
Anaesthesia
Local & Regional Anaesthesia
Dr. Dena A. Alkazzaz
F.I.C.M.S. (Anaesthesia & intensive care)
Lecturer of anaesthesia /dep. of surgery
/Mosul medical collage
Local anaesthesia
may be safer than general anaesthesia in certain
circumstances & lead to fewer unpleasant side effects, but it is often
ignored in favor of comparative speed & ease of administration of
general anaesthesia.
• Analgesia :
The state when only relief of pain is provided. This may
allow some minor surgical procedures to be performed, for example
infiltration analgesia for suturing.
• Anaesthesia :
The state when analgesia is accompanied by muscle
relaxation, usually to allow major surgery to be undertaken. Regional
anaesthesia may be used alone or in combination with general
anaesthesia.
All drugs will be referred to as local anaesthetics irrespective of the
technique for which they are being used.
Mechanism of action of local anesthetic drugs:
Agents injected or applied topically close to the cell or to the axonal
nerve process on which they are to act, they penetrate the axonal or
cell membrane where exert their blocking action.
Later on they are absorbed into the blood stream, destroyed &
eliminated.
Local anesthetic drugs are composed of aromatic & tertiary amine
groups, linked by a group that is either an ester or amide.
At relatively alkaline media around the nerve the local anesthetic
drugs molecule is lipophilic so enable the local anesthetic to penetrate
the lipoid membrane of the nerve axon. Inside the nerve is relatively
acidic & these leads to release of ionized form of local anesthetic that
it causes block the sodium channels in the nerve cell membrane &
thus prevent the ionic exchange essential for the normal transmission
of the electrical impulse along the axon.
Indication for Local or Regional Anaesthesia:
1.If life of the patient would be endangered by unconsciousness,
for example by respiratory obstruction.
2.Emergencies: when there is no time to reduce the hazards of
general anaesthesia, for example cases of full stomach & operative
obstetric delivery, in some cases of diabetes mellitus, myasthenia
gravis.
3.Avoid hazard of administration of general anaesthetic drugs, for
example
acute
intermittent
porphyria,
repeated
halothane
anesthesia, myotonia, and renal or hepatic failure.
4.Procedure require patient co-operation for example tendon repair
5. Minor superficial & body surface lesion for example dental
extraction, skin lesion, minor laceration & scar revision.
6. To provide postoperative analgesia for example circumcision,
thoracotomy, herniorraphy, skin graft donor site & abdominal
surgery.
7. Provide sympathetic block as in free flap or reimplantation
surgery or limb ischemia.
8. Blood loss can be reduced with controlled hypotension.
9. If the patient or the surgeon or the anesthetist has a preference
for local anesthesia & can convince the other parties that local
anesthesia is appropriate.
10. There is a considerable reduction in the equipment required
and the cost of anaesthesia.
Contra
indication
to
the
use
of
local
anaesthesia:
1. Known sensitivity or allergy to local anesthetic drugs.
2. Anatomical distortion or cicatrix formation.
3. Local infection or ischemia at the site of injection, that local
acidosis will block the effect of local anesthetic agent & also to
avoid spread of infection.
4. Risk of hematoma formation in certain sites (for example
epidural space) this due to medication such as anticoagulant or
due to bleeding tendency such as hemophilia.
5. Extensive surgery that will require toxic doses of local
anesthetic agent.
6. Lack the consent or co-operation on the part of patient.
7. If immediate anesthesia is required (for example
obstructed breach delivery).
8. Lacked of skilled personnel.
9. Lacked of resuscitation facilities.
Local anesthetic drugs: -
Most commonly used local anesthetic drugs are: -
1. Amide linked local anesthetic drugs; lignocaine,
prilocaine, bupivacaine, levo bupivacaine, ropivacaine.
2. Ester linked local anesthetic drugs; cocaine, procaine.
Lignocaine: -
1. Rapid onset of action.
2. Duration of action: 90 min without adrenalin, 120 min with
adrenaline.
3. Use for infiltration, peripheral nerve block, spinal, epidural,
intravenous regional, in concentration: 0. 5%, 1%, 1.5%, 2%
solution.
4. For topical anesthesia used in concentration of 4%, 5%.
5. Maximum safe dose 4.5mg/kg without adrenalin, 7mg/kg with
adrenaline.
Prilocaine: -
1. Onset slower than lignocaine.
2. Duration of action: little longer than lignocaine.
3. Concentration similar to that of lignocaine.
4. Toxicity less than that of lignocaine.
5. Maximum safe dose 8mg/kg.
6. Most important use: -
•
When large volume of drug is required.
•
Used in intravenous regional anaesthesia (IVRA) or Bier’s block
Bupivacaine: -
1.
Slower in onset than lignocaine.
2. Long duration of action because its greater ability to bind to
protein, so adrenaline has no effect on it.
3. Maximum safe dose 3mg/kg with or without adrenalin.
4. More potent than lignocaine so used in concentration 0.125-
0.75%.
Epinephrine (Adrenaline): -
Added to local anaesthetic solution in strength 1:80 000-
1:200 000 to obtain intense vasoconstriction (alpha-adrenergic
effect) so: -
1. Decrease blood flow at the site of injection, leading to
decrease vascular absorption & increase neuronal uptake of
local anaesthetic, so the depth & duration of neuronal
blockade are increased.
2. Decrease the likelihood of high blood level of local
anaesthetic (decrease toxic reaction of local anaesthetic).
3. In infiltration technique, local vasoconstriction leads to
decrease bleeding.
Side effect:
-
1. If injected intravenously may cause cardiac effect (ventricular
effect, ventricular tachycardia, ventricular fibrillation),
hypertension, and myocardial ischemia.
2. Should not be used for ring block of digit, penis, tip of nose that
may cause vasoconstriction of end arteries & lead to ischemia &
gangrene.
3. Local ischemia in infected area lead to anaerobic infection.
Local anaesthetic toxicity:-
High plasma levels of local anaesthetic can be found in:
1. Drug overdose
2. Direct intravascular injection
3. Rapid absorption/ injection into a highly vascular area
4. Cumulative effect of multiple injections or continuous infusion
Symptoms and signs of toxicity:-
Mild toxicity:-
1. Perioral tingling
2. Metallic taste
3. Tinnitus
4. Visual disturbance
5. Slurred speech
Moderate toxicity:-
1. Altered conscious state
2. Convulsion
3. Coma
Potentially fatal toxicity:-
1. Respiratory arrest
2. Cardiac arrhythmias
3. Cardiovascular collapse
Preparation & precaution before the use of
local anaesthesia:
-
1. Formal explanation to the patient & verbal consent.
2. Starvation especially when supplementary sedation is a
possibility.
3. Indwelling intravenous needle & infusion.
4. Monitoring: ECG, blood pressure, SpO2 (oximeter).
5. Resuscitation equipment: O2, suction, positive pressure
ventilation, defibrillator should be available.
6. Resuscitation medicine & supplementary drug & apparatus
for systemic analgesia & sedation should be available.

Types of Local Anaesthesia
Topical anaesthesia: -
Most local anaesthetics produce rapid anaesthesia when
applied to mucous membranes.
Sites:
eye (conjunctiva), nasal cavity, throat, larynx, lower
respiratory tract, ear, urethra, birth canal.
Application
: instillation, spray, ointment, pastes, gels.
1.EMLA cream: mixture of lignocaine & prilocaine for
application to the skin before venipuncture, this is especially
valuable for children but take one hour to act.
2.Lignocaine: 4% maximum 5ml in 70kg man.
3.Cocaine: 5% maximum 5ml in 70kg man.
Local infiltration - field block: -
Superficial injection into or around the lesion to block
sensory nerve ending for body surface surgery, it is simple,
familiar & reliable technique.
Peripheral nerve blocks
Major peripheral nerve blocks-plexus block
Peripheral nerve block is placed proximal to the site of the scheduled
painful procedure or the site of pain. These blocks can be
accomplished either by injecting local anesthetic according to: -
1.Anatomical
land marks (e.g. intercostals, finger& toe,
penile nerve block).
2.Searching for
paraesthesia
with the needle tip (some
technique of brachial plexus block).
3.Using a special
nerve stimulator
connected to the needle
(e.g. femoral nerve block, some techniques of brachial plexus
block).
Intravenous regional anaesthesia
(Bier’s block)
1. Produce anaesthesia to the limbs usually the upper limbs.
2. Large volume of local anaesthetic is used 30-40ml of 0.5% prilocaine
without adrenaline.
3. Used in patients when there is no contraindication to use arterial
tourniquet.
4. Cuff inflated 100 mmHg above the systolic blood pressure.
5. Local anaesthetic injected to intravenous cannula inserted as distal as
possible.
6. Cuff should be inflated at least 20min whatever the length of operation,
otherwise the concentration of local anaesthetic in the blood will reach
an unacceptably high level when it is deflated.
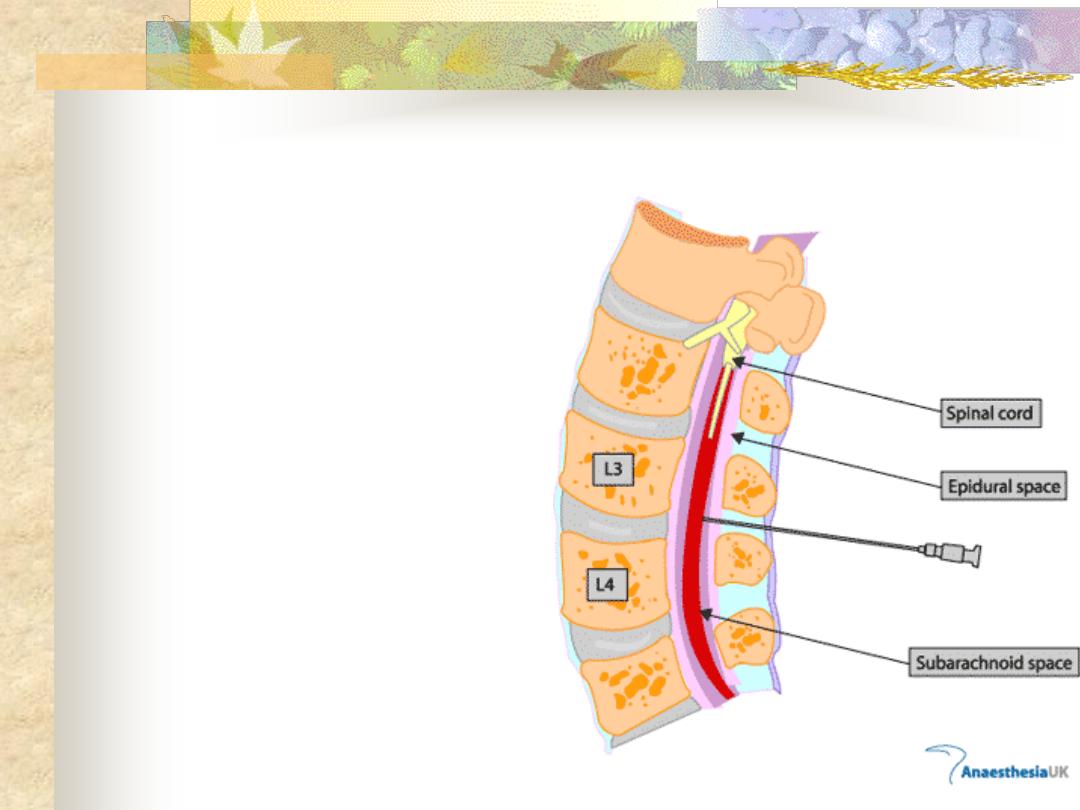
Central block-spinal/epidural block
Anatomy of the vertebral column& spinal cord& its
investing membrane
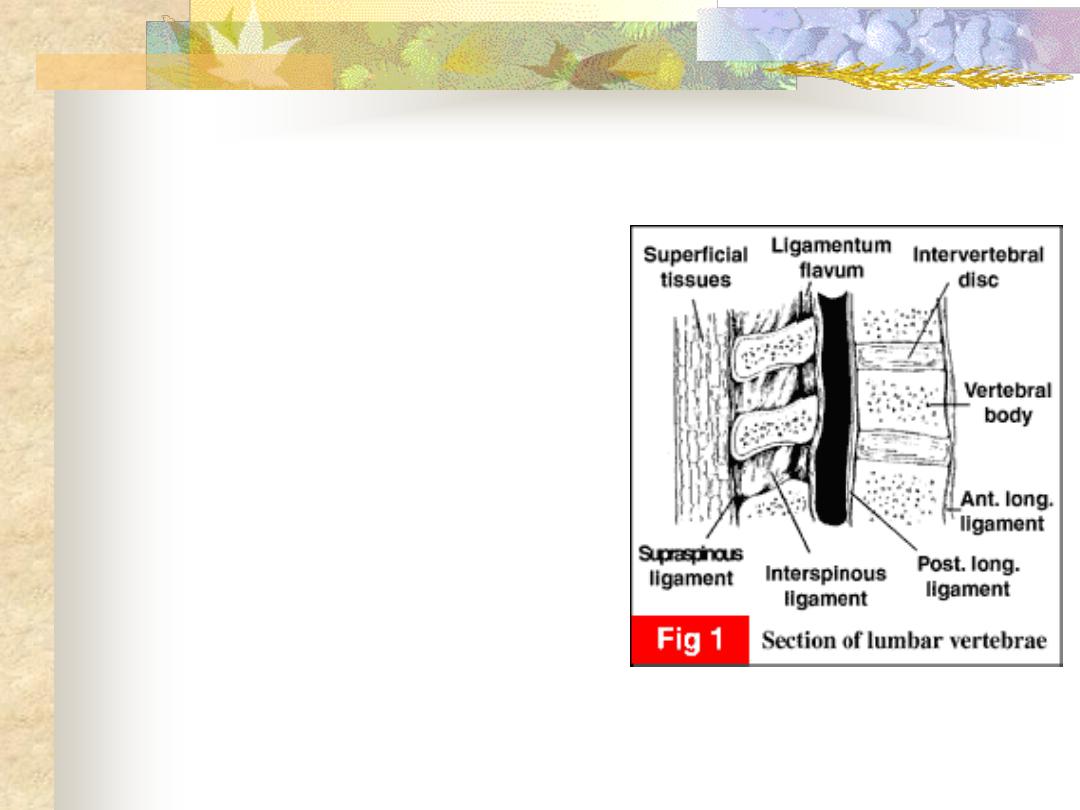
1. Spinal cord
: begin at foramen
magnum as a continuation of
medulla oblongata & terminates at L1-
L2 adults, L3 infants.
2. Closely invested by
piamater
.
3. Surrounded by
CSF
(cerebrospinal
fluid).
4. CSF contained in space enclosed by a
double membrane, an outer fibrous
membrane (
duramater
) & a thin
transparent membrane (the
arachnoid
mater
)
closely applied to its inner
surface.
5. Subdural space
: is potential space &
of limited practical importance.
6.
Subarachnoid space
: is space containing
CSF.
7. Dura &thus the
subarachnoid space
extend as
a tube ending blindly at the level of 2nd
sacral vertebrae in adults & lower in
children.
8. As
spinal cord
end at 1st or 2nd lumber
vertebrae so all lumber & sacral plexus
pass in subarachnoid space known as
cauda equina
, below 2nd lumber
vertebrae the subarachnoid space is
most easily entered by a needle
inserted between the lumber vertebrae.
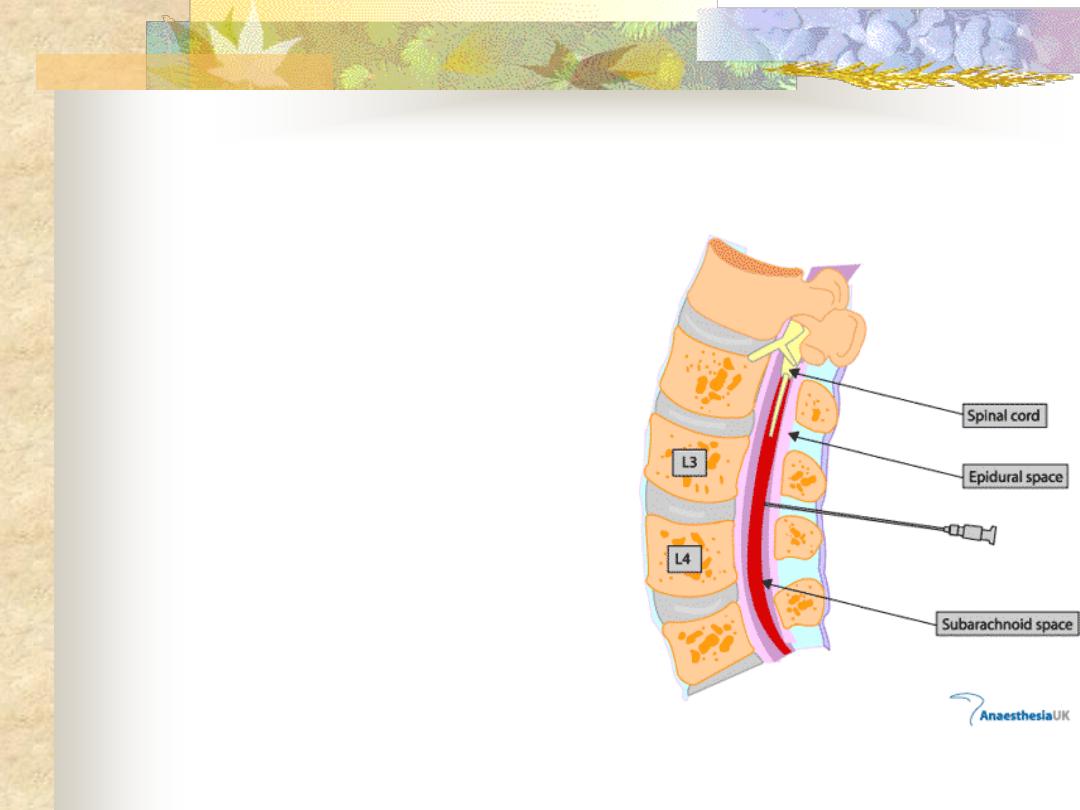
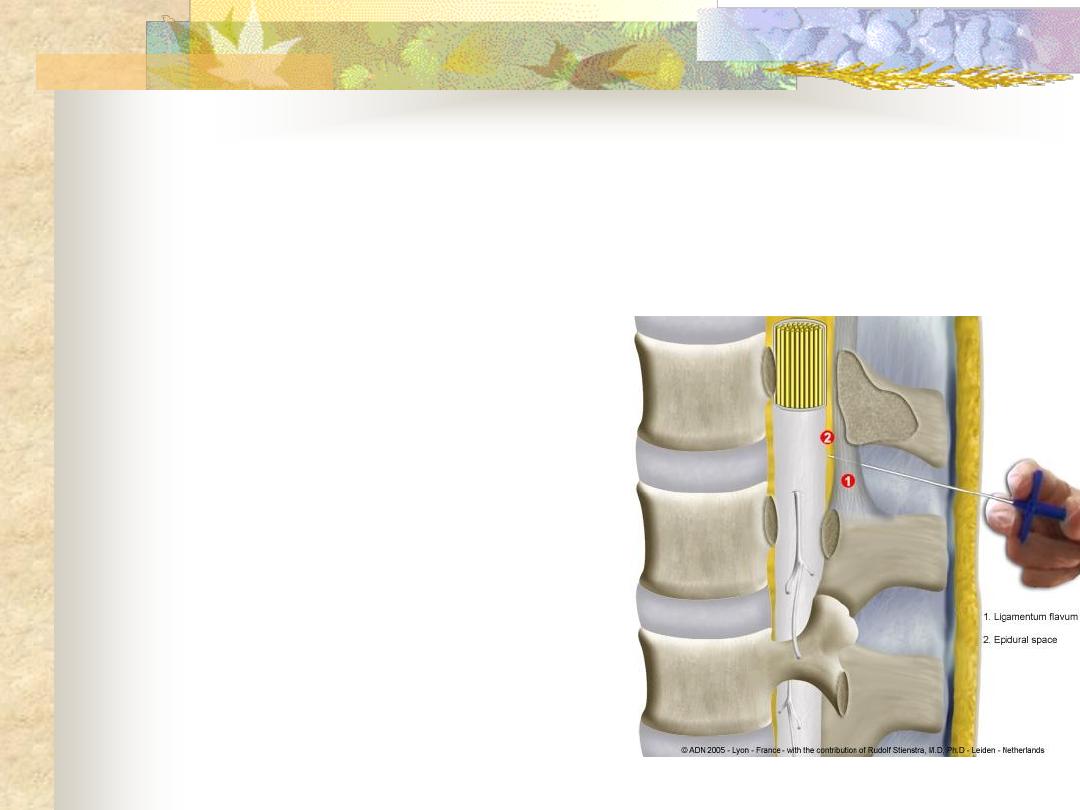
9.
Epidural (extradural) space
: lie
within bony vertebral canal
between the periosteum lining the
lamina of the vertebra, they are
fused at the foramen magnum
superiorly & space limited
inferiorly by sacral hiatus closed
by the sacrocoxygeal membrane.
The epidural space contains the
spinal nerves, alveolar tissue,
arteries & venous plexus.
Epidural space within the sacral
canal is known as
caudal epidural
space
.
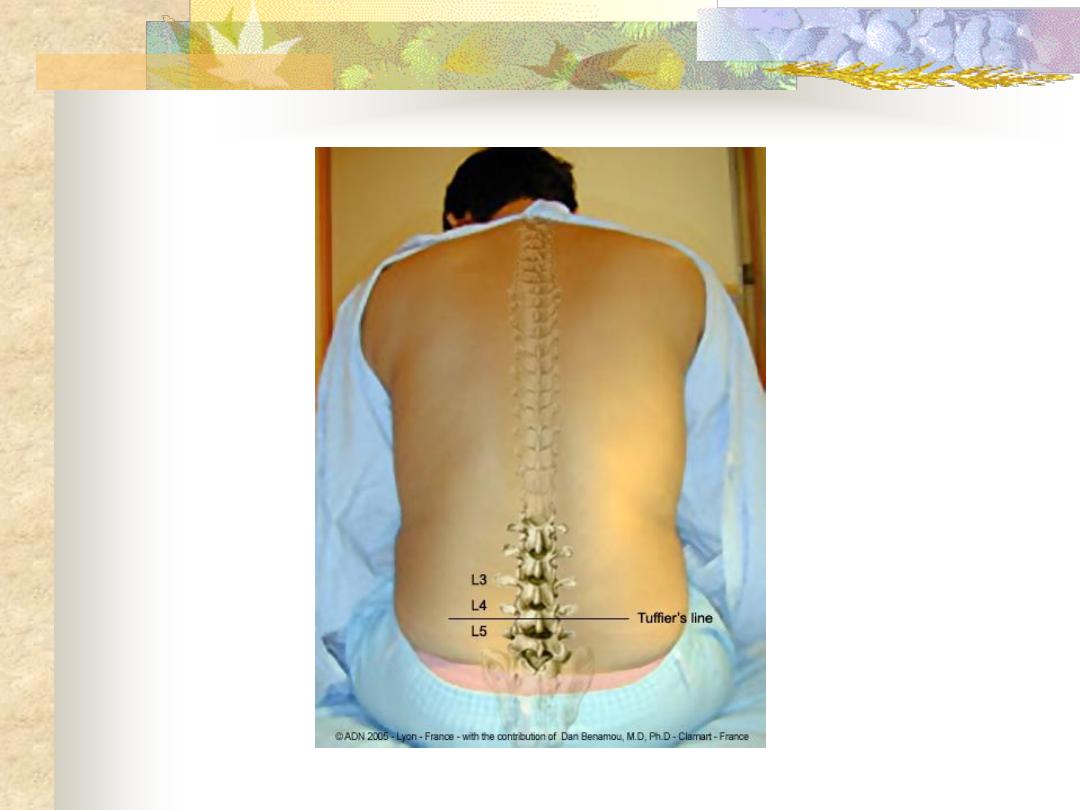

Spinal (subarachnoid) block: -
Earliest, most reliable &
effective technique.
Advantage: -
1. Evidence of correct
position (by withdrawal
of CSF).
2. Only small volume of
local anaesthetic is
needed.
Disadvantage:
1.Risk of introduces infection (meningitis).
2.Spinal headache (per & post operatively due to CSF leak at the site
of dural puncture).
3.Hypotension (due to sympathetic block).
4.High spread can cause prolonged respiratory paralysis necessitate
artificial ventilation.
5.Damage to the cord or to spinal nerve roots whether from direct
trauma or 2ry to spasm of the arteries supplying the cord or 2ry to
hypotension.
6.Urinary retention.
7.Backache.
8.Expanding hematoma & possible compression of spinal cord or
nerves.
Epidural block: -
Advantage: -
1. Easier to gauge & limit the
extend of the spread of
an epidural block,
because the content of
the space is not liquid.
2. Since dura is not
punctured, the danger of
meningitis, post
anaesthesia headache &
damage to the spinal
cord are reduced.
Disadvantage: -
1.Epidural block may be patchy due to anatomical variation like
fibrous septa in the epidural space.
2.Much larger doses of local anesthetic are required for epidural
block than for spinal subarachnoid anaesthesia.
3.Technique is more difficult than subarachnoid.
4.There is always a danger that either the needle or the catheter
may enter a blood vessel.
5.Dura may be penetrated with a wide bore needle so increase
incidence of spinal headache.
6.If dura is penetrated & not detected, the volume of local
anesthetic is several times than that required for spinal
anaesthesia may be injected subdurally causing total spinal
anaesthesia (hypotension, unconsciousness, apnea).
