1

2
3
Part:1
Surgery
Head injury
Primary injuries: at accident (fracture, hematoma, hemorrhage).
Secondary injuries: later on:
1- Hyperthermia increase intracranial pressure.
2- Hypotension hypovolemia.
3- Seizure increase brain demand.
4- Hypoxemia.
5- Hypoglycemia.
Head injury bleeding hematoma closed space compression of brain
secondary brain insult we must do decompression.
Do the following examinations:
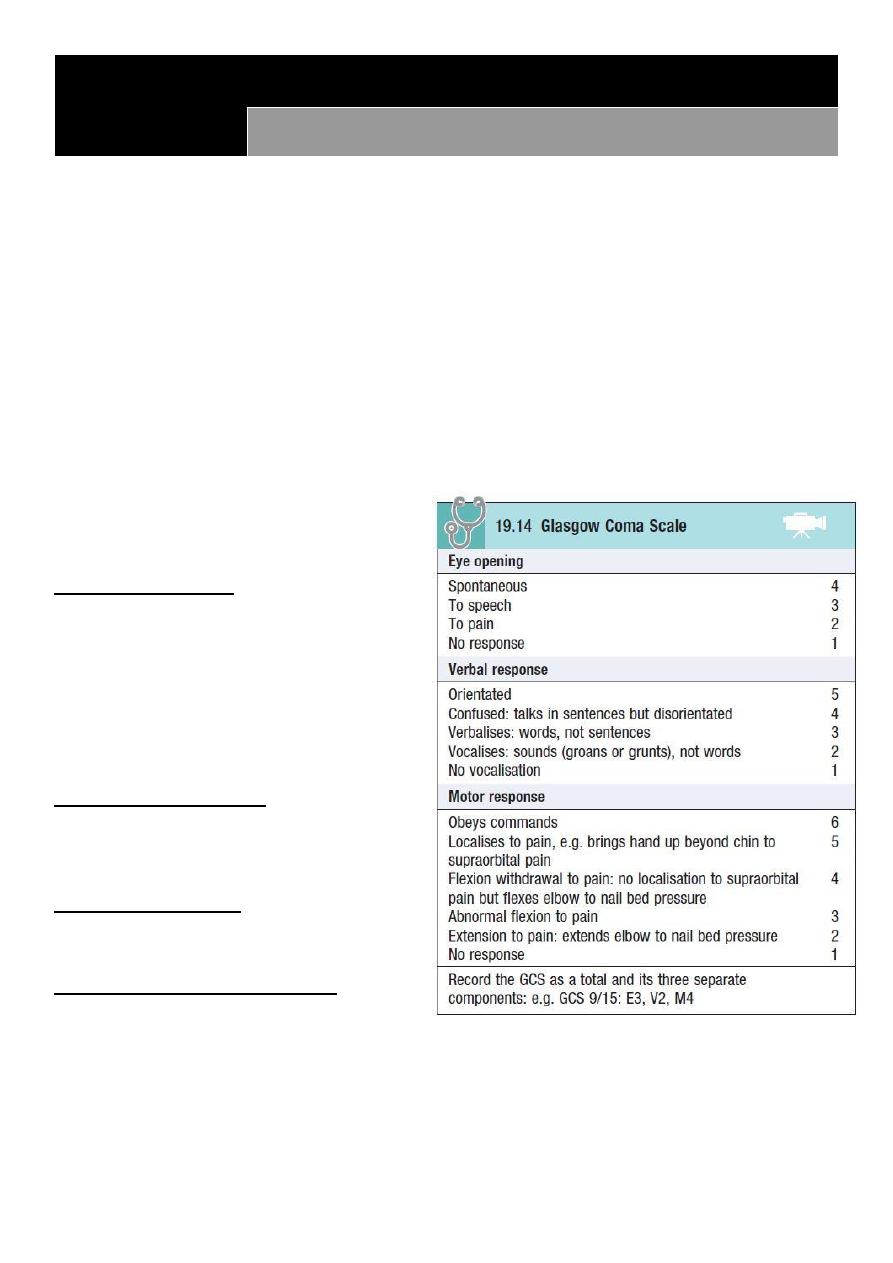
1- Glasgow coma scale.
2- Focal neurological signs.
3- Examination of pupil.
4- Signs of fracture at base of skull.
Glasgow coma scale:
From 0 to 3 dead person.
From 3 to 8 Severe.
From 8 to 13 moderate.
13 minimal.
14 and 15 normal.
8 or less patient need definitive
airway management.
Focal neurological signs:
Sensory examination.
Motor examination.
Reflexes examination.
Examination of pupil:
Dilatation of pupil in 3rd CN palsy.
Reactivity to the light.
Signs of fracture at base of skull:
Raccoon eye.
Bat sign.
Rhinorrhea and otorrhea.
Hemotympanum.
#Vital signs hypertension & bradycardia do CT scan see hematoma.
#Trait of increased intra-cranial pressure vomiting, hypertension, bradycardia.

4
#Indication of CT scan in head injury: (box in baily)
Low Glasgow coma scale.
Features of fracture of base of skull.
Focal neurological sings.
Deterioration of conscious level.
Age above 65.
Ante-grade amnesia.
Coagulopathy.
Seizure.
Alcoholic.
#Management:
First do primary and secondary survey of ATLS (ABCD).
High O2 flow.
Anticonvulsant foe seizure.
Glucose.
Fluid and electrolyte (but not give glucose water).
Correction of hyperthermia.
#Types of cranial hematomas:
Intra-axial hemorrhage: bleeding within the brain itself, or cerebral hemorrhage.
Extra-axial hemorrhage: bleeding that occurs within the skull but outside of the brain
tissue, falls into three subtypes:
o Epidural hematoma: rapidly accumulating hematoma between the dura mater and
the cranium.
o Subdural hematoma: occurs when there is tearing of the bridging vein between the
cerebral cortex and a draining venous sinus.
o Subarachnoid hemorrhage: is bleeding into the subarachnoid space (the area
between the arachnoid membrane and the pia mater surrounding the brain)
#Severity of head injury
Severe head injury (Glasgow Coma Scale score 3–8).
Moderate injury (Glasgow Coma Scale score 9–14).
Minor head injury (Glasgow Coma Scale score 15).
5
Part:2
Surgery
Neck swellings
Midline swelling
Lateral swelling
Thyroid enlargement
Branchial cyst
Thyroglossal cyst
Cystic hygroma
Peri-tracheal L.N enlargement
Sternocleidomastoid tumor
Single nodule in isthmus
Pharyngeal pouch
Chondroma of thyroid gland
Cervical lymphadenopathy
Sebaceous cyst
Lipofibroma
Thyroid cyst
Carotid body tumor
Mass related to skin
Thyroid enlargement
Dermoid cyst
Dermoid cyst
Lipoma
Sebaceous cyst, lipoma
Sub-hyoid bursa
Early stage of SCC
#History of neck swelling:
Onset, Duration, Possible cause, First symptom,
Associated symptoms, Progression, Persistent,
Multiplicity
Pain (10S), fever, weight change
Dysphagia, odynophagia, dysphonia, dyspnea, cough,
hemoptysis
Pain in the mouth, discomfort on eating, sore throats or ulceration, nasal discharge,
pain or blockage of the airway, pain in the throat or neck, changes in voice and
difficulty with breathing.
Family history, Personal history (Smoking, alcohol), Travel history
o Symptoms such as general malaise, fever and rigors and contact with people with
infectious diseases may indicate an infective cause of the swelling.
o Loss of appetite, loss of weight and pulmonary, alimentary or skeletal symptoms may
suggest a malignant cause.
o
Irritation of the skin associated with enlarged cervical lymph glands is often seen with
lymphoma
.
#Examination of neck swelling:
Inspection
Site (midline, anterior triangle, posterior triangle), Size, Shape, Surface, Skin over,
Surrounding, Scar, Other masses.
Palpation
Put gel on your hands.
6
Ask about pain.
Start away from the mass.
Examine: temperature, fluctuation, consistency, margin, overlying skin, attachment to
underlying tissue (fixity), fluctuation, reducibility, compressibility, cough impulse (in
pharyngeal pouch), pulsation (carotid), translumination (cystic hygroma, thyroid cyst,
thyroglossal cyst).
Percussion
In retrosternal extension of goiter (percuss on sternum) become dull.
Auscultation
Thyroid bruit in thyroid tumor for example.
7
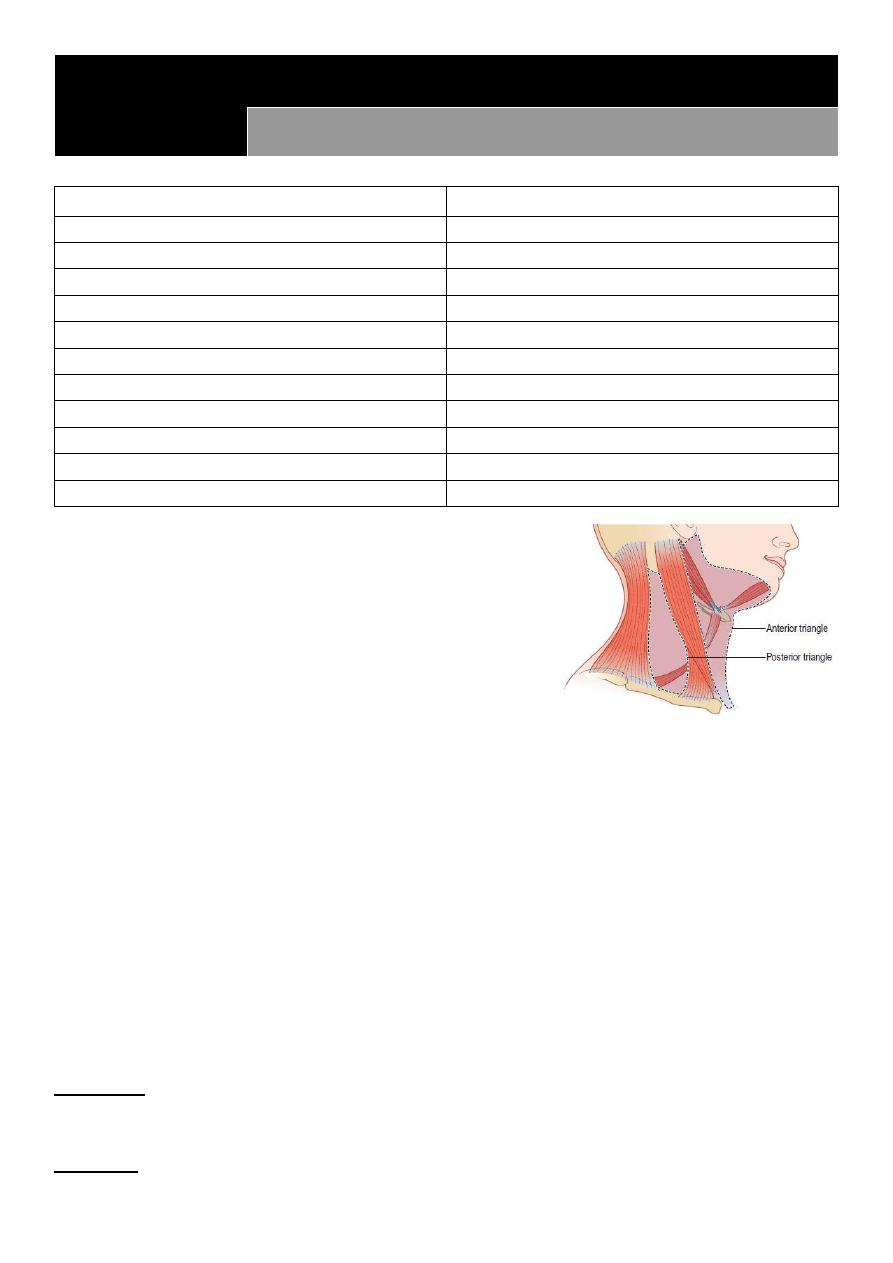
#Neck lymph nodes:
Information:
Lymph nodes in the neck are divided into anterior and posterior cervical groups:
Anterior cervical triangle is limited by the midline anteriorly, the clavicle below, and the
sternocleidomastoid muscle. It includes the submental, submandibular, jugular,
scalene, and supraclavicular lymph node groups.
Posterior cervical triangle is limited by midline, sternocleidomastoid, and trapezius
muscle. It includes the posterior cervical, post-auricular and the occipital groups.
Enlarged lymph nodes are examined for:
The lymph node areas involved.
Whether they are discrete or matted.
Approximate size of the lymph nodes.
Tender or not.
Consistency (Soft, rubbery, hard).
Mobile or fixed.
Abnormality of the overlying skin,
Levels of L.N:
Level 1 submental (1A) and submandibular (1B).
Level 2 Upper third of sternocleidomastoid.
Level 3 middle third of sternocleidomastoid.
Level 4 lower third of sternocleidomastoid.
Level 5 posterior triangle.
Level 6 peritracheal L.N.
Notes:
The anterior group is better examined from behind while the patient is sitting, and the
posterior group is examined from the front.
Examine the scalp if you find enlarged occipital and auricular L.N.
If the cervical L.N are enlarged, the axillary and inguinal L.N should be examined.
80% of enlarged L.N in adult is malignant.
Biopsy: used in case of solid mass or uncertain diagnosis.
Use FNA for diagnosis:
o If you find benign condition then do excisional biopsy.
o If you find limited malignant condition then do excisional biopsy.
o If you find extensive malignant condition then do radio or chemotherapy.
Causes of cervical lymphadenopathy:
Infection: Non-specific, Glandular fever, Tuberculosis, Syphilis, Toxoplasmosis, Cat-
scratch fever (Rochalimaea henselae)
Metastatic tumor: From the head, neck, chest and abdomen
Primary reticuloses: Lymphoma, Lymphosarcoma, Reticulosarcoma
Sarcoidosis

8
9
Part:3
Surgery
Thyroid gland
#Information:
Changes in hormone activity can be assessed by:
o Clinical examination.
o Measuring circulating tri-iodothyronine (T3) and thyroxine (T4) levels.
o Measuring the rate and quantity of radioactive iodine taken up by the gland.
Hormone secretion can be suppressed by:
o Iodine, which inhibits hormone release.
o Potassium perchlorate, which interferes with iodine trapping.
o Carbimazole and propylthiouracil, which inhibit the iodination of tyrosine and the
coupling of tyrosines to make thyronines.
o Destroying the gland surgically or with radiotherapy.
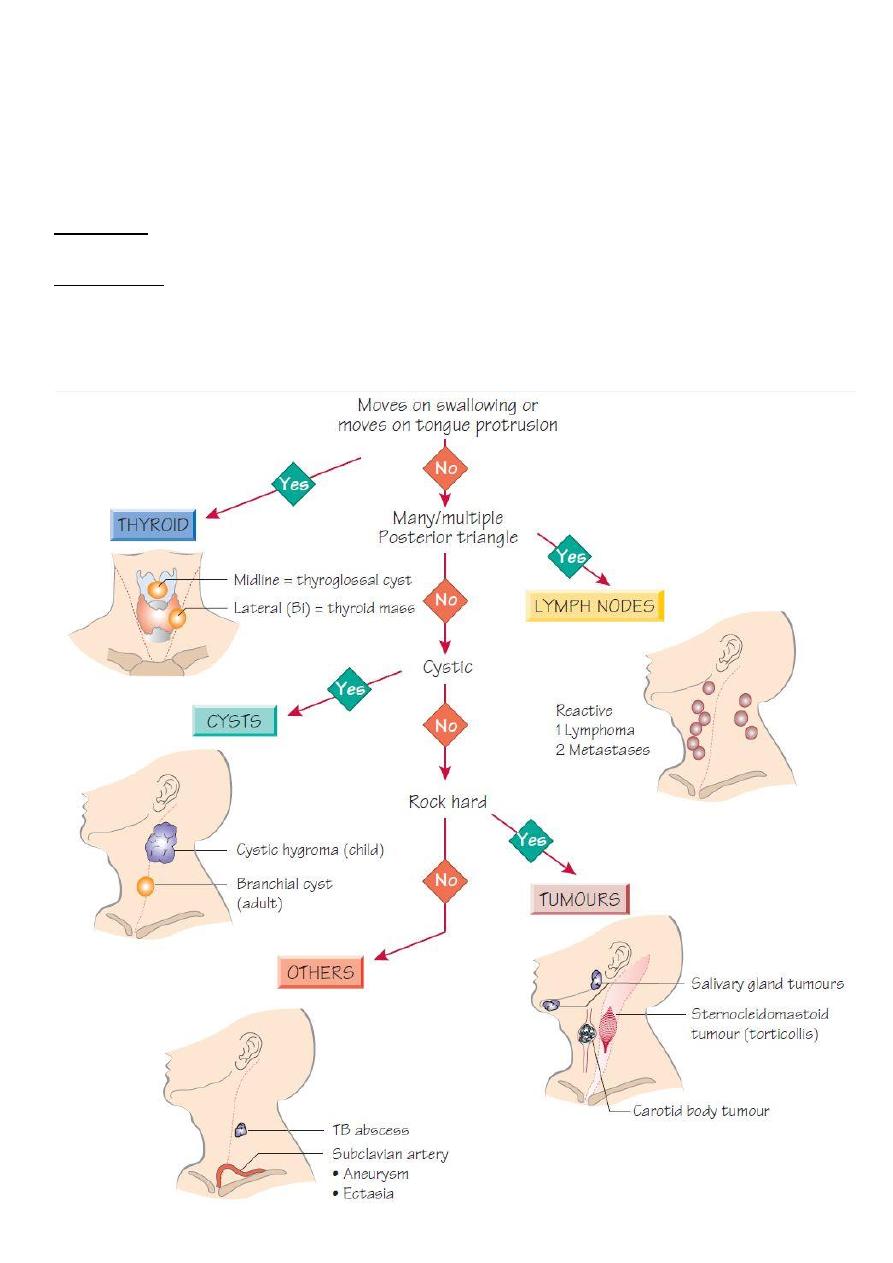
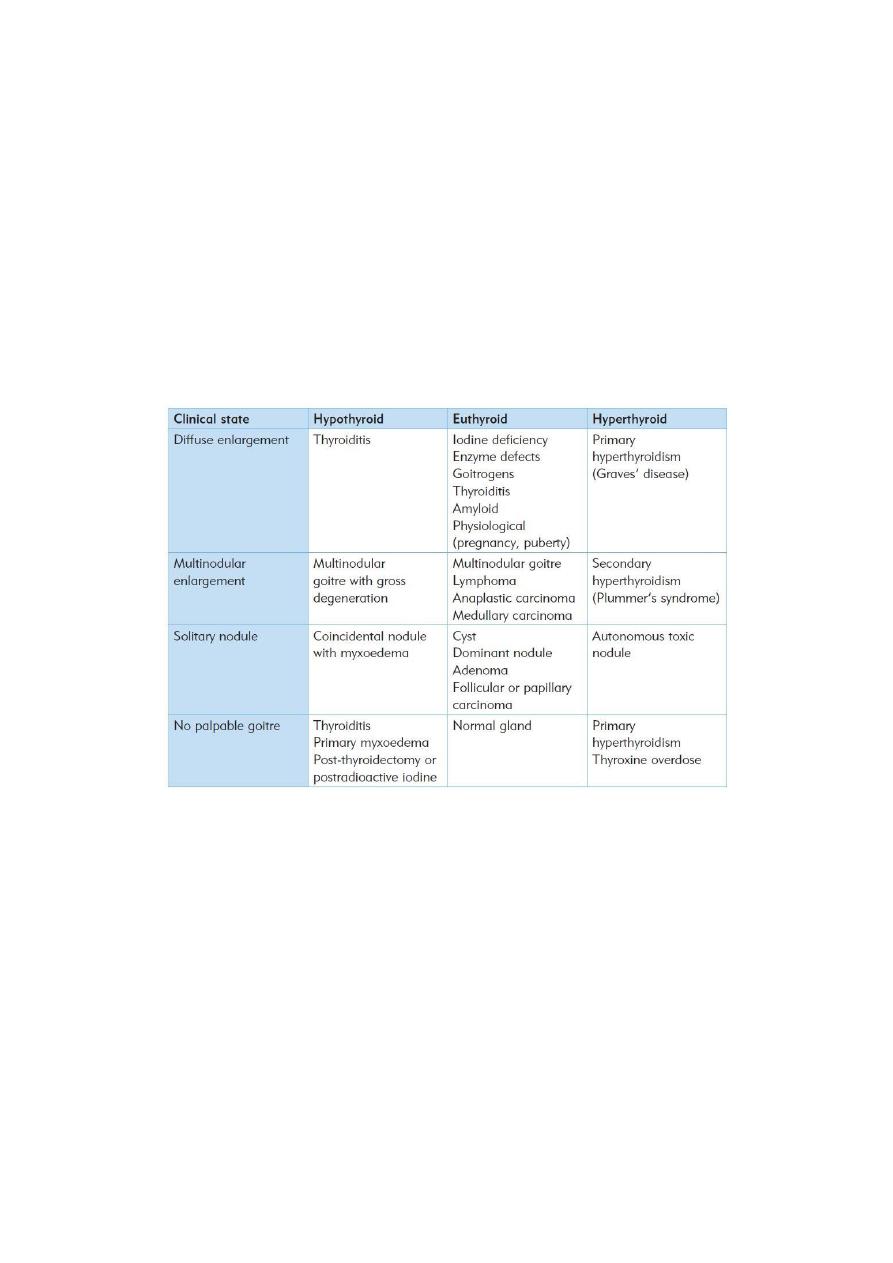
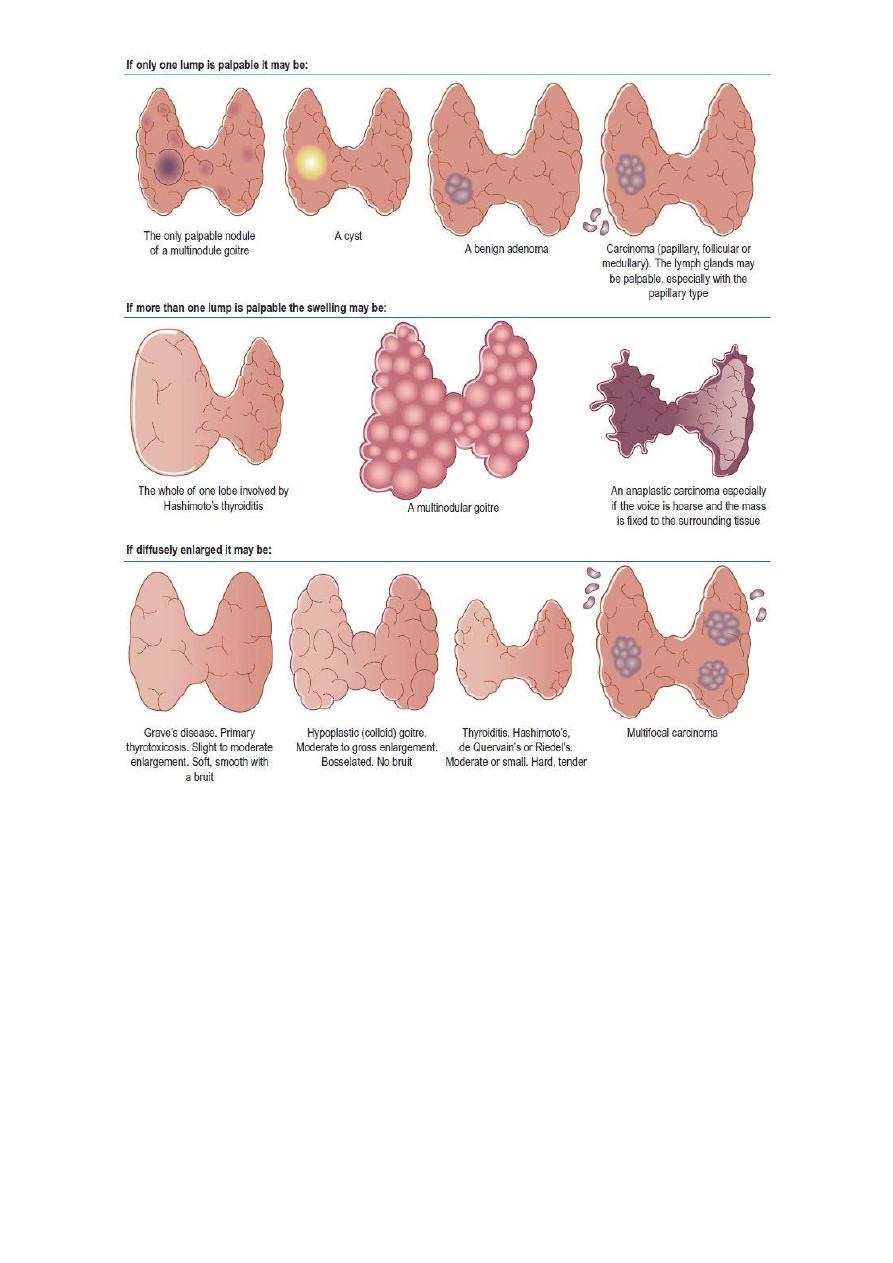
#Diagnosis of swellings in the neck:
History:
Is there one or more than one lump?
Where is the lump?
Is it solid or cystic?
Does it move with swallowing?
Multiple lumps: are invariably lymph glands.
A single lump:
In the anterior triangle that does not move with swallowing:
o Solid: Lymph gland, Carotid body tumor.
o Cystic: Cold abscess, Branchial cyst.
In the posterior triangle that does not move with swallowing:
o Solid: Lymph gland.
o Cystic: Cystic hygroma, Pharyngeal pouch, occasionally a secondary deposit of a
papillary thyroid carcinoma
o Pulsatile: Subclavian aneurysm.
In the anterior triangle that moves with swallowing:
o Solid: Thyroid gland, Thyroid isthmus lymph gland.
o Cystic: Thyroglossal cyst.
#Symptoms of thyroid disease:
The thyroid gland can cause two groups of symptoms and signs: those connected with the
swelling in the neck, and those related to the endocrine activity of the gland.
Neck symptoms:
11
o A lump in the neck: The majority of thyroid swellings grow slowly and painlessly.
o Discomfort during swallowing: This is not true dysphagia.
o Dyspnea: The whistling sound of air rushing through a narrowed trachea is stridor.
o Pain: occur in thyroiditis, Hashimoto’s disease, anaplastic carcinoma.
o Hoarseness: caused by a paralysis of one of the recurrent laryngeal nerves.
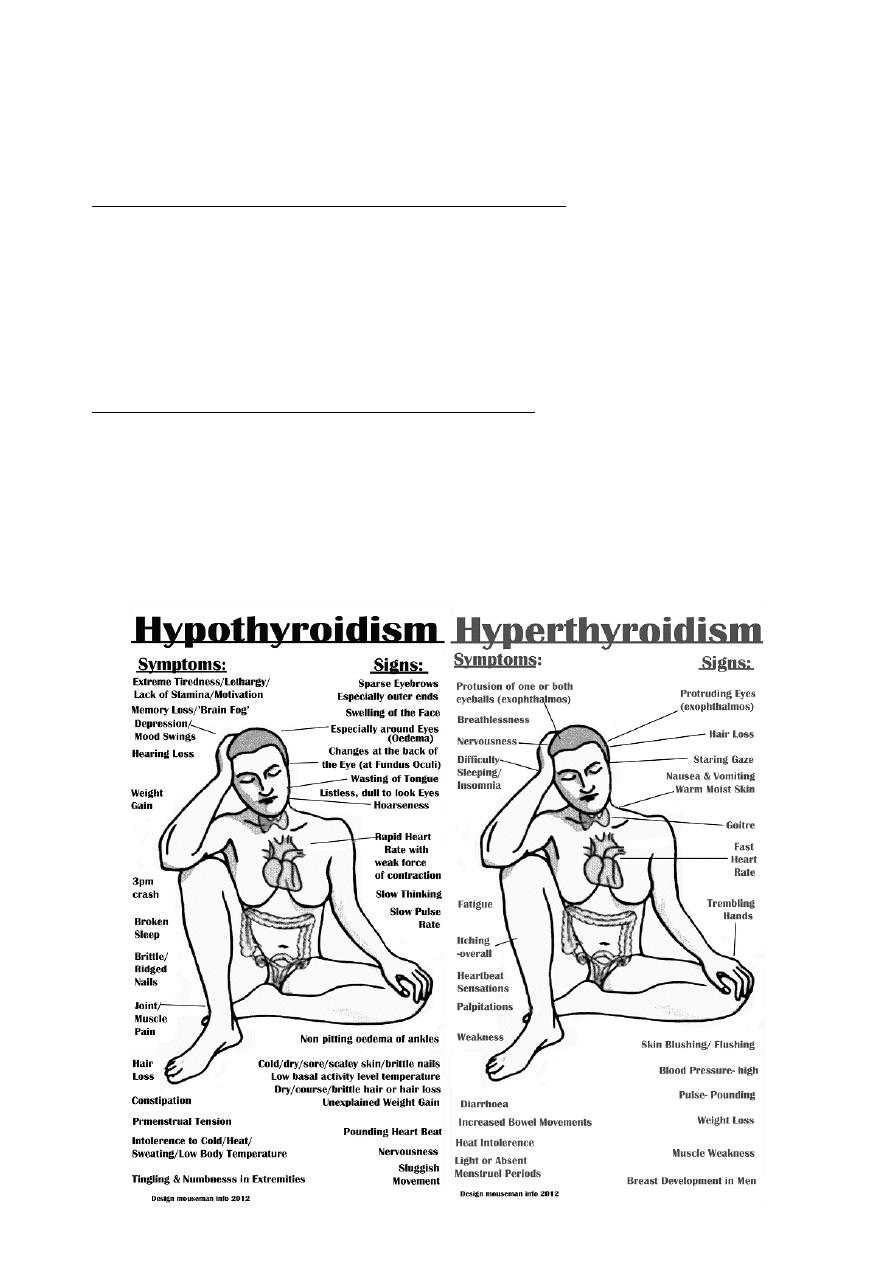
Symptoms and signs of hyperthyroidism/thyrotoxicosis:
o Nervous system: nervousness, irritability, insomnia, nervous instability, tremor of
the hands, full-blown thyrotoxic psychosis.
o Cardiovascular system: palpitations, breathlessness on exertion, swelling of the
ankles, chest pain, tachycardia, atrial fibrillation, dyspnea, peripheral swelling.
o Metabolic and alimentary systems: increase in appetite but loss of weight, diarrhea,
proximal muscle myopathies, preference for cold weather, excessive sweating,
intolerance of hot weather, amenorrhea.
Symptoms and signs of hypothyroidism/myxedema:
o Increase in weight, and constipation.
o Deposition of fat across the back of the neck and shoulders
o Slow thought, speech and action.
o Intolerance of cold weather.
o Loss of hair, especially the outer third of the eyebrows.
o Muscle fatigue.
o Dry skin and ‘peaches and cream’ complexion.

11
#History of thyroid gland:
Age, Sex, Geography, Diet, cause.
Local and general symptoms.
Duration of symptoms.
Family history.
Ask about: cold intolerance, sweating, appetite, sleep, menstrual problems.
Symptoms associated with malignancy: dyspnea, odynophagia, dysphagia, pain,
paresthesia, weight loss.
#Examination of thyroid gland:
Look at the whole patient:
o First confirm that the swelling in the neck is in the thyroid gland (move with
swallowing).
o Fast or slow movements and expressions, nervous and agitated.
o Thin or fat patient.
o What is the distribution of any wasting or fattening?
o Looks at thickness of cloths, sweating, feeling hot or cold.
o Pale or yellow lemon color occur in hypothyroidism.
o Loss of hair (in the outer third of the eyebrows) in hypothyroidism.
Look at the hands:
o Feel the pulse: Tachycardia (hyperthyroidism), bradycardia (hypothyroidism), atrial
fibrillation (thyrotoxicosis in middle or old age patient).
o Are the palms moist and sweaty?
o Is there a tremor? Thyrotoxicosis causes a fine, fast tremor.
o Look for finger clubbing, koilonychia, ecchymosis, wasting.
o Palmer erythema (hyperthyroidism) carpel tunnel syndrome (hypothyroidism).
Examine the eyes:
o Eye symptoms: double vision, pain in the eye if the cornea ulcerates.
o Eye signs: ecchymosis, bruises, sub-conjunctival hemorrhage, diversion sequence.
o Lid retraction and lid lag:
This sign is caused by over activity of the involuntary (smooth muscle) part of
the levator palpebrae superioris muscle.
Upper lid raised, Lower lid normal.
This is not exophthalmos.
o Exophthalmos:
The eyeball is pushed forwards by an increase in vretro-orbital fat, edema and
cellular infiltration.
Both lids moved away from center with sclera visible below or all-round the iris.
Because the eyes are pushed forwards, the patient can look up without
wrinkling the forehead.
In severe exophthalmos, the patient cannot close their eyelids and may develop
corneal ulceration
.
o Ophthalmoplegia:
It is weakness of the ocular muscles.

12
Caused by edema and cellular infiltration of the muscles themselves and of the
oculomotor nerves.
Particularly of the superior rectus and inferior oblique muscles (cannot look up
and out)
o Chemosis:
It is edema of the conjunctiva.
Caused by the obstruction of normal venous and lymphatic drainage of the
conjunctiva by the increased retro-orbital pressure.
Inspect the neck:
o Ask the patient to swallow: give a sip of water, all thyroid swellings ascend during
swallowing.
o Observe the general contours and surface of the swelling: the skin can be puckered,
tethered and pulled up by swallowing.
o Ask the patient to open their mouth and then to put out their tongue: If the lump
moves up as the tongue comes out, it is thyroglossal cyst.
o The neck veins will be distended if there is a mass obstructing the thoracic inlet.
o Is thyroid cartilage in the center of the neck or deviated to one side?
o See if there is scar (surgical or radiation scar).
Palpate the neck from the front:
o Confirm your visual impression of thyroid size, shape and surface, and to find out if
it is tender.
o Note the number, size, site, shape, nodularity, fixity, texture, consistency,
temperature, overlying skin for swelling.
o Can get below it or not? (Retrosternal extension).
o Check fixity by contraction of sternocleidomastoid muscle.
o Check the position of the trachea.
o Examine the position of thyroid cartilage.
Palpate the neck from behind the patient:
o Place your thumbs on the ligamentum nuchae and tilt the patient’s head slightly
forwards to relax the anterior neck muscles.
o Ask the patient to swallow while you are palpating the gland.
o With a retrosternal extension of the thyroid, it is important to assess whether you
can feel the lower border of the gland on swallowing or whether there is still a
significant extension lying behind the sternum.
o Feel the tenderness, shape, size, surface, consistency of thyroid gland or neck lump.
o Palpate the whole of the neck for any cervical and supraclavicular
lymphadenopathy.
Percussion:
o Used to define the lower extent of a swelling that extend below the suprasternal
notch.
o Percuss along the clavicles and over the sternum and upper chest wall.
o This can be done when standing in front of or behind the patient.
Auscultation:
o Listen over the swelling.
13
o Thyrotoxic and vascular glands and lumps may have a systolic bruit.
General examination:
o Examination of cardiovascular and nervous systems for any evidence of
hyperthyroidism or hypothyroidism.
o Examination of submental, submandibular, cervical, supraclavicular L.N.
o Reflexes: hyper reflexia (hyperthyroidism), slow relaxation phase (hypothyroidism).
#Examination of a patient with a goiter:
Look at the whole patient for agitation, nervousness or lethargy.
Examine the hands for sweating, tremor and tachycardia.
Examine the eyes for exophthalmos, lid lag, ophthalmoplegia and chemosis.
Examine the neck: always check that the lump moves with swallowing.
Palpate the cervical lymph glands.
Notes:
The only disease that move with protrusion of tongue is thyroglossal duct.
Cystic lesion with positive trans-lamination test is Branchial cyst.
Diffuse physiological thyroid enlargement: in growth, puberty, pregnancy need of
thyroxin increase so TSH level increase.
Previously doctors said that there is congenital ectopic thyroid tissue, but now they say
that this condition is not present, and there is acquired metastatic papillary carcinoma
instead of it.
Pretibial myxedema in grave's disease.
Proximal myopathy in hyperthyroidism.
Myxedema coma loss of consciousness due to hypoglycemia in the end stage of
hypothyroidism.
Berry's sign: In goiter, the carotid artery may be pushed posteriorly by the enlarged
thyroid and this is called displacement. When the infiltration of the carotid by the
tumor, the carotid pulse will be absent on that side. This is absent carotid pulse is
called Berry's sign. (examine it by palpation).
14
#Investigations in thyroid gland diseases:
Ultrasound of the neck: state of thyroid gland, calcifications, nodularity, L.N.
Radio-active iodine: diagnostic and therapeutic, detect hyperactive nodules.
X-ray: shifting of the trachea, widening of the mediastinum.
CT & MRI.
Thyroid function test: TSH, T3, T4, Thyroglobulin.
o Patient take thyroxin T4 high, T3 normal, TSH low.
o Hypothyroidism T4 low, T3 low, TSH high.
o Primary hyperthyroidism T4 high, T3 high, TSH low.
o Secondary hyperthyroidism T4 high, T3 high, TSH high.
Auto-antibody titers.
Blood test: serum calcium, blood count, ESR, CRP, CBC.
FNA, core biopsy, lobectomy (incisional or excisional biopsy).
Laryngoscope.
ECG: for atrial fibrillation.

15
Part:4
Surgery
Salivary glands
#Causes of swelling of a salivary gland:
Acute infection: Viral (e.g. mumps), Bacterial (e.g. Staphylococcus).
Duct obstruction
Sialectasis (chronic infection)
Tumour: Benign, Malignant.
Sarcoidosis (Mikulicz’s syndrome)
Sjogren’s syndrome
#Examination of Salivary gland swellings:
1- Approach
Sit/kneel to be at the same level as the patient's face
Examine as for any lump
2- Inspect
Swelling in the region of the parotid gland (lies wedged between the
sternocleidomastoid and the mandible) and the submandibular gland (at the angle of
the jaw, wedged between the mandible and mylohyoid)
Look for scars and the opening of a fistula (can follow parotidectomy or long-standing
parotid traumatic injury)
Stand back and look for facial asymmetry which occurs if the VIIth nerve is involved
with a parotid lesion.
3- Palpate from behind
Walk behind the patient and enquire about tenderness before palpating the swelling
Unilateral or bilateral?
Fixity? - ask patient to clench teeth
examine for other features as for any lump
check cervical lymphadenopathy
4- Other tests
Look inside mouth with pen torch at opening of parotid duct (Stensen's duct): opposite
upper 2nd molar and opening of submandibular duct (Wharton's duct)
Look for inflammation and pus, or the presence of a stone
Palpate the parotid duct and submandibular duct openings wearing a pair of gloves
Palpate the submandibular gland bimanually with a finger in the mouth and another
finger below the angle of the jaw
5- Completion
Perform a full ENT examination
16
#Parotid gland:
History:
Age: more common in the elderly and the debilitated.
Symptoms: pain, swelling, fever, rigor, others.
Systematic questions.
Previous history.
Examination:
Inspection: site, size, shape, surface, skin over, surrounding, scar.
Palpation: Tenderness, temperature, other features of swelling.
Mouth examination:
o Inspection: The orifice of Stensen's duct is opposite the second upper molar tooth
(color, pus, edematous).
o Palpation Feel the mouth of the duct (any thickening, swelling, tenderness).
Facial nerve examination:
o Facial deviation (as neurological exam).
o Corneal reflex.
o Special sensation to anterior 2/3 of the tongue.
Fixity: tension of masseter muscle, vertical and horizontal fixity, fixity to underlying
tissue.
Scar: searching for scar of previous surgery by elevating the ear.
Tonsillitis: open the mouth and see the tonsils.
Notes:
The parotid gland cannot be palpated bimanually because it lies behind the anterior
edge of the masseter muscle and the vertical ramus of the mandible.
Gentle pressure on the gland may produce a purulent discharge from the orifice of the
duct.
Why stones in submandibular gland is more than in parotid gland? The duct of
submandibular gland is more vertical and its secretion is mucous.
#Submandibular gland:
History:
Age: most common in young to middle-aged adults.
Sex: Males and females are equally afflicted.
Symptoms: pain and swelling beneath the jaw, caused by obstruction of Wharton’s
duct.
Development: The symptoms may recur and remit for periods of a few days or weeks if
the stone moves about in the duct, sometimes obstructing it, sometimes not.
Previous history.
Examination:
Inspection: site, size, shape, surface, skin over, surrounding, scar.
Palpation:
o Ballotable (finger below the tongue and finger from neck).
o Examine wharton's duct below the tongue.

17
Percussion.
Auscultation.
Nerves examination:
o Hypoglossal nerve: motor to the tongue examine tongue movement.
o Lingual nerve: sensation of posterior 1/3 of tongue.
o Marginal mandibular nerve.
Important structures of submandibular surgery: LDH Lingual nerve, Duct, Hypoglossal
nerve.
#Sublingual gland:
Ranula: caused by trauma or fibrosis that close the duct.
Ranula (unilateral), Ranging Ranula (bilateral).
Treatment: excision from mouth.
#Notes:
Stones: cause pain when see or eat food.
Fixity of mass:
o Contraction become more prominent (more movable) mass in the kin
o Contraction become more prominent (more fixed) mass in the fascia of
muscles.
o Contraction become less prominent mass deep to muscles.
Injury to hypoglossal nerve during surgery lead to atrophy of tongue in the
ipsilateral side.
