ESOPHAGEAL CARCINOMA
There are two types: squamous cell carcinomas and adenocarinomas. Worldwide, squamous cell carcinomas constitute 90% of esophageal cancers.Adenocarcinoma arising in Barrett esophagus is more common in whites than in blacks. By contrast, squamous cell carcinomas are more common in blacks worldwide. There are striking and puzzling differences in the geographic incidence of esophageal carcinoma.
Esophageal carcinoma (squamous cell type), females being affected more often than males.More common in Asian than UnitedState.
Risk factors for SCCof the esophagus
Esophageal DisordersLong-standing esophagitis, Achalasia, Plummer-Vinson syndrome (esophageal webs, microcytic hypochromic anemia, atrophic g]ossitis)
Life Style
Alcohol consumption
,Tobacco abuse,
Dietary
Deficiency of vitamins (A, C, riboflavin, thiamine, pyridoxine)
Deficiency of trace metals (zinc, molybdenum)
Fungal contamination of foodstuffs
High content of nitrites/nitrosamines
Genetic Pedisposition
Tylosis: in which there is hyperkeratosis of palms and soles
There is a link between mentioned risk factors and molecular changes;
* mutation of tumor suppressor gene P53
* mutation of k- RAS gene.
MORPHOLOGY
Squamous cell carcinomas are usually preceded by mucosal epithelial dysplasia followed by carcinoma in situ and, ultimately, by the emergence of invasive cancer, taking one of three forms:
(1) polypoid exophytic masses that protrude into the lumen;
(2) necrotizing cancerous ulcerations that extend deeply and sometimes erode into the respiratory tree, aorta, or elsewhere and
(3) diffuse infiltrative neoplasms that impart thickening and rigidity to the wall and narrowing of the lumen.
Whichever the pattern, about 20% arise in the cervical and upper thoracic esophagus, 50% in the middle third, and 30% in the lower third.
Adenocarcinomas appear to arise from dysplastic mucosa in the setting of Barrett esophagus. Unlike squamous cell carcinomas, they are usually in the distal one third of the esophagus and may invade the subjacent gastric cardia.
Microscopically, most tumors are mucin-producing glandular tumors exhibiting intestinal-type features, in keeping with the morphology of the preexisting metaplastic mucosa.
Clinical Features.
Esophageal carcinoma is insidious in onset and produces dysphagia and obstruction gradually and late. Weight loss, anorexia, fatigue, and weakness appear, followed by pain, usually related to swallowing.Diagnosis
is usually made by imaging techniques and endoscopic biopsy. Because these cancers extensively invade the rich esophageal lymphatic network and adjacent structures, surgical excision rarely is curative
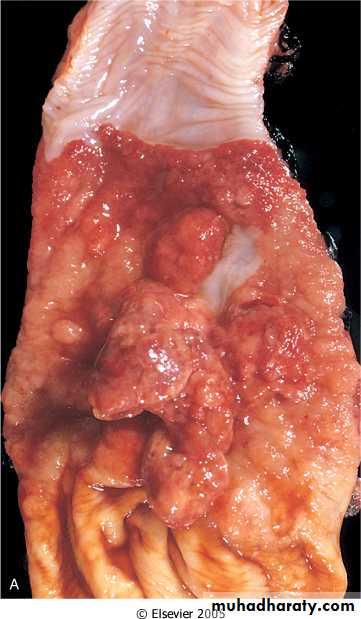
Large utcerared squamous cell carcinoma of the esophagus.
Stomach pathology
Intended Learning OutcomesBy the end of this lecture the student should know :
• 1- The congenital disorders of the stomach
• 2- Acute stomach inflammation and stress ulcers
3- Chronic Gastritis and its types
4- Chronic peptic ulcers and associated types
5- Gastric Carcinoma
ANATOMY OF STOMACH
StomachGastric disorders give rise to symptoms similar to esophageal disorders, primarily heartburn and vague epigastric pain. With breach of the gastric mucosa and bleeding, hematemesis or Melena may ensue.
Unlike esophageal bleeding, however, blood quickly congeals and turns brown.
CONGENITAL DISORDERS OF STOMACH
• 1. Pyloric stenosis:
Congenital stenosis of pylorus due to marked muscular hypertrophy of the pyloric sphincter, resulting in gastric outlet obstruction
• 2. Congenital Diaphragmatic hernia:
Congenital defect in the diaphragm, resulting in herniation of the abdominal organs into the thoracic cavityThe stomach is the most commonly herniated organ
GASTRITIS
Acute Gastritis Acute gastritis is an acute mucosal inflammatory process, usually of a transient nature. The inflammation may be accompanied by hemorrhage into the mucosa and, in more severe circumstances, by sloughing of the superficial mucosal epithelium (erosion). This severe erosive form of the disease is an important cause of acute gastrointestinal bleeding.Acute gastritis is frequently associated with the following:
• Heavy use of nonsteroidal anti-inflammatory drugs (NSAIDs), particularly aspirin.
• Excessive alcohol consumption
• Heavy smoking
• Treatment with cancer chemotherapeutic drugs
• Uremia
• Severe stress (e.g., trauma, burns, surgery)
ACUTE GASTRIC ULCERATION
Focal, acutely developing gastric mucosal defects are a well-known complication of therapy with NSAIDs. They may also appear after severe physiologic stress. Some of these are given specific names, based on location and clinical associations. For example:• Stress ulcers are most common in individuals with shock, sepsis, or severe trauma.
• Ulcers occurring in the proximal duodenum and associated with severe burns or trauma are called Curling ulcers.
• Gastric, duodenal, and esophageal ulcers arising in persons with intracranial disease are termed Cushing ulcers and carry a high incidence of perforation
Chronic Gastritis
Presence of chronic mucosal inflammation leading eventually to mucosal atrophy and epithelial metaplasia.
Pathogenesis:
A- Most important etiology is H.pylori chronic infection in areas where the infection is endemic
H. pylori is a noninvasive, non—spore forming, S-shaped gram-negative rod.
gastritis develops owing to the:
1- combined influence of bacterial enzymes and toxins ,
2- release of noxious chemicals by the recruited neutrophils.
Patients with chronic gastritis and H. pylori usually improve symptomatically when treated with antimicrobial agents.
B- Other forms of chronic gastritis are much less common is autoimmune gastritis, which results from autoantibodies to the gastric gland parietal cells. The autoimmune injury leads to gland destruction and mucosal atrophy, with concomitant loss of acid and intrinsic factor production. The resultant deficiency of intrinsic factor leads to pernicious anemia
A- Fundic type (Type A):
This is an autoimmune diseaseThere is decreased acidic secretion.
It usually involves the body and the fundus of stomach
B- Antral type (type B):
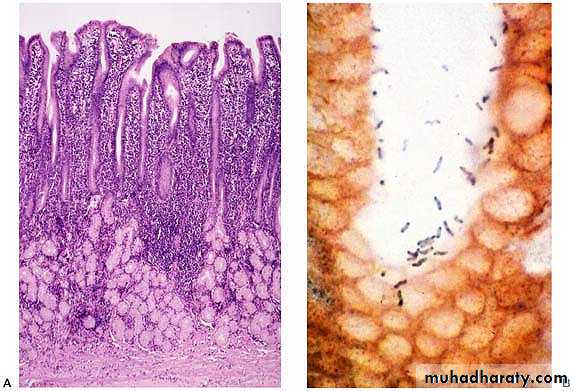
This type is commonly related to Helicobacter pyloriMicroscopic picture:
H- pylori organisms are visible in the mucous layer of the surface epitheliumFoci of acute inflammation
Chronic inflammation with lymphoid follicles
Intestinal metaplasia
Complication:
Increased risk of gastric carcinoma
MORPHOLOGY
Gross picture:Loss of rugal folds in the body and fundus
Microscopic picture:
Regardless of the cause or histologic distribution of chronic gastritis, the inflammatory Changes consist of:
1- a lymphocytic and plasma cell infiltrate in the lamina propria.
2- variable gland loss and mucosal atrophy.
3- When present H.pylori organisms are found nestled within the mucus layer overlying the superficial mucosal epithelium.
4- In the autoimmune variant, loss of parietal cells is particularly prominent.
5- Two additional features are of note, 1st Intestinal metaplasia refers to the replacement of gastric epithelium with columnar and goblet cells of intestinal variety. This is significant, because gastrointestinal-type carcinomas appear to arise from dysplasia of this metaplastic epithelium. Second, H. pylori induced proliferation of lymphoid tissue within the gastric mucosa has been implicated as a precursor of gastric lymphoma.
When severe parietal cell loss occurs in the setting of autoimmune gastritis, hypochlorhydria or achlorhydria occur.
Most important is the relationship of chronic gastritis to the development of peptic ulcer and gastric carcinoma,
Most patients with a peptic ulcer, whether duodenal or gastric, have H. pylori infection.
For autoimmune gastritis, the risk for cancer is in the range of 2% to 4% of affected individuals, which is well above that of the normal population.
Helicobacter pylori gastritis. A Steiner silver stain demonstrates the numerous darkly stained organisms along the luminal surface of the gastric epithelial cells. Note that there is no tissue invasion by bacteria
CHRONIC PEPTIC ULCER (BENIGN ULCER)
Peptic ulcerDefinition:
Ulcers of the distal part of stomach and proximal part of duodenum caused by gastric secretions (hydrochloric acid and pepsin) and impaired mucosal defenses
Etiology:
Chronic NSAID and aspirin useSteroids
Smoking
H.pylori
Complications:
Haemorrhage ( Haematemesis & melena)Iron deficiency anaemia
Gastric perforation
Pyloric obstruction
Duodenal peptic ulcer:
It is more common than gastric ulcersEitiology:
H.pylori
Increased gastric acid secretion
Increased rate of gastric emptying
Blood group O
Cirrhosis & COPD
Grossly (Location of Duodenal Ulcer:
It is located at the anterior wall of the proximal duodenumClinical presentation:
Burning epigastric pain 1-3 hours after eating and usually relieved by foodDuodenal ulcer. There are two sharply demarcated duodenal ulcers surrounded by inflamed duodenal mucosa. The gastroduodenal junction is in the midportion of the photograph
Gastric peptic ulcer:
Associated with H.pylori (75%)Location: lesser curvature of the antrum
Clinical presentation:
Burning epigastric pain, which worsens with eating?Grossly:
Small (<3cm), solitary ulcerRound or oval shape
Sharply demarcated " punched out" ulcers
Overhanging margins
Radiating mucosal folds