
Seminar
Pulmonary Embolism
DVT – Epidemiology and Etiology :
-Annual incidence of venous thromboembolism (VTE) is 1/1000
-DVT accounts for over one half of VTE
-Carefully evaluated, up to 80% of patients with VTE have one
or more risk factors
-Majority of lower extremity DVT arise from calf veins but ~20%
begin in proximal veins
-About 20% of calf-limited DVTs will propagate proximally
DVT – VTE Risk Factors
-
Malignancy
-Surgery
-Trauma
-Pregnancy
-Oral contraceptives or hormonal therapy
-Immobilization
-Inherited thrombophillia
-Presence of venous catheter
-Congestive failure
-Antiphospholipid antibody syndrome
-Hyperviscosity
-Nephrotic syndrome
-Inflammatory bowel disease
An Introduction to Pulmonary embolus
-Pulmonary embolism is a life-threatening condition that occurs
when a clot of blood or other material blocks an artery in the
lungs.
-This is an extremely common and highly lethal condition that is
a leading cause of death in all age groups.
-One of the most prevalent disease processes responsible for
in-patient mortality (30%)
-Overlooked diagnosis.

Pulmonary Embolism back ground
Prompt diagnosis and treatment can dramatically reduce the
mortality and morbidity rate.
Majority of the cases are unrecognised clinically.
One third of the patients who survive an initial PE die of a
future embolic episode.
Many patients who die of PE have
not had any diagnostic workup nor have they received any
prophylaxis for the disease
.
In most cases the CLINICIANS have not even considered the
diagnosis of PE.
Pathophysiology of pulmonary embolism
It is often a fatal complication of underlying venous
thrombosis
.
Normally microthrombi (RBC,Platelets and Fibrin) are
formed and lysed with in the venous circulatory system.
Under pathological condition these microthrombi may
escape and propagate and will block the pulmonary blood
vessels causing PE
Predisposing factors
Patients on prolonged bed rest for > a week. Prolonged
immobilization.
Patients in ICU, CCU.
After bypass surgery or any surgery.
All trimesters of pregnancy and puerperium.
Older patients – Age no bar still.
Predisposing factors
: 1-CCF. 2-Fractures. 3-Oral
Contraceptives. 4-Drug abuse. 5-MI. 6-Obesity. 7-Old age. 8-
Malignancy. 9-Catheter

Patient presentation
Haemoptysis, Dyspnoea and Chest pain –
o (Virchows Triad)
Back pain, Abdominal pain, wheezing, SOB, Seizures,
Productive cough, Hiccoughs, Fever……
Can be asymptomatic
Diagnostic Modalities in PE
ECG***
D Dimer assay test
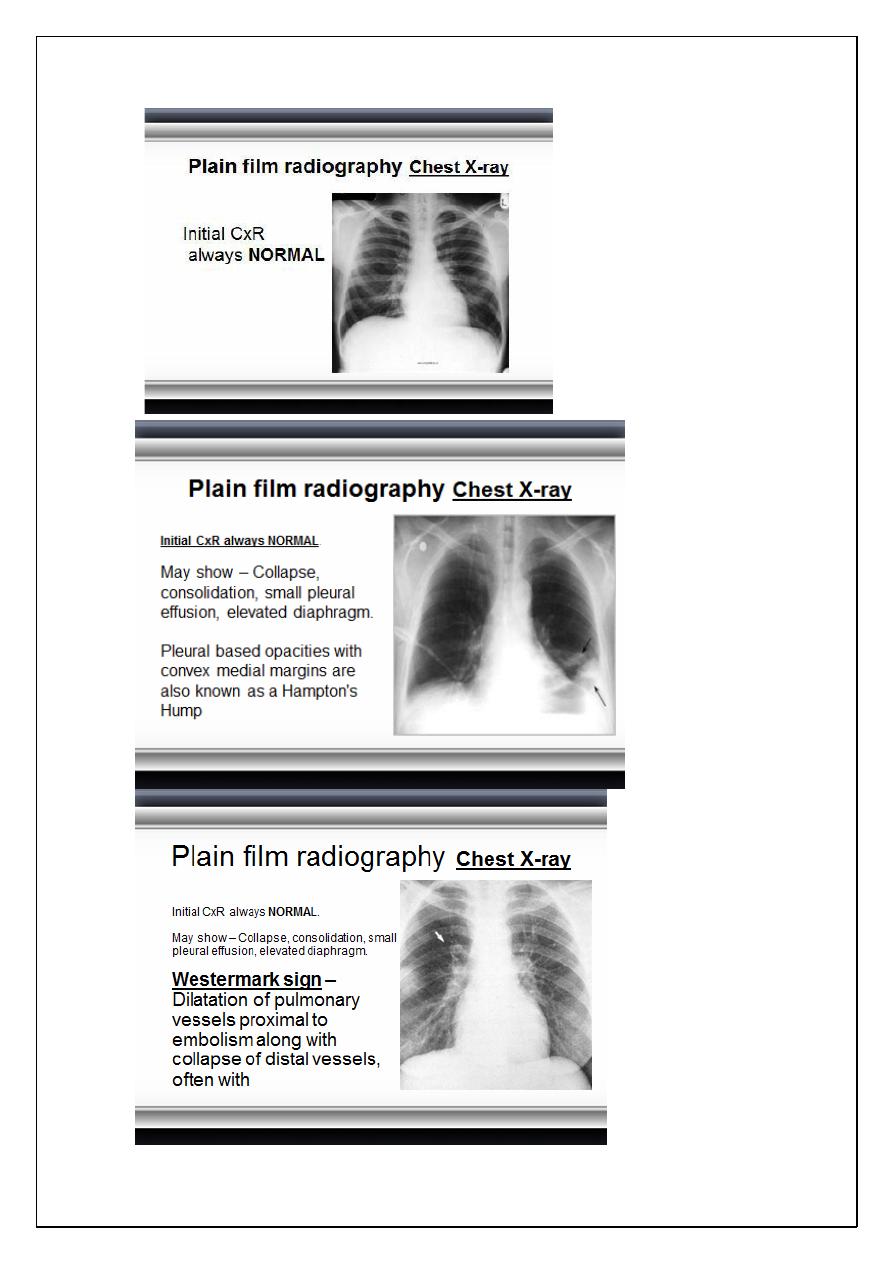
Plain film radiography
Radionuclide imaging (VQ Scan)
CT Angiography
Pulmonary angiography
Echocardiography Ultrasound(DVT)***
MRI & MRA0
D
-Dimer Assays
Gainfully employed to select patients for further
radiological imaging.
It is a cross linked fibrin degradation product and a
plasma marker of fibrin lysis.
Serum level less than 500ng/L excludes PE with 90-95%
accuracy.
Unfortunately a positive test is non specific (specificity
only 25 – 67% and occurs in about 40 – 69% of the patients
s
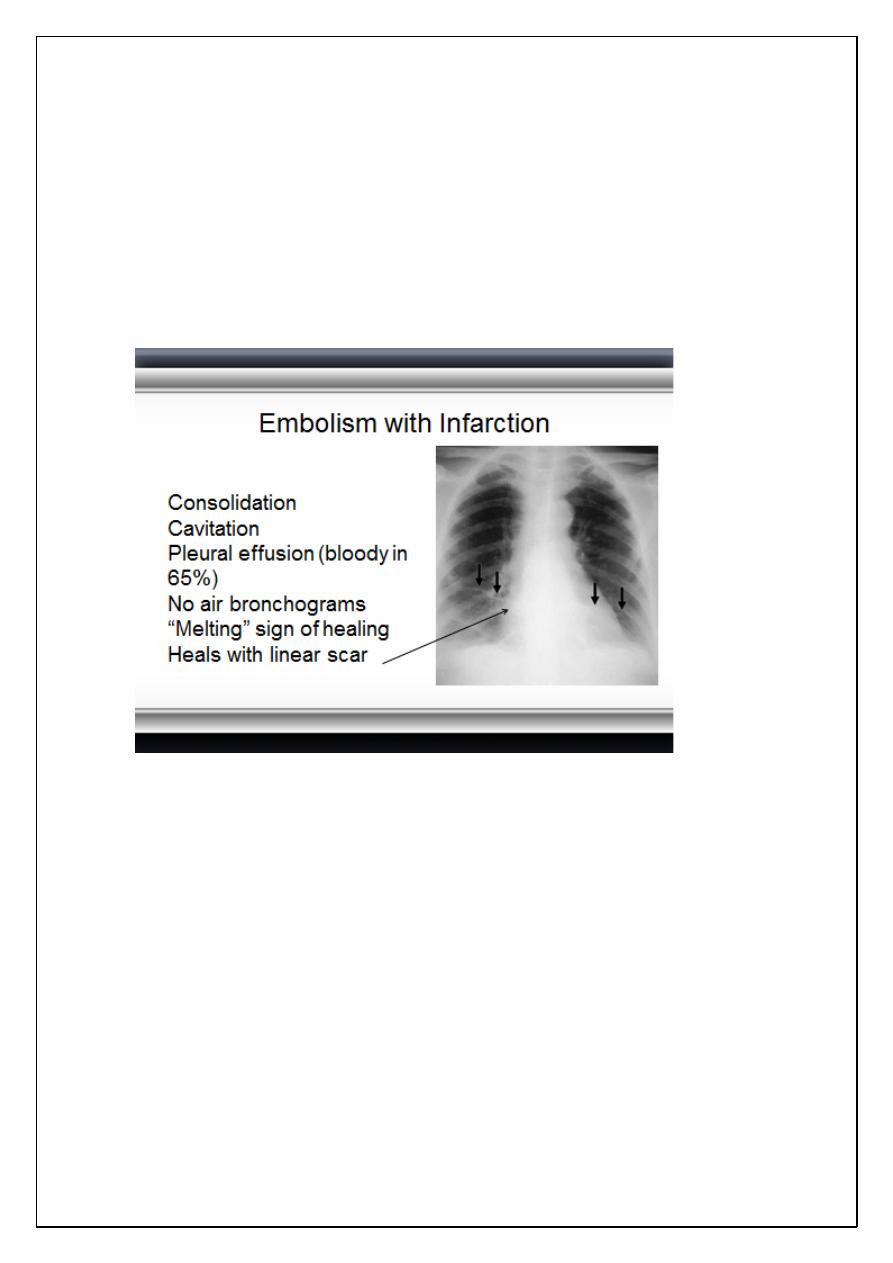
Embolism without Infarction
Most PEs (90%)
Frequently normal chest x-ray
Pleural effusion
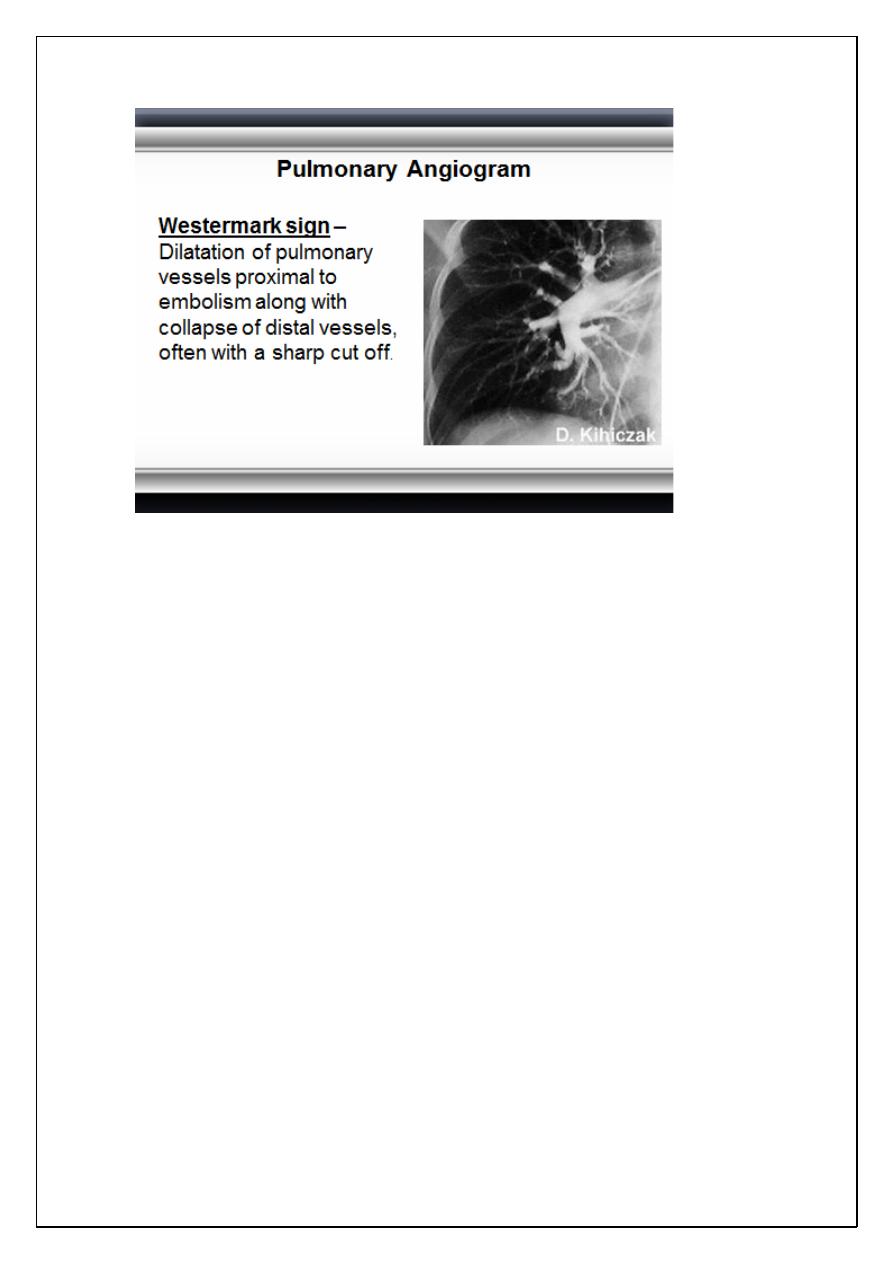
Westermark’s sign
“Knuckle” sign abrupt tapering of an occluded vessel
distally
Elevated hemidiaphragm
Ventilation
-perfusion scanning V/Q Scanning
Single most important diagnostic modality for detecting
PE.
Always indicated when PE is suspected and there is no
other diagnosis.
1 in every 25 pts sent home after a normal V/Q scan
actually has a PE that has been
MISSED
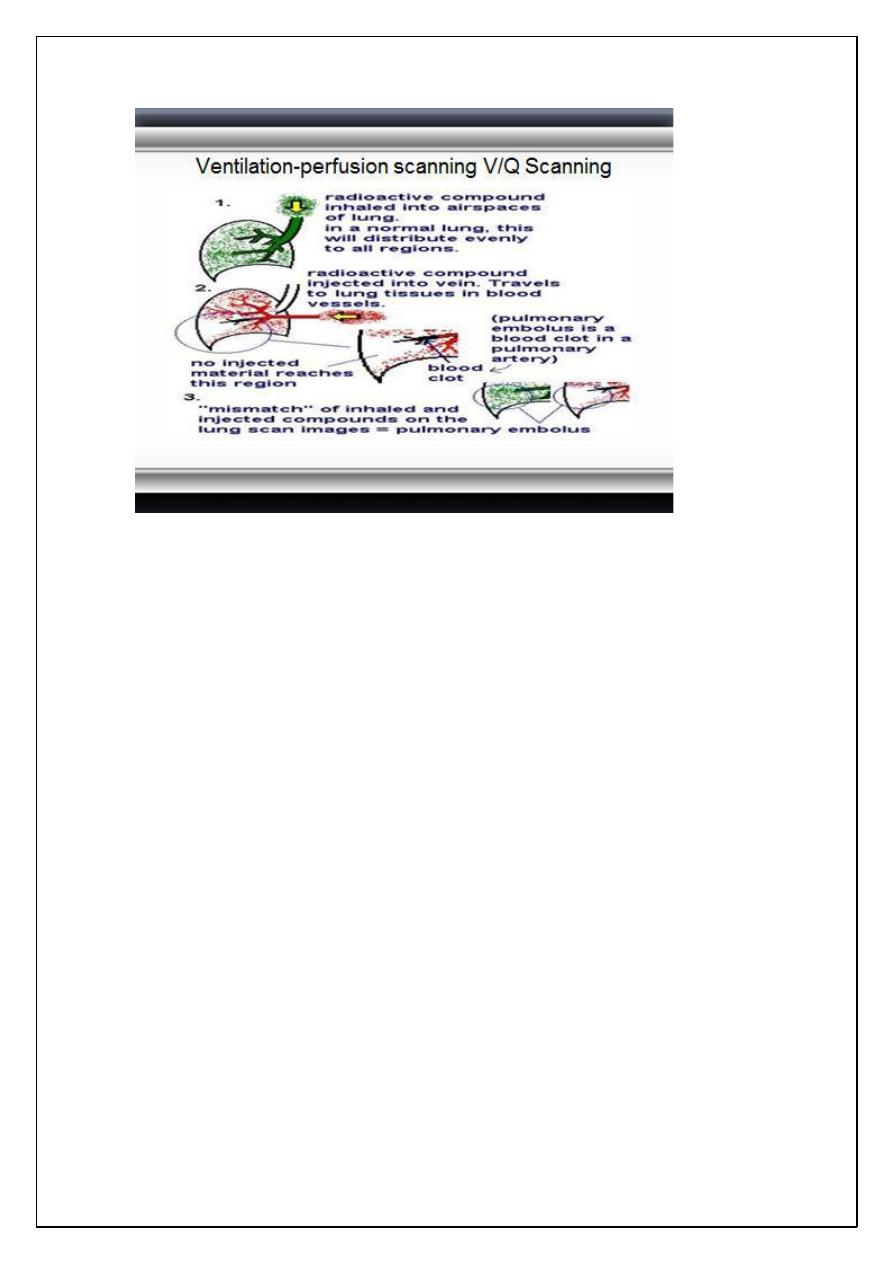
Ventilation
-perfusion scanning V/Q Scanning
Radiological procedure which is often used to confirm or
exclude the diagnosis of pulmonary embolism. It may also
be used to monitor treatment.
The ventilation part of the scan is the inhalation of
Krypton 81m, which has a short half life and is a pure
gamma emitter. Ventilation is assessed under a gamma
camera.
Ventilation
-
perfusion scanning V/Q Scanning
The perfusion part of the scan is achieved by injecting the
patient with technetium 99m, which is coupled with macro
aggregated albumin (MAA). This molecule has a diameter
of 30 to 50 micrometres, and thus sticks in the pulmonary
capillaries.
An embolus shows up as a cold area when the patient is
placed under a gamma camera. The MAA has a half life of
about 10 hours
Spiral CT
HRCT (spiral) CT with CT angiography is a promising
technique.
CT unlikely to miss any lesion.
CT has better sensitivity, specificity and can be used
directly to screen for PE.
CT can be used to follow up “non diagnostic V/Q scans.
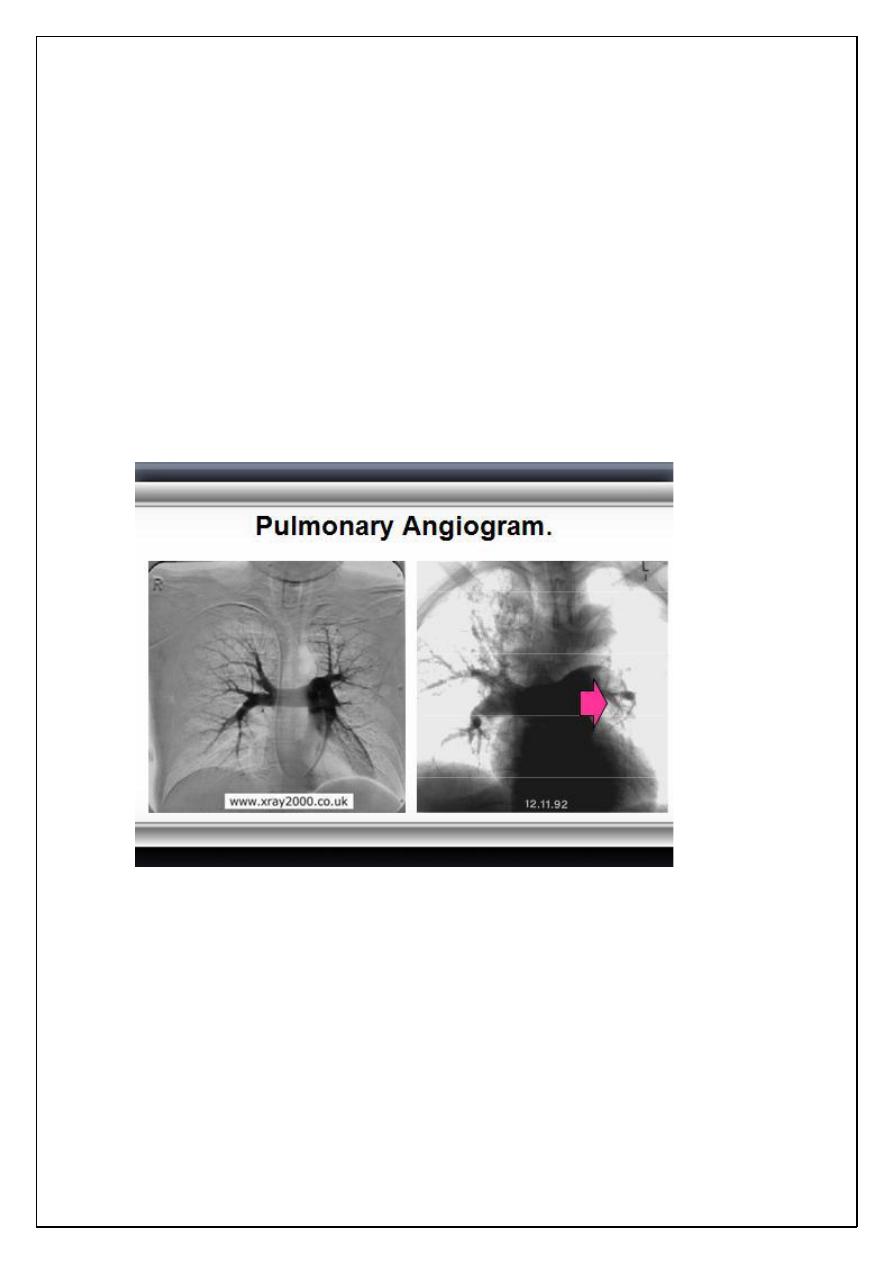
Pulmonary Angiogram
Positive angiogram provides 100% certainty that an
obstruction exists in the pulmonary artery.
Negative angiogram provides > 90% certainty in the
exclusion of PE.
Catherterisation of the
Subclavian vein
–
Superior vena
cava
–
right atrium
–
right ventricle
–
main pulmonary artery
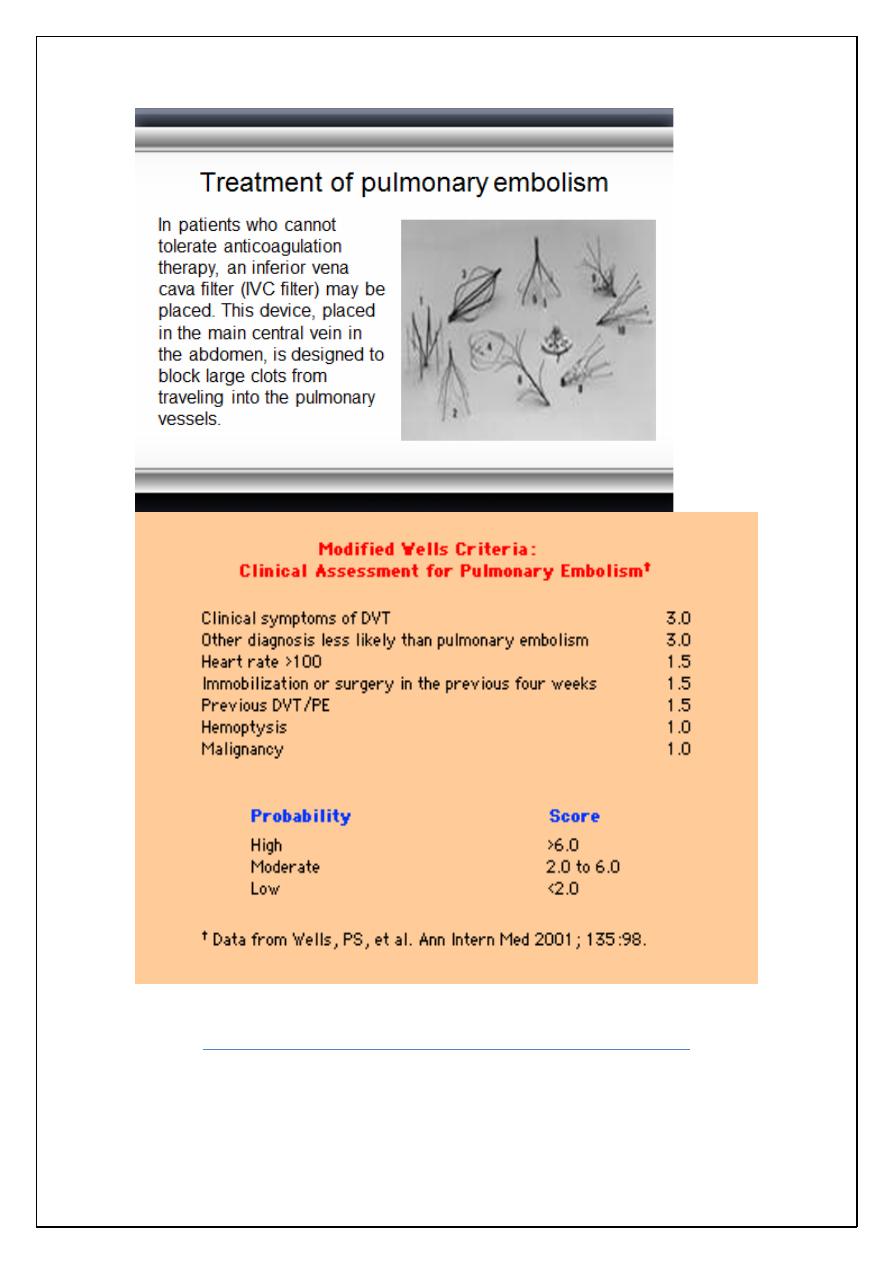
Treatment of pulmonary embolism
Emergency treatment and hospitalization are necessary.
In cases of severe, life-threatening pulmonary embolism,
definitive treatment consists of dissolving the clot with
thrombolytic therapy. Anticoagulant therapy prevents the
formation of more clots and allows the body to re-absorb
the existing clots faster.
Thrombolytic therapy (clot-dissolving medication)
includes streptokinase, urokinase, or t-PA.
Anticoagulation therapy (clot-preventing medication)
consists of heparin by
intravenous
infusion initially, then
oral warfarin (Coumadin).
Subcutaneous
low-molecular
weight heparin is often substituted for intravenous heparin
in many circumstances
ربما تكون عفويتك أ, عنصتت لا
جمل
