physiology GIT))
المحاضرة الأولىالمرحلة الثانية
Physiology of gastrointestinal tract (GIT)
The digestive system is a group of organs working together, responsible for taking whole foods and turning them into energy and nutrients to allow the body to function, grow, and repair itself.
The gastrointestinal tract is a continuous tube that stretches from the mouth to anus .its primary function is to serve as a portal whereby nutrients , vitamins minerals ,water and electrolyte can be absorbed into the body .
The major activities of GIT:
1- Ingested food .
2- Secretion of fluids and digestive enzymes. The meal is mixed with Secretion from gastrointestinal tract itself and organs that drain into it such as salivary gland, pancreas and gall- bladder
3- Mixing and movement of food and wastes. A variety motility patterns that serve to mix the meal with digestive secretions and move it along the length of GIT.
4- Digested food in which proteins , fats and complex carbohydrates are broken down into absorbable units.
5-Absorption of nutrients, electrolytes and water from the intestinal lumen to blood stream.
6- Excretion of wastes .The residues of the meal that cannot be absorbed are expelled from the body.
7-GIT have regulatory mechanisms act both locally and systematically.
8-GIT have large number of bacteria particularly in the colon or large intestine .
Electrical Activity of Gastrointestinal Smooth Muscle:-
The smooth muscle of the gastrointestinal tract is excited by almost continual slow, intrinsic electrical activity along the membranes of the muscle fibers. This activity has two basic types of electrical waves
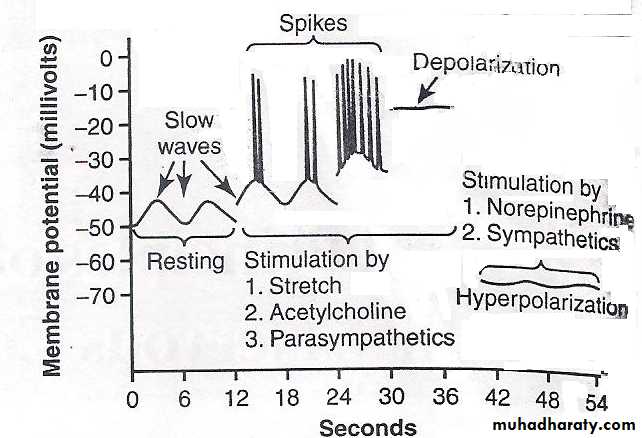
(1)slow waves and (2) spikes, the voltage of the resting membrane potential change to different levels, this have important effects in controlling motor activity of the gastrointestinal tract.
Slow Waves. Most gastrointestinal contractions occur rhythmically, by the frequency of “slow waves” of smooth muscle membrane potential. These waves, not action potentials, they are slow , undulating changes in the resting membrane potential .Their intensity usually varies between 5 and15 millivolts , and their frequency ranges in different parts of the human gastrointestinal tract from 3 to 12per minute about 3 in the body of the stomach, as much as 12 in the duodenum, and about 8 or 9 in the terminal ileum. .
slow waves is appear to be caused by complex interactions among the smooth muscle cells and specialized cells, called the interstitial cells of Cajal, act as electrical pacemakers for smooth muscle cells. These interstitial cells form network with each other and are interposed between the smooth muscle layers, with synaptic-like contacts to smooth muscle cells. The interstitial cells of Cajal undergo cyclic changes in membrane potential due to unique ion channels that periodically open and produce inward (pacemaker) currents that may generate slow wave activity.
Spike Potentials.
The spike potentials are true action potentials. They occur automatically when the resting membrane potential of the gastrointestinal smooth muscle becomes more positive than about -40 millivolts. in Figure( 2) each time the peaks of the slow waves temporarily become more positive than -40 millivolts, spike potentials appear on these peaks. The higher the slow wave potential rises ,the greater the frequency of the spike potentials ,usually ranging between 1 and 10 spikes per second, each gastrointestinal spike lasting as long as 10 to 20 milliseconds.
potential averages about -56 millivolts, but multiple factors can change this level. When the potential becomes less negative which is called depolarization of the membrane, the muscle fibers become more excitable.When the potential
becomes more negative, which is called hyperpolarization, the fibers become less excitable. Factors that depolarize the membrane—that is, make it more excitable—are (1) stretching of the muscle, (2) stimulation by acetylcholine, (3) stimulation by parasympathetic nerves that secrete acetylcholine at their endings, and (4) stimulation by several specific gastrointestinal hormones. Important factors that make the membrane potential more negative—that is, hyperpolarize the membrane and make the muscle fibers less excitable—are(1) the effect of norepinephrine or epinephrine on the fiber membrane and (2) stimulation of the sympathetic nerves that secrete mainly norepinephrine at their endings.
Membrane potentials in intestinal smooth muscle. Note the slow waves , the spike potentials, total depolarization, and hyperpolarization all of which occur under different physiologic conditions of the intestine.
Regulate GIT function:
This can be done by two pathways1-neural pathway 2-Humoral pathway1-neural pathway:
all the activities of GIT are involuntary controlled by (ANS); except ingestion (intake of food),mastication and defecation
Neural control can be divided into:
A-Intrinsic nerve supply
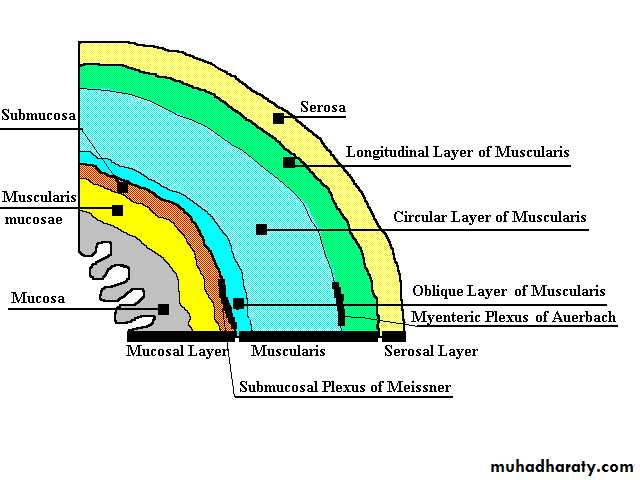
The GIT has an enteric nervous system or ( local brain) which control movement and secretion of GIT .Is composed of two layer of neurons and connecting fibers.The outer layer called the myenteric plexus(Auerbach’s) which control mainly the GIT movement which increased strength and frequency and GIT tone , and the inner layer called the submucousal plexus or (Meissner's plexus) which is controls secretion of submucosal gland .
Structure of GIT wall
The parasympathetic and sympathetic nervous signal to GIT from the brain and spinal cord alter the degree of activity of this enteric nervous system.
B-Extrinsic nerve supply; include
The Parasympathetic innervationsStimulation of parasympathetic nerve fibers releases acetylcholine and causes increase activity of the enteric nervous system which enhances the activity of GIT.
The sympathetic innervations:
It has inhibitory function that secrete mainly norepinephrine at their endings .
Nervous Control of Gastrointestinal Blood Flow:-
Stimulation of the parasympathetic nerves ,increases local blood flow at the same time that it increases glandular secretion. The effects of stimulation are not direct that glandular secretion lead to increase blood flow.
Sympathetic stimulation, by contrast, cause intense vasoconstriction of the arterioles with greatly decreased blood flow.
After a few minutes of this vasoconstriction, the flow often returns almost to normal by means of a mechanism called “auto regulatory escape.” That is, the local metabolic vasodilator mechanisms that are elicited by ischemia override the sympathetic vasoconstriction returning toward the necessary nutrient blood flow to the gastrointestinal glands and muscle .
sympathetic vasoconstriction in the gut allows shut-off of gastrointestinal and other splanchnic blood flow for short periods of time during heavy exercise, when increased flow is needed by the skeletal muscle and heart. Also, in circulatory shock (inadequate blood flow throughout the body),when all the body’s vital tissues are in danger of cellular death for lack of blood flow—especially the brain and the heart—sympathetic stimulation can decrease splanchnic blood flow to very little for many hours.
Sympathetic stimulation also causes strong vasoconstriction of the large-volume intestinal and mesenteric veins. This decreases thereby displacing large amounts of blood into other parts of the circulation. In hemorrhagic shock or other states of low blood volume, this mechanism can provide as much as 200 to 400 milliliters of extra blood to sustain the general circulation.
2-Humoral pathway:
This pathway called humoral because it Include hormones and neurotransmitters. GIT hormones are secreted from certain area of GIT and released into portal circulation to influence the function of other parts in GIT to regulate movement and secretion of the digestive enzyme ,this can be classified into 3 groups :
a-Gastrin family: function mainly on stomach to increase gastric secretion .
b-secretin family: secretin influence the secretion and movement of the small intestine ,and cholecystokinin -pancreozyme (CCK-PZ) ,which act mainly on the secretion of gall bladder and pancreas .
c-small poly peptides: are really neurotransmitters which may have local function on certain area of GIT example vasoactive intestinal poly peptide (VIP),substance P (neurotensin) common pathway to regulate vomiting, villikinin which regulate movement of the intestinal villi.