By Dr. ishraq mohammed

The puerperium refers to 6 weeks period following
childbirth , when considerable changes occur before
return to the pre-pregnancy state .
Physiological changes :
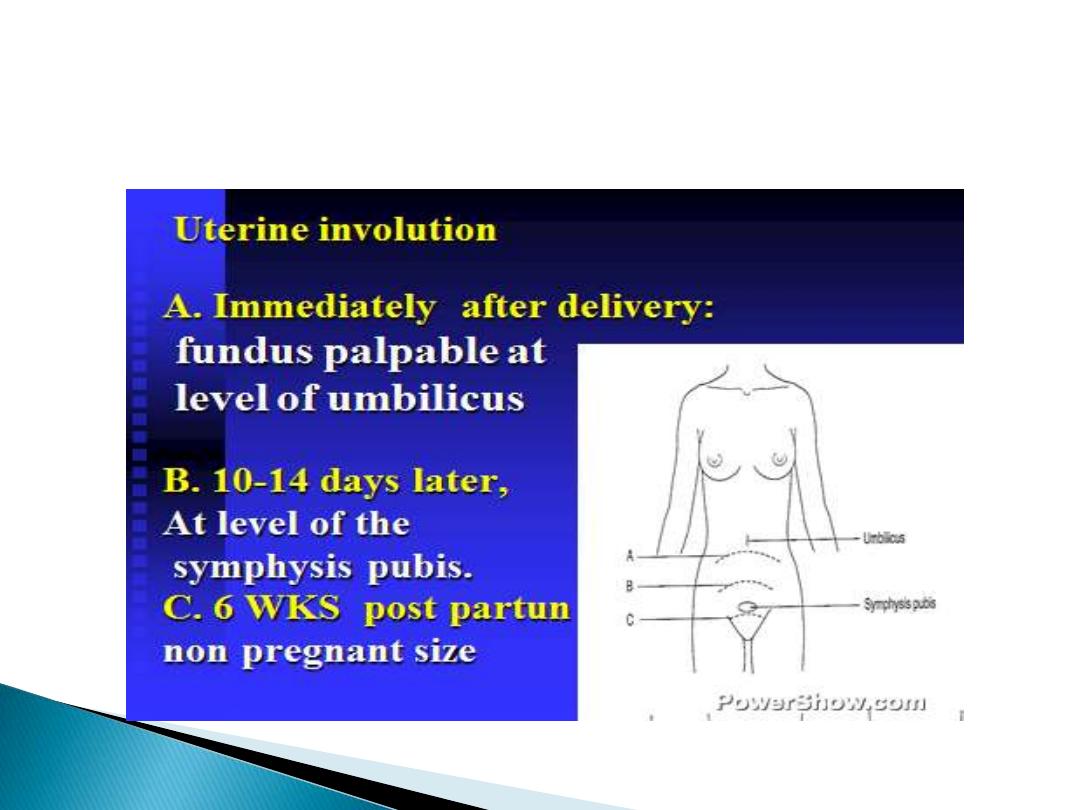
uterine involution:
Involution is the process by which the post-partum
uterus , weighing about 1 kg , return to its pre-
pregnancy state of less than 100 gm . Within 2
weeks, the uterus can no longer be palpable above
the symphysis .Involution occur by process of
autolysis , whereby muscle cells diminished in size
with no effect on number of muscle cells .Involution
appear to be accelerated by release of oxytocin in
women who are breastfeed.

Signs :causes of delayed involution :
1-full bladder.
2-loaded rectum.
3-uterine infection.
4-retained product of conception.
5-fibriods.
6-broad ligament haematoma.
A delay in involution in the absence of any
other signs or symptoms i.e. bleeding, is of
no clinical significance .

Genital tract changes :
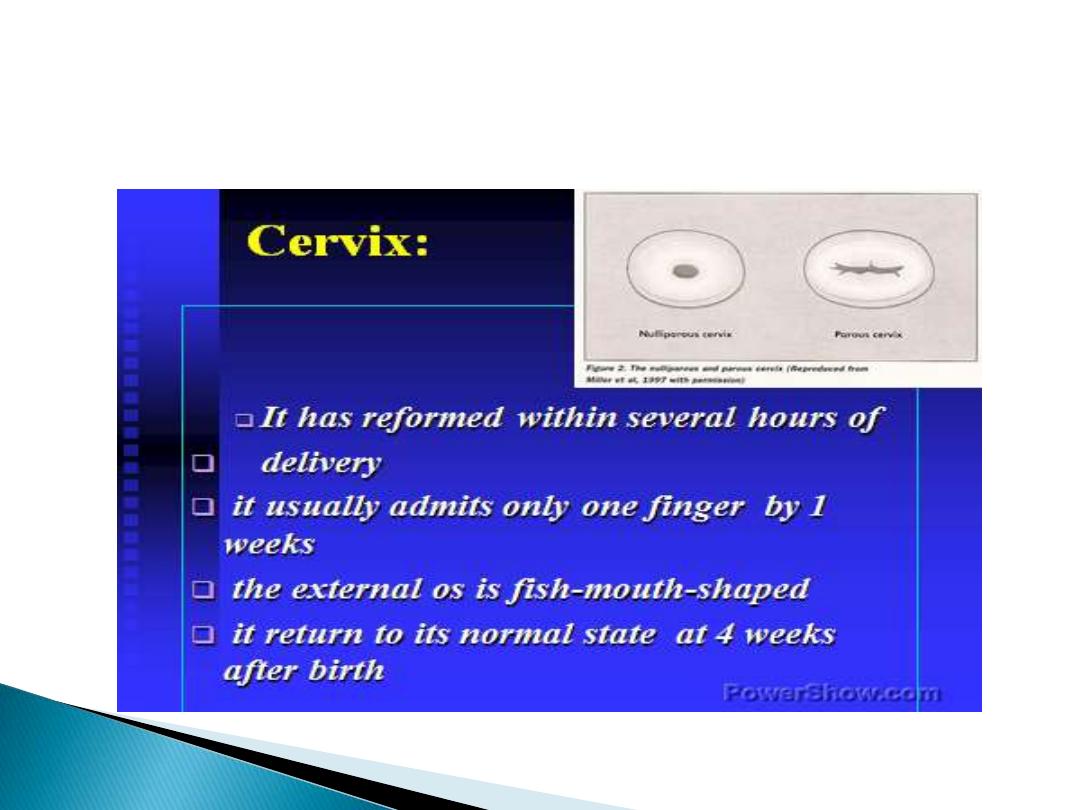
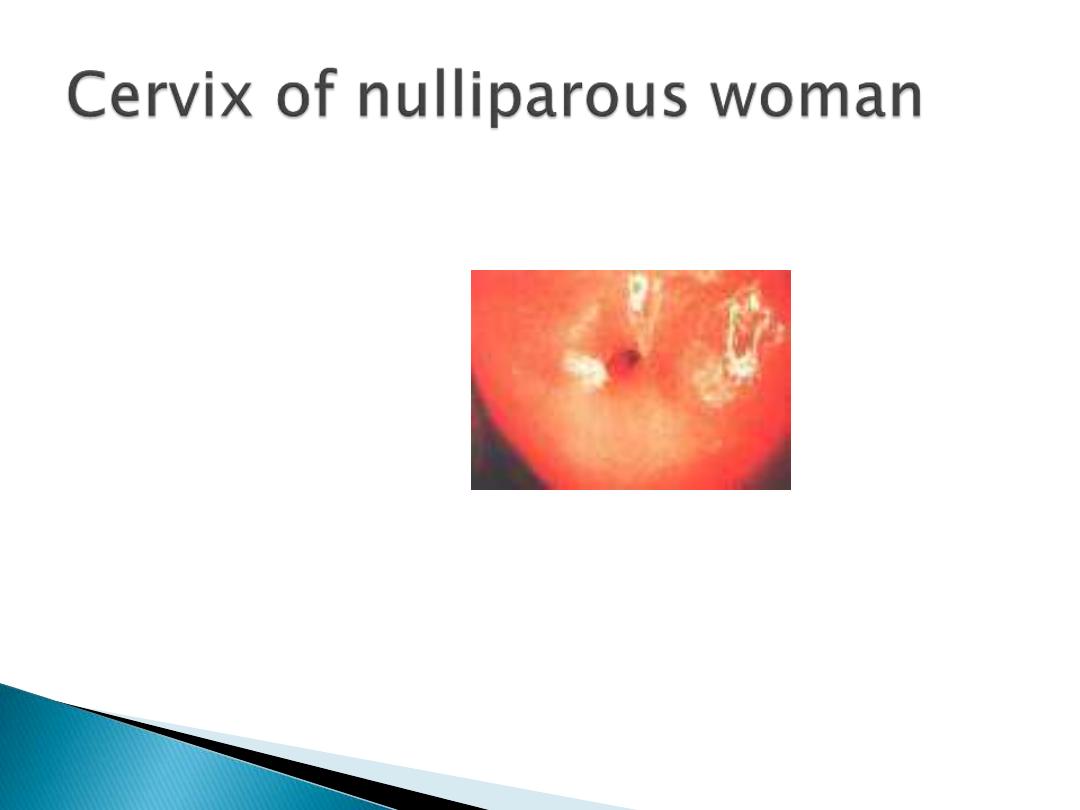
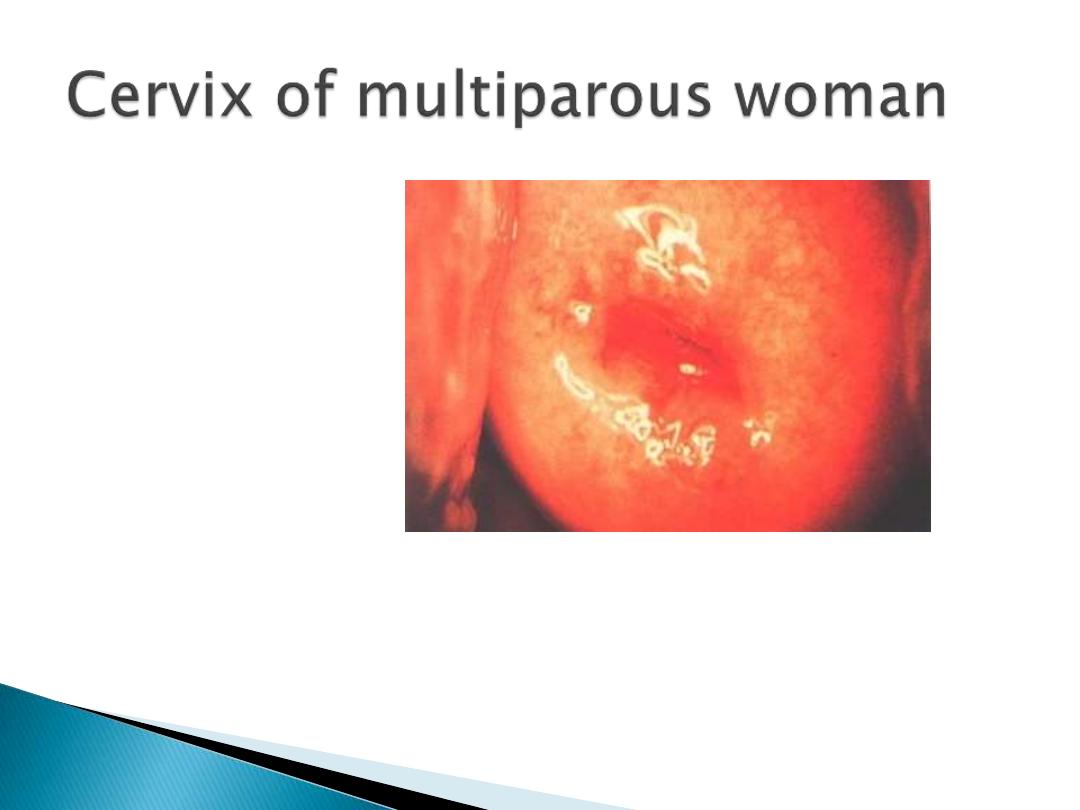
In first few days, the cervix can readily admit
two fingers , but by the end of the second
weeks the internal os should be closed.
However, the external os can remain open
permanently , giving characteristic
appearance to the parous cervix.
In the first few days , the stretched vagina is
smooth & oedematous , but by the third week
rugae begin to reappear

Lochia:
Lochia is the bloodstained uterine discharge that is composed of blood &
necrotic decidua. Only the superficial layer of decidua becomes necrotic
& is sloughed off . The basal layer adjacent to the myometrium is
involved in the regeneration of new endometrium & this regeneration is
completed by the third week.
During the first few days after delivery , the lochia is red [lochia rubra ].
LOCHIA SEROSA :serous discharge in the second week after delivery .
LOCHIA ALBA :whitish or yellow white discharge appear the second week.
Persistent red lochia suggest delayed uterine involution that is usually
associated with infection or a retained piece of placental tissue
.Offensive lochia suggest infection & should be treated with a broad-
spectrum antibiotics .Retained placental tissues associated with increase
blood loss . management includes the use of antibiotics & evacuation of
retained products.

Puerpural disorders:
1-perineal complications:
a- perineal discomfort :80% of patients, which last about 10 days .It is
greatest in women with episiotomies or tears & instrumental deliveries .
Treatment is by – local cooling.
- topical anesthesia.
-analgesia :paracetamol , diclofenac suppositories.
b-perineal infections: bacterial infection with signs of infections .
management by :-swabs for microbiological culture .
- broad spectrum antibiotics.
- if there is pus , drainage should be encouraged by
removal of any skin sutures.
c- spontaneous opening of repaired perineal tears & episiotomies :
is the result of secondary infection . The wound should be irrigated twice
daily & healing should be allowed by secondary intention .Sometimes
secondary suturing may be
required.

2- bladder complication
:
a- voiding difficulty &over-distension of the bladder :
either due to pain or peri-urethral oedema especially in
those undergoing traumatic delivery &those with multiple
lacerations or tears &those with vulvo-vaginal haematoma
.Also voiding difficulties is common in those with regional
anesthesia (epidural/spinal) because the bladder may take
up to 8 hours to regain normal sensation .Therefor urinary
catheter may be left in the bladder for the first 12-24
hours .
b-urinary incontinence :
either stress I. which is rare or true I.due to vesico-vaginal
,urethra-vaginal, or uretero-vaginal fistula .I due to fistula
usually appear in the second week when slough separate .

3- bowel complication
:
a- constipation :may be due interruption in the
normal diet &dehydration during labor .Advice on
adequate fluid intake &increase fiber intake .It
may also due to pain &fear of evacuation of the
bowel .
b- fecal incontinence :due to damage of anal
sphincter during delivery (occult damage ) .
Third &fourth degree vaginal tears are also
associated with anal incontinence .It may also
due to fistula (recto-vaginal fistula).

4- secondary post-partum haemorrhage
:
Is defined as fresh blood from the genital tract
between 24 hours &6 weeks after delivery .The
most common time of secondary PPH is 7-14
days .Causes :
1-retained placental tissues treatment is
evacuation of the uterus after antibiotics cover .
2-infection :endometritis .
3-hormonal contraception.
4-bleeding disorders e.g. von willbrand's diseas.
5-choriocarcinoma.

5-obestetric palsy
:
Is a condition in which one or both lower limbs may develop sign
of a motor &/ sensory neuropathy following delivery .the patient
present with foot drop & parasthesia .the mechanism
of injury is unknown &may be due to compression of the
lumbosacral trunk as it crosses the sacroiliac joint during
descent of the fetal head. Treatment is by bed rest , analgesia
&physiotherapy .
6-symphysis pubis diastasis :
Separation if the symphysis pubis can occur spontaneously or
surgical separation of the pubis in labor (symphysiotomy) can be
performed in cases of cephalo-pelvic disproportion to increase
pelvic diameter .Sign & symptoms include symphyseal pain ,
waddling gait , pupic tenderness &a palpable interpubic gap .
Treatment includes bed rest , anti-inflammatory agents,
physiotherapy &a pelvic corset .

7-thromboembolism :
There is a 5 folds increase in the risk of TE in
pregnancy & puerperium especially after C/S
.Management is by anticoagulant therapy .
8-puerpural pyrexia :
Is defined as temperature of 38c or higher on any two
of the first 10 days postpartum, exclusive of the first
24 hours.
In about 80% of women who develop a temperature in
the first 24 hours of vaginal delivery, no obvious
evidence of infection can be identified. The reverse
holds true for women delivering by C/S , when a
wound infection should be considered.

Diagnosis &management of PP.:
1-chest infection &pneumonia: present with cough , purulent sputum
&dyspnoea. Diagnosed by seputum M ,C&S ,CHEST X-RAY .treatment by
physiotherapy &AB.
2-tonsillitis :throat swab, AB .
3-Pyelonephritis: urine M, C&S, treatment by AB.
4-Endometritis with or without retained placental tissues :diagnosed by
pelvic U/S, treatment with AB, &uterine evacuation .
5-Deep venous thrombosis /pulmonary embolism :Doppler/ venogram of
legs, lung perfusion scan angiogram, chest x- ray ,blood gases. Treatment
with heparin .
6-mastitis &breast abscess: milk M, C&S . treatment is with AB &incision
&drainage for breast abscess.
7-wound infection .
8-meningitis : lumber puncture ,treatment with AB .

9- chest complication:
Chest complications are more likely to appear in
the first 24 hours after delivery , particularly after
general anesthesia .
1-atelactasis ;prevented with early ®ular
physiotherapy.
2-aspiration pneumonia (mandleson's syndrome
).
10-genital tract infection :
Genital tract infection following delivery is
referred to as puerperal sepsis .The incidence of
puerperal sepsis is 3%.

Aetiology of genital tract infection :
Puerperal infection is usually polymicrobial &involves contaminants from the
bowel that colonize the perineum & lower genital tract. The most identified
organisms were facultative gram-positive cocci, particularly group B
streptococcus, frequently co-exist with Mycoplasma species .
Factors that can facilitate infection:
1-following delivery , natural barriers to infection are temporarily removed &
therefore pathogenic organisms can ascend from lower genital tract into the
uterine cavity .
2-Placental separation exposes a large raw area equivalent to an open wound .
3- retained products of conception & blood clots within the uterus can provide an
excellent culture media .
4-lacerations of the genital tract , although may not need surgical repair , they
can become a focus for infection similar to iatrogenic wound such as C/S &
episiotomy .
Haemolytic Streptococcus group A &staphylococcus aureus are two exogenous
organisms that can cause puerperal infection. The toxin produced by these
organisms can result in a rapid deterioration into septicaemic shock .

Symptoms of puerperal pelvic infection :
1-malaise ,headache , fever, rigor .
2-abdominal discomfort , vomiting &diarrhea .
3-offfensive lochia .
4-secondary PPH.
Signs of puerperal pelvic infection:
1-pyrexia &tachycardia.
2-uterus-boggy, tender& large.
3-infected wound-C/S, perineal.
4-peritonism, paralytic ileus.
5-indurated adnexia .
6-bogginess in pelvis.

Investigation for puerperal genital infection:
1-full blood count :anaemia, leukocytosis, thrombocytopenia.
2-urea & electrolytes.
3-high vaginal swab &blood culture: infection screen .
4-pelvic U/S :retained product , pelvic abscess .
5-clotting screen (shock): DIC.
6-arterial blood gases: acidosis &hypoxia .
The common methods of spread of puerperal infection:
1-ascending infection from the lower genital tract or spread via the
fallopian tubes to the ovaries , giving rise to a salpingo-oophritis &
pelvic peritonitis .
2-infection may spread by contiguity directly into the myometrium &the
parametruim .
3-infection may spread via lymphatics & blood vessels .
In contrast to PID , tubal involvement in puerperal sepsis rarely cause
tubal occlusion & consequent infertility . Tubo-sepsis .

Common risk factors for puerperal infection :
1-Antenatal intrauterine infection.
2-C/S.
3-cervical cerclage for cervical incompetence .
4-prolonged labor
5-prolonged rupture of membrane.
6-multiple vaginal examination .
7-instrumental delivery.
8-manual removal of placenta .
9-retained product of conception.
10-obesity, diabetes, HIV.

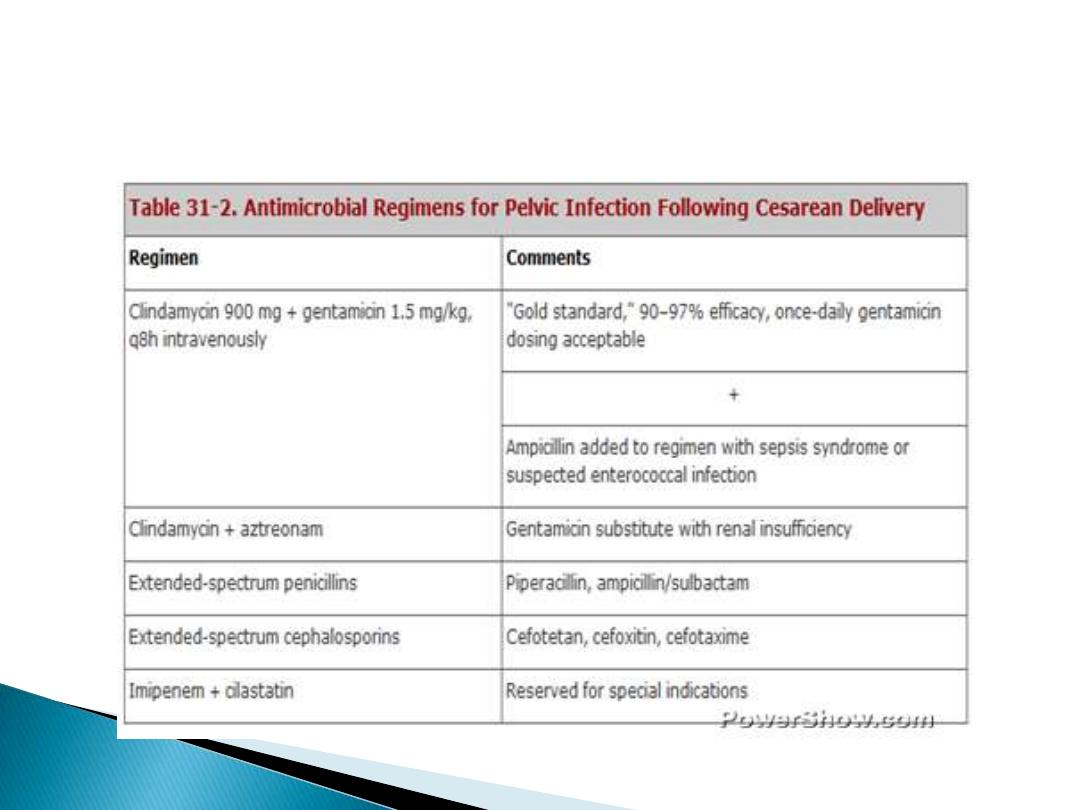
Treatment:
1- mild to moderate infection can be treated with
a broad-spectrum antibiotics e.g. cephalosporin
&metronidazole .
Depending on the severity of infection , the first
few doses should be given intravenously .
2-with sever infection , there is a release of
inflammatory &vasoactive mediators , this lead to
local vasodilatation &poor tissues perfusion
casing septic/ endotoxic shock ,&delay in
appropriate management could be fatal .

Prevention of puerperal sepsis:
1-good surgical approach .
2-use of aseptic techniques.
3-use of prophylactic antibiotics during C/S
in the form of a single intraoperative dose of
antibiotics (cephalosporin plus metronidazole
or amoxiclav )should be given after clamping
of the umbilical cord to avoid unnecessary
exposure of the baby to the antibiotics.


The breast :
Breastfeeding:
The advantage of breast feeding:
1-readily available at the right temperature &ideal
nutritional value .
2-cheaper than formula feed.
3-associated with a reduction in :
-childhood infective illness, especially gastroenteritis.
-fertility with amenorrhea .
-atopic diseases e.g. eczema &asthma.
-necrotizing enterocolitis in preterm babies .
-juvenile diabetes .
-childhood cancer, especially lymphoma .
-premenopausal breast cancer.

Breast disorders:
1-bloodstained nipple discharge.
2painful nipples .
3-calactocele.
4-breast engorgement :
Usually begins in the second or third postpartum day & if
breastfeeding has not established effectively , the over-
distended &engorged breast becomes very painful &can
give rise to puerperal fever up to 39c in 13% of patients .
Although the fever rarely lasts more than 16 hours, other
infective causes need to be excluded .
Treatment : allowing the baby easy access to the breast is
the most effective method of treatment &prevention .

5-mastitis :inflammation of the breast .
The affected segment of the breast is painful
&red &oedematous . Flu like symptoms develop
associated with pyrexia &tachycardia. In infective
mastitis the fever developed later &persist
longer. The most common infective organism is
staphylococcus aureus
. The most common
sources of infection are baby's nose or throat
.The milk should be sent for M& C&S &antibiotics
(flucloxacillin)can be commenced while awaiting
sensitivity result .
If breast abscess developed , it require drainage .

Contraception :
1- lactational amenorrhea :less than 2%in the first 6
months after delivery .
2- IUCD: it is best to wait at least 4 weeks to allow for
involution .
3-COCP:increase the risk of thrombosis &affect
breastfeeding but in patients who don't desire lactation it
should be commenced 4 weeks postpartum.
4-progestgen-only pills (mini-pills): should be
commenced about day 21 following delivery .
5-injectable contraception (depo-provera):given 3 monthly
& preferably be given 5-6 weeks post-partum.
6-Sterilization :in patients who have completed their
families , it can be performed during C/S. However, it is
better delayed until after 6 weeks postpartum , when it can
be done by laparoscopy .

Thank you
