1
HEAD INJURY
Incidence:
Head injury is a major cause of morbidity and mortality and is more in male than female.
Head injury is one of the most common reasons for attending emergency department.
Head injury is a major cause of death in working age group (age 15-45 years).
Types of head injury:
a. Blunt (Closed) Head Injuries: e.g.
Road traffic accidents (RTA).
Fall from height (FFH).
b. Penetrating Head injuries: including:
Low Velocity Injuries like Stab injuries.
High Velocity Injuries such as gunshots and shrapnel injuries.
Mechanism of head injury:
A. Contact Injuries:
caused by forces that occur during impact, and include:
1. Linear skull fractures.
2. Depressed skull fractures.
3. Basilar skull fractures.
4. Vascular damage (Extradural haematoma).
5. Coup contusions: result from trauma at the site of impact.
6. Countercoup contusions: remote from the site of the impact.
B.
Head Motion (Inertial) Injuries:
acceleration deceleration injuries ACDC
1. Translational acceleration.
2. Rotational acceleration.
Primary vs. Secondary Brain Injuries:
Primary Brain Injury: occurs at the time of impact.
Secondary Brain injuries: occurs late on is often preventable.
Skull fractures
Focal brain injury
Diffuse brain injury
1) Vault fracture
A. Linear
B. Depressed
2) Basilar fracture
1) Contusion
2) hemorrhage
epidural
subdural
intracerebral
subarachnoid
1) concussion
2) diffuse axonal
injury
2
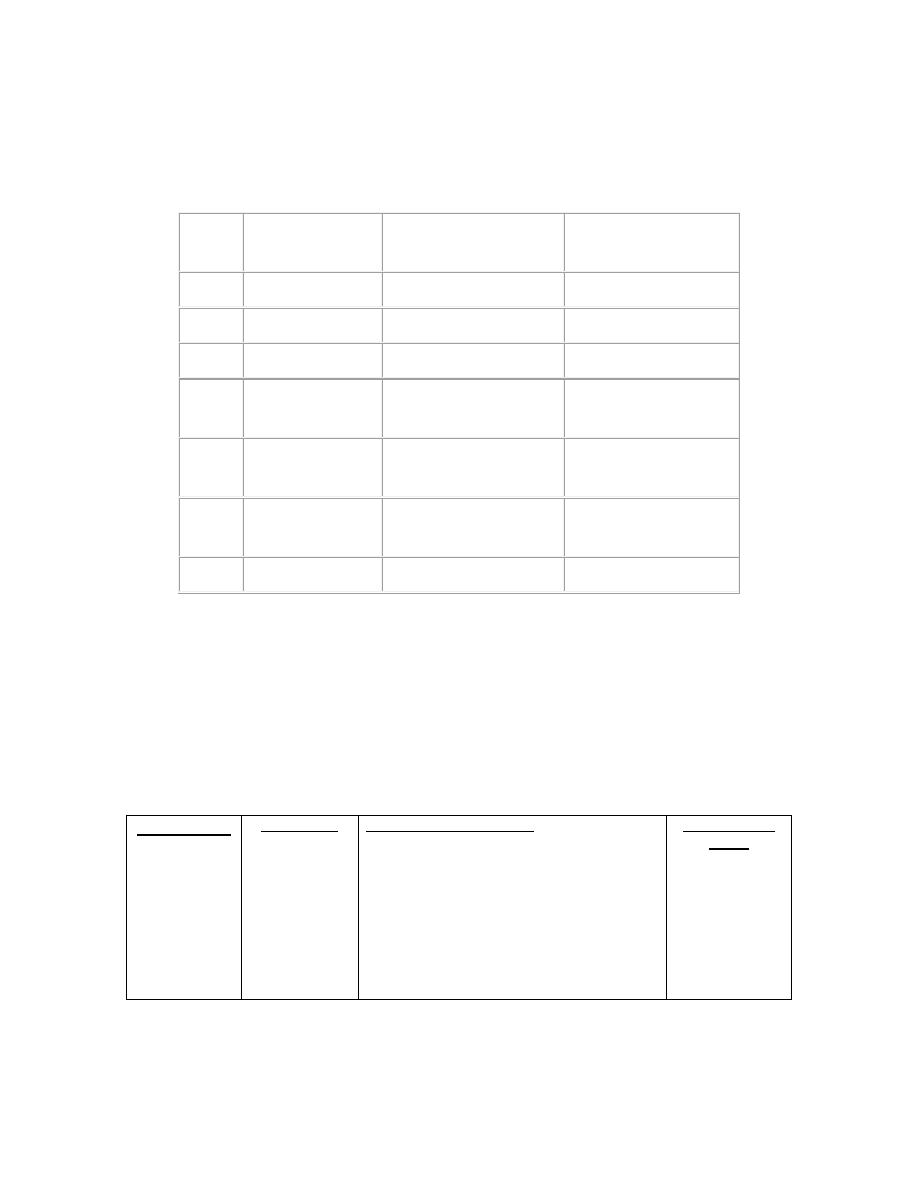
Classification of Head Injuries according to the Severity of Head Injury: by
using the Glasgow Coma Score (GCS):
Points
Best Eye
Opening
Best Verbal
Response
Best Motor
Response
6
-
-
Obeys commands
5
-
Normal oriented
Localizes to pain
4
Spontaneous
Confused
Withdraws to pain
3
To Verbal
command
Inappropriate words
Abnormal flexion
(decorticate)
2
To painful
stimulus
Incomprehensible
sounds
Extension response
(decerebrate)
1
Nil (Do not
open)
Nil (No sounds)
Nil (no motor
response)
T
Intubated patient
The total points are added. The higher the score, the better is the prognosis. According to
this scale, cases of head injury are classified into:
mild head injury : GCS : 14 - 15.
Moderate head injury: GCS : 9 - 13.
severe head injury: GCS : 3-8.
Pathology of head injury
Scalp injury
Avulsion
Abrasion
Laceration
Hematoma
Skull injury
Vault fracture
1. Linear
2. Depressed
Basilar
fracture
Focal intracerebral injury
1)
Epidural hematoma
2)
Subdural hematoma
3)
Subarachnoid hemorrhage
4)
Intracerebral hemorrhage
5)
Brain stem injury
6)
Cranial nerve injury
7)
Vascular injury
8)
Pituitary and hypothalamic
injury
Diffuse axonal
injury

3
Scalp laceration (wounds of the scalp):
They are caused by sharp or blunt instruments or fall on the head.
Common and may give rise to severe bleeding if not controlled.
In infants this can cause severe shock.
Depressed skull fractures may underlie a scalp injury.
Healing is rapid.
If infection occurs in the area of loose areolar tissue, extensive cellulitis is likely to occur.
Management:
If there is possibility of skull fracture, plain X-ray is performed.
Shaving widely around the wound at least 2cm from each edge prior to suturing.
Closure in 2 layers; galea to galea by absorbable suture and skin to skin by non
absorbable suture.
Scalp Haematoma (Subgaleal Haematoma)
May be subgaleal or subpericranial.
The soft fluctuant centers of scalp haematoma may be felt as depressed skull fracture
They are always associated with skull fracture in infants.
Management:
Symptomatic treatment by analgesia, reassurance and some time antibiotics.
It should not be tapped because of the risk of infection and osteomyelitis.
Correction of anaemia in children less than 1 year of age.
Skull Injuries (Skull Fractures):
1)
Fractures of the Vault; includes
1. Simple linear fractures
a. Require no specific neurosurgical treatment.
b. Result of blunt trauma and can radiate to the base.
c. Usually require computed tomography (CT)
d. Patient should be admitted for 48 hours of observation to exclude secondary
intracranial haematoma and brain oedema.
e. Fractures crossing the squqmous temporal bone may lacerate middle
meningeal vessels and cause extradural haematoma.
2. Depressed skull fracture : can be closed or opened (Compound).
Closed depressed fractures: plain X-ray will visualize the depressed segment.
Treatment of closed depressed fractures: usually conservative but surgery is for
Cosmetic especially females or if frontal area affected.
Fracture involving air sinus to prevent infection.
Fracture involving venous sinus with raised intracerebral pressure ICP
Underlying hematoma
FND related to underlying area due to mass effect.
Usually any compound one

4
Compound depressed fracture: will cause profuse bleeding, leakage of CSF and herniation of
the brain. Concussion is slight and there is usually no compression. The main hazard here is the
liability to infection.
Treatment of compound depressed fracture:
1) Medical treatment by antibiotics , analgesia and antiepileptics
2) Surgical treatment
Under GA and ETT
Proper position and incision.
Foreign bodies are meticulously removed.
depressed segment is gently elevated.
necrotic tissue is sucked and haemostasis is performed.
any dural tear is repaired.
removed bone segments are cleaned and replaced if posiible.
The pericranium and the scalp are sutured.
Complications of depressed fractures:
Dural tear leading to prolapse of the brain.
Infection; may lead to osteomyelitis or meningitis.
Epilepsy: either early or late. Elevation of the depressed segment may diminish, but does
not abolish this complication.
Cosmetic deformity.
Severe bleeding from one of the venous sinuses.
3. Diastatic fracture
It is separation of a cranial suture line.
It involves the coronal or lambdoid suture.
It is common in infants under 3 years old and rare in older age group.
4. Pond fracture
This is a smooth concave depression due to blunt trauma to the cranial vault.
Usually seen in children and also known as ‘ping-pong fracture.
Fracture will elevate spontaneously if less than 3cm in diameter.
If the fracture is more than 5cm in diameter, it may need surgical elevation.
2)
Fractures of the base of the skull
a. These are relatively frequent fractures.
b. Occult radiologically.
c. Diagnosed on clinical examination.
d. can result in CSF fistula that may persist, but usually seals off after a few days.
The essential features of base of skull fractures:
A. leakage of cranial contents, e.g. blood, CSF, or brain tissue.
B. Injury of cranial nerves.
C. Signs of brain injury.
5
Types of basilar skull base fractures are:
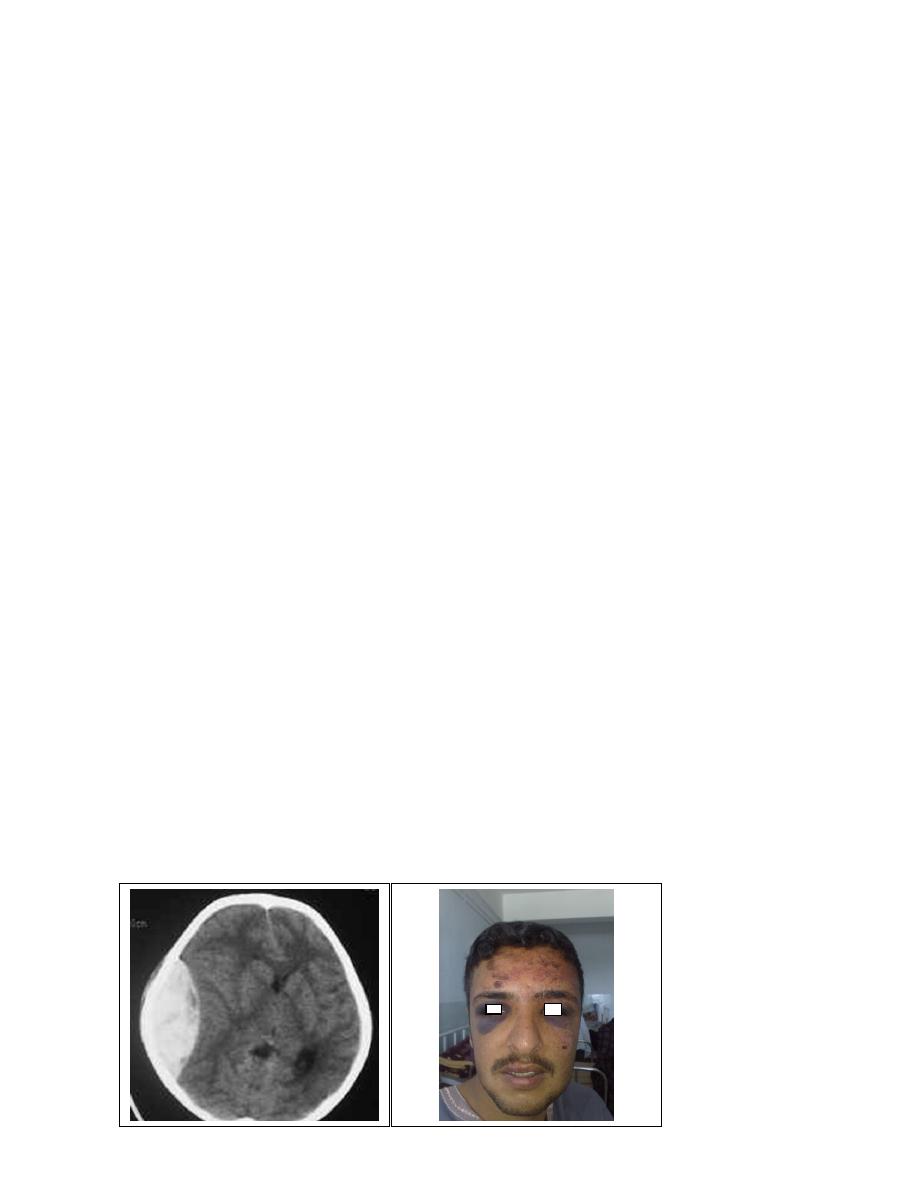
A. Anterior fossa:
May open into the frontal or ethmoidal air sinuses, or run across the cribriform plate.
Clinical presentations:
1)
Periorbital haematoma or ‘raccoon eyes’.
2)
CSF Rhinorrhoea.
3)
Rhinorrhagia.
4)
Subconjuctival haematoma.
5)
Anosmia: due to olfactory nerve injury.
6)
Nasal tip paraesthesia.
B. Middle fossa:
Involve the pertrous temporal bone.
Clinical presentations:
1. CSF Otorrhoea.
2. Haemotympanum.
3. Battle sign; discoloration over the mastoid process.
4. Facial VII and vestibulo-cochlear VIII cranial nerve palsies.
C. Posterior fossa: usually presents with:
1)
Boggy swelling and discoloration at the neck and suboccipital region.
2)
Injury to cranial nerves: 9
th
, 10
th
, and 11
th
cranial nerves at the jugular foramen.
3)
Retraction of the head and neck stiffness due to upper cervical nerves irritation.
Management of skull base fractures :
1)
Prevention of infection: prophylactic antibiotics.
2)
Control of CSF leakage: conservative or surgical intervention.
3)
Treatment of associated brain injury.
Indications for surgery (repair of tear) includes:
1)
Persistence of rhinorrhoea more than 10 days
2)
Presence of a fracture involving the frontal or ethmoidal sinus.
3)
Occurrence of meningitis.
[

6
Epidural hematoma
Incidence 1 % of head injury patient
Male to female 4:1
Affecting young adult , rare before 2 and above 60 years
Temporoparietal depressed fracture can disrupt the middle meningeal artery
through its bony groove within pterion causing bleeding that dissect dura from
the inner table
Source of bleeding from middle meningeal artery, middle meningeal vein , dura
venous sinuses and diploic space in skull fracture.
Clinical Picture:
1) Stage of concussion: brief period of loss of consciousness.
2) Stage of lucid interval: patient recover from concussion, blood will accumulate
gradually in the extradural space.
3) Stage of compression: shown clinically as:
Gradual progressive deterioration in the level of consciousness.
Contralateral hemiparesis due to cortical compression.
Tentorial herniation, with compression of oculomotor nerve, with
dilatation of ipsilateral pupil.
As the coma deepens the blood pressure rises and the pulse and respiration
slow down (i.e. features of increased intracranial pressure).
NOTE: this classic picture is found only in 10-30 % of patients
CT scan will show biconvex or lens shaped hyperdense lesion due to adherence of the dura
to the inside of the cranium at the sites of sutures.
An extradural haematoma is a neurosurgical emergency that will result in death if the
haematoma is not removed promptly.
Surgical treatment by evacuation of haematoma via
Emergency Craniotomy.
Care must be taken in assessing patients with linear fractures crossing the middle
meningeal territory.
Subdural hematoma
They are the most common intracranial mass lesions resulting from head trauma.
They are classified chronologically into:
1)
Acute Subdural Haematoma: less than 3 days
2)
Subacute Subdural Haematoma: 4-21 days
3)
Chronic Subdural Haematoma more than 21 days
Acute Subdural Haematoma :
Usually due to MORE SEVERE high velocity trauma and thus associated with a poorer outcome.

7
Source of bleeding (haematoma): include:
Most result from tears of a cortical artery.
Cortical lacerations or contusions.
Bleeding from tears in the dural venous sinuses.
Clinical Picture: patient will present with a picture similar to that of an extradural haematoma, but
there is persistent loss of consciousness with no lucid interval.
CT scan will show a concave hyperdence collection because blood follows the subdural space over
the convexity of the brain.
Acute Subdural Haematoma are rapidly evolving lesions and early evacuation via craniotomy is
mandatory.
Chronic Subdural Haematoma:
Most common in infants and in adults over 60 years of age secondary to SLIGHT blow to the
head which may pass unnoticed.
Source of bleeding (haematoma): usually from bridging veins as they pass to the venous
sinuses.
The patients present with progressive neurological deficits more than 3 weeks after the trauma,
or progressive headache , memory disturbances.
The initial head injury is often completely forgotten.
CT scan: the acute clotted blood is initially appears white (hyperdence), but as it liquefies, it
slowly becomes black (hypodense).
They should be drained if they continue to enlarge.
They are evacuated by drilling burr holes over the collection and washing it out with warmed
saline.
Subarachnoid Haemorrhage (SAH):
Trauma is the commonest cause of SAH although aneurysms are the most common cause of
spontaneous SAH.
Traumatic SAH is managed conservatively
Intracerebral Haematoma:
This is the least common of traumatic intracranial haematoma.
They are due to areas of traumatic contusion coalescing into a contusional haematoma.
Disrupted cerebral tissue release thromboplastins that potentiate haemorrhage.
CT scan: appear as hyperdence lesions with associated mass effect and midline shift.
Large intracerebral haematomas should be evacuated unless the patient’s neurological state is
improving.
Small inracerebral haematomas may not require removal, but be aware that they can expand.

8
post traumatic complications
CNS Infection:
Causes: includes:
1. Penetrating skull trauma.
2. Depressed skull fractures.
3. Base of skull fractures.
.
Presentations: either:
1. Meningitis.
2. Brain abscess.
3. Subdural empyemas.
These can all exacerbate situation of raised intracranial pressure.
Seizures:
They can increase both brain metabolism and blood flow, therefore increasing
intracranial pressure.
Hydrocephalus
: can develop either:
a. Acutely due to obstruction of CSF outflow due to intraventricular blood.
b. Delayed post-traumatic communicating hydrocephalus due to impaired CSF
reabsorption following traumatic subarachnoid haemorrhage.
Vascular changes (cerebral ischemia)
Cerebral Herniation
: the four major types of herniation are:
a. Subfalcine Herniation.
b. Uncal Herniation.
c. Tentorial Herniation.
d. Tonsillar Herniation.
CSF rhinorrhoea:
Occurs secondary to a fracture involving the paranasal sinuses (frontal, ethmoidal or
sphenoid) associated with dural tear.
A piece of brain tissue is forced into the dural tear and prevents its healing.
This complication is liable to be followed by meningitis.
The patient is treated early with antibiotics.
Indications for surgery(repair of tear) includes:
a. Persistence of rhinorrhoea more than 10 days
b. Presence of a fracture involving the frontal or ethmoidal sinus.
c. Occurrence of meningitis.
