
1
_______________________________________________________
Indications of blood components:
* Blood transfusion:
- Replace acute blood loss
- Chronic hemolytic diseases like thalassemia & sickle cell anemia
- Severe anemia (maintain Hb at 70 g/l if there is no cardiovascular diseases,
maintain Hb at 90g/l if there is known cardiovascular disease).
- Failure of other modalities of treatment.
* Platelet concentrate:
indicated in cases of thrombocytopenia as explained below :
- In acute leukemia maintain platelets count >10 if not bleeding & > 20 if there
is bleeding or at risk of bleeding .
- For minor invasive procedures maintain platelets > 50, for major operations
maintain platelets > 100 .
*Fresh frozen plasma :
- Warfarin associated hemorrhage
-Treatment of bleeding associated with multiple acquired clotting factor
deficiencies (liver disease, disseminated intravascular coagulation).
-Replacement solution for plasma exchange
* Cryoprecipitate:
-Congenital or acquired fibrinogen deficiency
-Dysfibrinogenemia
-Factor XIII deficiency
-Treatment of hemophilia A and von Willebrand disease when another more
suitable product is not available.
Acute Transfusion Reactions
.د
محمد
حارث
Seminars

2
Adverse transfusion reactions:
✓ Hemolytic reactions:
a. Acute hemolytic transfusion reaction
b. Delayed hemolytic transfusion reaction.
a. Acute hemolytic reaction:
characterized by the immediate destruction of donor erythrocytes by recipient
antibodies. These reactions are most commonly caused by ABO
incompatibilities or, occasionally, alloantibodies to other erythrocyte antigens
Signs and symptoms include fever, chills, dyspnea, red urine, flank pain, kidney
injury, DIC, and hypotension/shock.
Treatment of hemolytic reactions:
-stop the transfusion
- Start IV fluid immediately
- Catheterize the patient & monitor urine output
- Treat DIC if present
- Inform the transfusion department.
b. Delayed hemolytic transfusion reactions occur 2 to 10 days after
transfusion, are often extravascular, and present with fever, jaundice,
and worsening anemia.
hemoglobinur
ia
3
✓
Febrile non-hemolytic reaction:
Febrile nonhemolytic transfusion
reactions are common and occur within several hours of an erythrocyte or
platelet transfusion. Febrile nonhemolytic transfusion reactions are
mediated by the generation of leukocytederived cytokines during
erythrocyte and platelet storage. Symptoms include fever, chills, rigors, or
dyspnea.
-Management consists of transfusion discontinuation to exclude a more
serious transfusion reaction, acetaminophen for fever. Restart transfusion
at slower rate Leukoreduction of packed red blood cells and platelets
before storage significantly reduces the rate of febrile nonhemolytic
transfusion reactions.
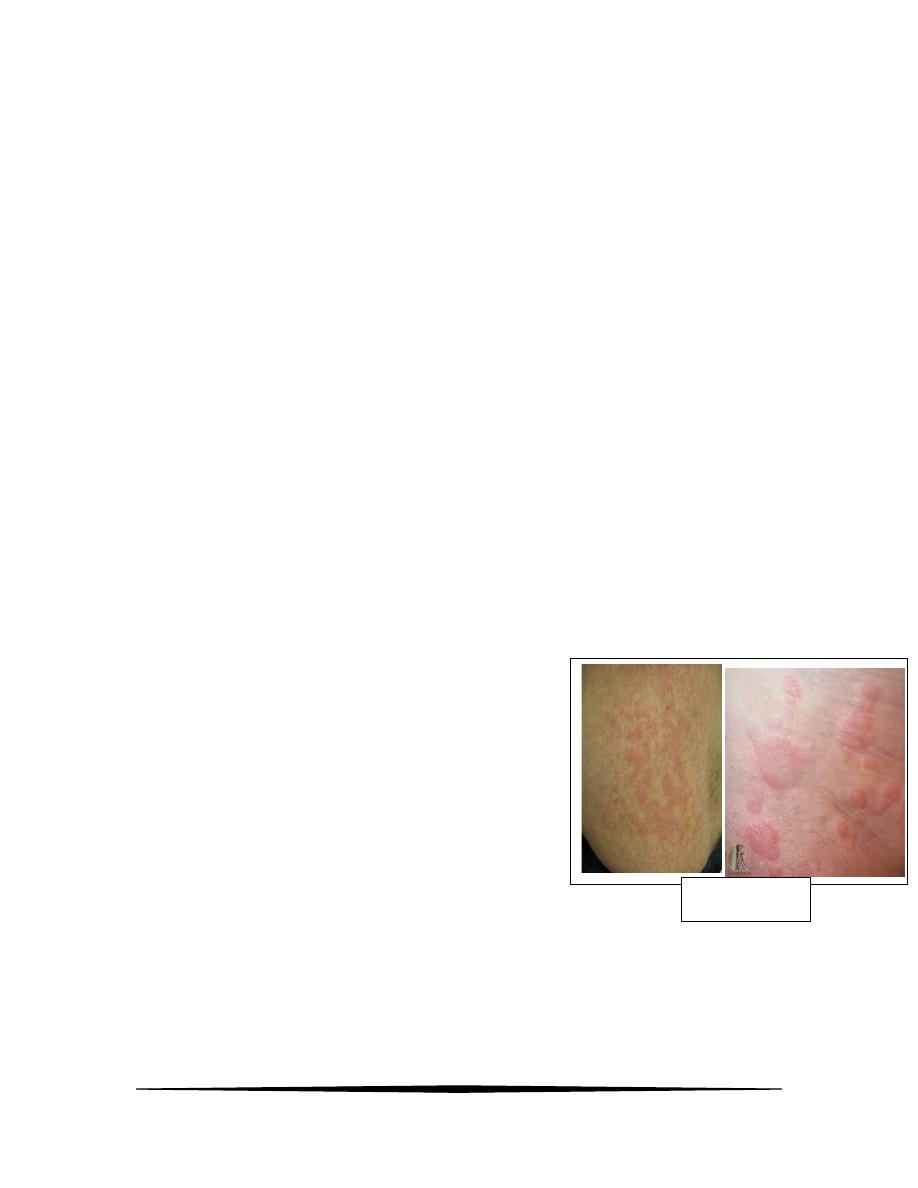
✓ Allergic reactions:
*Mild allergic reactions:
-occur because of recipient IgE antibodies with reactivity to allergens in
the plasma of the transfused product. Signs and symptoms are largely
restricted to urticaria & pruritus.
-Management include:
- Stop the transfusion temporarily
- Give anti histamine (allermin).
- Restart transfusion at slower rate
& observe closely.
urticaria

4
* Severe allergic reactions & anaphylaxis:
Rarely, anaphylaxis occurs within seconds to several minutes of
transfusion. Patients with IgA deficiency are at higher risk because of the
presence of anti IgA antibodies.
-Manifestations include the sudden onset of respiratory distress,
bronchospasm, angioedema, urticaria, nausea and vomiting, abdominal
pain, tachycardia, and hypotension.
-Management of severe allergy or anaphylaxis:
- Discontinue transfusion
- Give cholrphenirman iv slowly
- Give steroid (H.C.) 100 mg slowly iv
- Commence O2 & fluid support
- Give salbutamol nebulizer
- If severe hypotension or bronchospasm give adrenaline 0.5 mg IM.
✓ Transfusion-associated Circulatory Overload:
(raised CVP)!
Signs and symptoms include dyspnea, hypoxia, tachycardia, headache,
and hypertension, and physical examination demonstrates evidence of
pulmonary edema or other signs of volume overload. Risk factors include
age older than 60 years, chronic kidney disease, heart failure, number of
blood products transfused, and volume transfused per hour.
Management consists of transfusion discontinuation, O2, diuretic therapy
(Lasix 40 -80mg). Prevention includes a slower infusion rate (1
mL/kg/hour) and diuretic therapy between transfusion to maintain
euvolemia for those at risk.
5
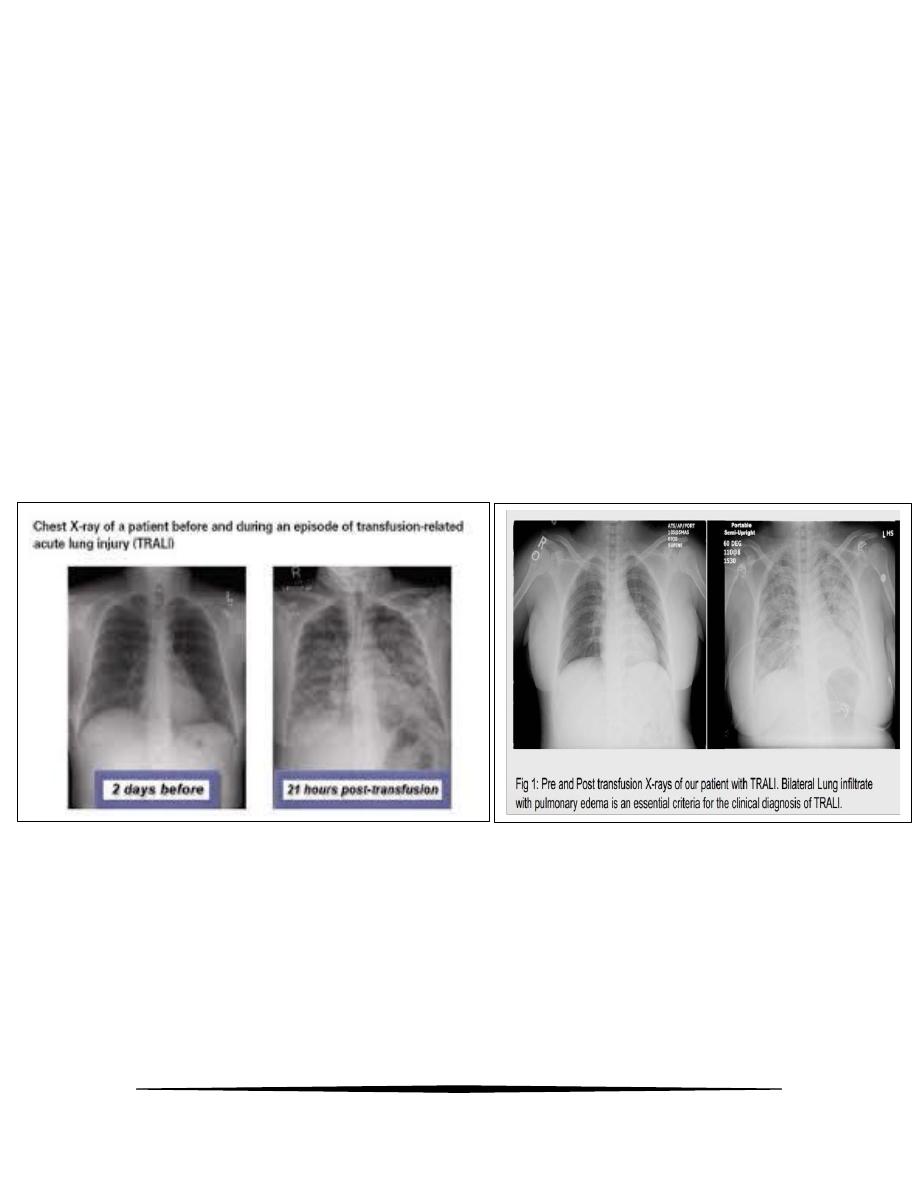
✓ Transfusion-related Acute Lung Injury (TRALI ):
(CVP IS NORMAL)
Transfusion-related acute lung injury (TRALI) is the leading cause of
transfusion-related mortality. It is characterized by the development of
acute lung injury within 6 hours of transfusion of erythrocytes, platelets,
or FFP. TRALI is mediated by initial priming of neutrophils in the
recipient's lung parenchyma (endothelial damage, for example) followed
by their activation by anti-HLA and antineutrophil antibodies present in
donor plasma. Signs and symptoms escalate quickly and include
dyspnea,COUGH , hypoxia, fever, chills, and hypotension. Chest
radiograph reveals diffuse bilateral pulmonary infiltratrate.
Management of TRALI:
- Discontinue transfusion.
- Give 100% O2.
- Treat as ARDS – ventilate if severely hypoxemic.
