Disorders of Salivary glands
Dr.MUSTAFA USAMA ABDUL MAGEEDGENERAL SURGEON
Lecturer in al MUSTANSARYIA MEDICAL COLLEGE
LEARNING OBJECTS
• To understand the anatomy , pathology of salivary gland diseases.• To learn how to take a history and examination from a patient present with salivary gland problem.
• How to investigate those patients ?
• To know the medical and surgical treatment of salivary gland diseases.
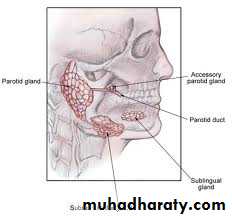
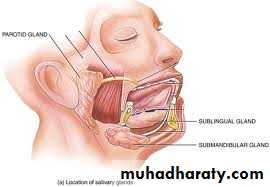
Anatomy of salivary glands
■ Two submandibular glands■ Two parotid glands
■ Two sublingual glands
■ Approximately 450 minor salivary glands
1. Introduction Salivary Gland is any cell or organ discharging a secretion into the oral cavity.
Major and minor Salivary Glands
• Major (Paired) :Parotid, Submandibular, Sublingual
• Minor: Those in the Tongue, Palatine Tonsil, Palate, Lips and Cheeks
2. anatomy of salivary glands .
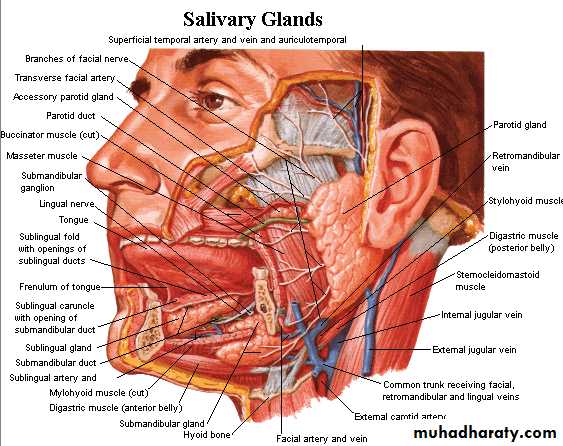
3.Parotid Gland Largest Average Wt - 25 gm Irregular lobulated mass lying mainly below the external acoustic meatus between mandible and sternomastoid. On the surface of the masseter, small detached part lies b/w zygomatic arch and parotid duct-accessory parotid gland or ‘ socia parotidis
What are the Structures within Parotid Gland?
1 branches of the facial nerve;2 the terminal branch of the external carotid artery that divides into the maxillary artery and the superficial temporal artery;
3 the retromandibular vein;
4 intraparotid lymph nodes.
Parotid Duct (ductus parotideus); Stensen’s duct
5 cm in length Appears in the anterior border of the gland Runs anteriorly and downwards on the masseter b/w the upper and lower buccal branches of facial NAt the anterior border of masseter it pierces Buccal pad of fat Buccopharyngeal fascia Buccinator Muscle It opens into the vestibule of mouth opposite to the 2 nd upper molar
Blood supply
Arterial Branches of Ext. Carotid AVenous Into Ext. Jugular Vein
Lymphatic Drainage Upper Deep cervical nodes via Parotid nodes
Nerve Supply
Parasymapthetic N Secretomotor via auriculotemporal N
Symapathetic N Vasomotor Delivered from plexus around the external carotid artery
Sensory N Reach through the Great auricular and auriculotemporal N .
Submandibular Salivary Glands
Irregular in shape ,Large superficial and small deeper partcontinous with each other around the post.Border of mylohyoid.
Superficial Part Situated in the digastric triangle Wedged b/w body of mandible and mylohyoid , 3 surfaces Inferior,Medial,Lateral .
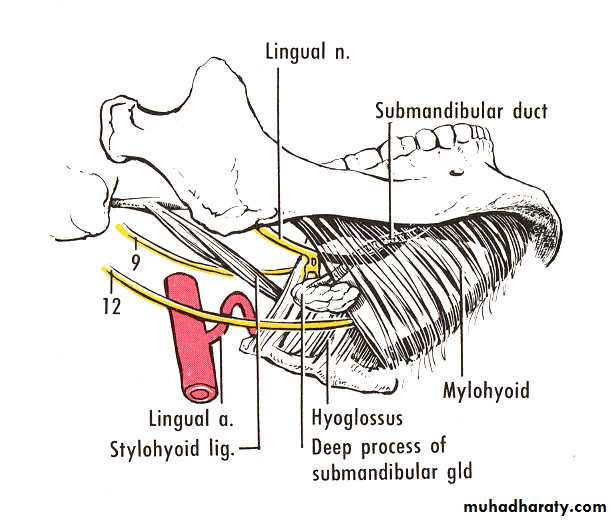
Deep part Small in size Lies deep to mylohyoid and superficial to hyoglossus and styloglossus Posteriorly continuous with superficial part around the posterior border of mylohyoid.
. Submandibluar duct( Whartons duct)
5 cm long Emerges at the anterior end of deep part of the gland Runs forwards on hyoglossus b/w lingual and hypoglossal N .At the ant. Border of hyoglossus it is crossed by lingual nerve Opens in the floor of mouth at the side of frenulum of tongue
Blood Supply
Arteries Branches of facial and lingual arteries.
Veins Drains to the corresponding veins
Lymphatics Deep Cervical Nodes via submandibular nodes.
Nerve Supply
Branches from submandibular ganglion, through which it receives:
Parasymapthetic fibers from chorda tympani.
Sensory fibers from lingual branch of mandibular nerve
Sympathetic fibers from plexus on facial A
Sublingual Salivary Glands
smallest of the three glands weighs nearly 3-4 gm Lies beneath the oral mucosa in contact with the sublingual fossa on lingual aspect of mandible.. Duct :Ducts of Rivinus 8-20 ducts Most of them open directly into the floor of mouth Few of them join the submandibular duct
Blood supply
Arterial from sublingual and submental arteries.
Venous drainage corresponds to the arteries Nerve Supply Similar to that of submandibular glands( via lingual nerve , chorda tympani and sympathetic fibers) .
Functions of Saliva
At least 8 major functions of saliva have been identified (8):1) Moistens oral mucosa. In fact, the mucin layer on the oral mucosa is thought to be the most important nonimmune defense mechanism in the oral cavity.
2) Moistens dry food and cools hot food.
3) Provides a medium for dissolved foods to stimulate the taste buds.
4) Buffers oral cavity contents. Saliva has a high concentration of bicarbonate ions.
5) Digestion. Alpha-amylase, contained in saliva, breaks 1-4 glycoside bonds, while lingual lipase helps break down fats.
6) Controls bacterial flora of the oral cavity.
7) Mineralization of new teeth and repair of precarious enamel lesions. Saliva is high in calcium and phosphate.
8) Protects the teeth by forming a “Protective Pellicle”. This signifies a saliva protein coat on the teeth which contains antibacterial compounds. Thus, problems with the salivary glands generally result in rampant dental caries.
What are the causes of salivary swelling?
A- infection
1- Acute ……………..(viral,bacterial).
2- Recurrence
Obstructive ………….calculus,stricture
Non-obstructive…..children ,menopausal females.
3-chronic infection..Tb ,Actinomycosis .
B-autoimune…………Sicca syndrome, Sjogren syndrome.
C.calculus ………………(sialolithiasis)D. cyst : ………………….simple cysts (parotid)
…………………..Mucus retention cysts.
E –infilteration : ……sarcoidoisis
F-systemic disease :
alcholic liver cirrhosis,Diabetes mellitus,pancreatitis,acromegaly,Malnutrition.
G-Drug :…………………phenthizaine ,phenylbutazone.
H- allergy :……………..iodine
I –Malignancy ………..(benign ,intermediate,malignant)
Note :80% of salivary gland neoplasm occur in the parotid gland.
Note: most stone occur in the submandibular gland.
History taking : Neck lump
AgeSite of lump
Single or multiple
Onset ,duration ,developmental time course congenital versus acquired .
Present or absent of pain.
Associated symptoms –dysphagia ,dysphonia,odynophagia .refered otalgia ,globus sensation ,cough and haemptysis ,weight loss ,sore throat ,intraoral disease (dental cares)
Social hx and habbit /risk factors –smoking ,alcohol.
Previous surgery or radiation
Systemic symptoms –fever ,night sweets pruritis ,anorexia ,malaise
Family history and Tb contactsForeign travel and risk factors for HIN infection.
Parotid examination:
Inspectboth sides Look for any scar in front of the tragus.
palpate
for any tenderness,for any lump ,the characteristic of the lump.
Ask the patient to clinch (test of fixity)
Examintion for lymph nodes .
The oral cavity /orophyrynx
Check the parotid duct (lies in opposite the upper second tooth (for pus ,calculi).
Check the oropharynx for any deep parotid tumour ar medialistion of tonsils.
Bimanual (feeling the duct,and the gland).
Integrity of facial nerve (raise Thiers eyebrow, shut your eye tightly, blow out their checks)
Submandibular ex:
Inspectboth sides for any scars any marginal mandibular nerve weakness .
Palpation
(tenderness),characterstics of lump .
Relation to mylohiod muscle ask the patient push their tongue against roof of mouth .also for sterncleidomastiod .
Inside mouth :
on check for wharton duct orfice under the toungue (pus ,calculi).Look for any carcinoma of the mouth ,for any dental infection.
Bimanual palpation (differentiate gland from lymph node),massage the gland looking for any pus .
Check for tongue sensation (lingual),mobility ( hypoglossal nerve ) malignant infiltration of nerve .
Check for any lymph node enlargement .
Disorders of sublingual gland :
Ranula :mucus extravasation cyst of sub lingual gland giving frog belly appearance .
Some resolve spontaneously .
Plunging Ranula :
some time the mucus penetrate the mylohyiod diaphragm reaching the neck giving dumbbell appearnce .
Diagnosis by MRI and U/S
Treatment transcervical surgical excision of sublingual and submandibular gland.samller cyst can treated by transoral cyst excision with or without marsipulazation.
Plunging Ranula
Large ranula affecting the floor of the mouth
Disorder of submandibular glandEctopic or abberant salivary gland (stafane bone cyst).
Inflammatory disorders of submandibular gland.
Sialadentis Could be acute ,chronic ,acute on chronic .
Acute (viral ,paramyxoviral(mumps),bacterial more common ,secondary to obstruction .
Chronic submandiblar sialadentis .
Obstruction and trauma
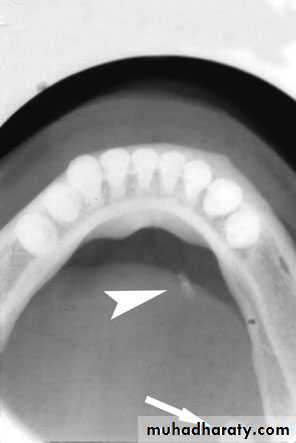
80% of sialoadenitis occur in sub mandibular salivary gland?80% is radio opaque stone.
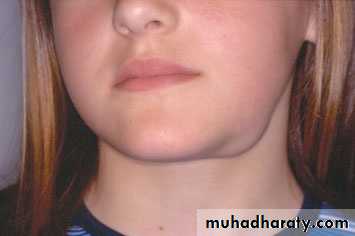
Acute left submandibular sialadenitis.
Clinical features:
If it is complete obstruction ,Painfull tender swellingSwelling related to meal usually disappear 1-2hrs after meal .
The gland examination is tender ,bimanual examination ,the duct draining pus from subligual orifice.
Acute suppurative submandibular sialadenitis. There ispus extruding from the left sublingual papilla.
If partial obstruction ,symptoms is less?
Treatment :submandibular gland excision .Note :some time stone intraoral can be removed transorally with out suturing the duct.why?
What are the indications of removal submandibualar gland?
• Tumor.
• Sialoadentis .
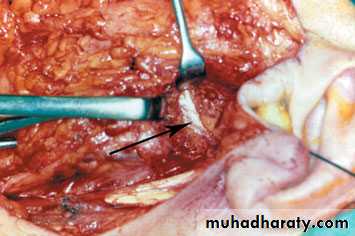
Three cranial nerves are at risk during removal of the submandibular gland:
1 the marginal mandibular branch of the facial nerve;2 the lingual nerve;
3 the hypoglossal nerve.
Complications of submandibular gland excision:
1 Haematoma;
2 wound infection;
3 marginal mandibular nerve injury;
4 lingual nerve injury;
5 hypoglossal nerve injury;
6 transection of the nerve to the mylohyoid muscle producing submental skin anaesthesia.
Salivary gland tumor
Type…. Location Frequency MalignantMajor
Parotid …… Common ….10–20%
Submandibular Uncommon …50%
Sublingual Very rare … 85%
Minor Upper aerodigestive tract Rare 90%
What are the Clinical features of malignant salivary tumours?
1 Facial nerve weakness;2 rapid enlargement of the swelling;
3 induration and/or ulceration of the overlying skin;
4 cervical node enlargement.
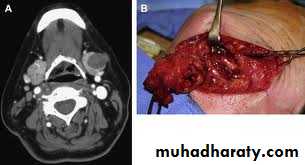
What are the investigation of salivary gland tumor ?
CT
MRI .
NOTE: the management of malignant submadibular gland tumors is to remove the gland with cuff of normal tissue.
Submandiblar gland tumor
Only 50% benignEven the malignant can be slowly growing
Benign tumor can be painful.
Open biopsy seeds tumor
Fine-aspiration does not but, rarely alter management.
Parotid gland disorders
Viral parotitis:the most common cause of acute painfull parotid swelling .
Affects children .
The disease start as constitutional symptom( fever, nausea, headache ) .( prodromal period)(1-2days).
After that the patient start to develop pain and swelling and this increase by drinking and eating .This continous for f-10 days .
Atypical symptoms unilateral swelling or submandibular swelling .
Diagnosis by mumps Vand S antigens.
Treatment is symptomatic (oral paracetmol and oral fuid intake).
Complication: orchitis ,oophritis, pancreatitis ,sensory neural deafness ,meningoencephalitis.(adult).
Other viral infection coxacki A and B,parainfluenza 1and 3,Echo and lymphocytic choriomengitis ,
Bacterial parotitis :
Dehydtarated elderly(reduse salivary flow.now adult without precipated factors.Infecting organism is Staphylococcus aureus, or steptococcal viridans .
Daignosis is clinical some time need u/s study.
Treatment : intravenous broad spectrum antibiotics and penicillinase-resistant agent (flucloxacillin).
Some time if u/s study shows abscess ,this need drainage with wide bore needle ,or formal drainage under general anesthetasia .
Recurrent parotitis of childhood :
Known atiology.
Age 3-4years .
Rapid one or both parotid swelling .recurrent swelling.
Diagnosis is made by history and sialograghy .
Snow storm appearance .
Treatment is conservatives ,then parotidectomy.
HIV –ASSOCIATED SIALOADENTIS:
like Sjogren syndrom but negative autoantibody screen .Other presentation syndrom like cyst ,facial disfigurement .
Diagnosis by CT,MRI (swiss-cheese of large cysts).
Surgery some time indicated .
Obstructive parotitis
Papillray obstruction :Trauma to parotid gland over extended upper denature flange ,or fracture upper molar tooth.
Stenosis and obstruction of saliva flow.
Treatment papillotomy.
Parotid stone :
Much rare than submandibularUsually radiolusent .
Sialography
Stone removed surgically either by exposing duct or parotidectomy approach.
Tumors of the parotid gland
Parotid gland is the most common site of benign salivary gland tumours.Most tumours arise in the superficial lobe and present as slow growing, painless swellings below the ear, in front of the ear or in the upper aspect of the neck. Less commonly,
tumours may arise from the accessory lobe
and present as persistent swellings within the cheek.
tumours may arise from the deep lobe of the gland and present as parapharyngeal masses
80–90% of tumours of the parotid gland are benign.
The most common being pleomorphic adenoma.Benign tumour of the left parotid gland producing characteristic deflection of the ear lobe
Pleomorphic adenoma arisingfrom the upper pole of the left parotid gland producing a pre-auricular swelling.
Deep lobe tumour of the right parotid presenting with a swellingof the right soft palate.
Magnetic resonance imaging (MRI) scan revealing aspace-occupying lesion (arrow) in the right parotid gland; histologyrevealed pleomorphic adenoma.Malignant salivary gland tumours are divided into two distinct sub-groups:
1 Low-grade malignant tumours, e.g. acinic cell carcinoma, are indistinguishable on clinical examination from benign neoplasms.2 High-grade malignant tumours usually present as rapidly growing, often painless swellings in and around the parotid gland.
Computerised tomographic (CT)scan of the left parotid gland revealing a cystic lesion (arrow). Histologyrevealed acinic cell carcinoma.
Type Sub-group Common examples
I AdenomaPleomorphic Pleomorphic adenoma
Monomorphic Adenolymphoma (Warthin’s tumour)
II Carcinoma
Low grade Acinic cell carcinoma
Adenoid cystic carcinoma
Low-grade muco-epidermoid carcinoma
High grade Adenocarcinoma
Squamous cell carcinoma
High-grade muco-epidermoid carcinoma
III Non-epithelial tumours
Haemangioma, lymphangioma
IV Lymphomas
Primary lymphomas Non-Hodgkin’s lymphomas
Secondary lymphomas Lymphomas in Sjögren’s syndrome
V Secondary tumours Local Tumours of the head and neck especially
Distant Skin and bronchus
VI Unclassified tumours
VII Tumour-like lesions Solid lesions Benign lymphoepithelial lesion
Adenomatoid hyperplasia
Cystic lesions Salivary gland cysts
ParotidectomySuperficial parotidectomy
Incision and development of a skin flapMobilization of the gland.
Location of the facial nerve trunk
Dissection of the gland off the facial nerve
Closure
1 The inferior portion of the cartilaginous canal. This is termed Conley’s pointer and indicates the position of the facial nerve, which lies 1 cm deep and inferior to its tip.
2 The upper border of the posterior belly of the digastric muscle. Identification of this muscle not only mobilises the parotid gland, but also exposes an area immediately superior, in which the facial nerve is usually located.
Radical parotidectomy
involves removal of all parotid gland tissue and elective sectioning of the facial nerve, usually through the main trunk .Complications of parotid gland surgery
1 haematoma formation;2 infection;
3 temporary facial nerve weakness;
4 transection of the facial nerve and permanent facial weakness;
5 sialocele;
6 facial numbness;
7 permanent numbness of the ear lobe associated with great auricular nerve transection;
8 Frey’s syndrome.
Frey’s syndrome
(gustatory sweating)
It results from damage to the autonomic innervation of the salivary gland with inappropriate regeneration.
starch iodine test dx
Rx:
Peventive: sternomastoid muscle flap;
• temporalis fascial flap;
insertion of artificial membranes between the skin and the parotid bed.
Management of established Frey’s syndrome: anti-perspirants, usually containing aluminium chloride;denervation by tympanic neurectomy;
the injection of botulinum toxin into the affected skin.
Granulomatous sialadenitis
This is a group of rare conditions that affect the salivary glandsproducing a variety of signs and symptoms, particularly painless swellings of the parotid and/or submandibular glands. Systemic upset is variable.
Mycobacterial infection.
Sarcoidosis. scratch disease, toxoplasmosis, syphilis, deepmycoses and Wegener’s granulomatosis, allergic sialadenitis and
sialadenitis associated with radiotherapy of the head and neck.
Tumour-like lesions
Sialadenosis (sialosis).
non-inflammatory swelling particularly affecting the parotid gland.
Most patients present between 40 and 70 years of age.
Causes: diabetes mellitus, alcoholism, other endocrine diseases, pregnancy, drugs, bulimia and other eating disorders, and idiopathic
diseases.
The treatment of sialosis is unsatisfactory, but treatment is aimed at the correction of the underlying disorder.
Sjِgren’s syndrome
Primary Sjögren’s syndromeMore severe xerostomia
Widespread exocrine gland
dysfunction
No connective tissue disorder
Secondary Sjögren’s syndrome
M:F: 1:10
Middle age
Underlying connective tissue
disorder
Benign lymphoepithelial lesion
20% develop lymphoma
Diffuse parotid swelling
20% bilateral
The diagnosis :is based on the history as no single laboratory investigation is pathognomonic of either primary or secondary Sjögren’s syndrome.
Complications of Sjögren’s syndrome:
B-cell lymphoma)xerostomia or keratoconjunctivitis sicca
the risk of accelerating dental caries.
include oral candidosis
Treatment of sjogren syndrom:
Drink large amount of water.
Xerostomia
1 chronic anxiety states and depression;2 dehydration;
3 anti-cholinergic drugs, especially antidepressants;
4 salivary gland disorders – Sjögren’s syndrome. Ascending parotitis is an occasional complication of xerostomia and is managed with antibiotics and increased fluid intake;
5 radiotherapy to the head and neck.
Sialorrhoea
It is seen in children with mental and physicalhandicap, notably cerebral palsy.
TREATMENT: bilateral submandibular gland excision.
OROPHARYNGEAL CANCER
Risk factors associated with cancer of the head and
neck
■ Tobacco
■ Alcohol
■ Areca nut/pan masala
■ Human papillomavirus
■ Epstein–Barr virus
■ Plummer–Vinson syndrome
■ Poor nutrition
Premalignant lesion:
Conditions associated with malignant transformationHigh-risk lesions
■ Erythroplakia
■ Speckled erythroplakia
■ Chronic hyperplastic candidiasis
Medium-risk lesions
■ Oral submucous fibrosis
■ Syphilitic glossitis
■ Sideropenic dysphagia (Paterson–Kelly syndrome)
Low-risk/equivocal-risk lesions
■ Oral lichen planus
■ Discoid lupus erythematosus
■ Discoid keratosis congenita
Potential for malignant change
The potential risk for malignant transformation:
• increases with increasing age of the patient;
• increases with increasing age of the lesion;
• is higher in smokers;
• increases with alcohol consumption;
• depends on the anatomical site of the pre-malignant lesion;
• is particularly high for leucoplakia on the floor of the mouth and
ventral surface of the tongue, particularly in younger women,
even in the absence of associated risk factors.
Leucoplakia with severe dysplasia of the lateral borderof the tongue.
Speckled leucoplakia on the lateral border of thetongue. Histology confirms carcinoma in situ.Chronic hyperplastic candidiasis of the left buccalmucosa.
Erythroplakia of the left soft palate and lateral pharyngealwall.Oral cavity cancer
Clinical features of oral cancer■ Persistent oral swelling for > 4 weeks
■ Mouth ulceration for > 4 weeks
■ Sore tongue
■ Difficulty swallowing
■ Jaw or facial swelling
■ Painless neck lump
■ Unexplained tooth mobility
■ Trismus
The TNM staging system
Primary tumour (T)
TX Primary tumour cannot be assessed
T0 No evidence of primary tumour
Tis Carcinoma in situ
T1 Tumour < 2 cm in greatest dimension
T2 Tumour > 2 but < 4 cm
T3 Tumour > 4 cm but < 6 cm
T4 Tumour invades adjacent structures, e.g. mandible, skin
Regional lymph nodes (N)
NX Regional lymph nodes cannot be assessedN0 No regional lymph node metastasis
N1 Metastasis in a single ipsilateral lymph node < 3 cm in
greatest dimension
N2a Metastasis in a single ipsilateral lymph node > 3 cm but not
more than 6 cm
N2b Metastasis in multiple ipsilateral lymph nodes, none > 6 cm
in greatest dimension
N2c Metastasis in bilateral or contralateral lymph nodes, none
greater than 6 cm in greatest dimension
N3 Metastasis in any lymph node > 6 cm
Distant metastasis
M0 No evidence of distant metastasis
M1 Evidence of distant metastasis
Stage
0 Tis N0 M0
I T1 N0 M0
II T2 N0 M0
III T3 N0 M0
T1, T2, T3 N1 M0
IV T4 N0 M0
Any T N2 M0
Any T N3 M0
Any T Any N M1
Treatment :Surgery and radiotherpy
Cervical lymph node excisionUlcerative squamous cell carcinoma of the anteriorfloor of the mouth
squamous cell carcinoma of the rightlateral border of the tongue.Lip cancer
Lip cancer presents early as it is readily visible to the patient.
In total, 95% of carcinomas of the lip arise on the lower lip.
Tumours tend to
spread laterally over the mucosal surface. Lymph node metastases, usually to the submental or submandibular nodes, occur late.
Squamous cell carcinoma of the lower lip.
LIP CANCERSurgery and external beam radiotherapy are highly effective methods of treatment for lip cancer.
Small size<2cm v or w shaped excision.
Intermediate local flap excision.
Extensive tumor Total lip reconstruction(T4)
Tongue cancer
Up to 30% of patients with a T1 (< 2 cm diameter) tumour have occult metastasis at presentation and should undergo simultaneous treatment of the neck by either selective neck dissection or radiotherapy.Resection resulting in partial or hemiglossectomy can be performed with either a cutting diathermy or laser if available.