Baghdad College of Medicine / 5
th
grade
Student’s Name :
Dr. Shatha Al-Kawaz
Lec. 1
Oesophageal Atresia &
Tracheoesophageal
Fistula
Wed. 21 / 12 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2016 – 2017
Oesophageal Atresia Dr. Shatha
21-12-2016
2
©Ali Kareem 2016-2017
Esophageal atresia and
Tracheoesophageal fistula malformation
The objectives: is to understand this complex congenital anomaly,
types, presentation how to diagnose and how to manage and
complications.
Presentation:
History and physical examination
A mother who is carrying a fetus with esophageal atresia may
have polyhydramnios
Characteristically, the neonate born with esophageal atresia drools and
has substantial mucus, with excessive oral secretions. If suckling at the
breast or bottle is allowed, the baby appears to choke and may have
difficulty maintaining an airway. If an oral tube is placed to suction the
stomach, it characteristically becomes blocked 10-11 cm from the lips.
EA is divided into two types isolated EA and syndromic .The acronym
VACTERL (vertebral defects, anorectal malformations, cardiovascular
defects, tracheoesophageal defects, renal anomalies, and limb
deformities) refers a set of associated anomalies that should be readily
apparent upon physical examination. If any of these anomalies are
present, the presence of the others must be assessed. The VACTERL
syndrome exists when three or more of the associated anomalies are
present. This syndrome occurs in approximately 25% of all patients with
esophageal atresia.
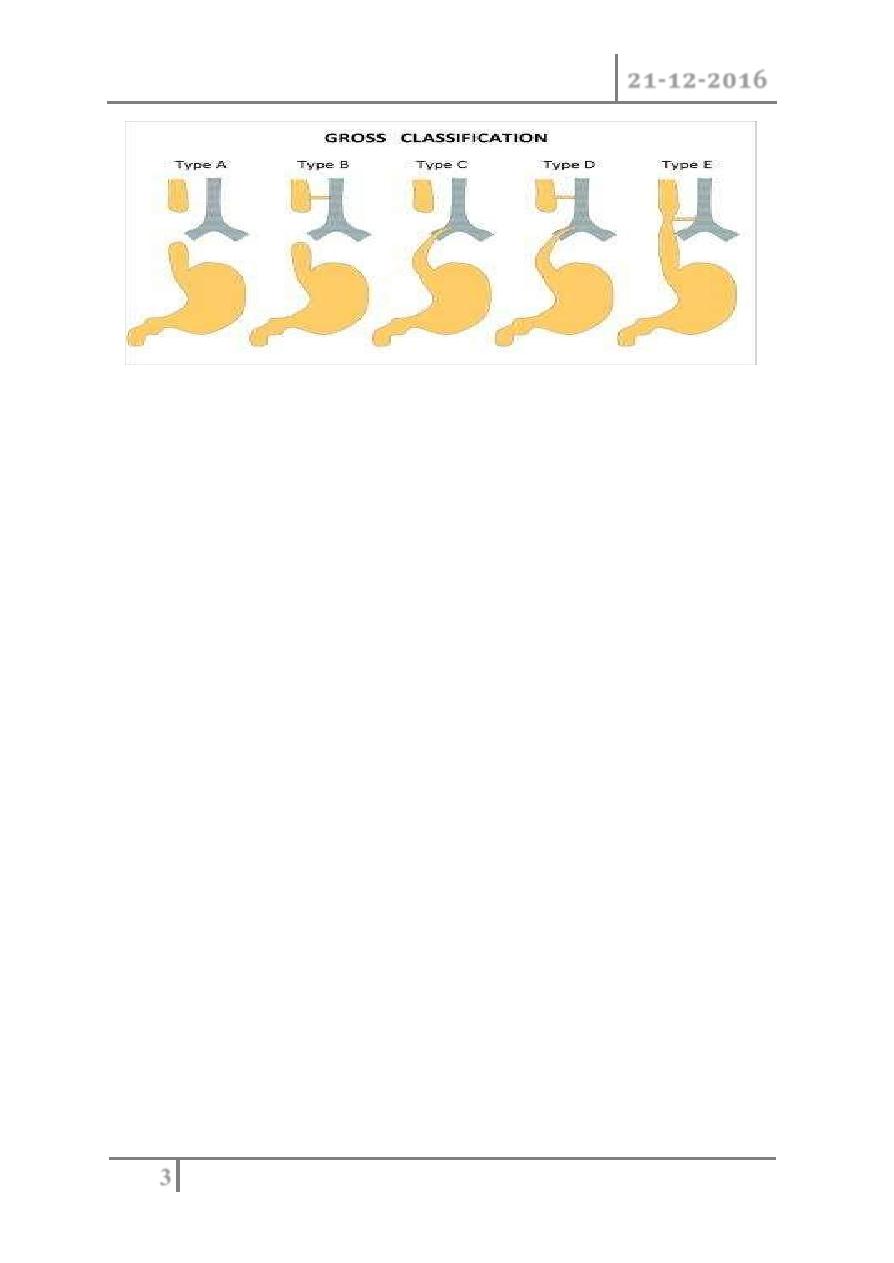
Classification
Oesophageal Atresia Dr. Shatha
21-12-2016
3
©Ali Kareem 2016-2017
The original classification system was devised by Vogt in 1929, and then
revised by Gross.
Oesophageal Atresia Dr. Shatha
21-12-2016
4
©Ali Kareem 2016-2017
1. Esophageal Atresia with Distal Fistula (Gross Type C) this is the most
common subtype, accounting for about 85% of EA anomalies. The very
dilated proximal esophagus has a thickened wall and descends into the
superior mediastinum usually to the third or fourth thoracic vertebrae.
The distal esophagus is slender and has a thin wall. It enters the
trachea posteriorly either at the level of the carina or 1
–2 cm higher.
The distance between the esophageal ends varies from very small to
quite wide.
2. Pure Esophageal Atresia without TEF (Gross Type A)
3. H-type Fistula without Esophageal Atresia (Gross Type E)
4. Esophageal Atresia with Proximal Fistula (Gross Type B)
5. Esophageal Atresia with Proximal and Distal Fistulas (Gross Type D)
DIAGNOSIS
Antenatal Diagnosis
o Ultrasonography, it relies on two nonspecific signs;
polyhydramnios and an absent or small stomach bubble, which
may be present with other fetal abnormalities.
o 3D power Doppler imaging is better diagnostic tool both
antenatally and postnatally.
o Magnetic resonance imaging (MRI) has been used to identify
other fetal thoracic lesions, and may be beneficial in patients
supposed to be at risk on prenatal ultrasound.
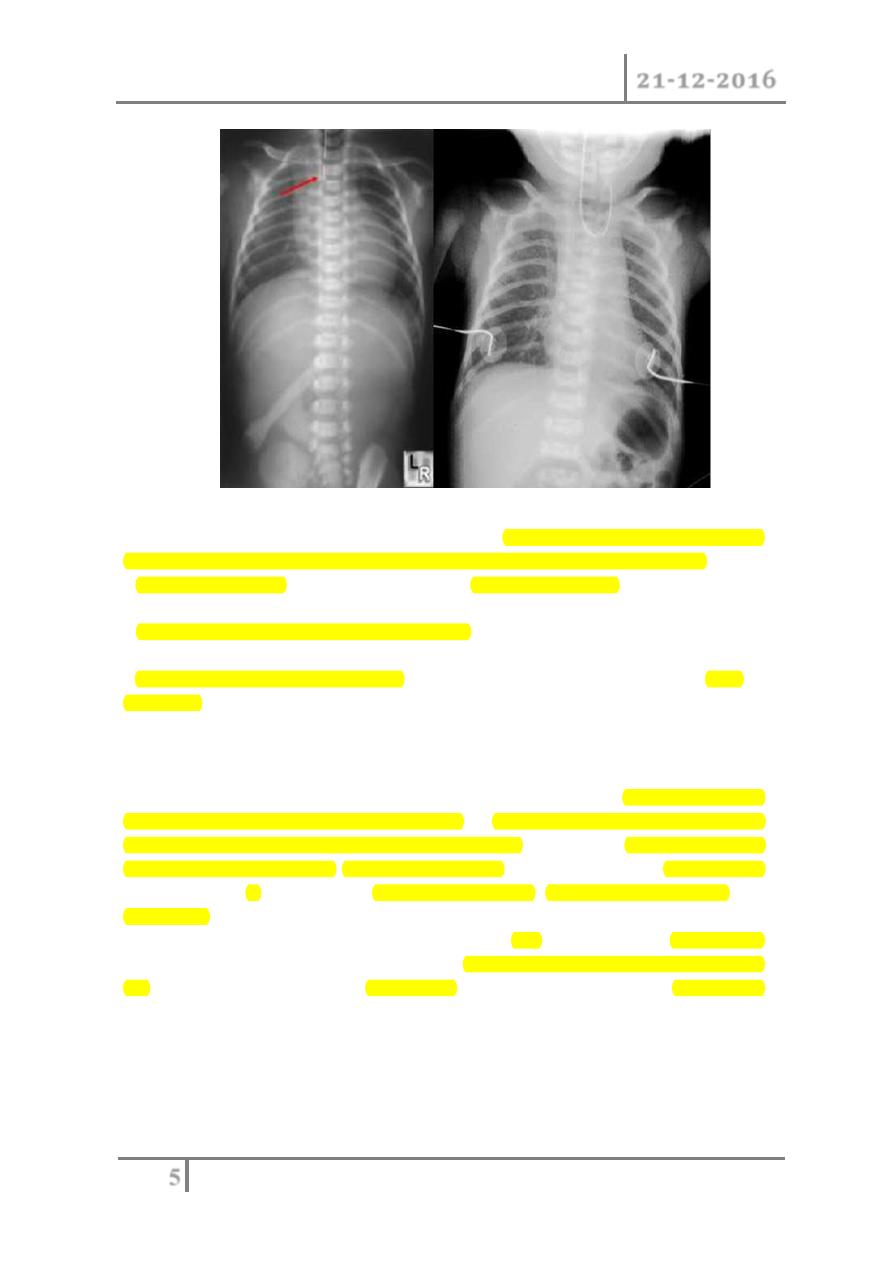
Postnatal diagnosis
If pregnancy was complicated by polyhydramnios or the neonate presents
with anomalies that fit the VACTERL association or the saliva accumulate
in the mouth; then feeding should be withheld until esophageal continuity
is confirmed. This is best done with a stiff 10 French catheter inserted
either through the nose or mouth. A chest film is then obtained. With EA,
the tip of the tube is found to be slightly curled in the blind upper pouch.
The presence of air in the stomach signifies the presence of a distal TEF.
Oesophageal Atresia Dr. Shatha
21-12-2016
5
©Ali Kareem 2016-2017
If there is any question about the diagnosis, a small amount of contrast can be
dripped into the upper pouch, but this needs to be done with fluoroscopy.
Echocardiography should be performed prior to operation as it may reveal
cardiac and/or aortic arch anomalies
Renal ultrasound and spine radiographs should be obtained as
well.
MRI and CT of neck and chest are the best two imaging modality; MRI is
preferred for its absence of radiation.
MANAGEMENT
Preoperative
Once the diagnosis of EA has been established, the baby should be
transferred to a pediatric surgical center. A 10 French tube is placed in the
upper esophagus and set to continuous suction. The child is positioned head-
up and on his or her side. Intravenous access is important, and the vital signs
are monitored. If the child is in respiratory distress, endotracheal intubation and
ventilation may be needed.
Generally, the operative treatment of EA/TEF is not regarded as an emergency
procedure. Thus, there is usually time to confirm the diagnosis and to assess
for
associated
anomalies.
Oesophageal Atresia Dr. Shatha
21-12-2016
6
©Ali Kareem 2016-2017
Operative repair aim to close the fistula and to restore the continuity of
the esophagus
Esophageal Atresia without Distal Fistula
A gasless abdomen is a sign of EA without distal fistula.
The initial treatment is a gastrostomy once placed; bolus feedings should be
instituted to enlarge both the small stomach and the distal pouch.
Delayed primary repair sometime is feasible; if not an alternative procedure
should be considered, such as a gastric pull-up or a jejunal, ileal, or colonic
interposition.
COMPLICATIONS
o Anastomotic Leaks.
o Anastomotic stricture.
o Recurrent Tracheoesophageal fistula.
o Tracheomalacia.
o Disordered Peristalsis/Gastroesophageal Reflux.
#END of this Lecture …
**Note : For all lectures I do(the previous lectures also) , always check the slides to
see all the pics because the lecture contain some of them.
Best Regards
