1
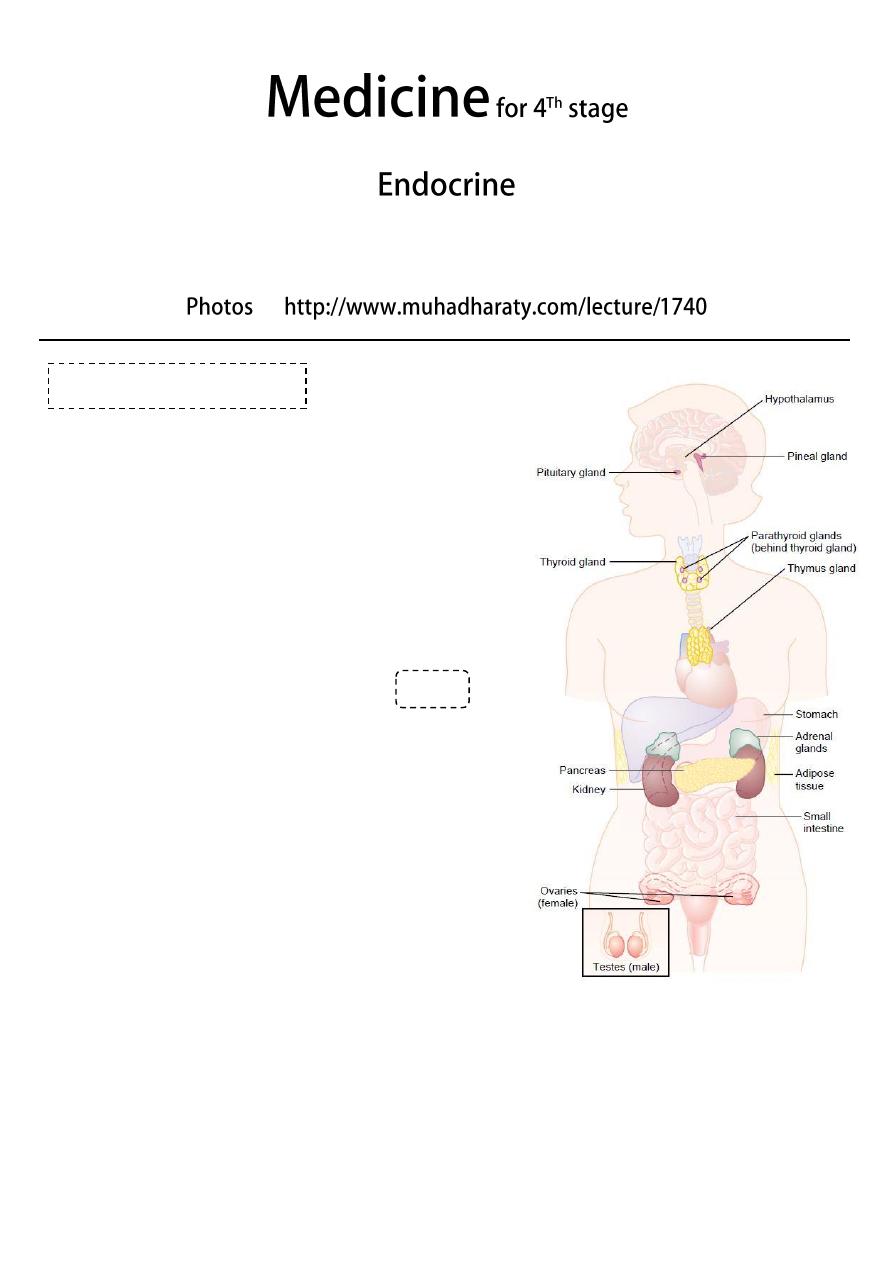
#Types of diseases of endocrine glands:
Increase secretion of hormones or increase
peripheral sensitivity to hormones.
Decrease secretion of hormones or increase
peripheral resistance to hormones.
Non-functioning tumor
lead to pressure effect
to surrounding structure and may lead to
decrease secretion of hormones.
#General endocrine examination:
Demeanour, mental state:
o Restless and agitated (hyperthyroidism).
o Slow and lethargic (hypothyroidism).
General appearance:
o Central obesity (Cushing’s syndrome)
Face:
o Features of Cushing’s syndrome, Addison’s
disease, and Acromegaly.
o Inspect the face and eyes for a 'spot'
endocrine diagnosis.
Eyes:
o Look for features of thyroid disease.
o Assess visual acuity and perform fundoscopy in patients with diabetes mellitus.
o Assess visual acuities and fields in patients with suspected pituitary tumors.
o Bitemporal hemianopia (due to compression of the optic chiasm by pituitary
tumor)
o Optic atrophy (longstanding optic pathway compression)
o Exophthalmos and Ophthalmoplegia.
General endocrine
لإلطالع

2
Mouth:
o Overgrowth of the chin and tongue (acromegaly)
o Buccal pigmentation (Addison's disease).
Neck:
o Examine the neck for goiter. If present, record its size, surface and consistency.
Hand:
o Tremor and palmar sweating (hyperthyroidism)
o Soft-tissue overgrowth (acromegaly)
o Large, sweaty, fleshy (acromegaly)
o Dysmorphism is abnormal metacarpal length (pseudohypoparathyroidism)
o Skin crease pigmentation (Addison's disease)
o Wasting of the thenar muscles due to carpal tunnel syndrome (hypothyroidism,
acromegaly).
o Palmar erythema.
Breast:
o Gynecomastia (Klinefelter's syndrome, galactorrhoea)
Chest:
o Look for a thoracic kyphosis, which may be a sign of osteoporotic vertebral
collapse.
Abdomen:
o Purple striae (Cushing's syndrome)
o Palpable, nodular liver, which is sometimes massively enlarged (Carcinoid
syndrome)
External genitalia:
o Inspect the amount of pubic hair and make a pubertal staging of all adolescents
using Tanner grading.
o In men, record testicular size and consistency.
o In women, look for virilising features.
Legs:
o Pretibial myxedema (Graves 'disease)
o Proximal muscle wasting or weakness (Cushing's syndrome and hyperthyroidism)
o Delayed tendon reflexes (hypothyroidism)
o Signs of diabetic neuropathy, ischemia, ulcers (diabetes mellitus)
o Pretibial myxedema, Necrobiosis lipoidica.
Skin surface:
o Abnormal pallor (hypopituitarism)
o Vitiligo, skin or scar pigmentation (Addison's disease)
o Plethora (Cushing's or carcinoid syndrome)
o thin, fragile skin with bruising after trivial trauma (Cushing's syndrome)
o Acanthosis nigricans in axilla and groin (obesity, diabetes mellitus)
Body hair:
o Is the body hair normal in quality and amount?
o Hirsutism in females (polycystic ovary syndrome)
o Loss of hair in the axillae and groins (hypopituitarism)
3
Bone:
o Osteoporosis (hyperthyroidism, Cushing’s syndrome, hypogonadism {loss of height,
thoracic kyphosis})
Pulse:
o Assess the pulse rate, rhythm and volume.
o Tachycardia and atrial fibrillation (thyrotoxicosis)
Blood pressure:
o Hypertension (Cushing's syndrome, Phaeochromocytoma, Conn's syndrome)
o Postural hypotension (adrenal insufficiency)
Measure the height and weight and calculate the body mass index:
o Use a stadiometer in children and adolescents.
o If the patient is obese, is the adiposity centrally distributed, e.g. Cushing's
syndrome or GH deficiency.
Urine:
o Test the urine for glucose, ketones, protein and nitrite.
Psychological:
o Formal psychological evaluation may be appropriate in selected patients (Cushing's
syndrome, hyperparathyroidism).
#Growth hormone (G.H) change diseases:
Decrease G.H secretion before puberty Dwarfism treated by giving G.H
injection for 6 weeks or more if the child less than 10 years old.
Decrease G.H secretion after puberty Lethargy.
Increase G.H secretion before puberty Gigantism.
Increase G.H secretion after puberty Acromegaly (Acro means periphery).
Presenting features of acromegaly:
o Early: Shoes, cloths, rings become smaller / bone pain / large periphery like nose,
forehead, lips, tongue, limbs, heart.
o Late: Pale, dizzy due to hypo-pituitarism which occur due to pressure effect of
macro-adenoma that secret G.H.
o Face: coarsening of features, thick greasy skin, enlargement of the nose,
prognathism (protrusion of the mandible) and separation of the lower teeth.
o Hands and feet: tight-fitting rings or shoes, carpal tunnel syndrome.
o Eye: bitemporal hemianopia.
o Hypertension and diabetes mellitus are common associations.
#Examination of patient with Hypopituitarism:
Anterior hypopituitarism is due to compression of the pituitary by a
macroadenoma, infarction after childbirth (Sheehan’s syndrome), severe head trauma,
cranial radiotherapy.
Pituitary gland
4
Extreme skin pallor a combination of mild anemia and melanocyte-stimulating
hormone deficiency.
Absent axillary hair.
Reduced/absent secondary sexual hair caused by gonadotrophin deficiency.
T
esticular atrophy.
Examine the eyes for
o Visual field defects (most often bitemporal hemianopia).
o Optic atrophy or cranial nerve defects (III, IV and VI) caused by a tumor
compressing the optic chiasm, optic nerve or cavernous sinus.
#Non- functioning tumor in pituitary gland:
Lead to pressure effect on the pituitary gland.
So decrease the secretion of some hormones start from least important to most
important First is LH + FSH G.H TSH ACTH.
Start treatment by replacement the most important hormone at first which is ACTH
then TSH then LH + FSH and if needed you can replace G.H.
Don't give thyroxin unless there is adequate level of hydrocortisone in the body
because if you give thyroxin with absence of cortisol there will be crisis. If you not
sure about the level of cortisol you can give both thyroxin + hydrocortisone.
Lead to pressure effect on optic chiasma lead to Bitemporal hemiplegia.
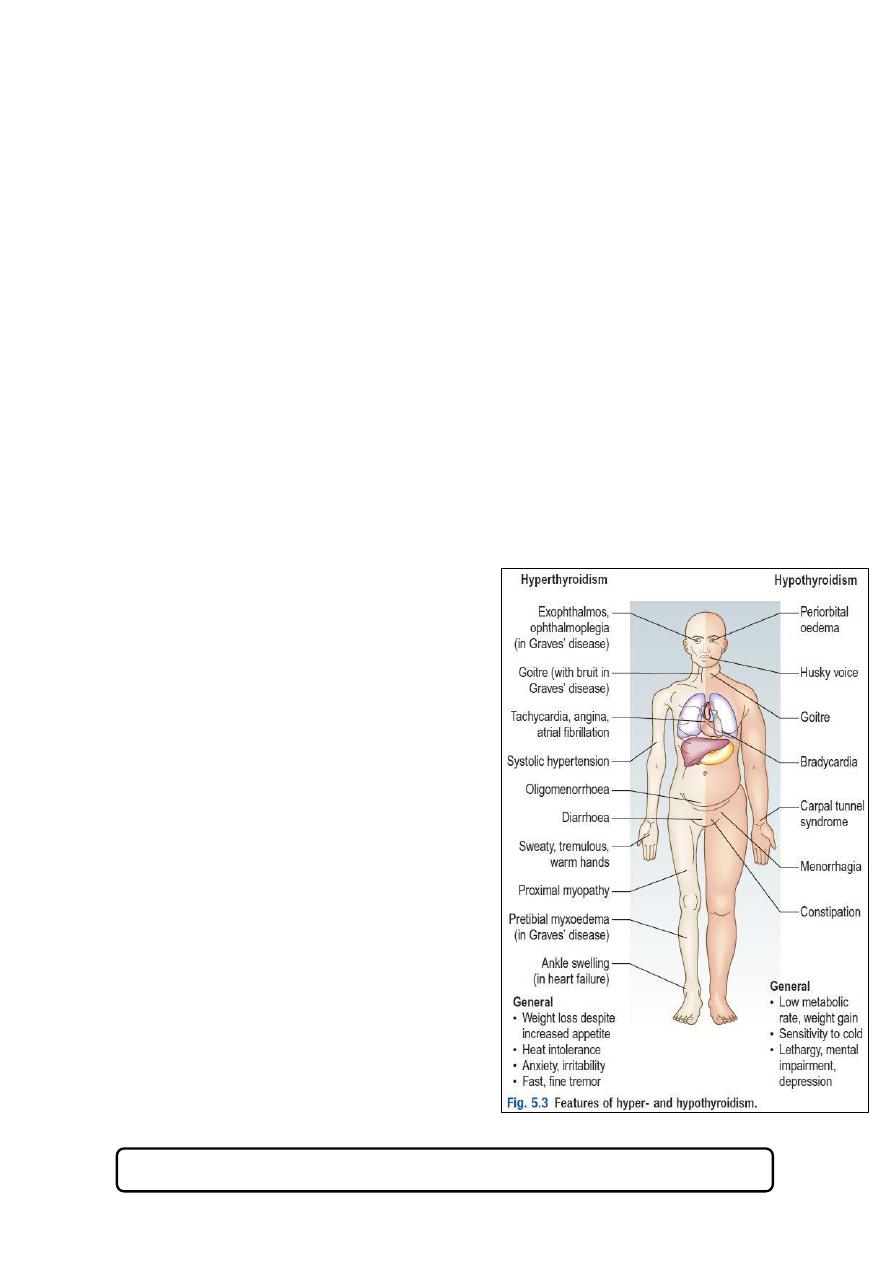
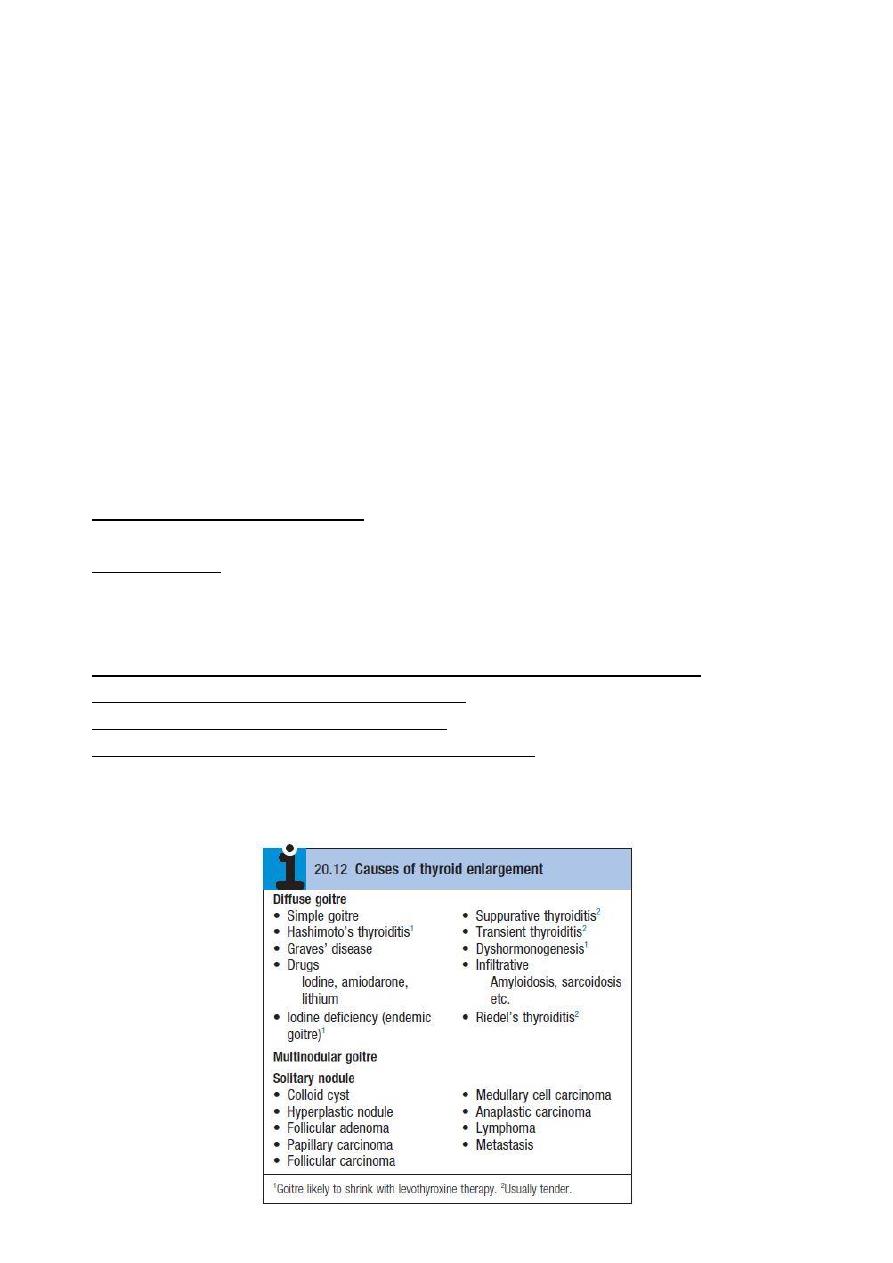
#Diseases of the thyroid gland:
Goiter is enlargement of the thyroid gland.
Hyperthyroidism (thyrotoxicosis) is a clinical state caused by increased levels of
circulating levels of the thyroid hormones, T3 and T4. Graves’ disease is the
commonest cause of hyperthyroidism.
Hypothyroidism is caused by reduced levels of thyroid hormones and is usually due to
autoimmune Hashimoto’s thyroiditis.
#Specific extra-thyroid features of Hyperthyroidism (thyrotoxicosis):
Exophthalmos (proptosis):
o It is increased protrusion of the eyeball from the orbit.
o It is caused by an inflammatory infiltration of the orbital contents (the soft tissues
and extra-ocular muscles, not the globe).
o It is usually bilateral.
Pretibial myxedema: Is a raised, discolored (usually pink or brown) indurated
appearance over the lower legs. It is associated with Graves’ disease, not
hypothyroidism.
Thyroid acropachy: is a periosteal hypertrophy of the distal phalanges which looks like
finger clubbing.
Thyroid gland
5
#Function of cortisol:
Maintain vascular changes in posture changes and other condition (hypo/hyper
tension).
Maintain sugar level in the blood.
#The counteracting hormones:
They are the hormones that counter act the function of insulin.
They increase the level of glucose in blood (energy).
They are the following thyroxin, glucagon, hydrocortisone, adrenaline, nor-
adrenaline.
#Notes on thyroid hormones:
Functions of them: give energy to the body + differentiation of cells.
99% of thyroid hormone are bound to thyroxin binding globulin (TBG).
The diagnosis of hyper or hypo thyrodisim is made by biochemical tools.
Primary Hypothyroidism TSH: ↑, Free T3 and free T4: ↓
Secondary Hypothyroidism TSH: ↓ or ↔, Free T3 and free T4: ↓
Hyperthyroidism TSH: ↓, Free T3 and free T4: ↑
#Causes of thyrotoxicosis:
Graves’ disease, Multinodular goiter, Solitary
thyroid adenoma, Thyroiditis.
Iodide-induced: Drugs (amiodarone),
Radiographic contrast media, Iodine
prophylaxis programme.
Extrathyroidal source of thyroid hormone:
Factitious thyrotoxicosis, Struma ovarii.
TSH-induced, TSH-secreting pituitary
adenoma, Follicular carcinoma ± metastases.
#Causes of hypothyroidism:
Autoimmune: Hashimoto’s thyroiditis,
Graves’ disease.
Iatrogenic: Radioactive iodine ablation,
Thyroidectomy, Drugs (Carbimazole).
Iodine deficiency: in mountainous regions.
Congenital: Thyroid aplasia and Infiltrative:
Amyloidosis, sarcoidosis.
Secondary hypothyroidism: TSH deficiency.
See this video http://www.muhadharaty.com/lecture/1198
6
#Examination of patient with thyroid gland diseases:
1- General:
Look for:
o Signs of weight loss or gain.
o Agitation, restlessness or apathy and lethargy.
o The facial appearance and expression.
Examine:
o Hands
o Pulse and blood pressure (BP)
o Arms and legs for: skin abnormalities, muscle power and the deep tendon reflexes.
o The eyes for:
Exophthalmos, diplopia, conjunctival edema or conjunctivitis, corneal ulceration.
Lid retraction: this is present if the sclera is visible above the iris.
Lid lag: ask the patient to follow your index finger as you move it from the upper
to the lower part of his visual field. Delay between the descent of the upper
eyelid in relation to that of the eyeball is lid lag.
2- Thyroid:
Inspect the neck from the front: Give the patient a glass of water and ask him to take a
sip. Look for a swelling while he swallows.
Ask the patient to sit with the neck muscles relaxed and stand behind him. Place your
hands gently on the front of the neck, with your index fingers just touching. Ask him to
swallow a sip of water and feel the gland as it moves upwards. Some patients find neck
palpation uncomfortable, so be alert for any signs of distress.
Note the size, shape and consistency of any goiter and feel for any thrill.
Measure any discrete nodules with callipers.
Record the maximum neck circumference of a large goiter using a tape measure.
Auscultate with your stethoscope for a thyroid bruit. A thyroid bruit may be confused
with other sounds: bruits from the carotid artery or transmitted from the aorta are
louder along the line of the artery. Transient gentle pressure over the root of the neck
will interrupt a venous hum from the internal jugular vein.
7
#Adrenal gland diseases:
Increase medulla hormones secretion (adrenals) Phaeochromocytoma.
Increase cortex hormone secretion (cortisol) Cushing's syndrome.
Decrease cortex hormone secretion (cortisol) Primary Addison's disease.
Increase cortex hormone secretion (aldosterone) Conn's syndrome also called
primary hyperaldosteronisim, features:
o Hypertension refractory to treatment, or in young patient.
o Hypokalemic alkalosis (because the renal tubules will excrete hydrogen and
absorb sodium).
Cushing's syndrome caused by excess exogenous or endogenous corticosteroid
exposure like: iatrogenic, ACTH-secreting pituitary microadenoma, primary adrenal
tumor, ectopic ACTH secretion.
Addison’s disease due to inadequate secretion of cortisol, usually secondary to
autoimmune destruction of the adrenal cortex.
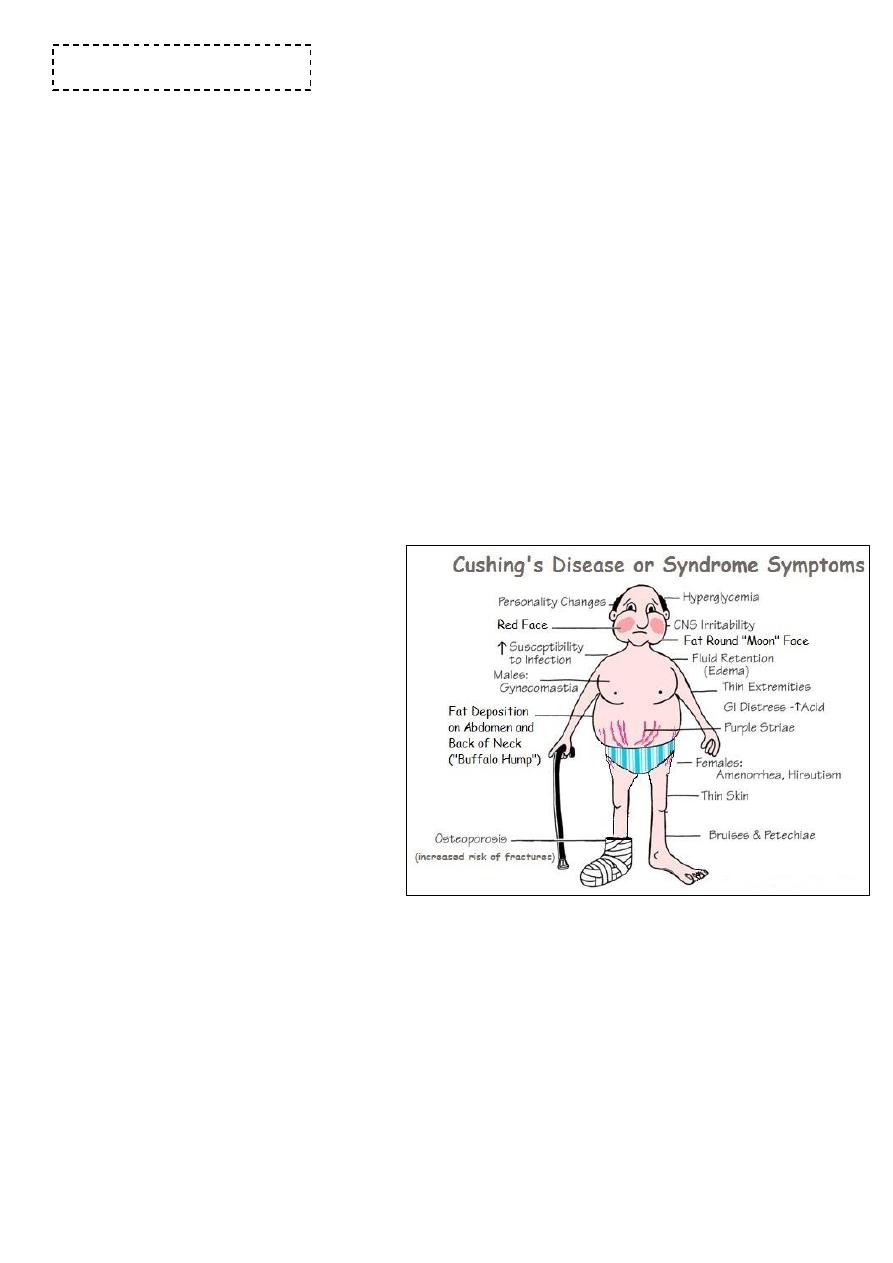
#Examination of patient with Cushing's syndrome:
Look at the face and general
appearance for central obesity
and a round face.
Examine the skin for thinning,
hyperpigmentation, acne,
hirsutism, bruising, striae
(especially abdominal) and signs of
infection or poor wound healing.
Examine the legs for evidence
of proximal muscle weakness and
edema.
Examine the eyes for cataracts,
and hypertensive changes.
Check the BP.
Perform urinalysis.
#Examination of patient with Addison’s disease:
Look for signs of weight loss.
Examine the entire skin surface for
o Abnormal or excessive pigmentation: this is most prominent in sun-exposed areas
or epithelia subject to trauma or pressure – skin creases, buccal mucosa and recent
scars.
o Excess pigmentation is produced by melanocyte-stimulating hormone in primary
adrenal insufficiency. It is most striking in white Europeans.
Adrenal gland
8
o Vitiligo (depigmentation of areas of skin) occurs in 10–20% of Addison's disease
cases.
Check the BP and test for postural hypotension Hypotension and postural
hypotension result from reduced mineralocorticoid effects.
#Secondary Addison's disease:
Decrease in the ACTH or adrenal hormone, due to extra-adrenal cause like tumor in
the pituitary gland and other diseases.
Lead to postural hypotension.
Hypoglycemic attack (palpitation, confusion, convulsion, coma, others).
Hepatic failure.
Lethargy and other non-specific features.
Decrease in aldosterone (hypotension, hyperkalemic alkalosis)
In primary Addison's disease there is color change but in secondary there is no color
change in the patient the cause of color changes is there is pro-hormone which
divided into two component, one of them is ACTH and the other is melanocyte
stimulating hormone which change the color of the body into darker color.
#Diabetic foot:
Diabetic patients have a 15% lifetime risk of foot ulcers, which are highly susceptible to
infection. Early recognition of the 'at-risk' diabetic foot is essential. There are two main
presentations:
Neuropathic: where neuropathy predominates but the major arterial supply is intact.
Neuro-ischemic: where reduced arterial supply produces ischemia and exacerbates
neuropathy.
Infection complicates both presentations.
#Examination of diabetic foot:
Inspection:
o Look for hair loss and nail dystrophy.
o Examine the skin (including the interdigital clefts) for excessive callus, infections
and ulcers.
o Ask the patient to stand and assess the foot arch.
o Look for deformation of the joints of the feet.
Palpation:
o Feel the temperature of the feet.
o Examine the dorsalis pedis and posterior tibial pulses. If absent, arrange Doppler
studies to evaluate ankle brachial pressure index.
Test for peripheral neuropathy: use a nylon monofilament which buckles at a force of
10 g to apply a standard, reproducible stimulus. Avoid areas of untreated callus.
Abnormal findings Hair loss, nail dystrophy, athlete’s foot, rocker-bottom sole,
warm feet occur in neuropathy and cold feet in ischemia, Sensory neuropathy,
Charcot’s arthropathy.
Pancreas
