gynecology
oj
kk
Total Lectures :19
Dr. Maad
Cervical cancer
Lec . 4
Done by :
Ali Faleh
2016-2017
مكتب اشور لالستنساخ

Cervical cancer Dr. Maad
[Year]
1
By : Ali Faleh
Cervical cancer
Introduction :
• Cancer of the cervix is the most common female genital cancer in developing
countries every year about 500,000 women , acquire the disease and 75% are
from frame developing countries.
• About 300,000 women also die from the disease annually and of these 75% are
from developing countries
• Finland which has an advanced population based screening program has one of
the lowest rates in the world.
Incidence :
• 4-6 % of female genital cancers.
• Age : 40-50 years old
Risk factors and aetiology
• Coitus at young age: <16 years old increased risk by 50%
• Number of sexual partners: 6 sexual partners or more increase risk by 14.2 folds.
• Smoking for > 12 years increase the risk by 12.7 folds.
• Male related risk factors:
number of the partners previous sexual relationships is relevant .
cervical cancer risk increased if partners has penile cancer (circumcision)
Previous wife with cervical cancer.
• Previous CIN
• Poor uptake of screening program.
Cervical cancer Dr. Maad
[Year]
2
By : Ali Faleh
• Long term use of the contraceptive pill increase the risk due to increasing
exposure to seminal fluids.
• Barrier method decrease the risk (condan)
• Immuno suppresion risk increased with immuno suppressed renal transplant
patients and in HIV positive women.
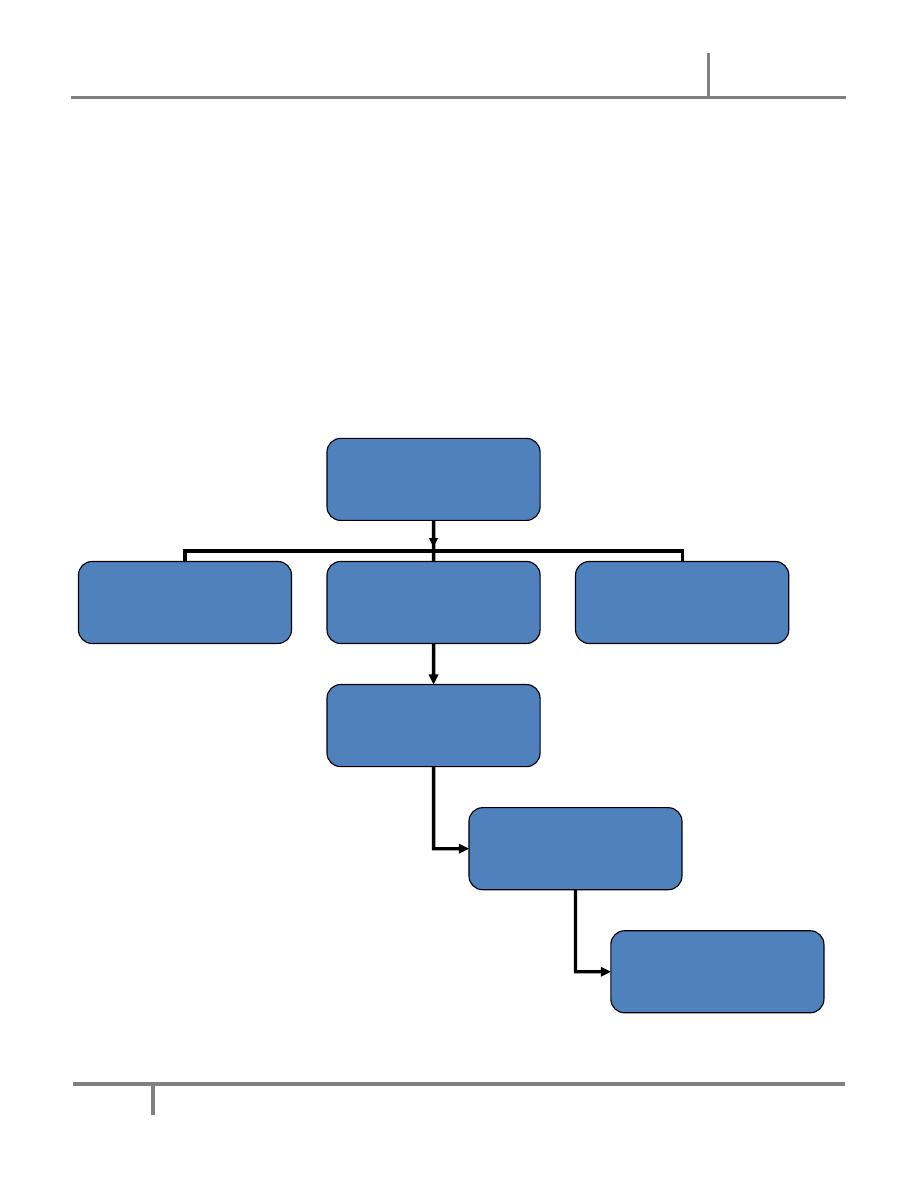
• HPV (Human papilloma virus ) infection mainly 16,18 the main aetiological is
infection with subtypes of HPV (16,18)
• Low socioecomic of PATIENT .
HPV 16,18
Smoking
Cervical cell
Male factors
Infhibation of CX cellp53 tumour
suppression gyne
Protection against
tumour
development lifted
Cancer develops
Cervical cancer Dr. Maad
[Year]
3
By : Ali Faleh
Type of suspected patients :
• Multiparous. + Low socioeconomic class.
• Poor hygiene.
• Prostitutes. + Low incidence in Muslims and Jews.
Predisposing factors:
1- Cervical dysplasia. 2- (Cervical intraepithelial neoplasia)
3- CIN III / CARCINOMA IN SITU
• THE LESION PROCEEDS THE INVASION BY 10-12 YEARS
Symptoms:
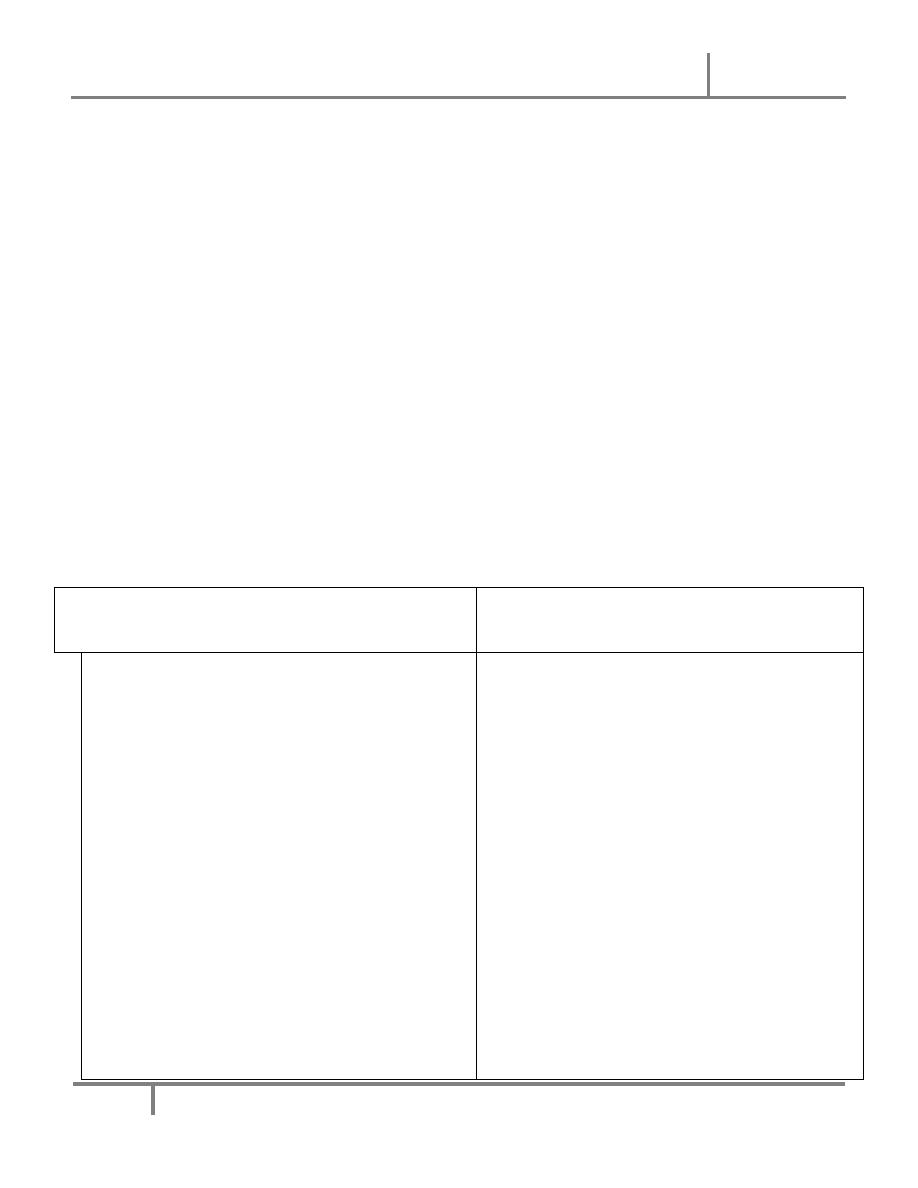
Early symptoms
Late symptoms
- None.
- Thin, watery, blood tinged vaginal
discharge frequently goes unrecognized
by the patient.
- Abnormal vaginal bleeding
Intermenstrual
Postcoital
Perimenopausal
Postmenopausal
- Blood stained foul vaginal discharge.
- Pain, leg oedema.
- Urinary and rectal symptoms
dysuria
haematuria
rectal bleeding
constipation
haemorrhoids
- Uraemia

Cervical cancer Dr. Maad
[Year]
4
By : Ali Faleh
Pathology type
Squamous cell carcinoma- 90%. Adenocarcinoma- 10%.
Types of growth
• Exophytic: is like cauliflower filling up the vaginal vualt.
• Endophytic: it appears as hard mass with a good deal of induration.
• Ulcerative: an ulcer in the cervix.
DIAGNOSIS
1- History :
• Many women are a symptomatic .
• Presented with abnormal routine cx smear
• Complain of abnormal vaginal bleeding
• I M bleeding
• post coital bleeding
• perimenopausal bleeding
• postmenopausal bleeding
• blood stain vaginal discharge
2- Examination:
• Mainly vaginal examination using cuscu’s speculem nothing is found in early stage
• Mass ,ulcerating fungating in the cervix
• P/V P/R is very helful.

Cervical cancer Dr. Maad
[Year]
5
By : Ali Faleh
Preoperative evaluation
• Review her history.
General examination witch involve :
o
Anaemia.
o
Lymphadenopathy-Supraclavicular LN.
o
Renal area.
o
Liver or any palpable mass.
o
Oedema.
Laboratory tests:
o
CBC, LFT, RFT, Urine analysis.
o
Tumour markers.
o
Chest X- ray, abdominal X- ray, IVU.
o
CAT, MRI, if necessary.
o
Ultrasound.
o
Lymphography, if necessary.
Staging
:
Best to follow FIGO system.
• Examination under anaesthesia.
• Bimanual palpation.
• P/V, P/R.
• Cervical biopsy, uterine biopsy.
Cervical cancer Dr. Maad
[Year]
6
By : Ali Faleh
• Cystoscopy, Proctoscopy, if necessary.
• Carcinoma of the cervix uteri.
•
Stage I
The carcinoma is strictly confined to the cervix (extension to the
corpus would be disregarded)
• IA Invasive carcinoma which can be diagnosed only by microscopy, with
deepest invasion ≤5 mm and largest extension≥7mm IA1 Measured stromal
invasion of≤3.0 mm in depth and extension of≤7.0 mm
• IA2 Measured stromal invasion of 3.0 mm and notN5.0 mm with an extension
of notN7.0 mm
• IB Clinically visible lesions limited to the cervix uteri or pre-clinical cancers
greater than stage IA⁎
• IB1 Clinically visible lesion≤4.0 cm in greatest dimension
• IB2 Clinically visible lesionN4.0 cm in greatest dimension
•
Stage II
Cervical carcinoma invades beyond the uterus, but not to the pelvic
wall or to the lower third of the vagina
• IIA Without parametrial invasion
• IIA1 Clinically visible lesion≤4.0 cm in greatest dimension
• IIA2 Clinically visible lesionN4 cm in greatest dimension
• IIB With obvious parametrial invasion
•
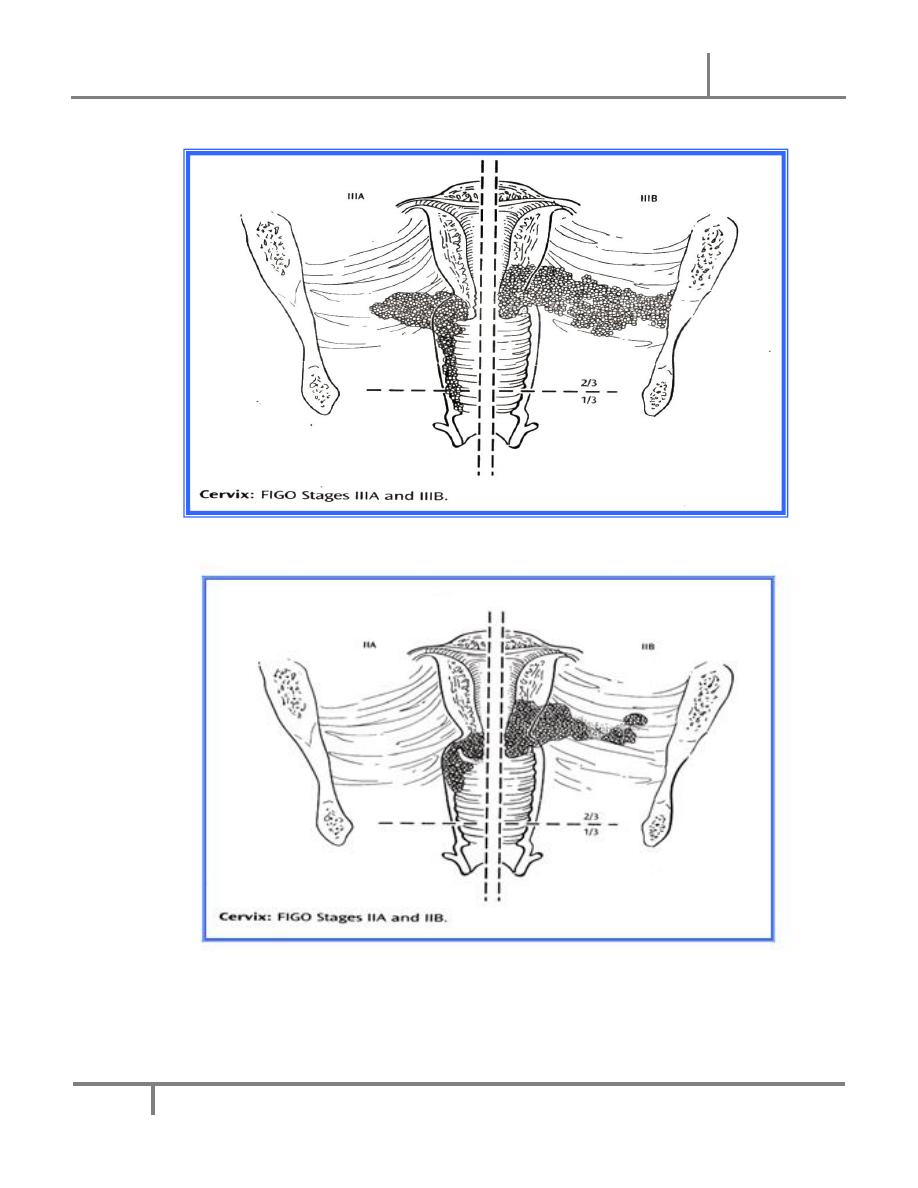
Stage III
The tumor extends to the pelvic wall and/or involves lower third of the
vagina and/or causes hydronephrosis or non-functioning kidney

Cervical cancer Dr. Maad
[Year]
7
By : Ali Faleh
• IIIA Tumor involves lower third of the vagina, with no extension to the pelvic
wall
• IIIB Extension to the pelvic wall and/or hydronephrosis or non-functioning
kidney
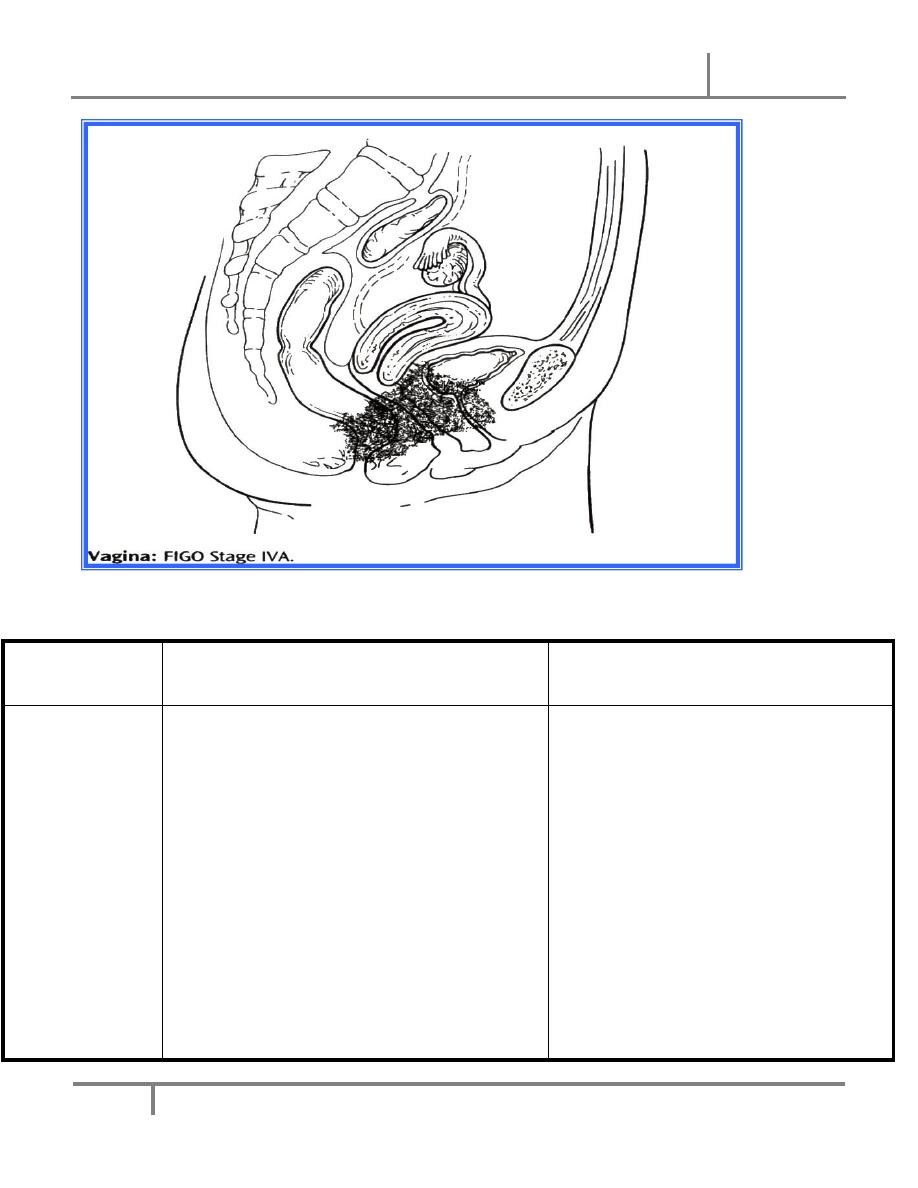
• Stage IV The carcinoma has extended beyond the true pelvis or has involved
(biopsy proven) the mucosa of the bladder or rectum. A bullous edema, as such,
does not permit a case to be allotted to Stage IV
• IVA Spread of the growth to adjacent organs
• IVB Spread to distant organs⁎
STAGES OF CANCER CERVIX
• Once cancer cervix is found (diagnosed), more tests will be done to find out if the
cancer cells have spread to other parts of the body. This testing is called staging.
Cervical cancer Dr. Maad
[Year]
8
By : Ali Faleh
• PLAN TREATMENT, A DOCTOR NEEDS TO KNOW THE STAGE OF THE DISEASE.
Cervical cancer Dr. Maad
[Year]
9
By : Ali Faleh
SPREAD:
Direct
Lymphatic
Dissemination (late)
- Uterus
body.
- Vagina.
-
Parametrium.
- Bladder and
rectum.
A- primary node:
parametrial.
Paracervical.
Vesicovaginal.
Rectovaginal.
Hypogastric.
Obturator and external iliac
- parametrial spread causes
obstruction of the ureters,
many deaths occur due to
uraemia.
- Obstruction to the cervical
canal results in pyometria.
Cervical cancer Dr. Maad
[Year]
10
By : Ali Faleh
B-Secondary nodes:
Common iliac
Sacral
Vaginal
Paraaortic + Inguinal.
DIFFERENTIAL DIAGNOSIS
• Cervical ectropion.
• Cervical tuberculosis.
• Cervical syphilis, Schistosomiasis, and Choriocarcinoma are rare causes.
TREATMENT
• Surgical….. or Radiotherapy or both .
• Radiotherapy and Chemotherapy followed by Surgery.
• Palliative treatment.
• The choice of treatment will depend on :
• Fitness & age of the patients
• Stage of disease.
• Type of lesion
• Experience and the resources avalible.

Cervical cancer Dr. Maad
[Year]
11
By : Ali Faleh
Surgical procedure
• The classic surgical procedure is the wertheim’s hystrectomy for stage Ib,IIa, and
some cases of IIb in young and fat patient
• Werthemeim’s hystrectomy
• Total abdominal hystrectomy including the parametrium.
• Pelvic lymphadenectomy
• 3 cm vaginal cuff
• The original operation conserved the ovaries ,since squamouss cell carcinoma
does not spread dirctly to the ovaries.
• Oophorectomy should be performed in cases of adenocarcinoma as there is 5-
10% of ovarian metastosis
• Surgery offers several advantage
• It allows presentation of the ovaries (radiotherapy will destroythem).
• There is better chance of preserving sexual function.
• (vaginal stonosis occur in up 85% of irradiates.
• Psychological feeling of removing the disease from the body .
• More accute staging and prognsis
COMPLICATIONS OF SURGERY
1- Haemorrhage: primary or secondary. 2- Injury to the bladder, uerters.
3- Bladder dysfunction. 4- Fistula.
5- Lymphocele. 6- Shortening of the vagina.

Cervical cancer Dr. Maad
[Year]
12
By : Ali Faleh
INDICATIONS OF P/O XRT FOLLOWING WERTHEIM’S
HYSTERECTOMY (STAGE I , IIa):
• Positive pelvic lymph nodes.
• Tumour close to resection margins and/or parametrial extension.
Radiotherapy
• Stage IIb and III
• Radical Radiotherapy
• External irradiation (Teletherapy).
• Intracavitary radiation (Brachytherapy).
• In some cases of stage IIa or b radio and chemotherapy to be given then followed
by simple hysterectomy -------
Palliative therapy
• For stage IV – individualized therapy.
• Some suitable for palliative XRT ( usually intracavitary Caesium).
• Some suitable for extensive surgery & some for chemotherapy
• Good nursing care.
• Analgesia-must be used in sufficient amount to ----- pain (Codein sulfate,
Pethidine, Morphine, Diamorphine).
• Antiemetic if necessary.
• IV drip, entral, and parentral feeding.
• Urinary Catheterization.
• Other measures for symptom relief.

Cervical cancer Dr. Maad
[Year]
13
By : Ali Faleh
PROGNOSIS
Depends on:
1- Age & Fitness of the patient.
2-
Stage of the disease.
3- Type of the tumour. 4- Adequacy of treatment.
THE OVERALL 5 YEARS SURVIVAL FOLLOWING THERAPY:
• Stage I -------80%
• Stage II-------50-60%
• Stage III-------30-40%
• Stage IV-------4%
MANAGEMENT OF RECURRENT DISEASE
• 1. Local recurrence:
Radiation – if not used.
Pelvic exenturation.
• 2. Distant disease
Chemotherapy.
Follow up policy
• On completion of treatment all patients are given a vaginal dilator to use until
vaginal mucosa healed, this prevents vaginal stenosis.
• Premenopausal patients commenced on HRT:
• post hysterectomy-Extraderm skin patches 50 meg twice weekly.
• No hysterectomy- Cycloprogyn 1mg daily.
• The patient to be seen 1/12 post-treatment.

Cervical cancer Dr. Maad
[Year]
14
By : Ali Faleh
• 3 monthly for 2 years.
• 4 monthly for 3rd year.
• 6 monthly until 5years.
• Then yearly all her life.
• Patients with stage I and II disease treated with radical radiotherapy will be
assessed by EUA approximately 3 months after completing treatment.
