ENDOCRINE DISEASE •
10
357
• Seminomas arise from seminiferous tubules. Metastases occur via the
lymphatics, often involving the lungs. • Teratomas arise from primitive
germinal cells. They may contain cartilage, bone, muscle or fat. Well-
differentiated tumours are the least aggressive; at the other extreme,
trophoblastic teratoma is highly malignant. • Leydig cell tumours are
usually small and benign, but secrete oestrogens leading to presentation
with gynaecomastia.
Clinical features and investigations
• The common presentation is incidental discovery of a painless testicular
lump, although some complain of testicular ache. • Suspicious scrotal lumps
are imaged by USS. • Serum levels of the ‘tumour markers’
α-fetoprotein
(AFP) and
β-hCG are increased in extensive disease. • Oestradiol may be
elevated, suppressing the levels of LH, FSH and testosterone. • Accurate
staging is based on CT or MRI.
Management and prognosis
• The primary treatment is surgical orchidectomy. • Radiotherapy is the
treatment of choice for early-stage seminoma. • Teratoma confi ned to the
testes may be managed conservatively, but more advanced cancers are
treated with chemotherapy. • Follow-up is by imaging and assessment of
AFP and
β-hCG. • 5-yr survival rates are 90–95% for seminomas and
60–95% for teratomas.
THE PARATHYROID GLANDS
The four parathyroid glands lie behind the lobes of the thyroid. Parathyroid
hormone (PTH) interacts with vitamin D to control calcium metabolism.
Calcium exists in serum as 50% ionised, and 50% complexed with organic
ions and proteins. The parathyroid chief cells respond directly to changes
in calcium concentrations, secreting PTH in response to a fall in ionised
calcium. PTH promotes reabsorption of calcium from renal tubules and
bone, stimulating alkaline phosphatase and lowering plasma phosphate.
PTH also promotes renal conversion of 25-hydroxycholecalciferol to the
more potent 1,25-dihydroxycholecalciferol, which results in increased
calcium absorption from food.
To investigate disorders of calcium metabolism, measurement of calcium,
phosphate, alkaline phosphatase and PTH should be undertaken. Most labo-
ratories measure total calcium in serum. This needs to be corrected if serum
albumin is low, by adjusting the value for calcium upwards by 0.1 mmol/l
(0.4 mg/dl) for each 5 g/l reduction in albumin below 40 g/l.
PRESENTING PROBLEMS
HYPERCALCAEMIA
Causes of hypercalcaemia are listed in Box 10.11. Primary hyperparathy-
roidism and malignant hypercalcaemia are the most common causes. Famil-
358
ENDOCRINE DISEASE •
10
ial hypocalciuric hypercalcaemia (FHH) is a rare autosomal dominant
disorder in which a mutation in the calcium-sensing receptor results in
increased PTH secretion with consequent calcium retention in the renal
tubules. FHH is almost always asymptomatic and without com plication.
Unnecessary parathyroidectomy may be undertaken if FHH is misdiag-
nosed as primary hyperparathyroidism.
Clinical assessment
• Symptoms and signs of hypercalcaemia include polyuria, polydipsia, renal
colic, lethargy, anorexia, nausea, dyspepsia, peptic ulceration, constipation,
depression and impaired cognition (‘bones, stones and abdominal groans’).
• Patients with malignant hypercal caemia can have a rapid onset of symp-
toms. • Hypertension is common in hyperparathyroidism. • Parathyroid
tumours are almost never palpable. • A family history of hypercalcaemia
raises the possibility of FHH or MEN.
Investigations
•
↓Plasma phosphate and ↑alkaline phosphatase support a diagnosis of
primary hyperparathyroidism or malignancy. •
↑Plasma phosphate and
↑alkaline phosphatase accompanied by renal impairment suggest tertiary
hyperparathyroidism (p. 360). • If PTH is normal or elevated and urinary
calcium is elevated, then hyperparathyroidism is confi rmed. • Low urine
calcium excretion indicates likely FHH, confi rmed by genetic analysis of
the calcium-sensing receptor. • If PTH is low and no other cause is apparent,
then malignancy with or without bony metastases is likely. The patient
should be screened with a CXR, isotope bone scan, myeloma screen and
serum ACE (elevated in sarcoidosis). PTH-related peptide, which causes
hypercalcaemia associated with malignancy, can be measured by a specifi c
assay.
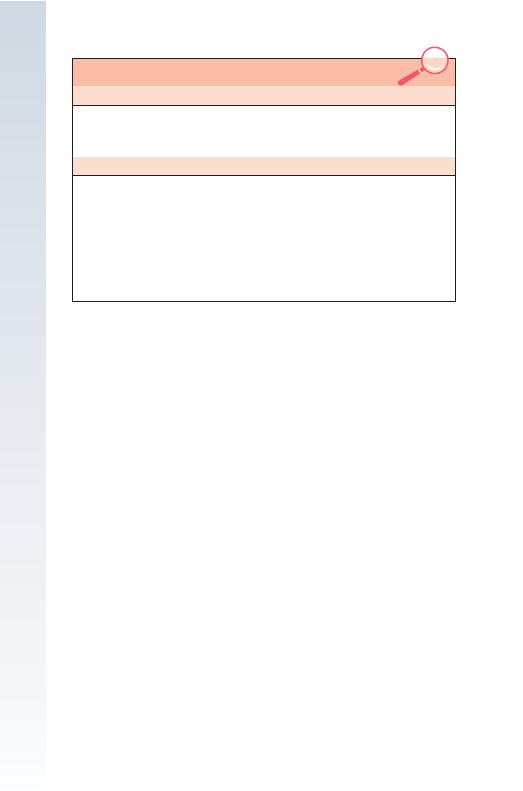
10.11 CAUSES OF HYPERCALCAEMIA
With normal/elevated (inappropriate) PTH levels
• Primary or tertiary hyperparathyroidism
•
Lithium-induced hyperparathyroidism
• Familial hypocalciuric hypercalcaemia
With low (suppressed) PTH levels
• Malignancy (e.g. lung, breast, renal, colonic and thyroid carcinoma,
lymphoma, multiple myeloma)
•
Elevated 1,25(OH)
2
vitamin D (vitamin D intoxication, sarcoidosis, HIV)
•
Thyrotoxicosis
• Paget’s disease with immobilisation
•
Milk-alkali syndrome
•
Thiazide diuretics
•
Glucocorticoid defi ciency
ENDOCRINE DISEASE •
10
359
Management
• Treatment of severe hypercalcaemia involves rehydration with normal
saline. • Bisphosphonates (e.g. pamidronate 90 mg i.v. over 4 hrs) reduce
serum calcium for a few weeks, working maximally at 2–3 days. If the
underlying cause cannot be removed, oral bisphosphonates should be
continued. • In very ill patients, forced diuresis with furosemide, glu-
cocorticoids, calcitonin or haemodialysis may need to be employed. •
For management of hyperparathyroidism, see page 361. • FHH does not
require therapy.
HYPOCALCAEMIA
The differential diagnosis of hypocalcaemia is shown in Box 10.12. It is
the ionised rather than total concentration which is biologically important.
The most common cause of hypocalcaemia is a low serum albumin with
normal ionised calcium concentration. Ionised calcium may be low with a
normal total serum calcium in alkalosis, e.g. hyperventilation (respiratory)
or Conn’s syndrome (metabolic).
Causes of hypoparathyroidism include:
• Parathyroid gland damage during thyroid surgery (transient hypo-
calcaemia in 10%, permanent in 1%). • Infi ltration of the glands, e.g.
haemochromatosis, Wilson’s disease. • Congenital/inherited, e.g. auto-
immune polyendocrine syndrome (APS) type I, autosomal dominant
hypoparathyroidism.
In pseudohypoparathyroidism there is tissue resistance to PTH. Clinical
features include:
• Short stature. • Short 4th metacarpals and metatarsals. • Rounded face.
• Obesity. • Calcifi cation of the basal ganglia.
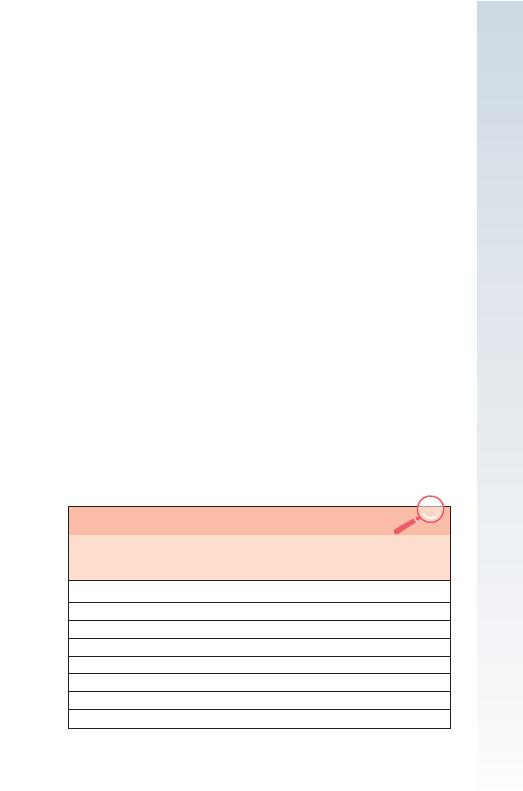
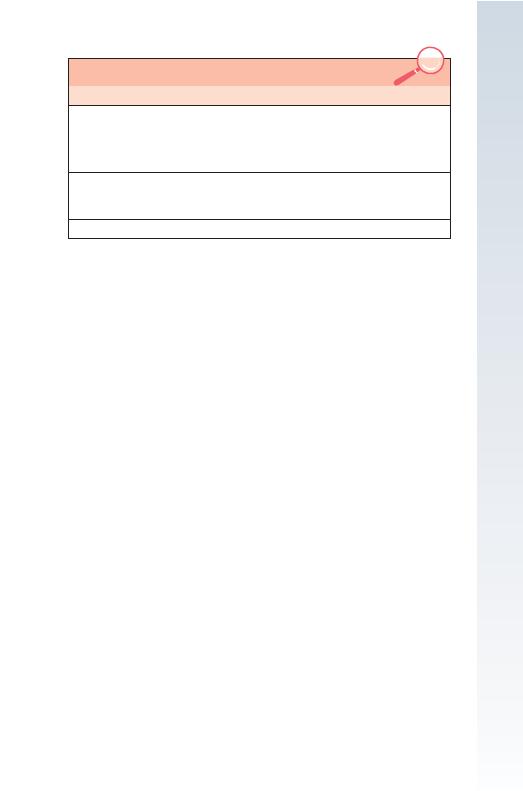
10.12 DIFFERENTIAL DIAGNOSIS OF HYPOCALCAEMIA
Total
serum
calcium
Ionised
serum
calcium
Serum
phosphate
Serum PTH
concentration
Hypoalbuminaemia
↓
→
→
→
Alkalosis
→
↓
→
→ or ↑
Vitamin D defi ciency
↓
↓
↓
↑
Chronic renal failure
↓
↓
↑
↑
Hypoparathyroidism
↓
↓
↑
↓
Pseudohypoparathyroidism
↓
↓
↑
↑
Acute pancreatitis
↓
↓
→ or ↓
↑
Hypomagnesaemia
↓
↓
Variable
↓ or →
360
ENDOCRINE DISEASE •
10
The term ‘pseudo-pseudohypoparathyroidism’ describes those with these
clinical features in whom serum calcium and PTH concentrations are
normal. Due to genomic imprinting, pseudohypoparathyroidism results
from inheritance of the gene defect from the mother, but inheritance from
the father results in pseudo-pseudohypoparathyroidism.
Clinical assessment
• Low ionised calcium increases excitability of peripheral nerves. • Tetany
can occur if total serum calcium is
<2.0 mmol/l (8 mg/dl). • In children
a characteristic triad of carpopedal spasm, stridor and convulsions
occurs. Adults complain of tingling in the hands and feet and around the
mouth. • When overt signs are lacking, latent tetany may be revealed by
Trousseau’s sign (infl ation of a sphygmomanometer cuff to more than the
systolic BP causes carpal spasm) or Chvostek’s sign (tapping over the facial
nerve produces twitching of the facial muscles). • Hypocalcaemia causes
papilloedema and QT interval prolongation, predisposing to ventricular
arrhythmias. • Prolonged hypocalcaemia with hyperphosphataemia may
cause calcifi cation of the basal ganglia, epilepsy, psychosis and cataracts.
• Hypocalcaemia with hypophosphataemia (vitamin D defi ciency) causes
rickets in children and osteomalacia in adults.
Management
• To control tetany, alkalosis can be reversed by rebreathing expired air
in a bag (
↑PaCO
2
). • Injection of 20 ml of 10% calcium gluconate
slowly into a vein will raise the serum calcium concentration immediately.
• I.V. magnesium is required to correct hypocalcaemia associated
with hypomagnesaemia. • Vitamin D defi ciency, persistent hypoparathy-
roidism and pseudohypoparathyroidism are treated with oral calcium salts
and vitamin D analogues (alfacalcidol, calcitriol). • Monitoring of therapy
is required because of the risks of iatrogenic hypercalcaemia, hypercalciuria
and nephrocalcinosis.
PRIMARY HYPERPARATHYROIDISM
The three categories of hyperparathyroidism are shown in Box 10.13.
• In primary hyperparathyroidism there is autonomous secretion of PTH,
usually by a single parathyroid adenoma. • In secondary hyperparathy-
roidism there is increased PTH secretion to compensate for prolonged
hypocalcaemia, thus increasing serum calcium levels by bone resorption.
It is associated with hyperplasia of all parathyroid tissue. • In a small pro-
portion of secondary hyperparathyroidism cases, continuous stimulation of
the parathyroids results in adenoma formation and autonomous PTH secre-
tion. This is known as tertiary hyperparathyroidism.
Primary hyperparathyroidism has a prevalence of 1 in 800 and is 2–3
times more common in women; 90% of patients are over 50. It also occurs
in MEN syndromes. Clinical presentation is described under hypercalcae-
mia (p. 358).
ENDOCRINE DISEASE •
10
361
Skeletal and radiological changes include:
• Osteoporosis-reduced bone mineral density on DEXA scanning. • Osteitis
fi brosa results from increased bone resorption by osteoclasts with fi brous
replacement. It presents as bone pain, fracture and deformity.
• Chondrocalcinosis is due to deposition of calcium pyrophosphate crystals
within articular cartilage, typically the knee, leading to osteoarthritis or
acute pseudogout. • X-ray changes include subperiosteal erosions, terminal
resorption in the phalanges, ‘pepper-pot’ skull and renal calcifi cation.
Imaging to locate the adenoma or differentiate hyperplasia has tradition-
ally not been necessary, but its increasing use allows more targeted resec-
tion through a smaller incision. Localisation of parathyroid tumours may
be carried out using
99m
Tc-sestamibi scanning, USS, CT or selective neck
vein catheterisation with PTH measurements. Without imaging, >90% of
adenomas can be located at surgery.
Management
Treatment of severe hypercalcaemia is described above (p. 359). Hypercal-
caemia in primary hyperparathyroidism responds less well to glucocorti-
coids and bisphosphonates. Most patients do not require urgent surgical
treatment. However, the only long-term therapy is surgery, with excision
of an adenoma or debulking of hyperplastic glands. Part of the hyperplastic
gland can be transplanted to the forearm to allow further debulking at a
later date. Post-operative hypocalcaemia can occur while residual sup-
pressed parathyroid tissue recovers.
Surgery is indicated for patients under 50 and for those with symptoms
or complications, e.g. peptic ulceration, renal stones, renal impairment
or osteopenia. The remainder can be reviewed annually, with assess-
ment of symptoms, renal function, serum calcium and bone mineral
density.
10.13 HYPERPARATHYROIDISM
Type
Serum calcium
PTH
Primary
Single adenoma (90%), multiple
adenomas (4%), nodular hyperplasia
(5%), carcinoma (1%)
Raised
Not suppressed
Secondary
Chronic renal failure, malabsorption,
osteomalacia and rickets
Low
Raised
Tertiary
Raised
Not suppressed
