
1 |
P a g e
Department of general medicine
Upper abdominal pain
( selected causes )
1- Acute pancreatitis
2- Chronic pancreatitis
3- Gallstones
4- Cholecystitis and cholangitis
Objectives :
1-approach to a patient with upper abdominal pain
- History
- Examination
- Investigation
- Treatment
2- causes of upper abdominal pain
3- specific pathologies
HISTORY :
Abdominal pain is not necessarily originated from the abdominal organs , it
might be radiated form extra abdominal structure .
A - pain from the intra abdominal organs which should be analyzed
according to specific parameters :
1- Main site
2- The onset
3- Radiation
4-Character
5- Frequency and periodicity
6- Severity
7- Special time of occurrence
8- Aggravating factors
9- Relieving factors
10- Associated phenomena
2 |
P a g e
B- pain from extra abdominal organs that radiate to the abdomen could be
from :
_ Ischemic heart diseases
- myocardial infarction
- angina pectoris
_ Pneumonia
_ Esophageal disorder
_ Root pain
EXAMNATION :
_ General examination and vital sings
- general look
- body build
- state of dehydration
- anemia
- jaundice
- temperature
- pulse rate
- respiratory rate
- blood pressure
Abdominal examination :
- Inspection
- palpation
- percussion
- auscultation
INSPECTION :
1_ skin and surface of abdomen
- scars
- striae
- prominent superficial veins
- pigmentation
3 |
P a g e
2_ shape of abdomen
3_ umbilicus
4_ movement of abdomen
5_ pulsation
6_ peristalsis
PALPATION :
1- superficial palpation
- tenderness
- rigidity
- any bulging mass
2_ deep palpation
- liver
- spleen
- kidneys
PERCUSSION :
Normally the abdomen is tympanic on percussion
except on enlarged organs ,
_don not percuss over a tender area!!!
the aim of percussion are :
-to confirm an enlarged organs
( liver , spleen ….etc )
-Liver percussion , spleen percussion
-to confirm a shifting dullness & transmitted thrill in
suspected ascites .
AUSCLTATION :
- listen to bowel sound
- to detect bruits
INVESTIGATION :
in general ;
- complete blood count
- liver function test
- renal function test and electrolytes

4 |
P a g e
- serum lipase & amylase
- urinalysis
- plain abdominal X-ray
-chest X-ray
- ECG
- US.
- CT.
- endoscopy
TREATMENT :
IS ACCORDINGLY ………!!!!
2- Causes of upper abdominal pain :
_
3-Specific pathologies :
Acute pancreatitis
_
Acute pancreatitis accounts for 3% of all cases of abdominal pain
admitted to hospital. It affects 2–28 per
100 000 of the population and is increasing in incidence. It is a
potentially serious condition with an overall mortality of 10%. About
80% of all cases are mild and have a favourable outcome. About 98%
of deaths from pancreatitis occur in the 20% of patients with severe
disease and about one-third of these occur within the first week,
usually from multi-organ failure.
After this time, the majority of deaths result from sepsis, especially
that complicating infected necrosis. Patients who are predicted to
have severe pancreatitis and those with necrosis or other
complications should be managed in a specialist centre with an

5 |
P a g e
intensive therapy unit
Key Point
§ Gallstones and alcohol use are the most common causes of acute
pancreatitis, accounting for 80% of cases in the United
States.
Clinical features
6 |
P a g e
Investigation :
_lab. Studies
- CBC ( leukocytosis )
- serum amylase & lipase ( elevated )
- serum electrolytes ( hypocalcemia , hypokalemia )
- blood urea nitrogen
- blood glucose ( hyperglycemia in severe cases )
- LDH.
- CRP. ( elevated )
- ABG . ( if pt. is dyspneic )
- IGg. level should be checked to evaluate for autoimmune pancreatitis )
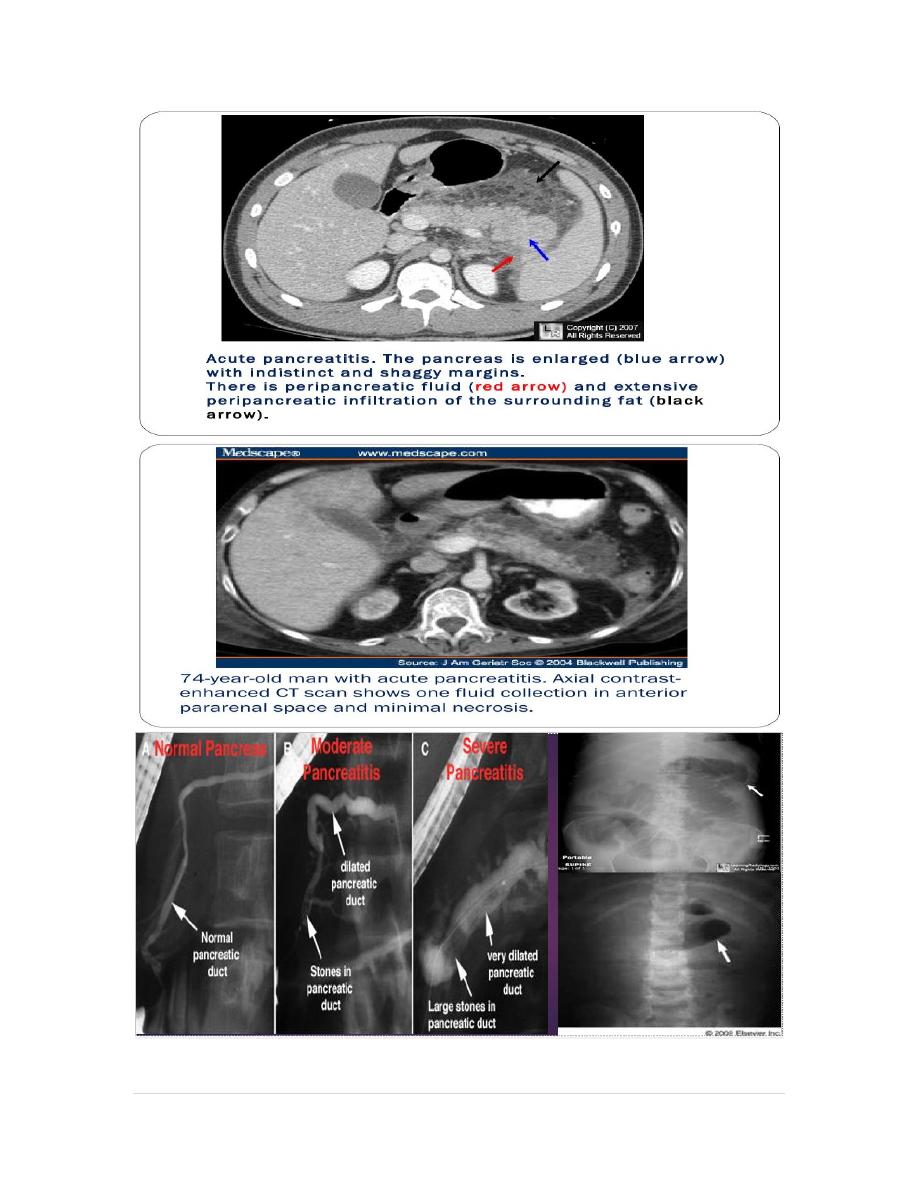
__ Abdominal x-ray
__ US.
__ CT.
__ MRI.
__ ERCP.
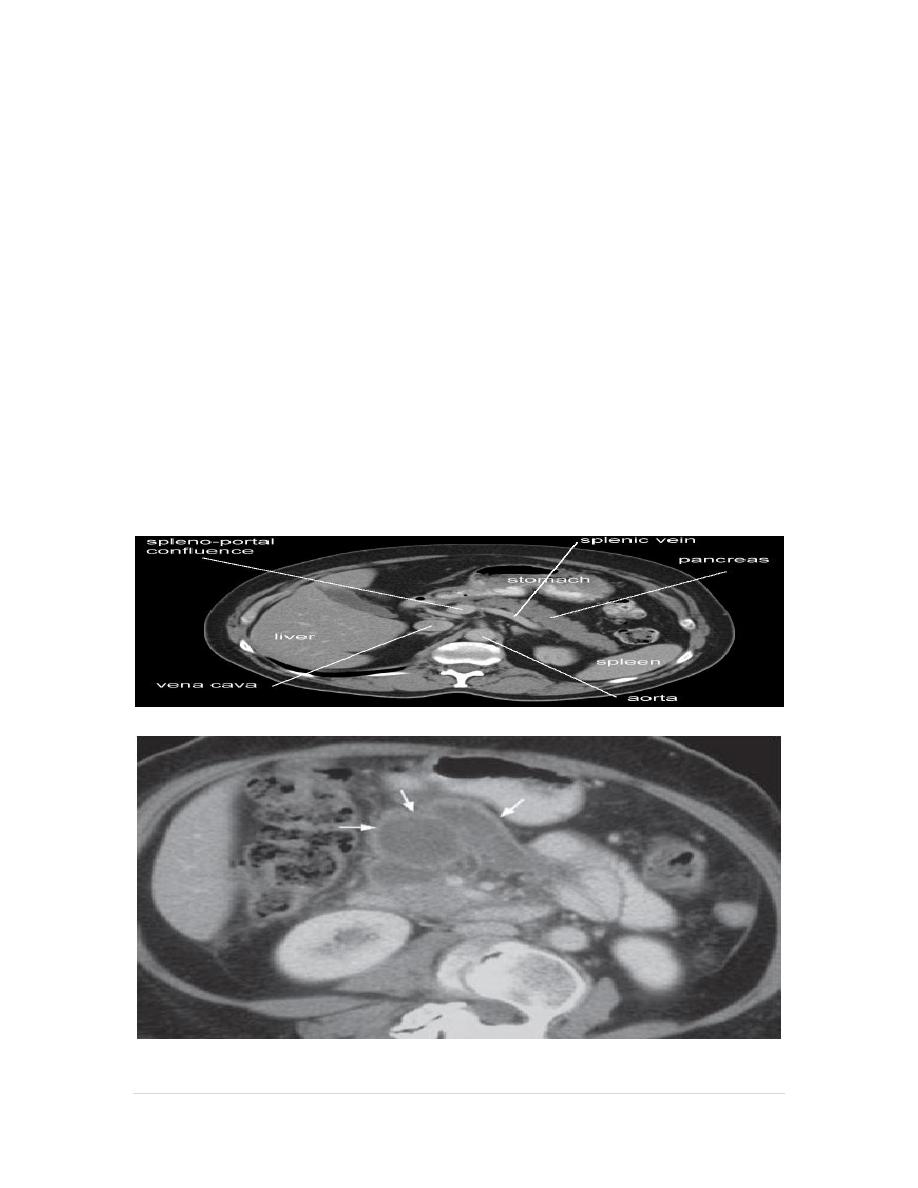
Edematous acute pancreatitis.
7 |
P a g e
8 |
P a g e
TREATMENT :
_
-Opiate analgesics should be given to treat pain
- Hypovolaemia should be corrected using normal saline or other
crystalloids.
-Admission to intensive care unit in sever cases.
- Oxygen should be given to hypoxic patients.
- Hyperglycaemia should be corrected using insulin.
- Hypocalcaemia need correction by intravenous calcium injection if
tetany occurs.
- Nasogastric aspiration if paralytic ileus is present
- Prophylaxis of thromboembolism with subcutaneous low-molecular-
weight heparin
- Prophylactic, broad-spectrum intravenous antibiotics, such as
imipenem or cefuroxime, to prevent infection
- Urgent ERCP to diagnose and treat choledocholithiasis.
- Treatment of complications like necrosectomy and drainage of
pancreatic abscess or pancreatic pseudocysts

9 |
P a g e
COMPLICATION :
Key Points
Diagnosis of acute pancreatitis requires two of three criteria:
(1) acute onset of upper abdominal pain,
(2) serum amylase or lipase level increased by at least three times the
upper limit of normal, and
(3) characteristic findings on cross-sectional
imaging.
_
Because gallstones are the most common cause of pancreatitis, all
patients should be evaluated with a transabdominal
ultrasound unless another obvious cause of pancreatitis is present.
_
Contrast-enhanced CT is not usually required to diagnose acute
pancreatitis; it is less sensitive than ultrasound for
gallstones, exposes patients to the risk of contrast-medium–induced
nephropathy (particularly in underresuscitated patients), and is
expensive.
_
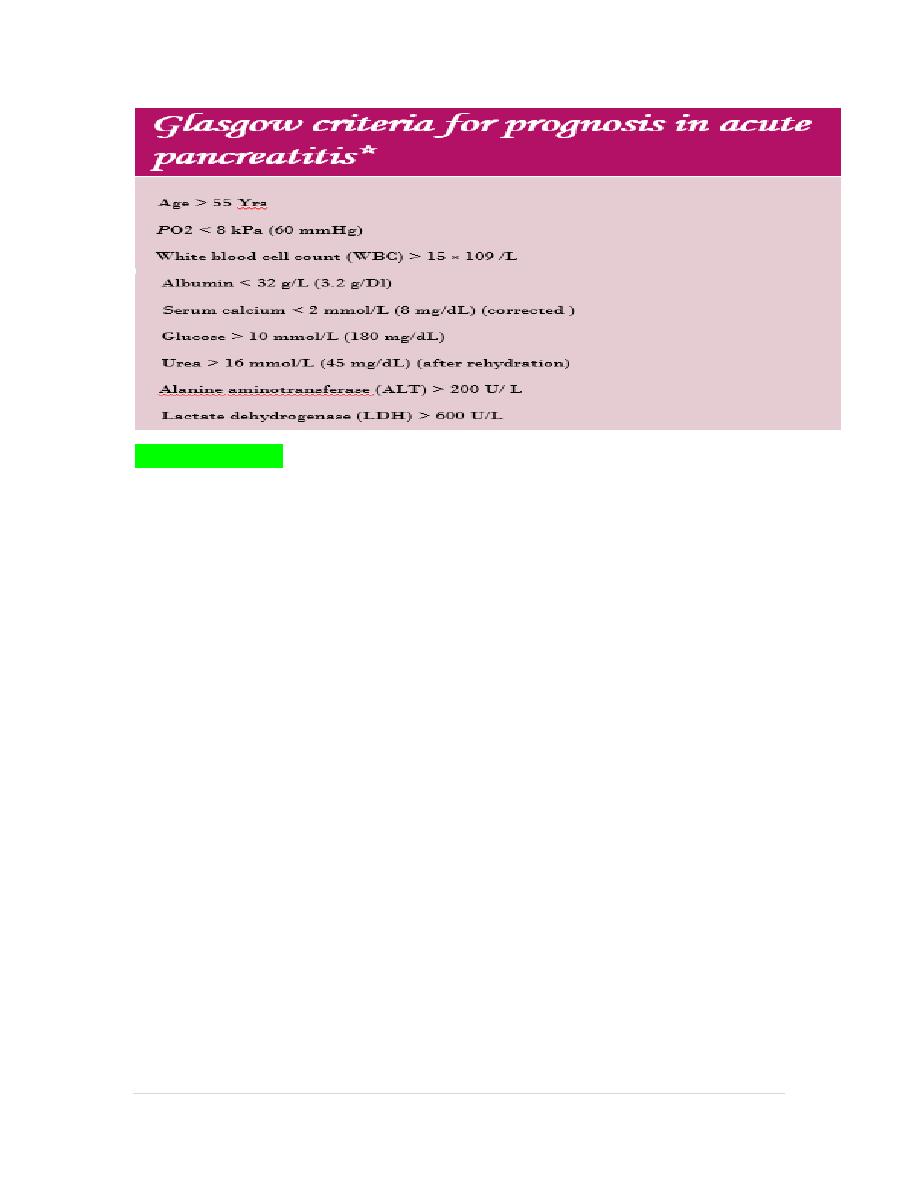
Poor prognostic indicators for acute pancreatitis are elevated serum
blood urea nitrogen level greater than 20 mg/dL (7.1
mmol/L), a hematocrit greater than 44%, or an elevated serum creatinine
level.
Chronic pancreatitis
Chronic pancreatitis is a chronic inflammatory disease characterised by
fibrosis and destruction of exocrine pancreatic tissue , Around 80% of cases
in Western countries result from alcohol misuse.
10 |
P a g e
Pathophysiology of chronic pancreatitis,
_
Alcohol and other risk factors may trigger acute pancreatitis(AP) through
multiple mechanisms. The first (or ‘sentinel’)episode of acute pancreatitis
initiates an inflammatory response involving T-helper cells.
_
Ongoing exposure to alcohol drives further inflammation but this is
modified by regulatory T cells with subsequent fibrosis, via activation of
pancreatic stellate cells.
_
A cycle of inflammation and fibrosis ensues, with development of chronic
pancreatitis. Alcohol is the most relevant risk factor, as it is involved at
multiple steps
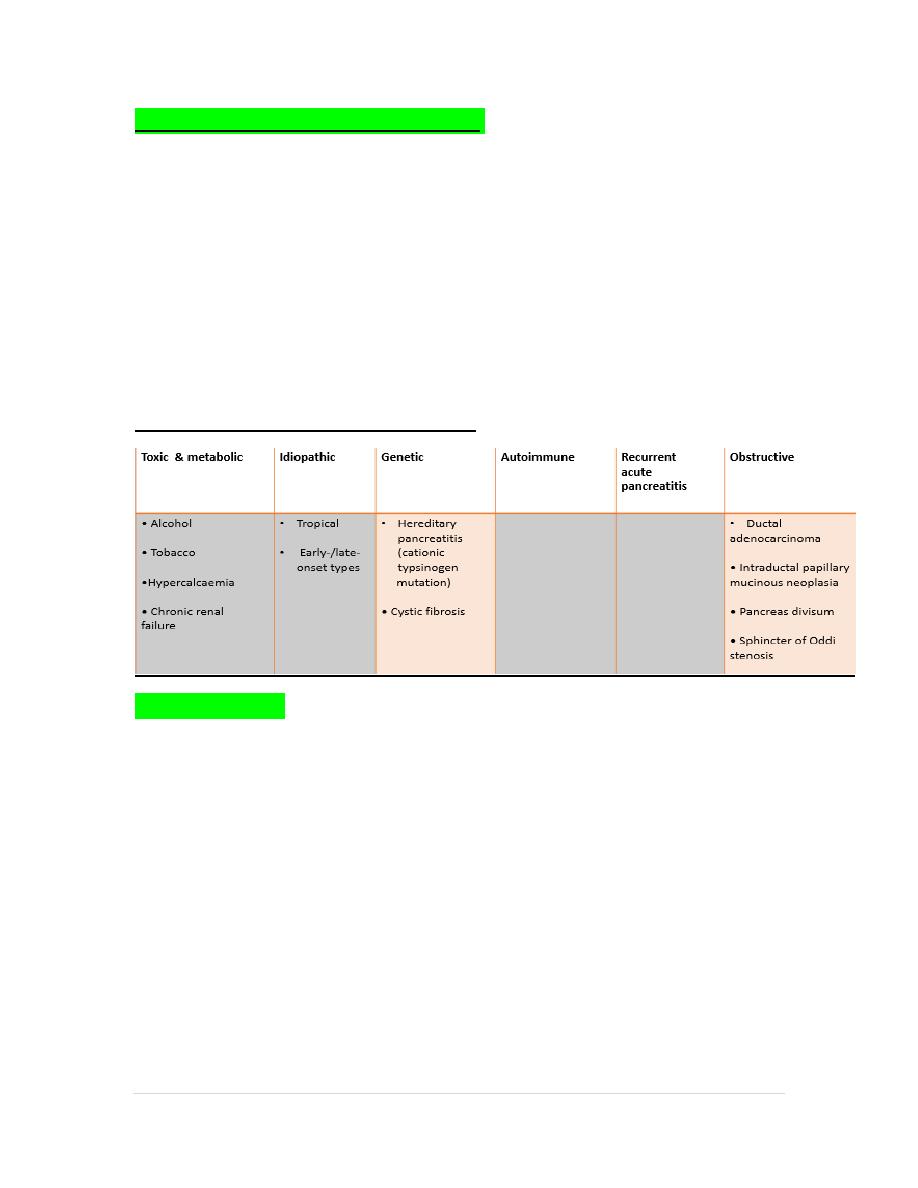
Causes of chronic pancreatitis: (tiger-o)
Clinical features :
Chronic upper abdominal pain, radiated to the back,
relieved by leaning forwards, drinking alcohol or opiate analgesics.
Weight loss, anorexia, steatorrhoea or diabetes.
Malnourished patient, skin pigmentation over the abdomen and back is
common and results from chronic use of a hot water bottle (erythema ab
igne).

11 |
P a g e
erythema ab igne
INVESTIGATION :
_
Imaging in chronic pancreatitis. A CT scan showing a
grossly dilated and irregular duct with a calcified stone (arrow A).
Note the
calcification in the head of the gland (arrow B). B MRCP of the same
patient showing marked ductal dilatation with abnormal dilated side
branches (arrows A). A small cyst is also present (arrow B).
_
Plain abdominal radiograph shows calcification in the pancreas
associated with osteomalacia secondary to malabsorption
Treatment :
1. Alcohol avoidance is essential, although some patients try to relieve pain
by drinking excessive alcohol which causes further pancreatic damages
2. Surgical procedures including partial pancreatic resection and
pancreatico-jejunostomy.
3. ERCP procedures: including dilatation and stent insertion of main
pancreatic duct and lithotripsy.
4. Medical treatment: Including enzyme replacement (exocrine function),
treatment of diabetes mellitus by insulin therapy and the most important is
pain reliving by giving different types of analgesics including narcotics
which may lead to drug addiction. Pain may be relieved some times by
giving oral pancreatic enzymes.. The medical treatment also includes
vitamins and mineral replacement and treatment of malabsorption.
5. Management of complications.
_
Key Points
The hallmark symptom of chronic pancreatitis is abdominal pain,
12 |
P a g e
often radiating to the back.
The common diagnostic criteria for chronic pancreatitis include
clinical features (pain, recurrent attacks of pancreatitis,
weight loss) with objective findings of calcifications, imaging features
of ductal dilatation or inflammatory masses, exocrine
pancreatic insufficiency, diabetes mellitus, and histologic findings.
Patients with chronic pancreatitis should be counseled to stop
smoking and drinking alcohol.
Gallstones
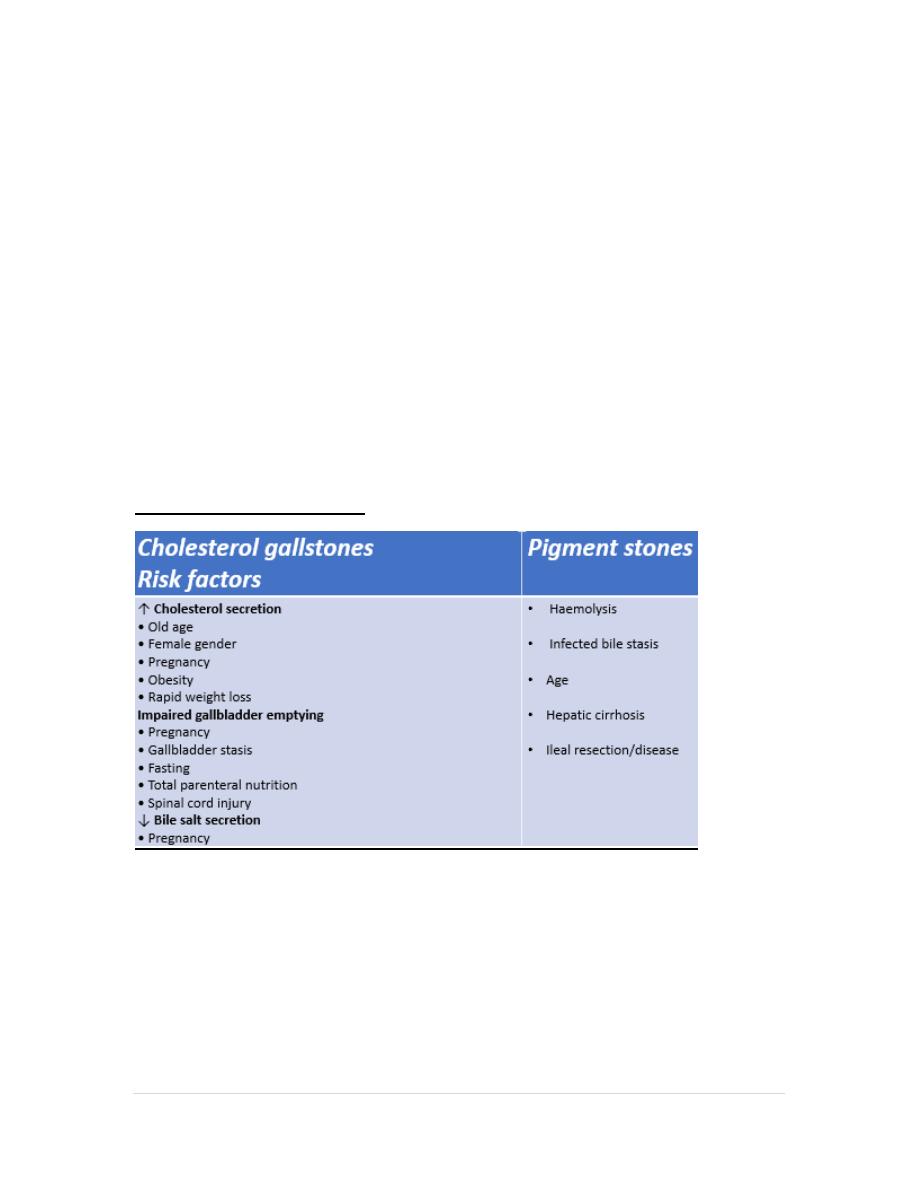
Gallstone formation is the most common disorder of the biliary tree and it
is unusual for the gallbladder to be diseased in the absence of gallstones, In
developed countries , gallstones occur in 7% of males and 15% of female
aged 18–65 years, with an overall prevalence of 11%.
Classification of gallstones
Clinical features and complications of gallstones :`
Clinical features
• Asymptomatic (80%)
• Biliary colic
• Acute cholecystitis
• Chronic cholecystitis

13 |
P a g e
Complications
• Empyema of the gallbladder • Porcelain gallbladder
• Choledocholithiasis • Acute pancreatitis
• Fistulae from gallbladder to duodenum/colon • Pressure
on/inflammation of the common bile duct by a gallstone in the cystic duct
(Mirizzi’s syndrome) • Gallstone ileus
• Cancer of the gallbladder
_
Investigation :
_
Ultrasound is the investigation of choice for diagnosing gallstones. Most
stones are diagnosed by transabdominal ultrasound, which has a greater
than 92% sensitivity and 99% specificity for gallbladder stones .
_
CT and MRCP are excellent modalities for detecting complications of
gallstones (distal bile duct stone or gallbladder empyema), but are
inferior to ultrasound in defining their presence in the gallbladder.
_
When recurrent attacks of otherwise unexplained acute pancreatitis
occur, this may result from ‘microlithiasis’ in the gallbladder or common
bile duct, and this is best assessed by endoscopic ultrasound (EUS).
Treatment :
Gallbladder stones
• Cholecystectomy: open or laparoscopic
• Oral bile acids: chenodeoxycholic or ursodeoxycholic (low
rate of stone dissolution)
Bile duct stones
• Lithotripsy (endoscopic or extracorporeal shock wave, ESWL)
• Endoscopic sphincterotomy and balloon trawl
• Surgical bile duct exploration
Key Points
Eighty percent of patients with asymptomatic gallstones remain
asymptomatic over a 15-year period, and most serious
complications of gallbladder stone disease are preceded by an episode of
biliary colic.
Cholecystectomy is not generally advised in asymptomatic patients with
gallstones.
14 |
P a g e
Cholecystitis (Acute cholecystitis):
clinical feature :
The cardinal feature is pain in the right upper quadrant but also in the
epigastrium, the right shoulder tip of the interscapular region.
Differentiation between biliary colic and acute cholecystitis may be difficult;
features suggesting cholecystitis include severe and prolonged pain, fever
and leucocytosis.
Examination shows right hypochondrial tenderness, rigidity worse on
inspiration (Murphy’s sign) and occasionally a gallbladder mass (30% of
cases). Fever is present but rigors are unusual. Jaundice occurs in less than
10% of patients and is usually due to passage of stones into the common
bile duct, or compression or even stricturing of the common bile duct
following stone impaction in the cystic duct (Mirizzi’s syndrome).
Gallbladder perforation occurs in 10–15% of cases, and gallbladder
empyema may arise.
Investigation :
Ultrasound is the investigation of choice for diagnosing gallstones. Most
stones are diagnosed by transabdominal ultrasound, which has a greater
than 92% sensitivity and 99% specificity for gallbladder stones .
CT and MRCP are excellent modalities for detecting complications of
gallstones (distal bile duct stone or gallbladder empyema), but are inferior
to ultrasound in defining their presence in the gallbladder.
When recurrent attacks of otherwise unexplained acute pancreatitis occur,
this may result from ‘microlithiasis’ in the gallbladder or common bile duct,
and this is best assessed by endoscopic ultrasound (EUS).
Treatment :
Medical
bed rest
pain relief
antibiotics and intravenous fluids
Moderate pain can be treated with NSAIDs but more severe pain should be
managed with
15 |
P a g e
opiates. A cephalosporin (such as cefuroxime) or piperacillin/tazobactam is
the usual antibiotic
of choice
Nasogastric aspiration is only needed for persistent vomiting.
Surgical
Urgent surgery is the optimal treatment when cholecystitis progresses in
spite of medical therapy and when complications such as empyema or
perforation develop.
Operation should be carried
out within 5 days of the onset of symptoms.
Key Point
§ Ninety percent of cases of acute cholecystitis occur in the setting of
obstruction of the cystic duct by gallstones.
§ Ultrasound is the diagnostic test of choice for gallbladder stones, and
findings include a thickened gallbladder wall and the
presence of pericholecystic fluid.
Acute cholangitis
is caused by bacterial infection of bile ducts and occurs in patients with
other biliary problems, such as choledocholithiasis (see below), biliary
stricture or tumours, or after ERCP. Jaundice, fever (with or without rigors)
and right upper quadrant pain are the main presenting features (‘Charcot’s
triad’).
Treatment
is with antibiotics, relief of biliary obstruction and removal (if possible) of
the underlying cause
