1
Bronchogenic Carcinoma
Introduction
• Lung cancer is the most common cancer world-wide, accounting for1.2 million new
cases annually in 2000 and causing 18% of all cancer deaths.
• The incidence of bronchial carcinoma increased dramatically during the 20th century.
In women, smoking prevalence and deaths from lung cancer continue to increase.
Risk factors :
▪ 1-Smoking: is by far the most important cause of lung cancer., for at least 90 being
proportional to the amount smoked and to the tar content of cigarettes. • The death
rate from the disease in heavy smokers is 40 times that in non-smokers. Risk falls
slowly after smoking cessation, but remains above that in non-smokers for many
years Exposure to naturally occurring radon is another risk. The incidence of lung
cancer is slightly higher in urban than in rural dwellers. which may reflect differences
in atmospheric
▪ 2-Radon,cadmium and arsenic exposure.
▪ 3-Asbestosis .
▪ 4-Air pollution.
▪ 5-Genetic.

2
Histologic classifications:-
1- SCLC
▪ 20%
▪ Includes :-oat cell carcinoma/intermediate /combined
2-NSCLC :-75-80%
▪ Adenocarcinoma:50%
▪ SCC:-30%
▪ Large cell carcinoma 15%
Symptoms
1. Cough is the most common early symptom.
2. Haemoptysis occurs especially in central tumours.
3. Bronchial obstruction may cause breathlessness ,stridor, lung collapse and
pneumonia.
4. Breathlessness reflect development of a large pleural effusion.
5. Pleural pain results from invasion of The pleura.
6. Horner's syndrome ( ipsilateral ptosis , enophthalmos, a small pupil and hypohidrosis
of the face ) is caused by involvement of the sympathetic chain.
7. Dysphagia result from mediastinal spread.
8. symptoms result from blood- borne metastases are focal neurological defects,
epileptic seizures, jaundice or bone pain
9. lassitude, anorexia and weight loss result from the presence of metastatic spread.
10. pancoast’s syndrome :-destruction of C8-T1
11. shoulder pain, arm atrophy .
Signs
▪ Old age.
▪ Cachexic (in late stage).

3
▪ Percussion:-dullness.
▪ LAP (scalene LN).
▪ Hoarsness of voice.
▪ Horner syndrome:-ptosis ,anhidrosis.
▪ Hypertrophic pulmonary osteoarthropathy and finger clubbing (softening of nail beds
with enlargement of finger tips).
▪ Sign of chronic hypoxia.
▪ Reduced chest expansion .
Patterns of spread
▪ Direct spread To pleura , Pericardium and others.
▪ Blood born:-to Liver, bone ,adrenal and brain.
▪ Lymphatic spread to the hilar ,trachiobronchial , mediastinal supraclavicular lymph
nodes leading to enlargment of the lymph node ( lymphadenopathy)
DIAGNOSIS
A complete history is taken and a physical examination is performed, with particular
attention to possible manifestation of the primary tumor.
INVESTIGATIONS
the main aim of investigations are to confirm the diagnosis, establish the histological cell
type and define the extent of the disease.
I- CHEST X- RAY:
1. Normal CXR when the tumor is small (1%).
2. Solitary pulmonary nodule-large circumscribed mass- Multiple nodular lesions.
3. obstructive emphysema: partial obstruction of bronchus resulting in obstructive
emphysema and inadequate drainage .
4. Atelectasis: due to complete bronchial obstruction.

4
5. Unresolved pneumonia: lung distal to lobar blockage not collapse…..but secretions
accumulate.
6. Cavity lesion: distal to obstructive pneumonia or ischemic necrosis within the tumor.
7. Unilateral or bilateral hilar enlargement.
8. Apical or subapical lesions: usually superior sulcus tumor.
9. pleural effusion – pericardial effusion.
10. Elevation of the diaphragm.
11. Pleural mass without rib destructions.
II- CT Scan:
▪ (A negative CT scan does not exclude the presence of carcinoma)
▪ The evaluation of the primary tumor.
▪ The assessment of regional lymph node enlargement.
▪ The detection of satellite nodules or mediastinal metastases.
III- Bronchoscopy:
▪ Three -quarters of primary lung tumors can be visualized and sampled directly by
biopsy and
▪ brushing using a flexible bronchoscope.
IV. Percutaneous needle biopsy under CT or ultrasound guidance:
more reliable way to obtain a histological diagnosis for tumors which are too peripheral.
V- Sputum cytology:
Not routine due to low yield, sometimes used if patient is unfit for bronchoscopy.
VI-Pleural aspiration (+ / -) biopsy:
indicated in all patients with a pleural effusion ,blind needle or radiologically guided
pleural biopsy is performed

5
VII- Mediastinoscopy:
surgical procedure under GA.required for staging prior to lung resection,can also be used in
difficult cases where other investigations have not led to a diagnosis.
VIII- Thoracoscopy:
allows direct visualization of the pleura..maybe required if pleural aspiration and biopsy are
negative
Positron emission tomography (PET) scanning
▪ specialized imaging technique that uses short-lived radioactive drugs to produce
three-dimensional colored images of those drugs in the tissues within the body.
▪ PET scans can determine whether a tumor tissue is actively growing and can aid in
determining the type of cells within a particular tumor.
A Pet scan detects elevated radiolabelled glucose metabolism in areas affected by tumor
and can be used prior to surgery (or radical radiotherapy) to detect unsuspected metastatic
disease. Small cell lung cancer tends to metastasise early, therefore patients with this
tumor are not suitable for surgical intervention.
Head CT, radionuclide bone scanning ,liver USS and bone marrow biopsy are reserved for
patients with clinical , hematological or biochemical evidence of tumor spread to such
sites.
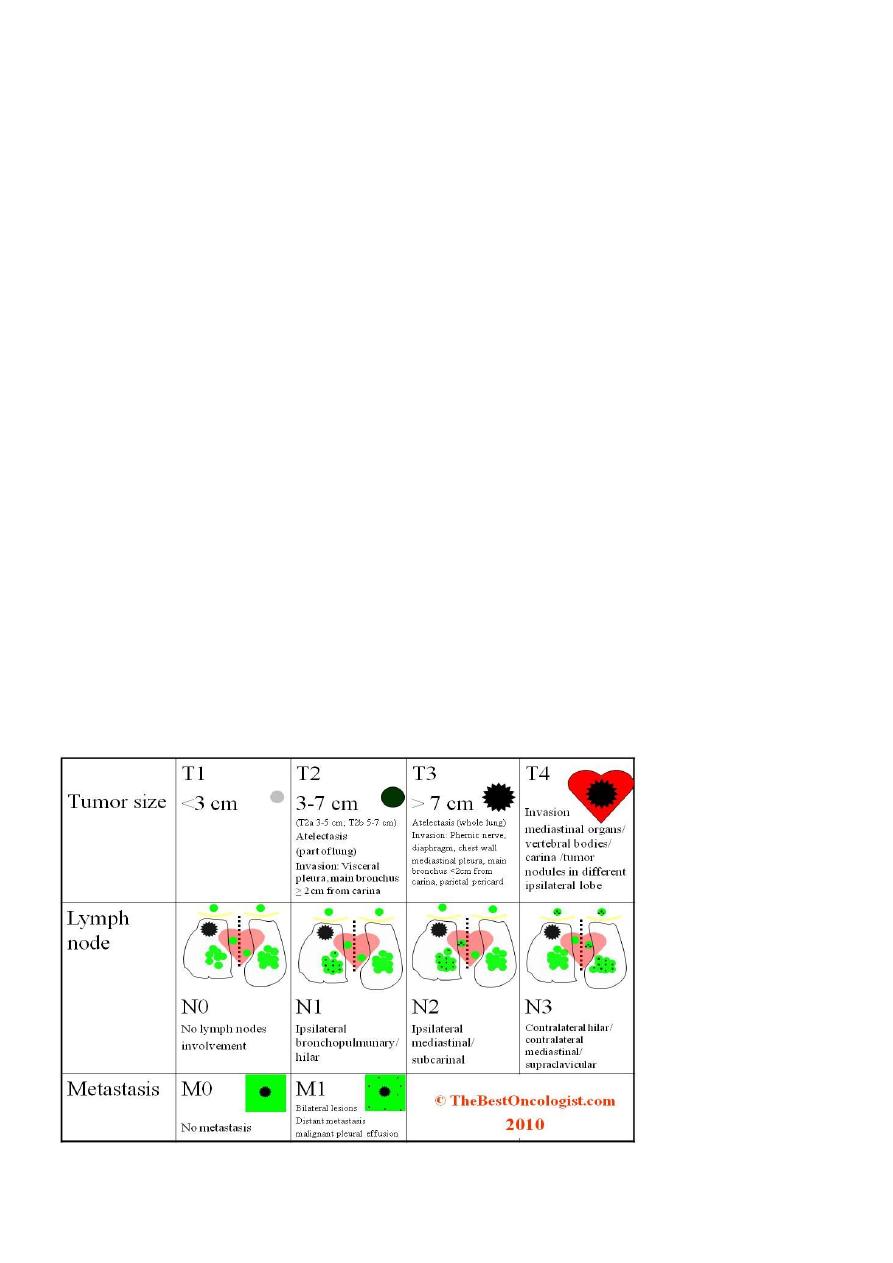
STAGING OF BRONCHOGENIC CARCINOMA
International TNM Staging system for Lung Cancer
Tumor (T)
TX Occult carcinoma (malignant cells in sputum or bronchial washing
But tumor not visualized by imaging studies or bronchoscopy)
T1 Tumor 3 cm or less in greatest diameter,surrounded by lung or
Visceral pleura,but not proximal to a lobar bronchus
T2 Tumor >3 cm.in diameter,or with involvement of main bronchus
At least 2 cm. distal to carina, or with visceral pleural invasion, or
With assosciated atelectasis or obstructive pneumonitis extending
6
To hilar region but not involving the entire lung
T3 Tumor invading chest wall,diaphragm,mediastinal pleura, or parietal
Pericardium, or tumor in main bronchus within 2 cm. of, but not
invading carina , or atelectasis of obstructive pneumonitis of the
entire
lung
T4 Tumor invading mediastinum ,heart, great vessels, trachea, esophagus
Vertebral body, or carina, or ipsilateral malignant pleural effusion
Nodes (N)
N0 No regional lymph node metastases
N1 Metastases to ipsilateral peribronchial or hilar nodes
N2 Metastases to ipsilateral mediastinal or subcarinal nodes
N3 Metastases to contralateral mediastinal or hilar or to any scalene
or supraclavicular nodes
Distant Metastases (M)
M0 No distant metastases
M1 Distant metastases

7
Management
• 2/3 of pts are inoperable.
• The type ,stage of lung cancer&overall health of the patient, determine the modlity
of Rx.
• Modlities of Rx
• Lung cancer surgery
• Chemotherapy
• Radiation therapy
• Laser and stenting
Surgery
▪ Surgical resection is the choice for stage 1,stage 2 and selected cases of stage3.
▪ Resection of the tumour & the grossly involved regional mediastinal & bronchial L.N.
▪ Complications :-
1. Lobar collapse.
2. Prolonged pulmonary insufficiency.
3. Bronchopleural fistula.
4. Air leak.
Contraindications to surgical resection in bronchial carcinoma
1. distant metastasis (M1).
2. malignant pleural effusion (T4).
3. invasion of central mediastinal structures such as the heart , trachea, esophagus and
great vessels (T4).
4. contralateral mediastinal nodal involvement (N3).
5. Severe unstable cardiac or other comorbid medical condition.
6. FEV1 < 0.8 L

8
Factors determine inoperability
Chemtherapy
• For SCLC
• Improve survival upto80%.
• Reduces systemic recurrence.
• Prolonged disease free survival.
• (Combinations of iv. Cyclophosphamide,vincristene and itoposide is most commonly
used)
side effect: nausea and vomitting>> Give 5HT3 receptor antagonist
• CHEMOTHERAPY is less effective in NSCLC
• Using of platinuim based chemotherapy gives 30% response rate and small
increase in survival.
Molecularly targeted therapy
▪ Molecularly targeted therapy involves the administration of drugs that have been
identified to work in subsets of patients whose tumors have specific genetic changes
(driver mutations) that promote tumor growth.
) %
(Iressa) are more specifically target cancer
cells, resulting in less damage to normal cells than general chemotherapeutic agents.
▪ Erlotinib and gefitinib target a protein called the epidermal growth factor receptor
(EGFR) that is important in promoting the division of cells.

9
Molecular testing: For advanced NSCLCs
The gene encoding this protein is mutated in many cases of
, creating a driver mutation that encourages tumor growth.
These other targeted therapies include ALK tyrosine kinase inhibitor drugs crizotinib
(Xalkori) and ceritinib (Zykadia) that are used in patients whose tumors have an
abnormality of the ALK gene as the driver mutation.
Radiation
▪ It is less effective than surgery
▪ CHART : continuous hyperfractionated accelerated radiotherapy,small more frequent
doses
Neoadjuvant :before surgery given to down stage the disease.
Adjuvant: Prevention of local tumour recurrence,post operative care.
Palliative :-in pt with severe complication such as SVC obstruction,recurrent
hemoptysis, chest wall pain due to invasion of chest wall,obstruction of trachea and
main bronchus.
Curative:-contraindications
◦ malignant plural effusion
◦ distant metastases
◦ active pulmonary infection
Paraneoplastic syndrome
1.Endocrine syndrome :
a) Cushing syndrome: oat cell carcinoma secrete ACTH.
b) Secretion of ADH by oat cell lead to water retention and brain edema.
c) Hypercalcaemia due to secretion of parathyroid like hormone by squamuscell
carcinoma
2.Neurological syndrome:
a. peripheral neuropathy,
b. encephalopathy

10
c. myopathy
3. Dermatomyocytis
4. Pulmonary osteoarthropathywith clubbing of fingers
PROGNOSIS
The overall prognosis in bronchial carcinoma is very poor, with around 70% of patients
dying within a year of diagnosis and only 6-8% of patients surviving 5 year after diagnosis.
The best prognosis is with well- differentiated squamous cell tumors that have not
metastasized and are amenable to surgical resection
