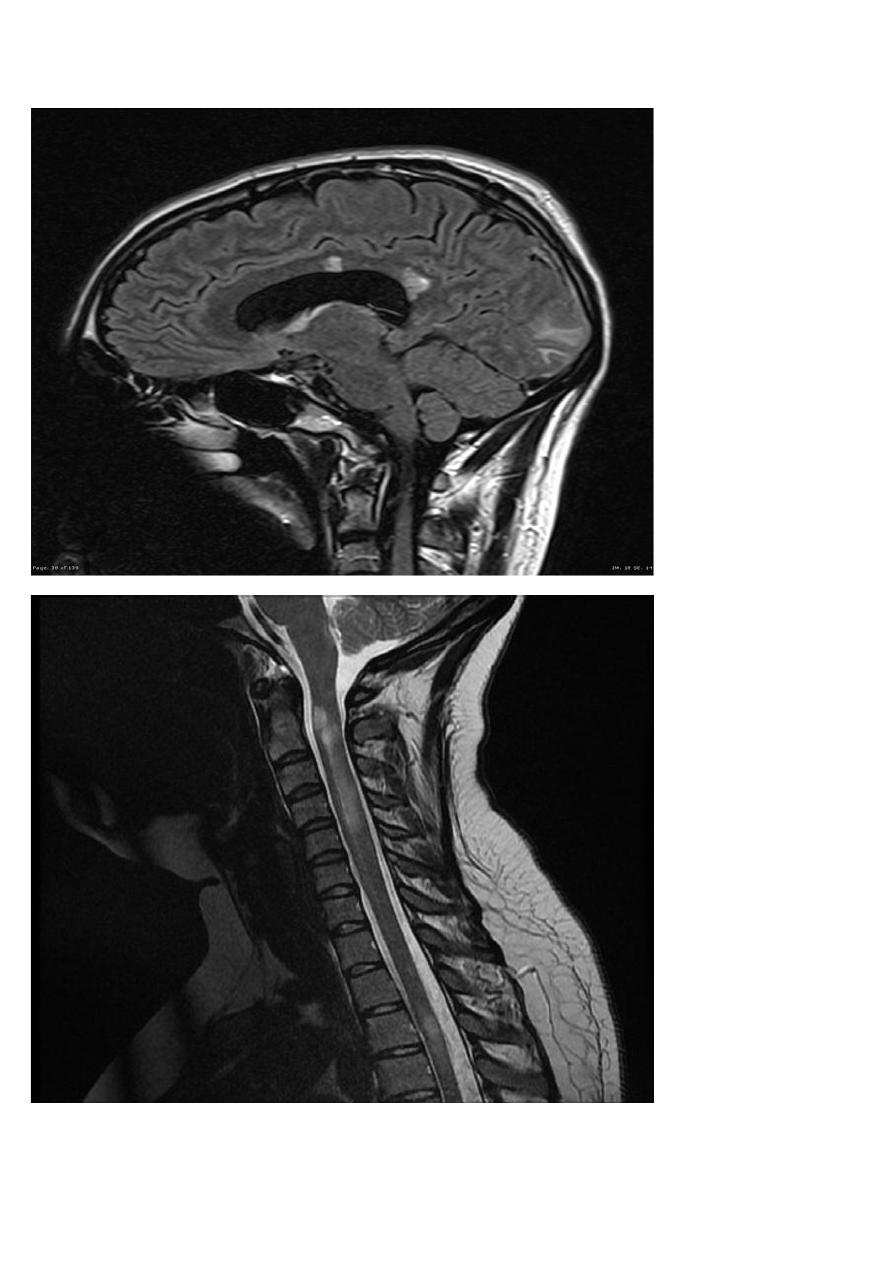
-MRI :characteristic abnormalities are found in >95% of patients,
although more than 90% of the lesions visualized by MRI are
asymptomatic
-Lesions are frequently oriented perpendicular to the ventricular
surface,(Dawson’s fingers)
-Lesions larger than 6 mm located in the corpus callosum,
periventricular white matter, brainstem, cerebellum, or spinal cord are
particularly helpful diagnostically
-Evoked potentials:potentials EP testing assesses function in afferent
(visual, auditory, and somatosensory) or efferent (motor) CNS pathways
-Abnormalities on one or more EP modalities occur in 80–90% of MS
patients
-Cerebrospinal fluid:CSF abnormalities found in MS include a
mononuclear cell pleocytosis and an increased level of Igg index and
oligoclonal band

#DISORDERS THAT CAN MIMIC MS:
-Acute disseminated encephalomyelitis (ADEM)
-Neuro myelitis optica
-Antiphospholipid antibody syndrome
-Behçet’s disease
-Neoplasms (e.g., lymphoma, glioma, meningioma)
-Sarcoidosis
-Stroke and ischemic cerebrovascular disease
#Treatment of Multiple Sclerosis
Therapy for MS can be divided into several categories:
1-treatment of acute attacks
2-treatment with disease-modifying agents that reduce the biological activity
of MS,
3-symptomatic therapy
-Glucocorticoids are used to manage either first attacks or acute
exacerbations.
-They provide short-term clinical benefit by reducing the severity and
shortening the duration of attacks.
-Glucocorticoid treatment is usually administered as intravenous methylprednisolone,
500–1000 mg/d for 3–5 days
#DISEASE-MODIFYING THERAPIES FOR RELAPSING FORMS OF
MS (RRMS, SPMS WITH EXACERBATIONS)
Seven such agents are approved by the U.S. Food and Drug Administration
(FDA): (1) IFN- β-1a (Avonex), (2) IFN- β-1a (Rebif), (3) IFN- β-1b (Betaseron),
(4) glatiramer acetate (Copaxone), (5) natalizumab (Tysabri), (6) fingolimod
(Gilenya), and (7) mitoxantrone (Novantrone)
#CLINICAL VARIANTS OF MS
-Neuromyelitis optica (NMO), or Devic’s syndrome, is an aggressive
inflammatory disorder consisting most typically of attacks of acute ON and
myelitis
- Attacks of ON can be bilateral (rare in MS) or unilateral
-myelitis can be severe and transverse (rare in MS) and is typically
longitudinally extensive, involving three or more contiguous vertebral
segments
-The brain MRI was classically thought to be normal at the onset of NMO
-Up to 40% of patients have a systemic autoimmune disorder, often systemic
lupus erythematosus, Sjögren’s syndrome, myasthenia gravis, Hashimoto’s
thyroiditis
-highly specific autoantibody directed against the water channel protein
aquaporin-4 is present in the sera of 60–70% of patients who have a clinical
diagnosis of NMO.

