Symptoms associated with CRC
weight lossloss of appetite
night sweatsfever
rectal bleedingchange in bowel habits
obstructionabdominal pain & mass
iron-deficiency anemia
iron deficiency anemia in an older man means gastrointestinal cancer until proved otherwiseAppendix
appendicitis is the most common acute abdominal condition the surgeon is called on to treat. ACUTE APPENDICITISNo age is immune, but the peak incidence is in the second and third decades.
Males are affected more often than females in a ratio of 1.5:1.
Pathogenesis. Appendiceal inflammation is associated with obstruction in 50% to 80% of cases, usually in the form of a fecolith and, less commonly, a gallstone, tumor, or ball of worms (Oxyuriasis vermicularis). With continued secretion of mucinous fluid, the build-up of intraluminal pressure presumably is sufficient to cause collapse of the draining veins. Obstruction and ischemic injury then favors bacterial proliferation with additional inflammatory edema and exudation, further embarrassing the blood supply. Nevertheless, a significant minority of inflamed appendices have no demonstrable luminal obstruction, and the pathogenesis of the inflammation remains unknown.
MORPHOLOGY At the earliest stages, only a neutrophilic exudate may be found throughout the mucosa. submucosa, and muscularispropria.
this signifies early acute appendicitis for the operating surgeon. As the Inflammatory process worsens, there is abscess formation within the wall, along with ulcerations and foci of necrosis in the mucosa. This state constitutes acute suppurative appendicitis. Further appendiceal compromise leads to large areas of hemorrhagic green ulceration of the mucosa, and green-black gangrenous necrosis through the wall extending to the serosa, creating acute gangrenous appendicitis
The inflamed appendix (bottom) is red, swollen, and covered with a (fibrinous exudate. For comparison, a normal appendix is shown (top).
histologic criterion for the diagnosis of acute appendicitis is neutrophilic infiltration of the muscularis propria.
TUMORS OF THE APPENDIX
Carcinoids are the most common form of neoplasia in the appendix. The only other lesions worthy of mention are mucocele of the appendix and mucinous neoplasms.
Mucocele refers to dilation of the lumen of the appendix by mucinous secretion.
Mucinous neoplasms range from the benign mucinous cystadenoma, to mucinous cystadenocarcinoma, which invades the wall, to a form of disseminated intraperitoneal cancer called pseudomyxoma peritonei. The cystadenoma is histologically identical to analogous tumors in the ovary. The malignant mucin-secreting neoplasms (cystadenocarcinomas) invade the wall, allowing tumor cells to implant throughout the peritoneal cavity, which becomes filled with mucin (pseudomyxoma peritonei).
PANCREAS
Pancreatitis
ACUTE PANCREAIITIS
Inflammation of the pancreas, almost always associated with acinar cell injury. Acute pancreatitis is characterized by the acute onset of abdominal pain resulting from enzymatic necrosis and inflammation of the pancreas. Typically, there is an elevation of pancreatic enzymes in blood and urine. The release of pancreatic lipases causes fat necrosis in and about the pancreas.
MORPHOLOGY
The four basic alterations are:(1) proteolytic destruction of pancreatic substance.
(2) necrosis of blood vessels with subsequent interstitial hemorrhage,
(3) necrosis of fat by lipolytic enzymes.
(4) an associated acute inflammatory reaction. The extent and predominance of each of these alterations depend on the duration and severity of the process.
A common sequel of acute pancreatitis is a pancreatic pseudocyst,, which does not contain an epithelial lining. Drainage of pancreatic secretions into this space (from damaged pancreatic ducts) may lead to massive enlargement of the cyst over months to years.
Etiology.
A variety of predisposing conditions for acute pancreatitis have been identified. Most common are gallstones and alcoholism, which together are responsible for approximately 80% of the cases. The remaining specific causes are unusual, and 10% to 20% of cases of acute pancreatitis are without apparent predisposing influencesClinical Features.
Abdominal pain is the cardinal manifestation of acute pancreatitis. Its severity varies with the extent of pancreatic injury. Localization in the epigastrium with radiation to the back is characteristic. Shock, a common feature of acute pancreatitis, is caused not only by pancreatic hemorrhage but also by release of vasodilatory agents.
The mortality rate with severe acute pancreatitis is high, about 20% to 40%. Death is usually caused by shock, secondary abdominal sepsis, or the acute respiratory distress syndrome.
CHRONIC PANCREATITIS
• Chronic pancreatitis is characterized by repeated bouts of mild to moderate pancreatic inflammation, with continued loss of pancreatic parenchyma and replacement by fibrous tissue.• The disease is protean in its manifestations and most frequently middle aged men, particularly those who are alcoholic.
• Biliary tract disease plays a less important role in chronic pancreatitis than in the acute form of the disease,
• hypercalcemia and hyperlipoproteinemia predispose to chronic pancreatitis.
• Almost half of the patients have no apparent predisposing influences and are therefore said to have idiopathic pancreatitis.
MORPHOLOGY
In chronic pancreatitis, the pancreas is transformed into a densely fibrotic organ with extensive atrophy of the exocrine glands, sometimes with remarkable sparing of the islets. A chronic inflammatory infiltrate around lobules and ducts is usually present, and there is variable obstruction at pancreatic ducts of all sizes by protein plugs. Grossly, the gland is hard, sometimes with extremely dilated ducts and visible calcified concretions. Pseudocysts similar to those described in acute pancreatitis may be present, either internal or external to the pancreatic substance.
Neoplasms
A broad spectrum of exocrine neoplasms can arise in the pancreas. They may be cystic or solid; some are benign, while others are among the most lethal of all malignancies.CYSTIC NEOPLASMS
Only 5% to 15% of all pancreatic cysts are neoplastic (most cysts are pseudocysts). While some, such as the serous cystadenoma, are entirely benign, others, such as mucinous cystic neoplasms, can be benign or malignant
Close to 95% of mucinous cystic neoplasms arise in women, and, in contrast to serous cystadenomas, they can be associated with an invasive carcinoma.
Pancreatic mucinous cystadenoma. A, Cross-section through a mucinous multiloculated cyst in the tail of the pancreas. The cysts are large and filled with tenacious mucin. B,The cysts are lined by columnar mucinous epithelium, and a dense "ovarian" stroma is noted.
Carcinoma of the Pancreas
• The term carcinoma of the pancreas is meant to imply carcinoma arising in the exocrine portion of the gland.• Carcinoma of the pancreas is now the fifth most frequent cause of death from cancer in the United States, preceded only by lung, colon, breast, and prostate cancers. Its incidence has remained unchanged over 50 years.
• One consistent association has been noted: the incidence rates are several times higher in smokers than in nonsmokers.
• The peak incidence occurs in persons between 60 and 80 years of age.
• As with other cancers, carcinomas of the pancreas show multiple mutations in cancer-associated genes. Most common are mutations in the K-RAS gene and in the tumor suppressor gene CDKN2A, both noted in 90% of cases. Indeed, the combination of CDKN2A and K-RAS mutations consider"print” of pancreatic cancers. P53 gene is also mutated in more than half of cases.
MORPHOLOGY
Approximately 60% to 70% of the cancers of this organ arise in the head of the pancreas, 5% to 10% in the body, and 10% to 15% in the tail; in20%, the tumor diffusely involves the entire gland. Virtually all of these lesions are adenocarcinomas arising from the ductal epithelium. Some may secrete mucin, and many have an abundant fibrous stroma,With carcinoma of the head of the pancrease the ampullary region is invaded, obstructing outflow of bile. In marked contrast, carcinomas of the body and tail of the pancreas do not impinge on the biliary tract and hence remain silent for some time. They may be quite large and widely disseminated by the time they are discovered. They extend through the retroperitoneal spaces, infiltrate adjacent nerves, and occasionally invade the spleen, adrenals, vertebral column, transverse colon, and stomach. Distant metastases occur, principally to the lungs and bones
Microscopically,
there is no difference between carcinomas of the head of the pancreas and those of the body and tail of the pancreas. Most grow in more or less glandular patterns ; they may be either mucinous or non-mucin secreting. In many cases, the glands are atypical, irregular, and small, and they are lined by anaplastic cuboidal to columnar epithelial cells.
Clinical Features. From the preceding discussion, it should be evident that carcinomas in the pancreas usually remain silent until their extension impinges on some other structure. It is when they erode into posterior soft tissues and affect nerve fibers that pain appears.
Obstructive jaundice is associated with most cases of carcinoma of the head of the pancreas . Spontaneously appearing phlebothrombosis (Trousseau sign), also called migratory thromhophlebitis, is sometimes seen with carcinoma of the pancreas, particularly that of the body and tail. However, this syndrome is not pathognomonic for cancer in this organ
The liver
HepatitisHepatitis:-mean any inflammatory lesion of the liver. This term is not used for local lesions such as an abscess but only when there is diffuse involvement of the liver.
There are many etiological factors that causing hepatitis such as alcoholic hepatitis, drug induce hepatitis and viral hepatitis.
Viral hepatitis -: main infection of the hepatocytes by virus that produces necrosis and inflammation of the liver and presented with jaundice. It caused mainly by hepatotropic viruses( which are hepatitis virus A,B,C,D,E,G).
Hepatitis viruses C &B are the most common cause of chronic hepatitis, liver cirrhosis and hepatocellular carcinoma.
-:Acute viral hepatitis
it can caused by any one of the hepatotropic viruses. The clinical feature of the disease more or less is the same and the patient presented with non specific constitutional symptoms such malaise, generalized fatigability, nausea, loss of appetite, weight loss, low grade fever, headache, muscle & joint pain &diarrhea with enlarge tender liver. Then the patient enter the icteric phase and once jaundice appear other symptoms begin to disappear. In a few weeks to several months, the jaundice and most other systemic symptom disappear and convalescence begins.Pathological Features:-
Classical Acute Hepatitis:- The morphological feature of all types of acute viral hepatitis are the same, so there is diffuse hepatic involvement with more severe change in the perivenular areas. The most striking feature is1. focal necrosis (necrosis of small clusters of hepatocytes)within the hepatic lobule
2. There is scattered necrosis of single liver cells within the hepatic lobule and these cells appear as small, deeply eosinophilic, containing pyknotic nuclear material called (Councilman, acidophilic bodies or apoptotic bodies) and these bodies have been extruded from the liver cell plate into the sinusoid.
3. There is many liver cells show varying degrees of hydropic swelling (balloon cells) with a vacuolated cytoplasm. The hepatocytes necrosis is associated with mononuclear inflammatory cell infiltration, predominantly lymphocytic.
The liver is quickly recovers from the acute injury and return to normal by diminishes of necrosis &hyperatrophy, hyperplasia of the surviving hepatocytes .
Chronic Hepatitis:- is defined as inflammation of the liver continuing without improvement for at least 6 moths. It may occur as a sequel of HCV,HBV infection or due to alcoholic liver disease, long standing biliary obstruction, Wilson disease & other metabolic disorder.
The pathological features of chronic hepatitis include the piecemeal necrosis, portal inflammation, periportal fibrosis & lobular inflammation, necrosis & regeneration.
Piecemeal necrosis:-the lesion is essentially periportal& refers to focal destruction of the limiting plate of hepatocytes.
A periportal chronic inflammatory infiltrate, which creates an irregular border between the portal tracts& the lobular parenchyma.
Chronic hepatitis is subdivided into a benign form ; chronic persistent hepatitis in which the inflammation is largely confined to the portal areas, and a more aggressive form; chronic active hepatitis in which there is portal, periportal, acinar involvement with progressive fibrosis ending in cirrhosis.
chronic persistent hepatitis is a mildest form of chronic hepatitis which may be seen in patients with chronic active hepatitis who go into remission either spontaneously or due to immunosuppressant therapy.
Liver Diseases
The changes in the liver that caused by high consumption of alcohol include fatty change of the liver, alcoholic hepatitis, hepatic fibrosis & cirrhosis. Only fatty change is a reversible disorder while alcoholic hepatitis is consider as precursor for liver cirrhosis.Alcoholic Fatty Liver:- accumulation of fat in hepatocytes (steatosis). The pathogenesis of fatty liver is clearly depend on the intake of ethanol because it is fully and rapidly reversible when the alcohol consumption is stopped.
Within hepatocyte, ethanol
1. increases fatty acids synthesis
2. decreases mitochondrial oxidation of fatty acids
3. increases the production of the triglycerides
4. impairs the release of lipoproteins.
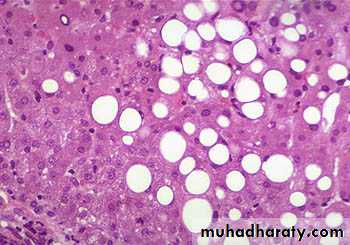
Morphological Features:-
Grossly the liver become yellow and enlarged (some times becomes three times than the normal weight).Microscopically: the extent of fat accumulation varies from minute droplets scattered in the cytoplasm of a few hepatocytes to distention of the entire cytoplasm of most cells by coalesced fat droplets. The hepatocytes become just like adipocyte with distended clear cytoplasm and the nucleus is displaced to the periphery and become flattened
Diagrammatic representations of the morphologic features of acute andchronic hepatitis. Bridging necrosis (and fibrosis) is shown only for chronichepatitis; bridging necrosis may also occur in acute hepatitis (not shown).
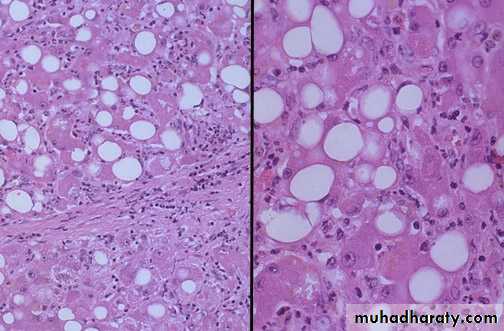
Alcoholic Hepatitis:- which is usually superimposed on fatty liver & appear as an acute necrotizing lesion characterized by
1)ballooning and necrosis of hepatocytes predominantly in the central zone together with
2)neutrophilic inflammatory response
3) presence of hyaline cytoplasmic inclusions with invisibly damaged hepatocyte &these inclusion bodies appear as irregular solid eosinophilic masses mainly in a perinuclear location & the called Mallory bodies
4)perivenular fibrosis.
If alcoholic hepatitis is continued so it may result in progressive fibrosis & scaring. Fibrous septa may extend and form links between contiguous perivenular areas and between hepatic veins and portal tracts. The liver architecture is distorted and liver cirrhosis is established.
In alcoholic steatosis: lipid accumulates within the cytoplasm of hepatocytes, creating large clear vacuoles within cells. The nuclei in such cells are compressed to the periphery of the cell.
Alcoholic hepatitis:Mallory's hyaline is seen here, but there are also neutrophils, necrosis of hepatocytes, collagen deposition, and fatty change.
Alcoholic hepatitis. A, The cluster of inflammatory cells marks the site of a necrotic hepatocyte. A Mallory body is present in a second hepatocyte (arrow). B, Eosinophilic Mallory bodies are seen in hepatocytes, which are surrounded by fibrous tissue (H&E).
Alcoholic cirrhosis. A, The characteristic diffuse nodularity of the surface reflects the interplay between nodular regeneration and scarring. The greenish tint of some nodules is due to bile stasis. A hepatocellular carcinoma is present as a budding mass at the lower edge of the right lobe (lower left of figure). B, The microscopic view shows nodules of varying sizes entrapped in blue-staining fibrous tissue. The liver capsule is at the top (Masson trichrome).
Liver Cirrhosis
The end stage of chronic liver disease is cirrhosis.Cirrhosis is a condition involving the entire liver in which the parenchyma exchanged into a large number of nodules separated from one an other by irregular branching &anastamosing sheets of fibrous tissue.
Classification of liver cirrhosis: their is an aetiological and morphological classifications
Aetiological classification:-
Acquired
1. alcoholic
2. post viral
3. Biliary cirrhosis ;
primary
Secondary (due to bile duct destruction)
Inherited
1. haemochromatosis
2. wilsons' disease
3. alpha-1 antitrypsin deficiency
Morphologically cirrhosis are classified into:-
1. micronodular cirrhosis in which the nodules are approximately up to 3mm indiameter
2. macronodular cirrhosis in which the nodules are of variable size & may be ranged up to l cm diameter.
3. Mixed type in which both small & large nodules are present. This pattern ismost frequently seen in end stage cirrhosis.
A close-up view of a micronodular cirrhosis in aliver with fatty change demonstrates the small,yellow nodules
Micronodular cirrhosis is seen along with moderate fattychange. Note the regenerative nodule surrounded by fibrousconnective tissue extending between portal regions.
In macronodular cirrhosis, the regenerative nodules are large and irregular insize and shape. The fibrous septa are often broad. is most often seen following chronic active viral hepatitis.
Pathology and Pathogenesis:- cirrhosis results from long continuous loss of liver cells, with a persistent inflammatory reaction accompanied by fibrosis & compensatory hyperplasia.
Grossly:-the liver may be of normal size or enlarge if there is fatty change or excessive development of hyperplastic regenerating nodules. However it shrinks as the disease progress due to loss of liver cells exceeding regeneration. The surface is diffuse nodular & on cut section the parenchyma is divided into rounded nodules separated by bands of fibrous tissue. The color is either pale if there is fatty change, bile stained if there is cholestasis and red if there is congestion.
complications of cirrhosis:-
1. Hepatocellular failure2. Portal hypertension
3. Liver cell carcinoma which arise in 10-15% of all cirrhotic patients.
Tumors and Tumors Like Conditions :-
Focal nodular hyperplasia:- solitary or multiple benign hepatocellular nodules developed in the liver in the absence of cirrhosis occurs most frequently in young middle age adults. It is a well demarcated poorly encapsulated nodule with a central fibrous scar. It represent a nodular regeneration in response to focal vascular injury and not a real neoplasm per se.Benign tumors:-
1. cavernous hemangioma:- it is a well demarcated lesion consist of endothelial cells-lined vascular channels & intervening stroma.
2. adenoma:- occurs in young females who are on oral contraceptive drug. Histologically composed of sheet or cords of cells resemble normal hepatocytes.
Malignant:-
1. Hepatoblastoma:-aggressive hepatocellular tumor of childhood & it usually fatal.
2. Hepatocellular carcinoma:-malignant tumor of hepatocytes that’s closely linked to HBV infection, HCV, alcoholic liver cirrhosis &haemochromatosis. In 85% of
patients there is raising in serum levelof α-fetoprotiens. Hepatocellular carcinoma may appear grossly as:-
i) Unifocal usually massive tumor.
ii) Multifocal ( malignancy made of widely distributed nodules of variable size
iii) Diffusely infiltrative( cancer may involve the entire liver).
Microscopically; either well differentiated to anaplastic, but trabecular, acinar, pseudoglandular patterns may present.
3. cholangiocarcinoma:-it is of adenocarcinoma type typically with abundant fibrous stroma ( desmoplastic)that why the tumor grossly appear firm and gritty in consistency.
Diseases of Gallbladder
Cholelithiasis:- is defined as the presence of the stones within the lumen of the gallbladder or in the extrahepatic biliary tree.Gallstones are formed from the constituents of the bile( cholesterol, bile pigments, calcium salts & other organic material in various proportions).
The risk factors of gallstones formation:-
Gall stones are commonest in:-
1. Late adult life2. Premenopausal women & that is due to estrogen effect which stimulate the formation of lithogenic bile from the liver (estrogen increase the hepatic secretion of the cholesterol & decrease the secretion of the bile acids).
3. Women on oral contraceptive pills
4. Obesity
5. Familial predisposition
6. Diabetes
7. Patients who undergo ileal resections(there is an increase tendency for stone formation due to decreased in bile acid pool).
Pathogenesis:- the exact mechanism of gall stones formation seems to be due to change in the composition of the bile, local factors in the gallbladder & biliary tract infection.
Types of gallstones:-
1. Cholesterol stone:- is the commonest type2. Bile pigment stone
3. Calcium carbonate stones
Cholesterol gallstones. Mechanical manipulation during laparoscopic cholecystectomy has caused fragmentation of several cholesterol gallstones, revealing interiors that are
pigmented because of entrapped bile pigments. The gallbladder mucosa is reddened and irregular as a result of coexistent chronic cholecystitis.
Pigment gallstones. Several faceted black gallstones are present in this otherwise unremarkable gallbladder
Cholecystitis:- inflammation of gallbladder is one of the commonest cause of abdominal pain & frequently required cholecystectomy.
Acute cholecystitis:-is a diffuse inflammation of the gallbladder usually secondary to obstruction of the gallbladder outlet.
Pathogenesis:- about 90-95% of cases are associated with gallstones which causing obstruction to the bile outflow & the bile become over concentrated. The over concentrated bile causing irritation & inflammation to the mucosal wall of the gallbladder & the inflammatory reaction is aggravated by secondary bacterial infection.
Grossly:- the external surface of the gallbladder is congested and layered with a fibrinous exudates. Gallstones are usually found within the lumen, some of them obstructing the cystic duct. Some times the luminal cavity are distended & contain a cloudy purulent fluid (empyema) that is occur when there is complete obstruction of the cystic duct by stones with superadded secondary bacterial infection.
Microscopically:-edema & hemorrhage in the wall with acute and chronic inflammation. Secondary bacterial infection may lead to suppuration of the wall. The mucosa shows focal ulceration or in severe cases wide spread necrosis in which the term gangrenous cholecystitis is applied.
Chronic cholecystitis:-is a persistent inflammation of the gallbladder wall, is almost invariably associated with gallstones.
It is the most common disease of the gallbladder which resulted from repeated attacks of acute cholecystitis, or from long standing gallstones & in this cases the pathogenesis may be due to chronic irritation by the stones with chronic chemical injury to the gallbladder epithelium.
.
Grossly:-the wall of chronically inflamed gallbladder is thickened & firm. Gallstones are usually found within the lumen
Microscopically:- the wall is fibrotic & usually it is penetrated by sinuses of Rokitansky-Aschoff (epithelial down growths through the muscular coats forming gland like structures). Chronic inflammation of variable degree may be seen in all layers. In long standing cases of chronic cholecystitis the wall of the gallbladder may become calcified, in which case the term porcelain gallbladder is used
Tumors:-
Benign tumors:-benign tumors of gallbladder &extrahepatic bile duct are rare.In gallbladder papillomas are the most common benign tumors, Mucous gland adenoma in the infundibulum are also associated with stones. Adenomyoma, fibroma,lipoma, leiomyoma are rare.
Benign tumors of the bile ducts are the same benign tumors of the gallbladder but they are more important clinically because they can cause obstruction to the biliary flow and jaundice.
Carcinoma of the gallbladder:- the most common malignant gallbladder tumors is the adenocarcinoma which founded in 2% of patients who undergo gallbladder surgery. This tumor is usually associated with cholelithiasis, chronic cholecystitis, and it is more common in women than men. The calcified gallbladder (porcelain gallbladder) is more liable to developing gallbladder carcinoma.
Pathology:- it may occur anywhere in the gallbladder but most frequently in the fundus. The tumor is charactaristecally an infiltrative, well differentiated adenocarcinoma. It usually desmoplastic and thus the wall of the gallbladder becomes thickened and leathery. The tumor mainly metastasis by lymphatic although vascular spread and direct spread into the liver and adjacent structure can occur.
Cholangiocarcinoma. A, Autopsied liver showing a massive neoplasm in the right hepatic lobe and innumerable metastases permeating the entire liver. B, Microscopic view
showing tubular glandular structures embedded in a dense sclerotic stroma.