
MEDICINE
haematology
oj
Lec.47
Dr.Ali M.
Anemia
Lec .4
2/3/2017
Done by : Taher Ali Taher
2016-2017
مكتب اشور لالستنساخ
2/3/2017
anemia
Dr.Ali M.
1
By : taher ali taher
Objectives
By the end of this lecture, the student should be able to :
1-state the mechanism ,causes and effects of anemia in pregnancy.
2-state the mechanism and diagnosis of anemia of chronic disease.
3-enumerate the causes of aplastic anemia.
4-give a statement about the diagnosis and treatment of aplastic anemia and
myelodysplastic syndrome.
Clinical Scenario
A 20 year old female is pregnant at 5 months.
She presented with progressive pallor and dizziness on standing.
Her clinical exam revealed pallor without splenomegaly.
Her hemoglobin was 8 gm/dl.
What is your differential diagnosis?
Anemia of Pregnancy
By the second trimester of pregnancy, at least a mild degree of maternal
anemia is universal ( Hb > 10 g/dl).
Significant anemia ( hemoglobin concentration <10 g/dl) occurs with a
prevalence ranging between 2% and 26%, depending upon the
population studied.
In all populations, but particularly in the less-developed countries of the
world, anemia is a major health problem.
It contributes to maternal and fetal morbidity and mortality.
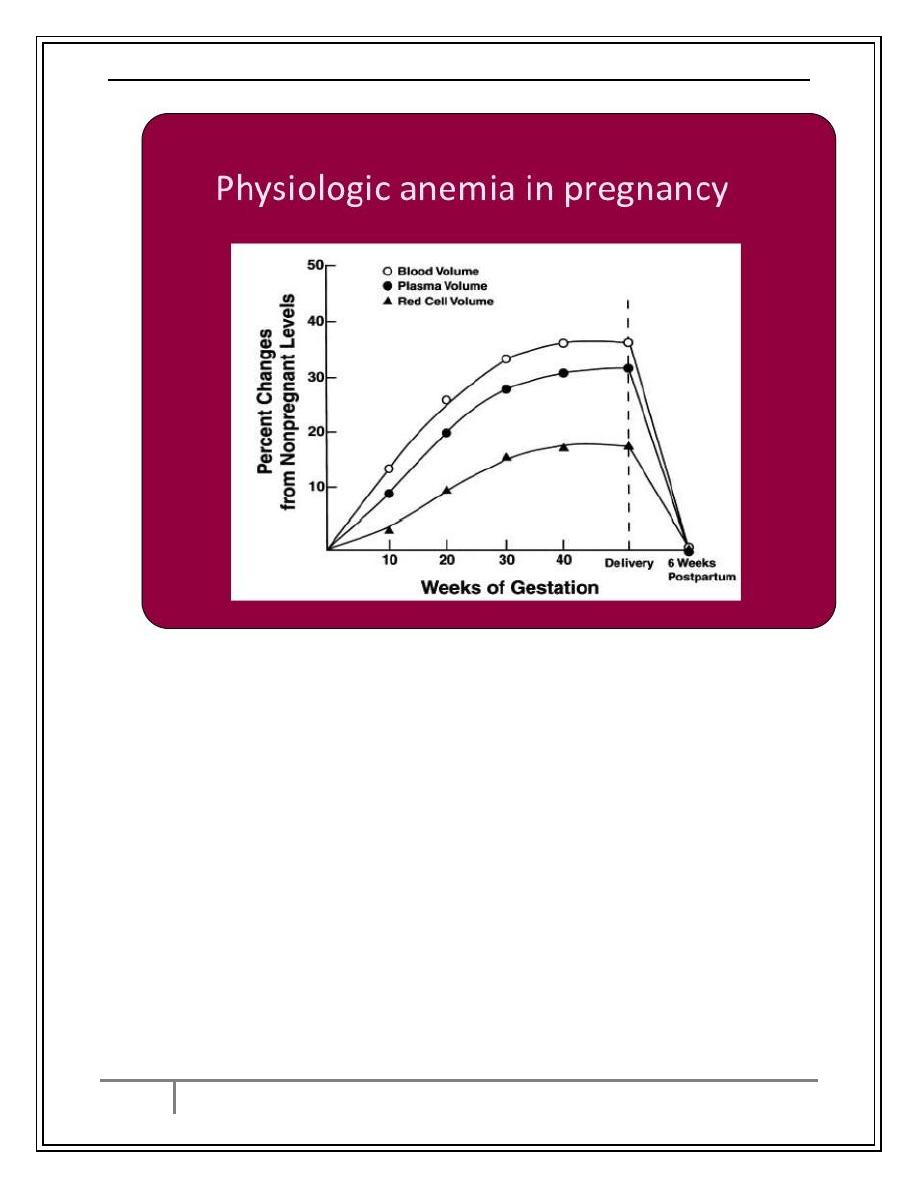
Physiological Anemia of Pregnancy
Plasma volume begins to increase during the sixth week of pregnancy.
There is no significant increase in erythrocyte production during the first
trimester.
Dilutional anemia is first apparent by the seventh to eighth week.
Increase in erythrocyte production is apparent during the second
trimester.
Lowest hemoglobin explainable by dilutional effect (the physiologic
anemia of pregnancy) is 11 g/dl in the first trimester and 10 g/dl in the
second and third trimesters.
Physiologic anemia of pregnancy is normochromic and does not worsen
during the third trimester, and does not require additional evaluation or
specific treatment.
2/3/2017
anemia
Dr.Ali M.
2
By : taher ali taher
Causes of Anemia of Pregnancy
o Nutritional / Iron deficiency anemia
o Pre-pregnancy poor nutrition very important
o folate deficiency
o Chronic blood loss due to parasitic infections – Hookworm
o Multiparity
o Multiple pregnancy
o Acute blood loss
o Recurrent infections (UTI) - anemia due to impaired erythropoiesis
o Hemolytic anemia with pre-eclampsia
o Hemoglobinopathies like Thalassemia, sickle cell anemia
o Aplastic anemia is rare
2/3/2017
anemia
Dr.Ali M.
3
By : taher ali taher
Effects on Mother and Baby
Higher incidence of pregnancy complications :Pre-eclampsia, abruptio
placentae, preterm labor
Predisposed to infections like – UTI, puerperal sepsis
Increased risk to Post partum bleeding
Lactation failure
Maternal mortality – due to CHF, Cerebral anoxia, Sepsis,
Higher incidence of abortions, preterm birth
Low APGAR score of baby at birth
Neonate more susceptible for anemia & infections
Higher Perinatal morbidity & mortality
Anemic infant with cognitive & affective dysfunction
Management
Physiological anemia does not require treatment, prophylactic folate
with iron are given orally.
Pathological anemia is treated accordingly.
Blood transfusion is indicated if the patient comes with severe anemia
just before delivery where the time for treatment to take effect is short.
Blood transfusion is also used for severe anemia if the cause can not be
corrected by treatment.
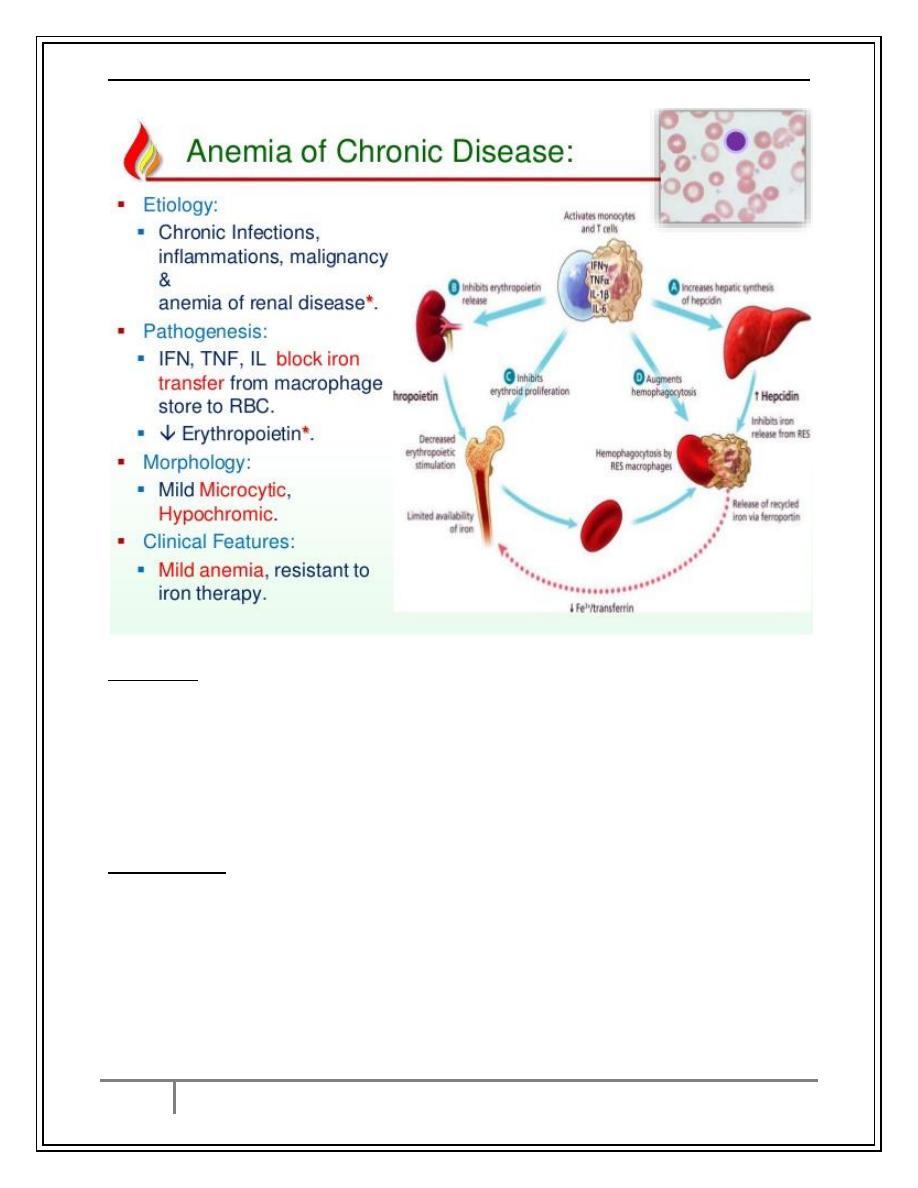
Anemia of Chronic Disease
Etiology
Infections, cancer, endocrine disorders (e.g. thyroid).
Inflammatory and rheumatologic disease.
Renal disease.
Pathophysiology
A mild hemolytic component is often present, red blood cell survival
is moderately decreased.
Erythropoietin levels are normal or slightly elevated but are
inappropriately low for the degree of anemia, erythropoietin level is
low in renal failure
Iron cannot be removed from its storage pool in hepatocytes and RES
cells.
2/3/2017
anemia
Dr.Ali M.
4
By : taher ali taher
Anemia of Chronic Disease
Diagnosis
RBC are usually normocytic normochromic if the anemia is mild, but
may be microcytic normochromic, or even microcytic
hypochromic,Hb rarely < 9 g/dL except in renal failure.
Serum iron, TIBC, and % saturation all normal or slightly reduced,
serum ferritin is normal or increased.
Normal or increased iron stores in bone marrow, decreased “normal”
sideroblasts.
Management
Resolves if underlying disease is treated.
Erythropoietin may normalize the hemoglobin value especially in
chronic renal failure. Dose of erythropoietin required is lower for
patients with renal disease
2/3/2017
anemia
Dr.Ali M.
5
By : taher ali taher
Case Presentation
A 50 year old female presented with one month history of progressive
pallor, multiple ecchymoses ,epistaxis and attacks of fever and sore
throat.
Her clinical examination revealed severe pallor, multiple bleeding
spots on her legs .
Blood counts revealed pancytopenia
What is your differential diagnosis?
Aplastic Anemia
Etiology
1- Radiation
2- Drugs
anticipated (chemotherapy)
idiosyncratic (chloramphenicol, phenylbutazone)
3- Chemicals
benzene and other organic solvents
DDT and insecticides
4- Post viral e.g. hepatitis B, parvovirus,HIV.
5- Idiopathic
often immune (cell mediated)
6- Paroxysmal nocturnal hemoglobinuria
7- Marrow replacement
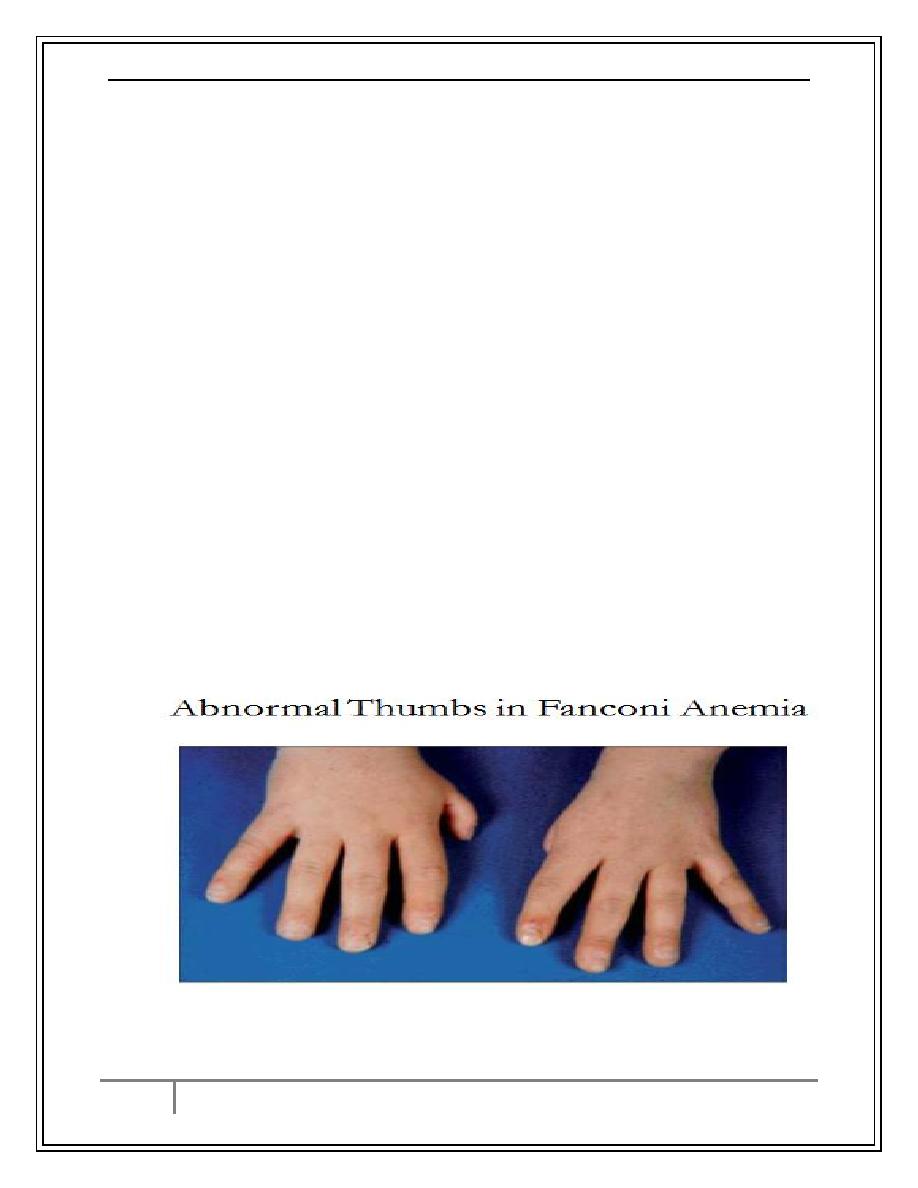
8- Congenital: Fanconi anemia, associated with dysmorphic features.
2/3/2017
anemia
Dr.Ali M.
6
By : taher ali taher
Clinical Presentation of Aplastic Anemia
1- Occurs at any age
2- Slightly more common in males.
3- Can present acutely or insidiously.
4- Features of anemia or neutropenia or thrombocytopenia (any
combination).
o
Thrombocytopenia as bruising, bleeding gums, epistaxis.
o
Anemia as SOB, pallor and fatigue.
o
Presentation of neutropenia ranges from infection in the mouth to
septicemia.
Aplastic Anemia
Diagnosis
1- CBC: Pancytopenia
normochromic normocytic anemia.
neutrophil count < 1.5 x 10
9
/L.
platelet count < 20 x 10
9
/L.
corrected reticulocyte count < 1%.
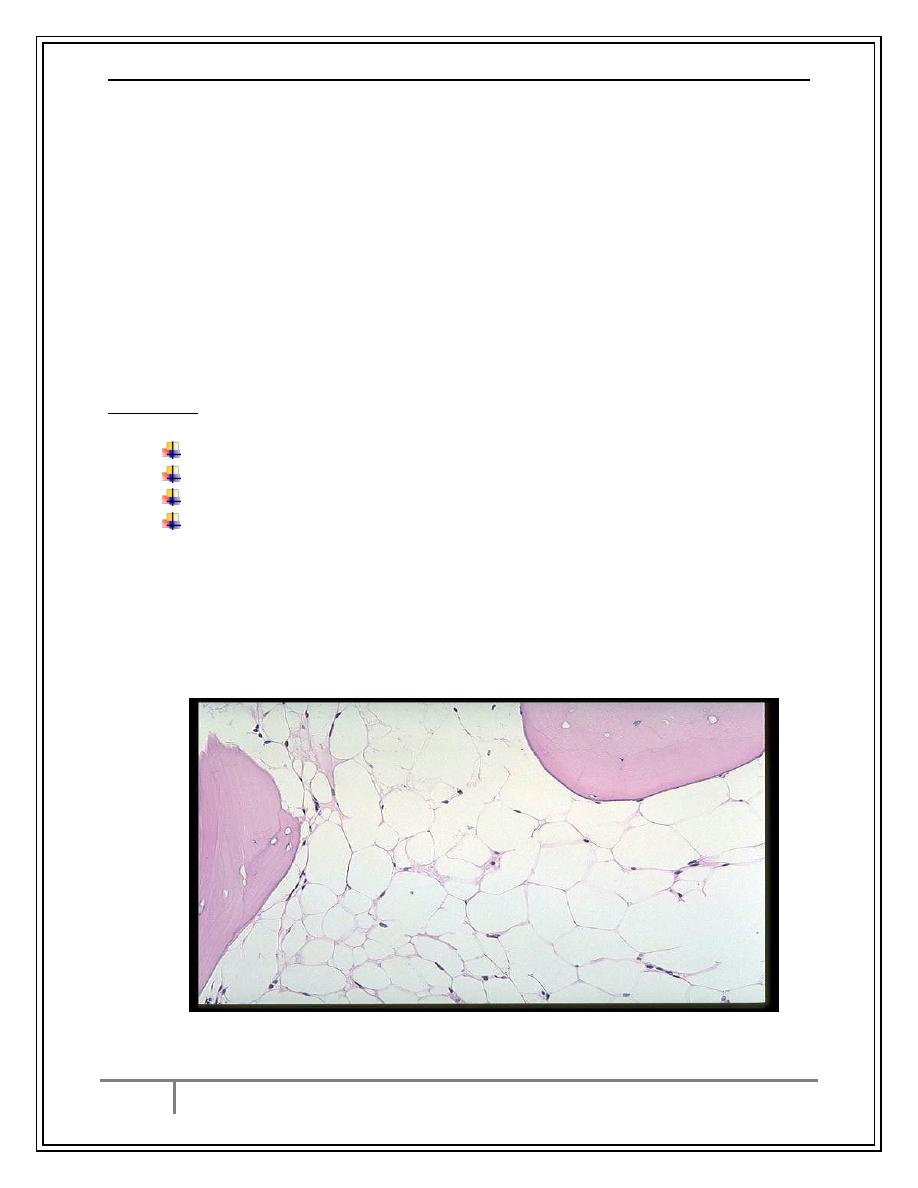
2- Bone marrow aspirate and biopsy
aplasia or hypoplasia of marrow cells with fat replacement.
Aplastic Bone Marrow Biopsy
2/3/2017
anemia
Dr.Ali M.
7
By : taher ali taher
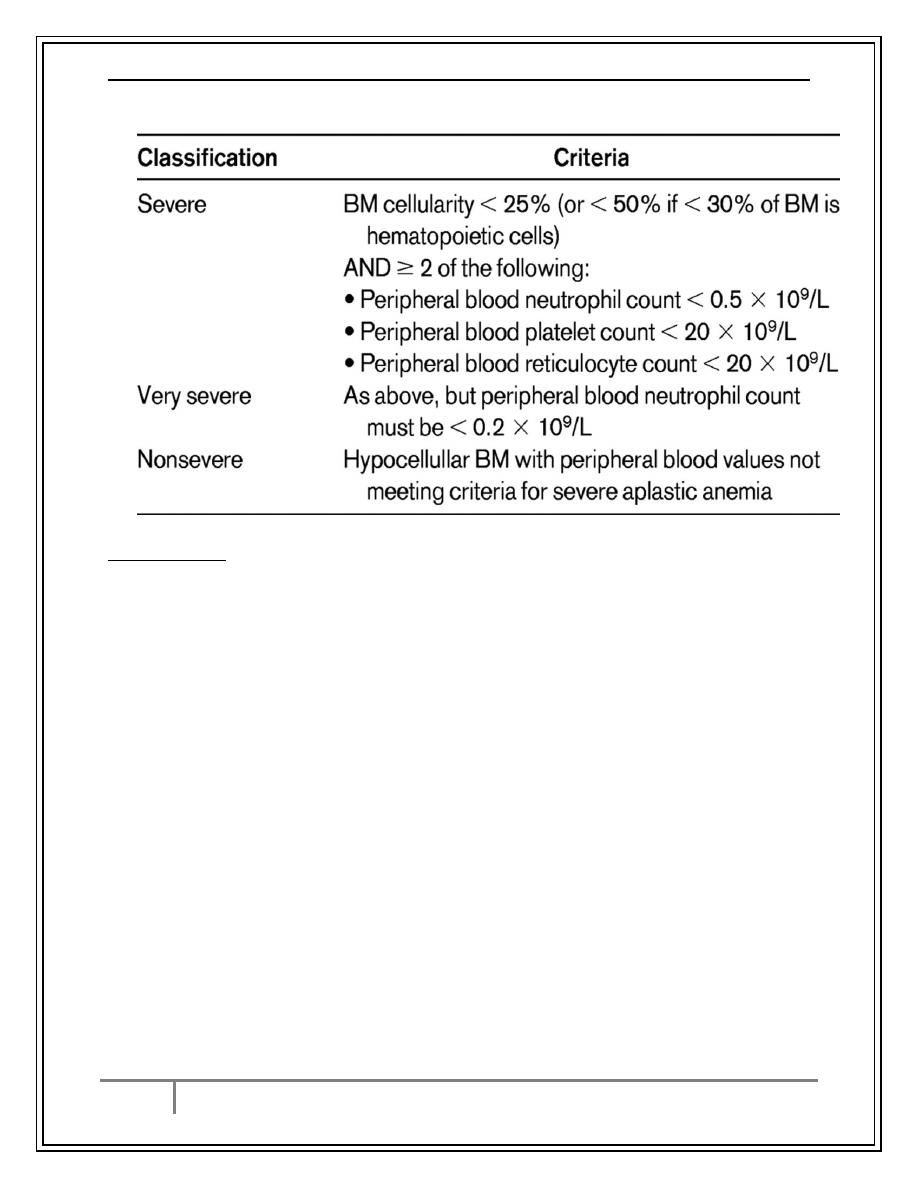
Classification of Severity
Aplastic Anemia
Management
o
Removal of offending agents.
o
Supportive care:
o
red cell transfusion to correct anemia, we try to exclude family members
eligible to be BM donors.
o
platelet transfusions in patients with severe thrombocytopenia and active
bleeding.
o
CMV negative patients should receive CMV negative blood products.
o
Antibiotics and antifungal drugs to treat febrile episodes aggressively as
these patients can die quickly from bacterial sepsis or disseminated
fungal infection.
o
Antithymocyte globulin (50-60% of patients respond) for patients who
are >45 years of age and those who have no donor for bone marrow
transplant
o
Cyclosporin A, mainly useful for mild cases.
o
Allogeneic bone marrow transplantation for patients<45 y
minimize blood products on presentation.
only irradiated, leuko-depleted blood products should be used to
minimize CMV transmission.
CMV negative blood for CMV negative patients.
2/3/2017
anemia
Dr.Ali M.
8
By : taher ali taher
MYELODYSPLASTIC SYNDROMES (MDS)
Pathophysiology
A. A group of clonal bone marrow stem cell disorders characterized by
one or more cytopenias.
B. Ineffective hematopoiesis despite presence of adequate numbers of
progenitor cells (bone marrow is usually hyper-cellular).
C. Dysplastic changes affect all the hematopoietic cell lines due to
abnormal maturation and differentiation which include abnormal size
, nuclear shape and cytoplasmic granules
D. The blood elements are dysfunctional.
E. There is increased liability for transformation to AML.
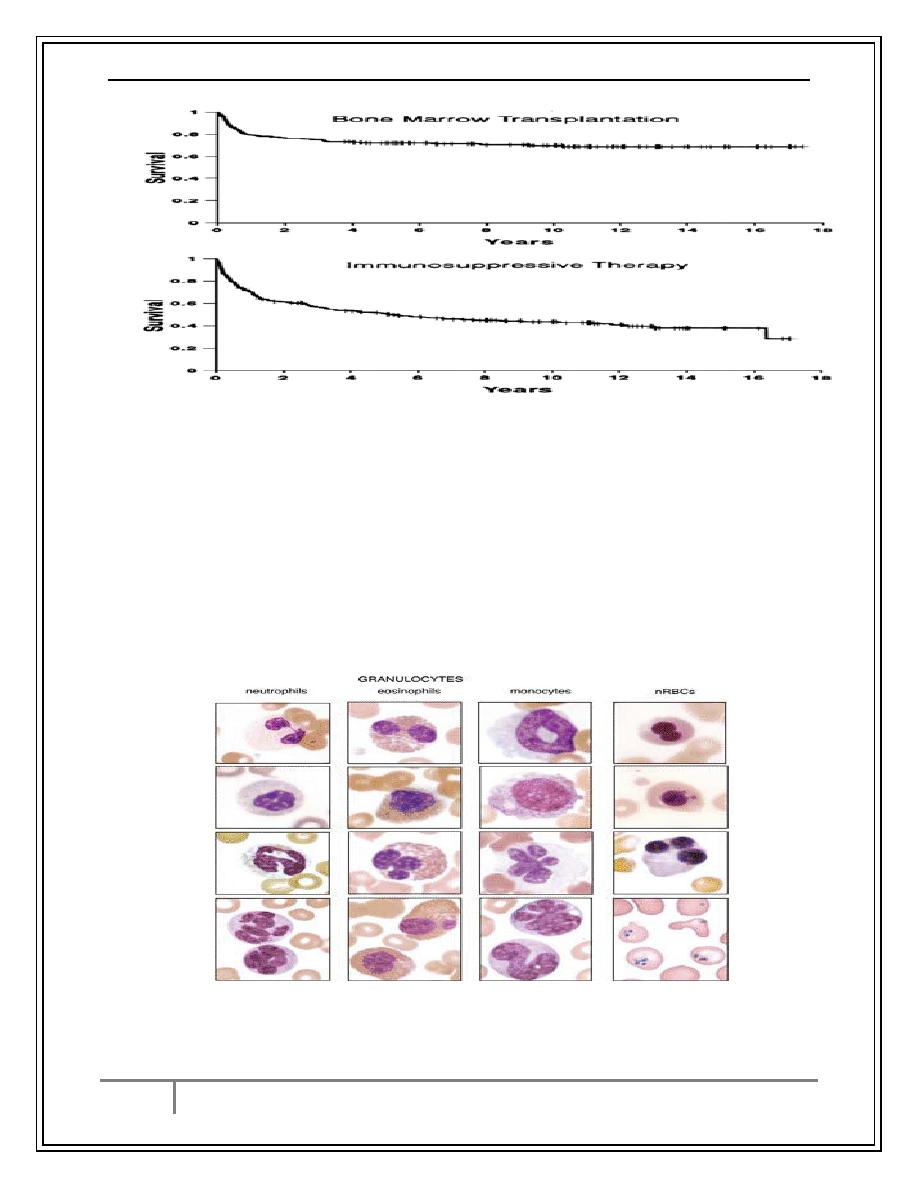
Dysplastic nuclear features in circulating cells. Composite image taken from several cases of
myelodysplastic syndrome showing dysplastic nuclear features seen in circulating granulocytes
and nucleated RBCs. The right lower figure shows numerous Pappenheimer bodies.
2/3/2017
anemia
Dr.Ali M.
9
By : taher ali taher
MDS
Types
i. Refractory anemia (RA).
ii. Refractory anemia with ring sideroblasts (RARS).
iii. Refractory anemia with excess blasts (RAEB).
iv. Refractory anemia with excess blasts in transformation (RAEB-T).
v. Chronic myelomonocytic leukemia (CMML).
Clinical Presentation
A. Related to bone marrow failure, most common in elderly, usually > 70
and post-chemotherapy or radiation
B. Usually insidious in onset: fatigue, weakness, pallor, infections,
bruising and rarely weight loss, and hepatosplenomegaly
Diagnosis
1- Anemia ± thrombocytopenia ± neutropenia
RBC: variable morphology with decreased reticulocyte count.
WBC: decrease in granulocytes and abnormal function.
Platelet: either too large or too small and thrombocytopenia.
2- Bone marrow : dysmyelopoiesis in bone marrow precursors
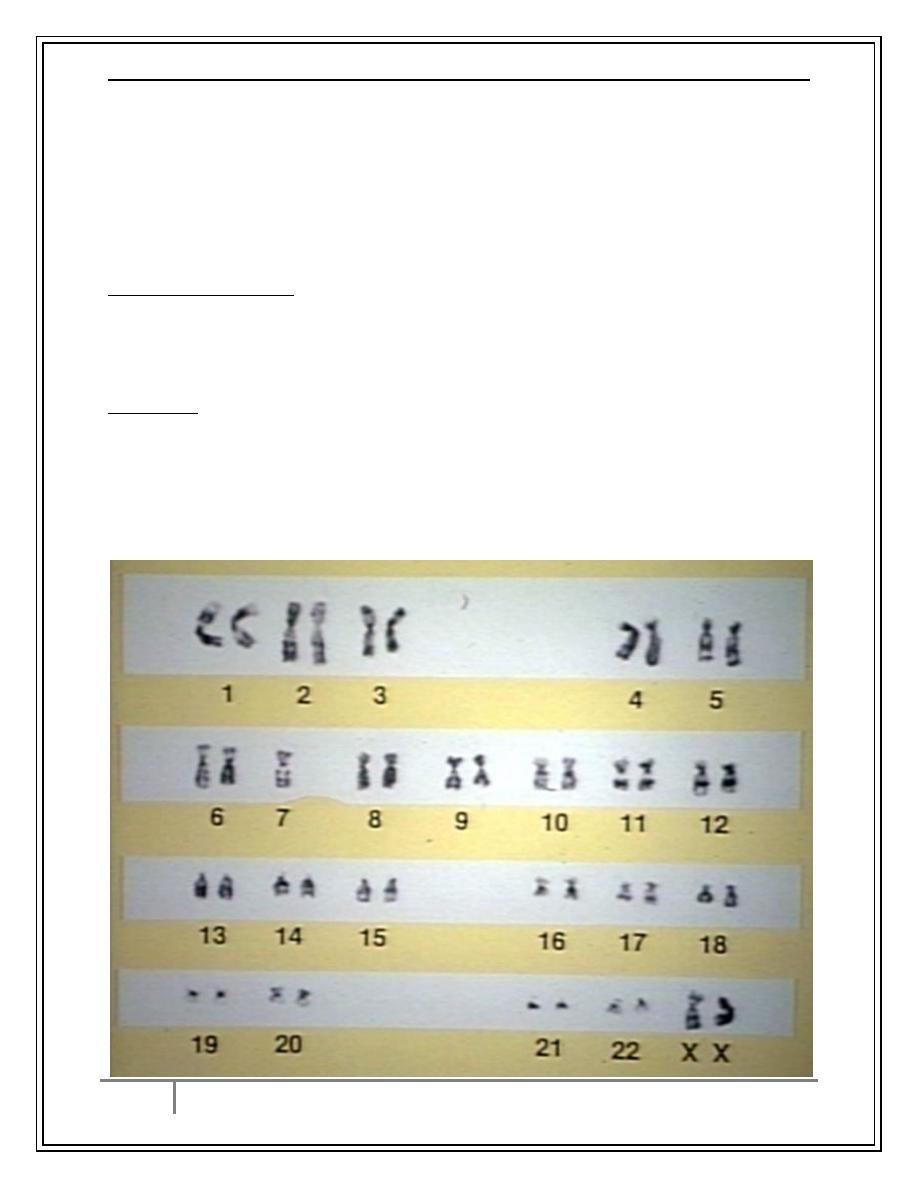
3- Chromosomal Abnormalities:5,7,8 ,others
2/3/2017
anemia
Dr.Ali M.
10
By : taher ali taher
Management
1- Symptomatic (transfusion, antibiotics)
2- Growth factors: Erythropoietin,G-CSF.
3- Cytotoxics for RAEB & RAEB-T&CMML
4- Bone marrow transplant for young patients with advanced disease.
5- Immune modulating and differentiating agents .
Conclusion
1-Anemia of pregnancy is a common problem, it may be physiological.
2-Pathological severe anemia is associated with maternal and neonatal
morbidity.
3-Anemia of chronic disease is common and can be missed for iron deficiency.
4-Anemia of chronic renal failure responds to erythropoietin.
5-Aplastic anemia is due to stem cell failure.
6-The best treatment is allogeneic stem cell transplantation.
7-Myelodysplastic syndrome is a group of disorders affecting bone marrow
stem cells that result in dysplastic changes, di or pancytopenia and tendency to
transform into AML.
…the end…
