1
DISORDERS OF THE SPINAL NERVES AND SPINAL CORD
The spinal cord and spinal roots may be affected by intrinsic disease or by disorders of the
surrounding meninges and bones. The clinical presentation of these conditions depends on
the anatomical level at which the cord or roots are affected, as well as the nature of the
pathological process involved. It is important to recognise when emergency surgical
intervention is necessary and to plan investigations to identify such patients.
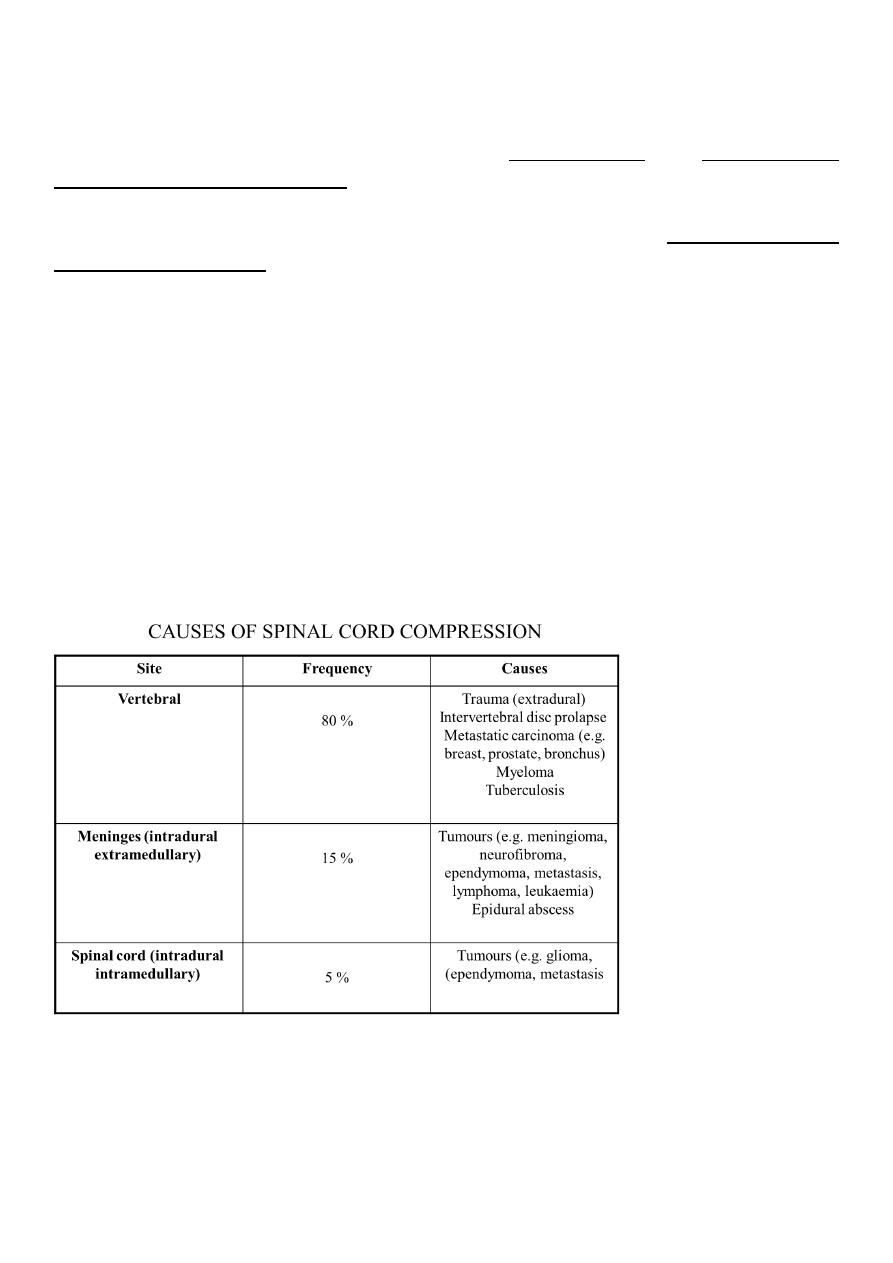
COMPRESSION OF THE SPINAL CORD
Acute spinal cord compression is one of the most common neurological emergencies
encountered in clinical practice. A space-occupying lesion within the spinal canal may
damage nerve tissue either directly by pressure or indirectly by interfering with blood supply.
Oedema from venous obstruction impairs neuronal function, and ischaemia from arterial
obstruction may lead to necrosis of the spinal cord. The early stages of damage are reversible
but severely damaged neurons do not recover; hence the importance of early diagnosis and
treatment.
Clinical features
The onset of symptoms of spinal cord compression is usually slow (over weeks), but can be
acute as a result of trauma or metastases, especially if there is associated arterial occlusion.

2
SYMPTOMS OF SPINAL CORD COMPRESSION
Pain
Localised over the spine or in a root distribution, which may be aggravated by coughing,
sneezing or straining
Sensory
Paraesthesia, numbness or cold sensations, especially in the lower limbs, which spread
proximally, often to a level on the trunk
Motor
Weakness, heaviness or stiffness of the limbs, most commonly the legs
Sphincters
Urgency or hesitancy of micturition, leading eventually to urinary retention
Pain and sensory symptoms occur early, while weakness and sphincter dysfunction are
usually late manifestations.
The signs vary according to the level of the cord compression and the structures involved.
There may be tenderness to percussion over the spine if there is vertebral disease, and this
may be associated with a local kyphosis.
Involvement of the roots at the level of the compression may cause dermatomal sensory
impairment and corresponding lower motor signs.
Interruption of fibres in the spinal cord causes sensory loss
SIGNS OF SPINAL CORD COMPRESSION
Cervical, above C5
Upper motor neuron signs and sensory loss in all four limbs
Diaphragm weakness (phrenic nerve)
Cervical, C5 to T1
Lower motor neuron signs and segmental sensory loss in the arms; upper motor neuron
signs in the legs
Respiratory (intercostal) muscle weakness
Thoracic cord
Spastic paraplegia with a sensory level on the trunk

3
Conus medullaris
Lesions at the end of the spinal cord cause sacral loss of sensation and extensor plantar
responses
Cauda equina
Spinal cord ends at approximately the T12/L1 spinal level and spinal lesions below this level
can only cause lower motor neuron signs by affecting the cauda equina
INVESTIGATION OF ACUTE SPINAL CORD SYNDROME
Plain X-rays of spine may show bony destruction and soft-tissue abnormalities and are an
essential initial investigation
Chest X-rays may provide evidence of systemic disease
MRI of spine is the investigation of choice; myelography also localises the lesion and, with
CT in suitable cases, defines the extent of compression and associated soft-tissue
abnormality
CSF should be taken for analysis at the time of myelography. In cases of complete spinal
block this shows a normal cell count with a very elevated protein causing yellow
discoloration of the fluid (Froin's syndrome). Acute deterioration may develop after
myelography and the neurosurgeons should be alerted before it is undertaken.
Serum B
12
Needle biopsy is required prior to radiotherapy to establish the histological nature of the
tumour.
Management
Treatment and prognosis depend on the nature of the underlying lesion. Benign tumours
should be surgically excised, and a good functional recovery can be expected unless a
marked neurological deficit has developed before diagnosis.
Extradural compression due to malignancy is the most common cause of spinal cord
compression in developed countries and has a poor prognosis, although useful function can
be regained if treatment is initiated within 24 hours of the onset of severe weakness or
sphincter dysfunction. Surgical decompression may be appropriate in some patients, but
has a similar outcome to radiotherapy.
4
Spinal cord compression due to tuberculosis is common in some areas of the world, and
requires surgical treatment if seen early. This should be followed by appropriate anti-
tuberculous chemotherapy for an extended period.
Traumatic lesions of the vertebral column require specialised neurosurgical treatment.
5
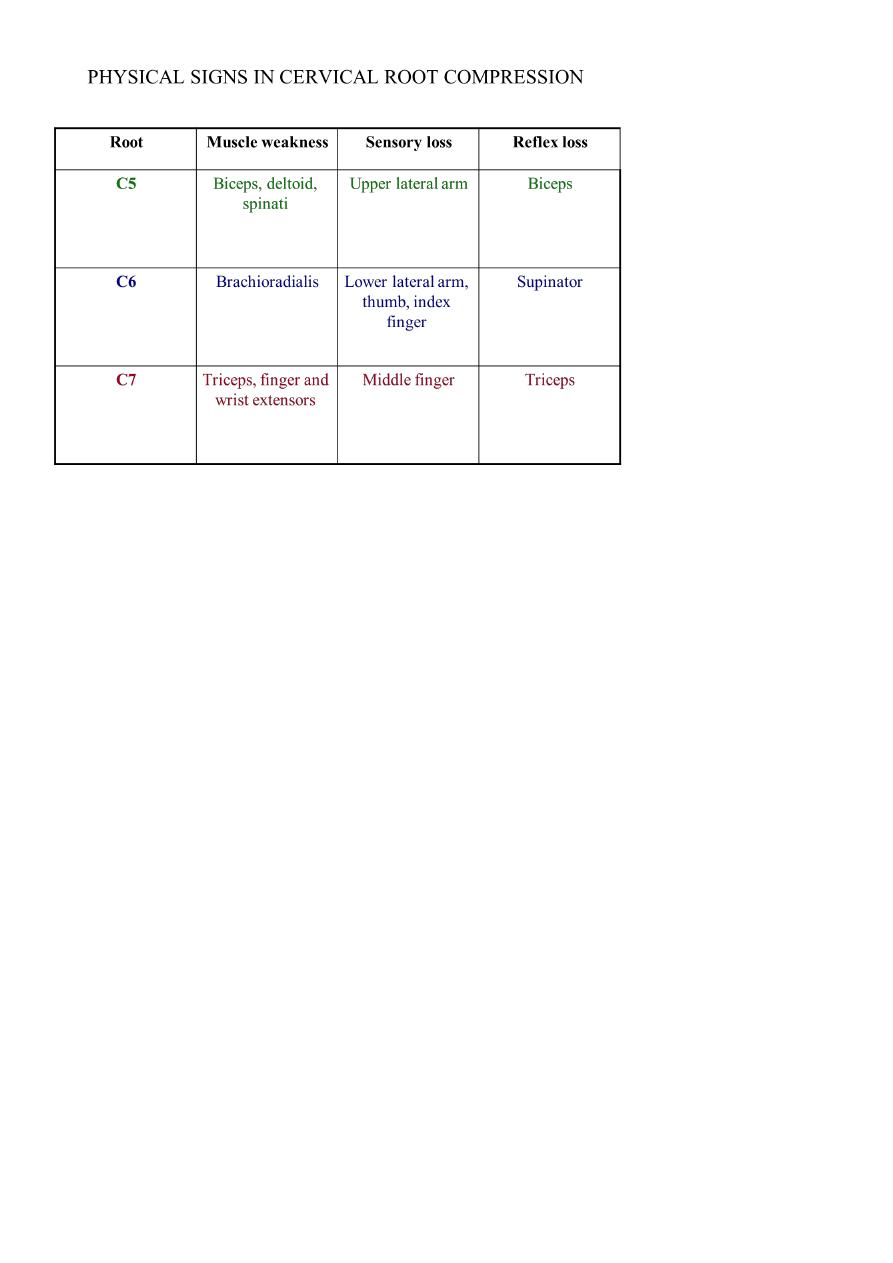
CERVICAL SPONDYLOSIS
In the cervical spine, some degree of osteoarthritic degenerative change is a normal
radiological finding in the middle-aged and elderly. Degeneration of the intervertebral discs
and secondary osteoarthrosis (cervical spondylosis) is often asymptomatic, but may be
associated with neurological dysfunction. The C5/6, C6/7 and C4/5 vertebral levels and C6,
C7 and C5 roots, respectively, are most commonly affected
CERVICAL SPONDYLOTIC RADICULOPATHY
Compression of a nerve root occurs when a disc prolapses laterally, which may develop
acutely or more gradually due to osteophytic encroachment of the intervertebral foramina.
Clinical features
The patient complains of pain in the neck that may radiate in the distribution of the
affected nerve root. The neck is held rigidly and neck movements may exacerbate pain.
Paraesthesia and sensory loss may be found in the affected segment and there may be
lower motor neuron signs, including weakness, wasting and reflex impairment
6
Investigations
Plain X-rays, including lateral and oblique views, should be obtained to confirm the
presence of degenerative changes and to exclude other conditions, including destructive
lesions. If surgery is contemplated, MRI is required. Electrophysiological studies rarely add
to the clinical examination, but may be necessary if there is doubt about the differential
diagnosis between root and peripheral nerve lesions.
Management
Conservative treatment with analgesics and physiotherapy results in resolution of
symptoms in the great majority of patients, but a few require surgery in the form of
foraminotomy or disc excision.
CERVICAL SPONDYLOTIC MYELOPATHY
Dorsomedial herniation of a disc and the development of transverse bony bars or posterior
osteophytes may result in pressure on the spinal cord or the anterior spinal artery which
supplies the anterior twothirds of the cord
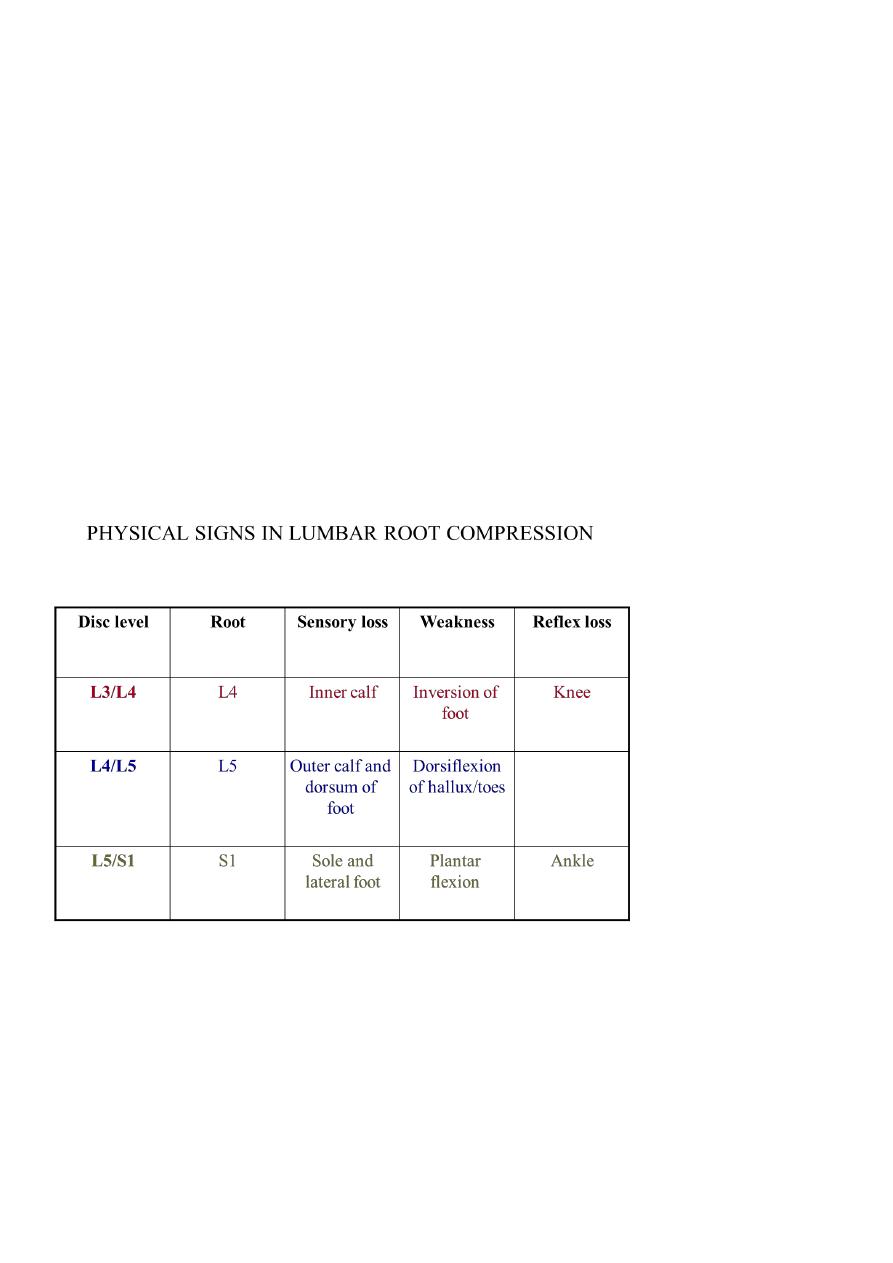
LUMBAR DISC HERNIATION
Acute lumbar disc herniation is often precipitated by trauma, usually by lifting heavy
weights while the spine is flexed. The nucleus pulposus may bulge or rupture through the
7
annulus fibrosus, giving rise to pressure on nerve endings in the spinal ligaments, changes
in the vertebral joints or pressure on nerve roots.
Clinical features
The onset may be sudden or gradual. Alternatively, repeated episodes of low back pain may
precede sciatica by months or years. Constant aching pain is felt in the lumbar region and
may radiate to the buttock, thigh, calf and foot. Pain is exacerbated by coughing or straining
but may be relieved by lying flat.
The altered mechanics of the lumbar spine result in loss of lumbar lordosis and there may
be spasm of the paraspinal musculature. Root pressure is suggested by limitation of flexion
of the hip on the affected side if the straight leg is raised (Lasègue's sign). If the third or
fourth lumbar roots are involved, Lasègue's sign may be negative, but pain in the back may
be induced by hyperextension of the hip (femoral nerve stretch test).
Investigations
Plain X-rays of the lumbar spine are of little value in the diagnosis of lumbar disc disease,
although they may show other conditions such as malignant infiltration of a vertebral body.
CT, especially using spiral scanning techniques, can provide helpful images of the disc
protrusion and/or narrowing of the exit foramina. MRI is the investigation of choice if
available, since soft tissues are well imaged.

8
Management
Some 90% of patients with sciatica recover with conservative treatment with analgesia and
early mobilisation; bed rest does not help recovery. The patient should be instructed in
back-strengthening exercises and advised to avoid physical manoeuvres likely to strain the
lumbar spine. Injections of local anaesthetic or corticosteroids may be useful adjunctive
treatment if symptoms are due to ligamentous injury or joint dysfunction. Surgery may
have to be considered if there is no response to conservative treatment or if progressive
neurological deficits develop. Central disc prolapse with bilateral symptoms and signs and
disturbance of sphincter function requires urgent surgical decompression.
LUMBAR CANAL STENOSIS
This is due to a congenital narrowing of the lumbar spinal canal exacerbated by the
degenerative changes that occur with age.
