Baghdad College of Medicine / 5
th
grade
Student’s Name :
Dr. Shatha Al-Kawaz
Lec. 3
Abdominal wall defect in
neonate
Wed. 28 / 12 / 2016
DONE BY : Ali Kareem
مكتب اشور لالستنساخ
2016 – 2017
Abdominal Wall defect Dr. Shatha
28-12-2016
2
Congenital abdominal wall defects
Objectives: to study the neonatal abdominal wall defect,
embryology, etiology, diagnosis, how to differentiate between
omphalocele and gastroschisis and management.
Abdominal wall defects are divided into omphalocele and gastroschisis. The
incidence in live birth is approximately 1 in 4000.
The abdominal wall forms during the 4
th
week of gestation from
differential growth of the embryo causing infolding in the craniocaudally
and mediolateral direction. The lateral abdominal folds of the embryo
meet in the anterior midline and surround the yolk sac eventually
constricting the yolk sac into yolk stalk that becomes the umbilical cord.
During the 6
th
week of gestation rapid growth of the intestine causes
herniation of the midgut into the umbilical cord. Elongation and rotation
of midgut occurs. By week 10, the midgut has returned to the abdominal
cavity.
An omphalocele occurs if the intestine fails to return to the
peritoneal cavity.
The etiology of gastroschisis less clear, many theories
1. Failure of mesoderm to form in the anterior abdominal wall.
2. Failure of lateral folds to fuse in the midline leaves a defect to the
right side of the umbilicus.
3. Thrombosis of the right omphalomesenteric vein (umbilical vein)
causing necrosis to the surrounding abdominal wall leading to right
side defect.
4. Rapture of an omphalocele in utero
Abdominal Wall defect Dr. Shatha
28-12-2016
3
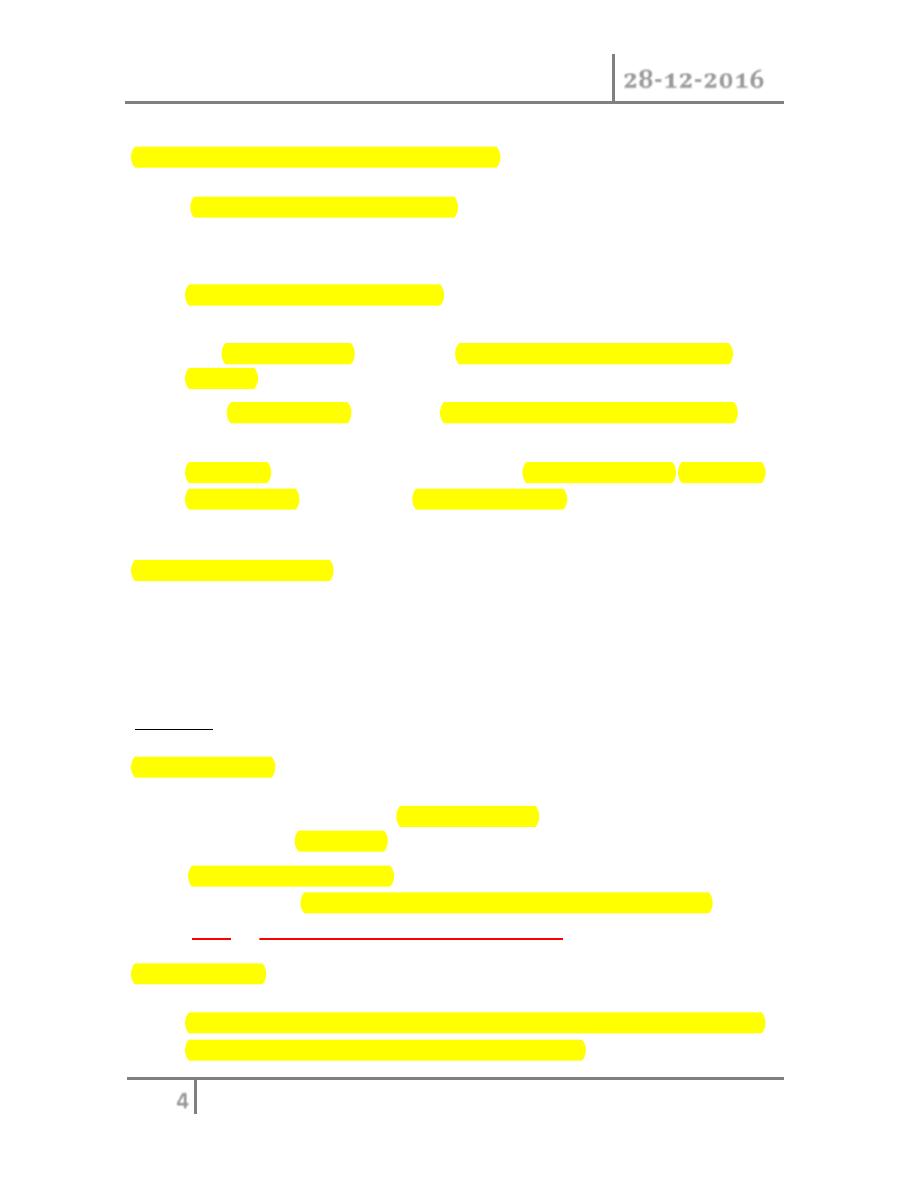
Differentiating Characteristics between Gastroschisis and Omphalocele
Characteristic
Omphalocele
Gastroschisis
Herniated
viscera
Bowel ± liver
Bowel only
Sac
Present
Absent
Associated
anomalies
Common (50%)
Uncommon (<10%)
Location
of defect
Umbilicus
Right of umbilicus
Mode of
delivery
Vaginal/cesarean
Vaginal
Surgical
management
Nonurgent
Urgent
Prognostic
factors
Associated anomalies
Condition of bowel
Diagnosis
o U/S these two conditions are often diagnoses on prenatal
ultrasonography and are easily differentiated by the location of
the defect and by the presence or absence of a sac surrounding
the eviscerated bowel.
o Elevation of maternal α-feto protein
Gastroschisis:
Perinatal care:
Due to prolong exposure of the bowel of a neonate with gastroschisis
to the damage effect of amniotic fluid, bowel edema, poor motility and
malabsorption is noticed significantly.
The delivery for fetuses with gastroschisis is better to be carried in tertiary
perinatal center so as to provide immediate neonatal and pediatric
surgical experience.
Abdominal Wall defect Dr. Shatha
28-12-2016
4
Neonatal resuscitation and management:
o Intravenous fluid resuscitation, the neonates with gastroschisis have
significant evaporative water loss from the open abdominal cavity
and exposed bowel.
o Nasogastric decompression to prevent gastric and
intestinal distension.
o The herniated bowel should be wrapped in warm saline soaked
gauze.
o The infant placed with the bowel and legs in a plastic bag to
reduce evaporative losses.
o Although gastroschisis most often is an isolated anomaly, thorough
examination of the neonate should be done to exclude the
coexistence of other congenital anomalies.
Surgical management:
The primary goal is to return the viscera to the abdominal cavity while
minimizing the risk of damage to the viscera due to direct trauma or to
increased intra abdominal pressure.
Options
Primary closure
o Is practiced for neonate when reduction of the herniated viscera is
thought to be possible
o Or using the prosthetic options when primary fascial closure cannot
be achieved, non-absorbable mesh or bioprosthetic material such as
dura or porcine small intestinal sub mucosa can be used.
Staged closure
Consist of placing the bowel into a prefabricated silo with a circular
spring that is positioned under fascial opening. Can be inserted at
Abdominal Wall defect Dr. Shatha
28-12-2016
5
delivery room or bedside without general anesthesia, the bowel is
reduced once or twice daily into the peritoneal cavity, when the reduction
is completed the definitive closure can be performed. This process takes
between 1-14 days.
This procedure is used to avoid ischemic injury to the viscera due
to the high intra-abdominal pressure.
Postoperative course
o Enteral feeding is delayed for few weeks while awaiting return
of bowel function.
o Nasogastric decompression.
o Parenteral nutrition.
o Prokinetics for treatment of GIT dysmotility e.g
erythromycin, metoclopramide, domperidone, cisapride.
The long term outcomes for patients born with gastroschisis are
generally excellent.
The presence of bowel atresia is the most important prognostic
determinant for poor outcome.
Omphalocele
Perinatal care
o Mode of delivery should be decided by the obstetrician. But in
giant omphalocele cesarean section is preferable because of the
fear of liver injury.
o Delivery at a tertiary center is preferable for immediate access
to neonatal and pediatric surgical expertise.
Neonatal resuscitation and management
o
A thorough search for associated anomalies should be
Abdominal Wall defect Dr. Shatha
28-12-2016
6
done,(cardiac evaluation ,renal, neonatal hypoglycemia for
possibility of Bechwith- Weidemann syndrome ,and blood sample
for genetic evaluation if indicated.
o Intravenous access and fluid resuscitation, infants with omphalocele
do not have as significant fluid and temperature losses as those with
gastroschisis but the loss are higher than those with intact
abdominal wall.
o The omphalocele itself can be dressed with saline soaked gauze to
minimize those losses.
o Nasogastric tube.
Surgical management
Treatment options depend on the size of the defect, gestational age
and the presence of associated anomalies.
Immediate primary closure: is used in infants with small defects or
larger but still easy to close.
Staged neonatal closure : this method utilize the existing amnion sac
with serial inversion, or the sac is excised and replaced with mesh and
then closed over time.
Delayed staged closure:
Used for large omphalocele, the sac is excised and a silastic silo is used
with serial reduction similar to that of gastroschisis.
Scarification treatment
Non operative technique is used for neonates who can't tolerate operation
or the defect is too large that initial repair will result in potential life-
threatening abdominal compartment syndrome. So an agent is used that
allows an eschar to develop over the intact amnion sac. This eschar will
epithelialize over time leaving ventral hernia that require repair later in
life. Iodine, silver sulfadiazine, and neomycin ointment is use
Abdominal Wall defect Dr. Shatha
28-12-2016
7
Postoperative course
o Most of patients require mechanical ventilation after primary
closure for few days.
o Nasogastric tube for gastric decompression.
o feeding can begin when nasogastric tube output is no longer
bilious and bowel activity has occurred
o antibiotics for 48 hours (if there is no infection)
o If a hernia develops, closure usually can be done after age of
one year.
Post-operative complications
1. increase intra abdominal pressure
2. acute hepatic congestion
3. renal failure
4. bowel infarction
UMBILICAL HERNIA
The objective: to understand the embryology, anatomy, incidence,
natural history, management and complications of umbilical hernias in
children.
Umbilical hernia is a common disorder in children that pediatric
and general surgeons are frequently asked to evaluate and treat.
Anatomy
After birth, closure of the umbilical ring is the result of complex
interactions of lateral body wall folding in a medial direction, fusion
of the rectus abdominis muscles into the linea alba, and umbilical
Abdominal Wall defect Dr. Shatha
28-12-2016
8
orifice contraction . Failure of these closure processes results in
umbilical hernia. The hernia sac is peritoneum, which is usually very
adherent to the dermis of the umbilical skin. The actual fascial
defect can range from several millimeters to 5 cm or more in
diameter. The extent of skin protrusion is not always indicative of
the size of the fascia
defect. Thus, it is important to palpate the
actual fascia defect by reducing the hernia to assess whether
operative or nonoperative treatment is appropriate.
Incidence
The incidence of umbilical hernia in the general population varies
with age, race, gestational age, and coexisting disorders.
Premature and low birth weight infants have a higher incidence than
full-term infants. Infants with certain other conditions, such as
Beckwith–Wiedemann syndrome, Hurler syndrome, various trisomy
conditions (trisomy 13, 18, and 21), and congenital hypothyroidism, also
have an increased incidence.
Treatment:
o Most of the umbilical hernias will close spontaneously. It seems
very safe to observe the hernia until ages 3 to 4 years to allow
closure to occur. Pressure dressings and other devices to keep the
hernia reduced do not enhance the closure process and may
result in skin irritation and breakdown.
o The primary danger associated with observation therapy is the
possibility of incarceration or strangulation although it is rare;
Patients with small fascial defects (0.5–1.5 cm in diameter)
appear more prone to incarceration.
o The operative closure of an umbilical hernia is generally
straightforward, and can usually be completed as an outpatient
Abdominal Wall defect Dr. Shatha
28-12-2016
9
procedure. Methods used commonly in the adult, such as
prosthetic placement, are almost never needed in the child;
fascial defect is closed by interrupted sutures of nonabsorbable
material in transverse direction. Excision of the redundant skin is
usually not performed because it tends to return to its normal
appearance.
Inguinal hernia and hydrocele
Objectives: to study inguinal hernia and hydrocele in pediatrics,
its incidence, embryology, presentation, diagnosis and treatment.
Inguinal hernia repair is one of the most common operations performed
by pediatric surgeons; an inguinal hernia in a child usually refers to an
indirect inguinal hernia
INCIDENCE
o Approximately 1–5% of all children will develop an inguinal hernia
and a positive family history is found in about 10%.
o There is an increased incidence in twins, more frequently in male
twins. Male to- female ratio was 5 to 1.
o Right-sided hernias were twice as common as those on the left.
o The incidence of an inguinal hernia varies directly with the degree
of prematurity
EMBRYOLOGY
The processus vaginalis is a peritoneal diverticulum extending through
the internal inguinal ring into the inguinal canal. It can be seen by 3
months of fetal life, the gonads are attached to the scrotum by the
Abdominal Wall defect Dr. Shatha
28-12-2016
10
gubernaculum in the male and to the labia via the round ligament in the
female. Gonadal descent begins by 3 months gestation, the testis begins
to descend down the canal by the seventh month of fetal life preceded
and guided by the processus vaginalis. The processus, which is located
anterior and medial to the cord structures, gradually obliterates, also
closes by 7 months of fetal life
Failure of obliteration may result in a variety of inguinal-scrotal
anomalies, including complete persistence result in scrotal hernia, distal
processus obliteration and proximal hernia patency, complete patency
with a narrow opening at the internal ring referred to as a
communicating hydrocele
CLINICAL PRESENTATION
o Most hernias are asymptomatic except for inguinal bulging with
straining. They are often found by the parents or pediatrician on
routine physical examination. The diagnosis is clinical and
depends on the history and physical examination
o The differential diagnosis includes a retractile testis,
lymphadenopathy, hydrocele, and prepubertal fat.
o Ultrasonography (US) can be used to identify a PPV indirectly via
widening of the internal inguinal ring the technique is highly
operator dependent.
o Inguinal hernia is a high risk hernia, particularly in early infancy,
as it is complicated by incarceration, occasionally leading to
intestinal obstruction and strangulation.
o In young infants with undescended testes and associated hernia,
the testis is sometimes at risk of torsion or atrophy caused by
compression of the vascular supply by a hernia sac filled with
bowel at the level of the internal inguinal ring

Abdominal Wall defect Dr. Shatha
28-12-2016
11
Incarceration
o The incidence of incarceration is highest in the youngest
patients, particularly premature infants and infants under
the age of one year.
o Symptoms of incarceration are frequently manifested as a
fussy or inconsolable infant with intermittent abdominal
pain and vomiting. A tender and sometimes erythematous
irreducible mass is noted in the groin. Abdominal distention
is a late sign, as are bloody stools.
Indication for surgery
Because of the high rate of complications associated with inguinal hernia
,there is no place for conservative management except in an instance of
an isolated hydrocele of the tunica vaginalis , spontaneous involution
often occur at 6-12 month of age. As long as the hydrocele does not
change in size, this can be observed. All other inguinal scrotal anomalies
require surgical intervention.
Pediatric indirect inguinal hernias are usually repaired through an
inguinal crease incision the sac is clamped and divided. A high ligation
is performed after the sac is opened and inspected. Mesh or prosthetic
materials are almost never required in children.
#END of this Lecture …
**Note : For all lectures I do(the previous lectures also) , always check the slides to
see all the pics because the lecture contain some of them.
Best Regards
