Mineral trioxide aggregate (MTA)
is a biomaterial that hasbeen investigated for endodontic
applications since the early 1990s
By Dr. Balsam M. Mirdan
approval for endodontic use by the U.S. Food and Drug Administration in 1998
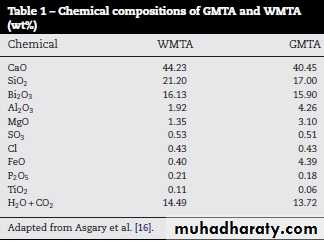
CHEMICALLYmixture of a refined Portland cement
bismuth oxide
contain trace amounts of SiO2, CaO, MgO, FeO, K2SO4, Al2O3 and Na2SO4
MTA is an endodontic cement that is extremely biocompatible, capable of stimulating healing and
osteogenesis, and is hydrophilic.
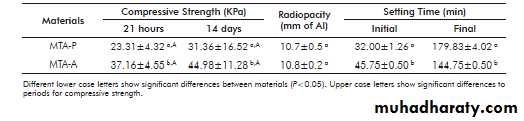
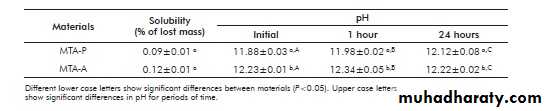
PHYSICAL PREOPERTIES
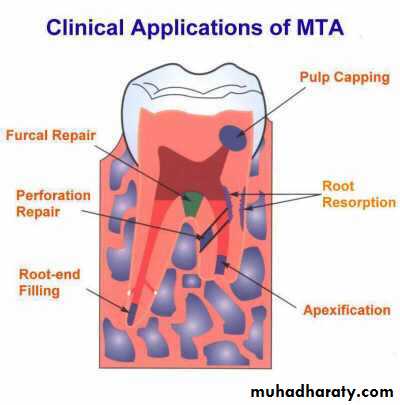
Indications
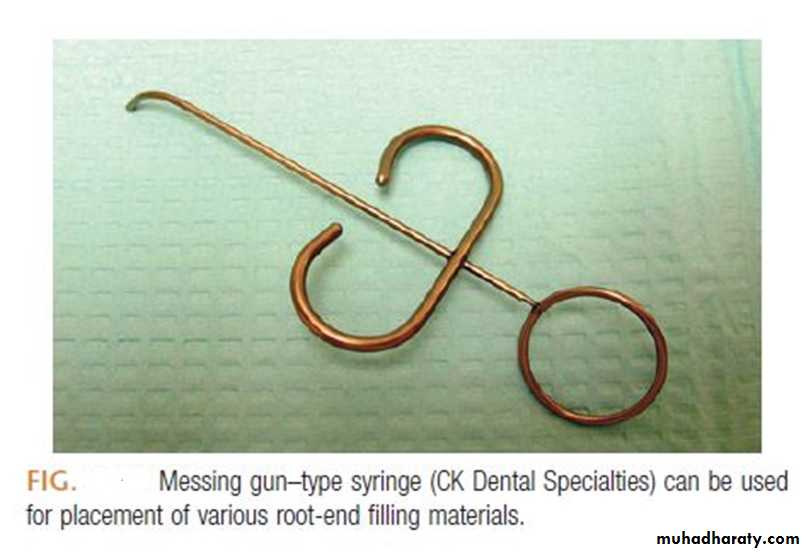
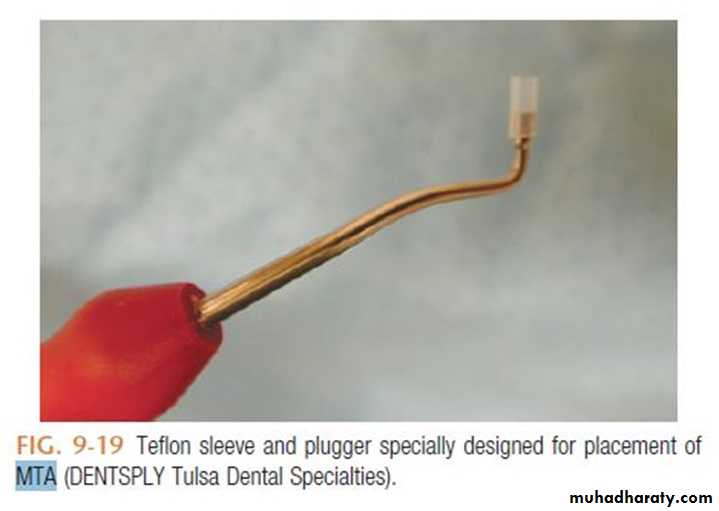
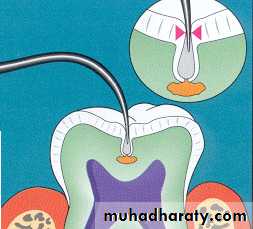
MTA has been used in both surgical and non-surgical applications including;1. Root end fillings
2. Direct pulp capping
3. Perforation repairs in roots or furcation
4. Apexification, etc.
It’s also useful for the troublesome problems of strip perforations and perforating resorptive defects.
MTA may be ideal material for use against bone, because it’s the only material that consistently allows for the overgrowth of cementum and formation of bone and may facilitate the regeneration of periodontal ligament
Contraindications
The material is not recommended for obturation of primary teeth that are expected to exfoliate since the material is slowly absorbed, if at all.Disadvantage
________??????????
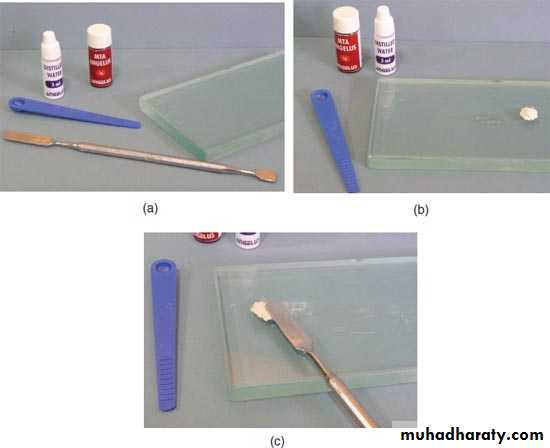
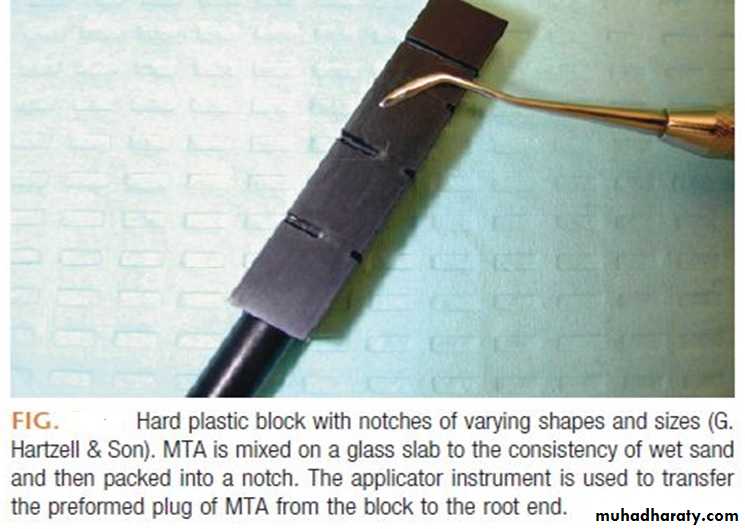
Mixing MTA
• Prepared immediately before use. Kept always in closed containers or free from moisture.• Powder: Water = 3: 1.
• Glass or paper slab used for mixing with – plastic / metal spatula.
•
MECHANISM OF ACTION:
From the time that MTA is placed in direct contact with human tissues, it appears that the material does the following3• Creates an antibacterial environment by its alkaline pH
• Modulâtes cytokine production
• Encourages differentiation and migration of hard tissue-producing cells and
• Forms HA (or carbonated apatite) on the MTA surface and provides a biologic seal.
INTRODUCTION TO LASERS
BYDr. Balsam M. Mirdan
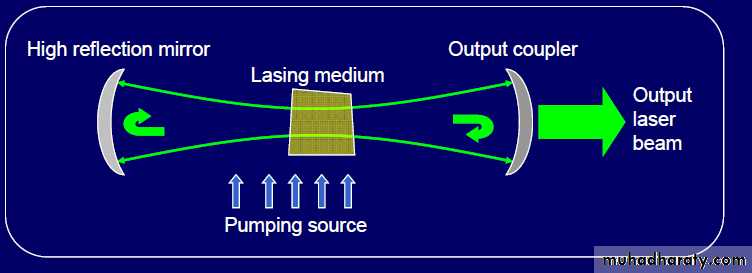
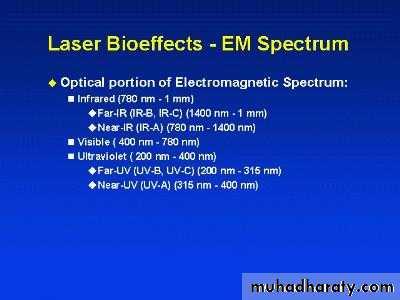
Lasers are devices that generate or amplify coherent radiation at frequencies in the infrared, visible, or ultraviolet regions of the electromagnetic spectrum.
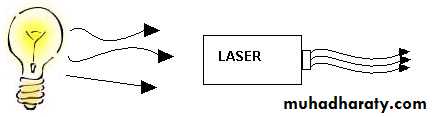
Incandescent vs. Laser Light
Many wavelengths
MultidirectionalIncoherent
Monochromatic
Directional
Coherent
In short
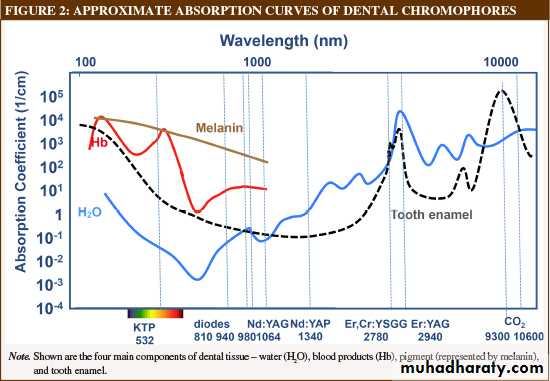
There are factors affects the inter action between laser used and tissues these are:Tissue side;
• Absorption coefficient, scattering coefficient and the refractive index of the tissue to the incident wavelength.
2. Temperature of the tissue.
3. the chemical contained in the tissue.
Laser side;
• Wavelength• Intensity
• Mode of operation
• Pulse duration
• Repetition rate
• Irradiated area
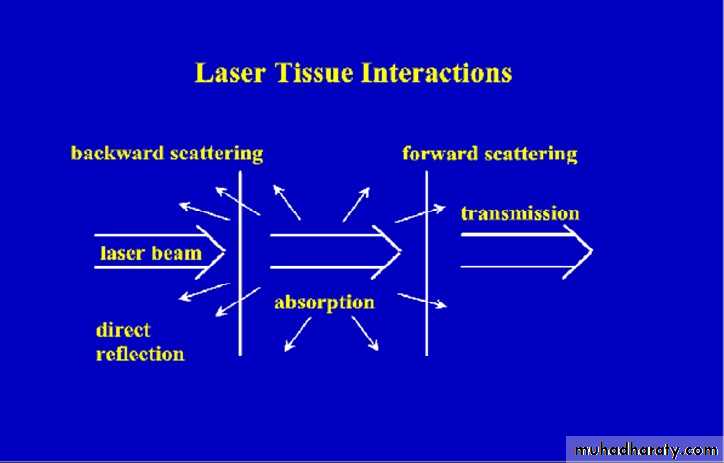
INCIDENT
LIGHTREFLECTION
TRANSMISSIONABSORPTION (A)
SCATTERING(S)
Laser tissue interaction
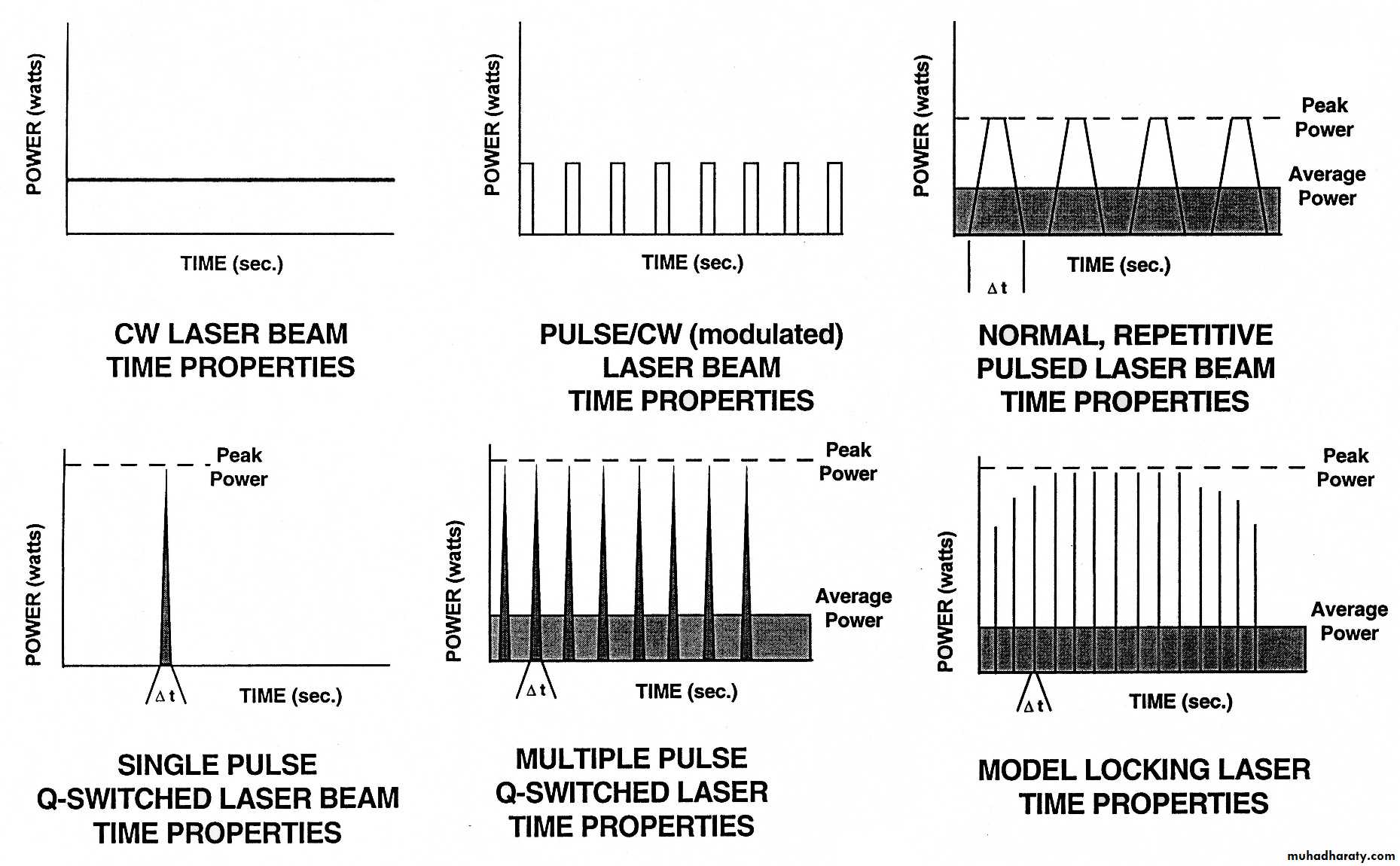
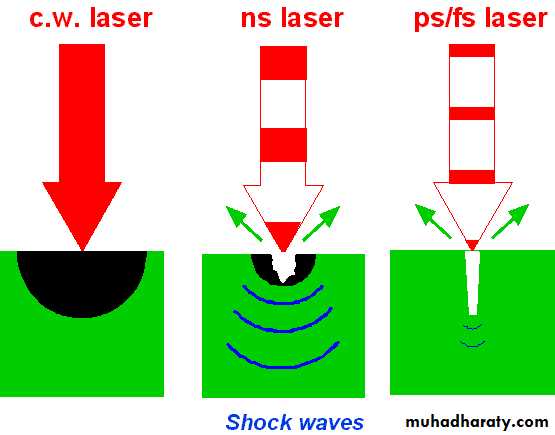
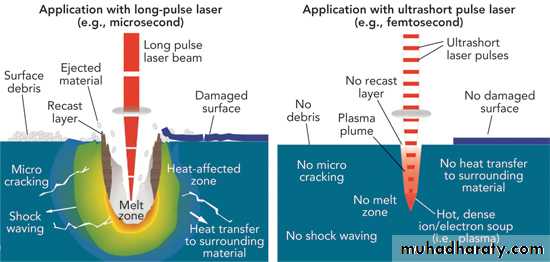
Continuous vs. Pulsed Lasers
Thinner pulses give higher peaks for same average Power.
Δτ=ms,μs
λ=IRλ=VIS,UV.
Δτ=ps,fs
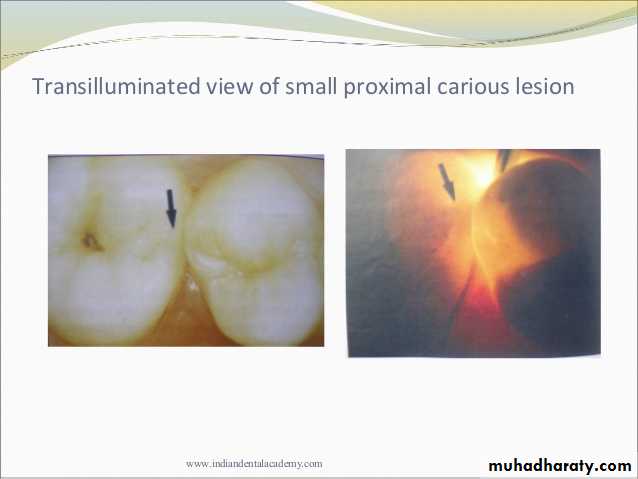
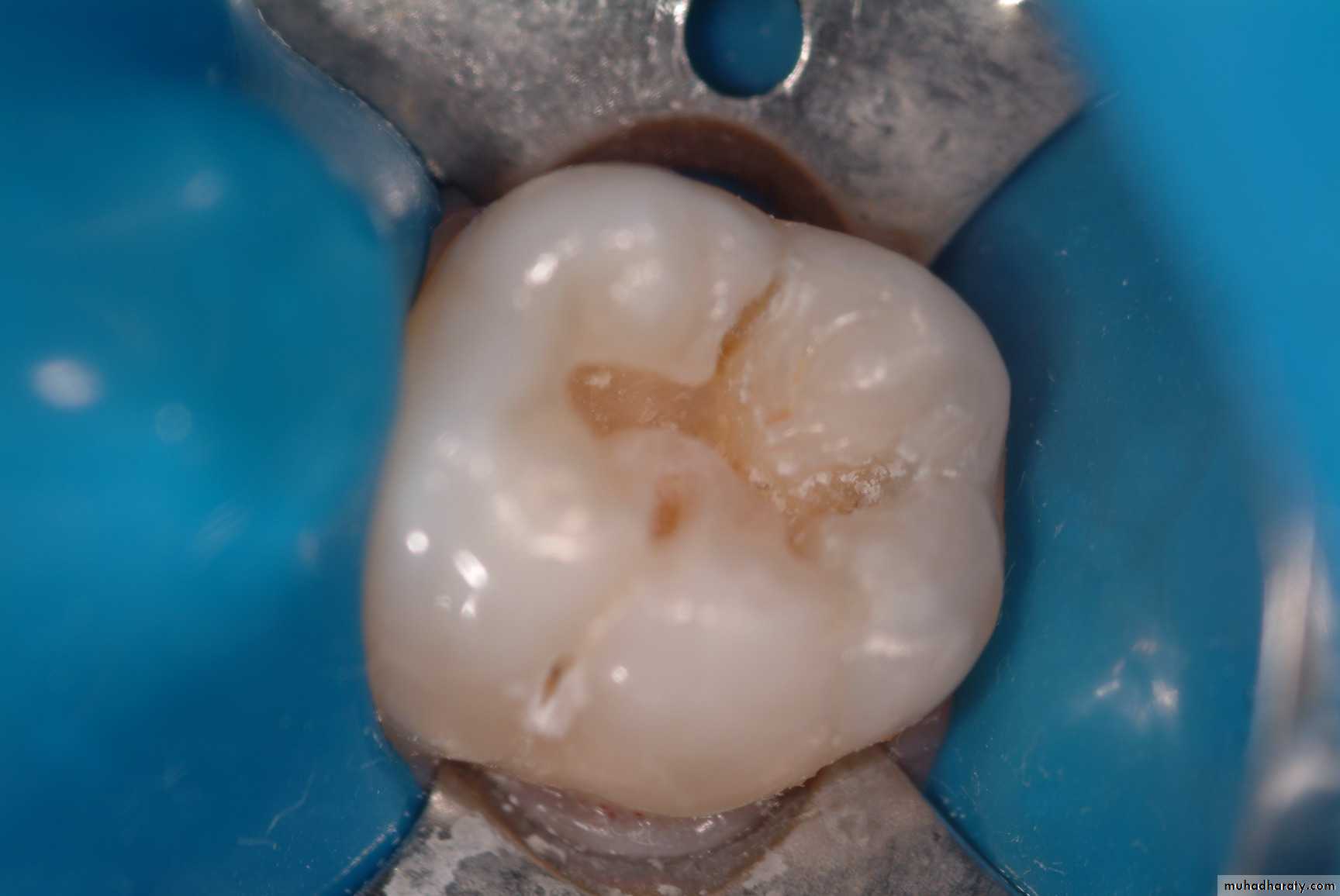
Diagnosis Of Dental Caries
Reflectance diffused reflection disturbs the diagnosis
Earliest caries detection, traditionally by use of mirror and light, as well as bitewing radiographs, can now be aided by new innovations in dental magnification and imaging, laser fluorescence and quantitative light-induced fluorescence.
Fluorescence of teeth started at 1911 by Stabll using the UV. light
Source
350nm, 410nm and 530nmFluorescence
427480
580
Higher intensity in caries region
blue light excitation
400nmVisible
High fluorescence in sound tooth structure the demineralized region appear dark
Amount of mineral loss are correlated strongly to loss of fluorescence
Red light excitation
655nm700nm-800nm
Healthy tooth structure shows
little or no fluorescence,
red fluorescence is proportional to
severity of tooth decay
Laser in Conservative Dentistry
CARBONDIOXIDE LASER- WAVELENGTH: 10.6um
DENTIN DESENSITIZATION
ARGON LASERS
- WAVELENGTH: 488,514.5um
- USES: CURING , SOFT TISSUE DESENSITIZATION
.Nd:YAG [NEODYMIUM:YTTRIUM-ALLUMINIUM
GARNET] LASER
- WAVELENGTH: 1.064um
- USES: SOFT TISSUE DESENSITIZATION , ANALGESIA
TOOTH WHITENING , PERIODONTICS,
ENDODONTICS
ERBIUM[Er]:YAG LASER
- WAVELENGTH: 2.94um- USES: HARD TISSUE
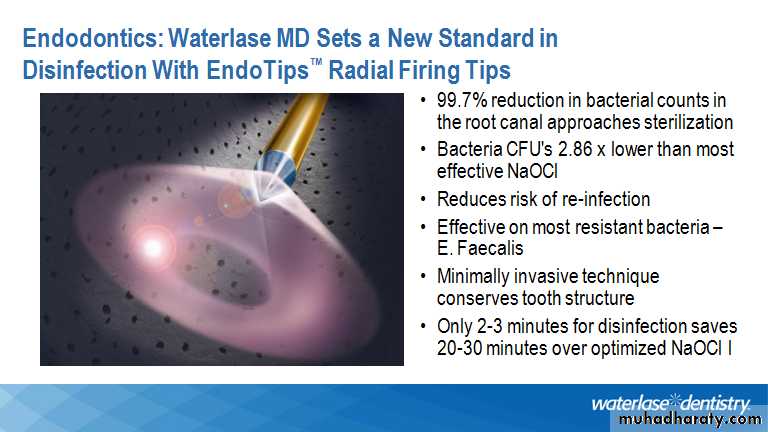
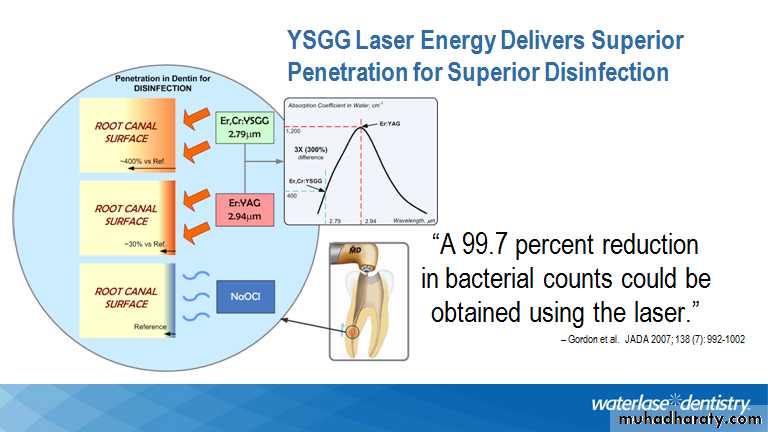
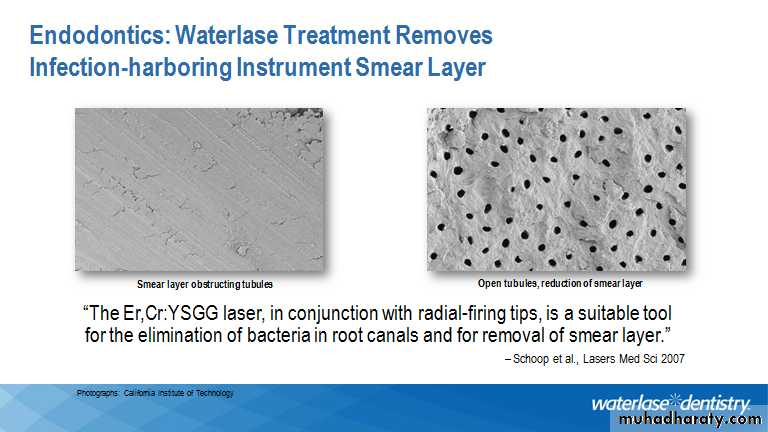
ERBIUM-CHROMIUM[Er-Cr]:YSGG LASER
- WAVELENGTH: 2.79um- USES: HARD TISSUE
DIODE
- WAVELENGTH: 800-830nm and 940, 980nm- USES:SOFT TISSUE , PERIODONTICS
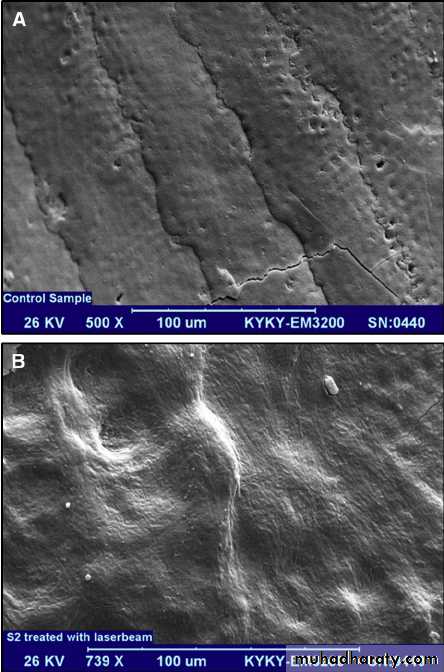
Effect on carious lesions
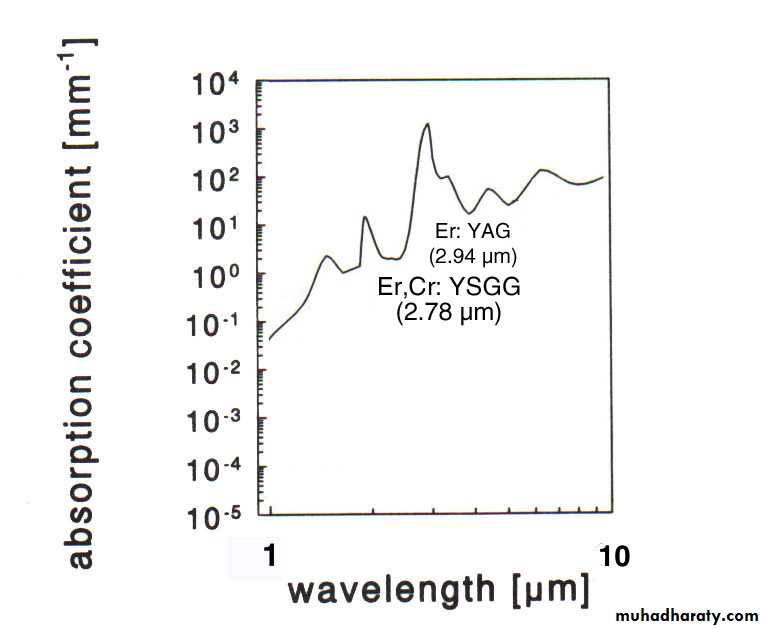
Absorption in Water
Reference source: Optical-Thermal Response of Laser Irradiated Tissue by Ashley J. Welch et al., 1996
300 %
Difference
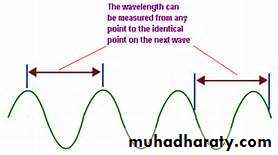
• Wavelength
Laser Parameters
x 1,000,000
Soft tissue coagulation is much better with Er:Cr:YSGG vs. Er:YAG (less bleeding)
Efficient excitation of bigger volume of water with Er:Cr:YSGG vs. Er:YAG
• Wavelength
ADVANTAGES OF LASERS
(1).Minimal damage to surrounding tissues.(2).Haemostatic effect by sealing blood vessels.
(3).Reduction of postoperative inflammation &edema.
(4).Little postoperative scarring.
(5).Reduction in postoperative pain sensation
since nerve endings are blocked.(6).Dressing & suturing is not required for
wound closer.(7).Operating time is reduced.
(8).Sterilization of wound due to reduction inin amount of microorg. exposed to laser
irradiation.
(10).Excellent wound healing.
(11).Laser exposure to tooth enamel causesreduction in caries activity.
DISADVANTAGES OF LASERS
(1).Laser beam could injure the patient or operatorBy direct beam or reflected light, causing retinal
burns.
(2).It available only at big hospital & treatment is
very expensive.(3).Specially trained person is needed.
Maintenance needed frequently and it is expensive